Abstract
HIV incidence is increasing among men who have sex with men (MSM) despite years of prevention education and intervention efforts. Whereas there has been considerable progress made in identifying risk factors among younger MSM, older MSM have been largely neglected. In particular, the role of alcohol and drug use in conjunction with sex has not been thoroughly studied in older MSM samples. This article reviews the small body of literature examining the association of substance abuse and risky sexual behavior in this population and provides a methodological critique of the reviewed studies. The data show that older MSM are engaging in risky sexual behavior, with the likelihood of engaging in risky sexual activities increasing with the use of alcohol and other drugs. Methodological limitations prevent strong conclusions regarding whether the sexual risk behaviors of older MSM differ from those of younger MSM, and the extent to which alcohol and drug use may differentially contribute to engagement in sexual risk-taking as a function of age. Future research is needed to clarify these associations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite decades of HIV/AIDS awareness and prevention efforts, the rate of new HIV infections appears to be on the rise in recent years. From 2004 to 2007, the Centers for Disease Control (CDC) reported a 15% increase in the incidence of HIV among the 34 states with established HIV reporting [1]. In addition to an overall increase in new HIV diagnoses, the CDC reports a 26% increase in new HIV diagnoses among men who have sex with men (MSM). Although other risk groups (injection drug users and high-risk heterosexuals) have experienced a decrease in HIV diagnoses since 2000, rates among MSM continue to rise, with male-to-male sexual contact accounting for 53% of all new HIV infections in 2006 [2]. It is clear that the HIV prevention needs of men who have sex with men have gone beyond the reach of current strategies, with the development of more effective education campaigns needed to focus on the specific risk factors associated with HIV transmission in this population.
Although continued research is necessary to understand the unique behavioral, social, and psychological factors associated with risky sexual behavior specifically among MSM, one predominant risk factor of HIV infection noted repeatedly in generalized sexual risk literature is alcohol use. Based on the transmission hypothesis [3], the alcohol myopia theory and the alcohol expectancy theory [3–5] have been the foundation for numerous empirical studies focusing on more generalized populations. However, existing findings regarding the association between alcohol use and sexual risk taking specifically among MSM are not definitive. A 2009 literature review by Woolf and Maisto [6] reports that due to a consistent lack of experimental study design, the nature of the relationship between alcohol use and risky sex behaviors in MSM remains unclear. Although it is the case that “in general, the global, situational, and event-level studies showed a significant relationship between alcohol use and unprotected anal intercourse (UAI), continued research is warranted in order to determine under which specific conditions alcohol use leads to risky sex” [6, p. 777]. Similarly, studies focusing on the association of sexual risk to stimulant drug use suggest that substances such as methamphetamine, cocaine, poppers, and ecstasy are behaviorally disinhibiting, which likely contribute to increased rates of unprotected sex and HIV seroconversion among recreational drug users [7–10]. However, findings are again often limited to global and situational level studies with few experimentally based examinations.
A greater understanding of the conditions that moderate the relationship between alcohol or substance use and sexual risk behavior among MSM is needed to design more effective HIV education and prevention campaigns. As noted by the Global HIV Prevention Working Group [11], targeted, localized efforts tailored to meet the needs of a specific population increase prevention success. HIV prevention efforts have historically stratified their messages according to risk categories such as sexual identity and drug use, and one area that has begun to increase in focus recently is age-specific prevention. Whereas increasing emphasis has been placed on younger MSM populations, a small body of literature has begun to examine the ways in which alcohol and other drug use affect engagement in risky sexual behaviors among an older MSM population. This paper aims to review and offer a methodological critique of the existing literature focusing on the association of alcohol and substance use to sexual risk among older MSM. To give context for the importance of this review, we first provide a brief overview of the current risky sexual and substance-related behaviors of older MSM.
Age-Specific Risks: The Argument for Focus on Older MSM
Several studies have offered evidence of a “young age risk effect” for HIV among MSM [12, 13], though this finding is not consistently noted in the literature. Indeed, other studies [14, 15] have found no evidence of a young age risk effect, with a study by Chen, Weide, and McFarland [16] showing elevated risk behavior among both younger and older MSM. Additionally, as noted by Crepaz et al. [17], the finding that younger MSM are more likely than older MSM to engage in UAI does not necessarily indicate that younger MSM are more at risk. For example, UAI in the context of a monogamous, HIV− relationship carries no risk for HIV infection.
One consequence of accepting the “young age risk effect” is the tendency to ignore the unique challenges and prevention needs of older MSM. As noted by Anderson [18], most education programs to date have targeted younger at-risk groups. Among more general studies of MSM, historically there has been a lack of research on older MSM dating back to some of the first studies on homosexual men. In a 1986 paper, J. Harry [19, pp. 21] brought attention to the fact that samples “appear to under-represent (gay men) over 45 years of age”. The same lack of representation continues today in risk literature, as stated by Jimenez [20, pp. S222]: “older MSM largely have been ignored by research and intervention efforts aimed at curbing the HIV pandemic.” This under-representation may be due to the fact that many studies recruit samples from gay bars and gay organizations—activities in which older men are less likely to participate [21].
HIV and Sexual Risk Behaviors Among Older MSM
As the CDC [22] reported, in recent years there has been an increase in new HIV/AIDS diagnoses among Americans age 50 and older, accounting for 17% of new diagnoses. In addition, persons aged 50 and over accounted for 24% of persons living with HIV/AIDS and 35% of all deaths from AIDS. Although these latter increases may or may not exclusively represent an actual increase in the rate of infections (vs. the aging of the HIV+ population due to treatment advances), findings provide evidence that older adults are continuing to engage in behaviors that put them at risk for contracting HIV. Indeed, in a nationwide study examining risk behaviors among MSM (N = 4,295), findings indicated that both younger (age 16–25) and older (age 46 and older) MSM engaged in risky sexual behaviors, though they differed in the types of sexual risk behavior that they engaged in [23]. Whereas younger MSM were more likely to engage in UAI with HIV-negative partners or partners of unknown HIV status, MSM age 46 and older were more likely to engage in unprotected anal intercourse with HIV+ partners. Older MSM were also more likely than their younger counterparts to have at least ten partners over a 6-month period.
Research suggests that older men who have sex with men may face a unique set of challenges, and some of these issues may play a role in their risky sex behavior. A series of interviews led by Murray and Adam [24] revealed that many older gay men experience concerns about living up to the idealized standard of younger gay men, panic and dread at the loss of their desirability, and feelings of worthlessness, depression, and isolation. These factors may result in older MSM “trading off” safe sex in order to fulfill their emotional needs. There are also physiological problems to consider: many men in the Murray and Adam [24] study reported a struggle with erectile dysfunction, which condom use exacerbates. These feelings and experiences might influence older MSM to compromise their safety, and, in some instances, they may be putting themselves at more of a risk than younger MSM. Furthermore, older MSM report more negative peer norms regarding safe sex [12] and rate protected anal intercourse as less pleasurable than younger MSM [15].
Additionally, although younger men account for the majority of new HIV infections among MSM (especially among ethnic minority populations), engaging in sexual risk behaviors as an older MSM carries its own specific risks. As reported by the CDC [22], as the age at time of HIV diagnosis increases, the average time to an AIDS diagnosis decreases. Similarly, advanced age at time of AIDS diagnosis is inversely related to survival rate at 12, 24, and 36 months following the diagnosis. Findings suggest that, although rates of HIV infection seem to convey a higher level of risk with younger populations, older adults exposed to HIV may suffer more severe consequences in terms of rapid health declines and decreased survival with the disease. As such, under-representation of older MSM in risk reduction research is a significant problem.
Alcohol and Substance Use Among Older MSM
Although there have been several studies that looked at age differences in relation to factors associated with risky sex among MSM, there has been a paucity of research on age-related differences in the effects of substance use on risky sex behaviors. Indeed, such factors as partner status [17], having sex with a female partner [25], feeling invulnerable to AIDS [25], intercourse type [26], and peer norms [12] have been examined and found to have differential effects on sexual risk behavior for older versus younger MSM. As alcohol and drug use is a common topic in general MSM literature, especially in relation to HIV risk behavior, the lack of research focusing on substance use and risky sexual behavior among older MSM signifies an important gap in the literature.
Although existing research has shown that alcohol consumption, use of most illegal drugs, and presence of substance use disorders tend to decrease over the lifespan [23, 27, 28], several factors demonstrate the importance of examining risky alcohol and substance use behaviors in older populations. First, although older adults tend to drink less than their younger counterparts, patterns are shifting, such that more recent cohorts of older adults are drinking more than older adults of previous generations [28]. Therefore, as the population of MSM continues to age, there is an increasing chance they will be drinking at elevated levels and will experience the behavioral and health risks associated with increased alcohol consumption. Second, although Salomon et al. [23] found that younger MSM were more likely to have used marijuana, hallucinogens, cocaine, and amphetamines during the study’s 6-month assessment period, older MSM (age 46 years and older) were more likely to have used inhaled nitrates/poppers and to have injected drugs including heroin and steroids, putting them at high risk for HIV and other communicable diseases. Additionally, older adults with elevated alcohol consumption and substance use (especially those over 65) may be prone to consequences rarely noted among younger populations such as aggravation of preexisting conditions like stroke, hypertension, memory loss, or other cognitive dysfunction [28]. Finally, as older persons are more likely to be taking medications associated with declining health, they may also be at increased risk for experiencing negative behavioral and medical consequences related to mixing alcohol and illegal drugs with prescription medications, such as confusion, decline in decision making capabilities, and serious risks to their health [28]. Given these concerns, it is important to gain a better understanding of the ways in which alcohol and other drug use affect engagement in risky sexual behaviors among an older MSM population. This paper aims to review and offer a methodological critique of the existing literature focusing on the association of alcohol and substance use to sexual risk among older MSM. Subsequent sections will include discussions of the search strategy and inclusion criteria, a brief review of included studies, followed by a methodological critique of the literature.
Methods
Search Strategy and Criteria for Inclusion
The aim of this critical literature review, then, is to identify and discuss the existing research related to alcohol and substance use and risky sexual behavior in older MSM, as well as to note limitations of the reviewed studies and directions for future research. Articles for this review were obtained by conducting a combined PsycINFO and PubMed search using terms for age (“age differences,” “older,” “aged”), MSM (“MSM,” “male homosexuality,” “same-sex intercourse,” “gay men”), high-risk sexual behavior (“risky sex,” “sexual risk,” “condom use,” “UAI”), and substance use (“substance use,” “alcohol,” “drugs”). From this list, the articles selected were restricted to those using data collected after 1981 (the announcement of AIDS, its transmission, and its dangers), those that looked specifically at MSM (rather than a larger at-risk group), and those that examined age differences in samples including participants over the age of 50. The 50 years of age cut-off used to define “older MSM” in this review was chosen to be consistent with age group categories used often by the CDC [1, 2, 22] when describing HIV/AIDS epidemiology. Based on these inclusion criteria, nine studies were selected, with a detailed account of methodology, sample size, age categorization, and major study findings provided in Table 1.
The following review of these studies is arranged according to the specificity of the research design. Studies that investigate substance use at the global level are the least specific and will be discussed first, followed by studies with a situation level approach, and, finally, studies at the event level. Global association studies are those that examine the correlation between the frequency (or quantity) of substance use and risky behavior. Situational association studies examine substance use in conjunction with risky sexual behavior, for example, by assessing the experience of drinking alcohol before or during unprotected sex in a certain time period. Event-level studies are the most specific and examine substance use in relation to a specific sexual partner or act. A summative methodological critique of the literature will be included following the review of all included studies.
Results
Substance Use and Sexual Risk Behavior Among Older MSM: Global Studies
Four studies met the inclusion criteria of this review and examined the relationship between substance use and risky sex in MSM at the global level. Klitzman, Greenberg, Pollack, and Dolezal [29] examined the use of MDMA (ecstasy) and its relationship to risky sexual behaviors among men who have sex with men. The relationship between the use of MDMA and risky sexual behavior among older MSM is of particular interest due to its common use in the gay community and the previous finding that MSM who use MDMA engage in UAI more frequently than non-using MSM [29]. Of the 733 MSM surveyed, 100 (13.7%) reported ecstasy use in the past 6 months. Findings from multiple logistic regression analyses indicated that MSM reporting ecstasy use tended to be younger and more likely to engage in risky sex behaviors including increased frequency of URAI and UIAI. Although high frequency MDMA users tended to be younger and more likely to visit bars and clubs, no significant differences were noted in regards to risky sexual behavior between high frequency and low frequency MDMA users [29]. Overall, the findings of this study indicate that MDMA users are more likely to be younger and are more likely to engage in risky sex behaviors, compared to MSM who did not report MDMA use in the assessment period. The authors propose one possible explanation for the difference in rate of use between younger and older MSM is the finding that MDMA is most frequently used at clubs in the early hours of the morning, where older MSM may have less exposure to the drug. This hypothesis is consistent with the finding that weekly bar/club attendance declines with age [29]. Indeed, only one participant over the age of 50 (.76%) reported using ecstasy in the past 6 months.
In a second global study, Dolcini, Catania, Stall, and Pollack [8] presented HIV prevalence and risk behavior information for urban MSM over the age of 50 using self-report (via individual phone interviews) and biomedical testing data. Of the 507 older MSM surveyed, 13% were HIV positive as self-reported and verified by HIV testing procedures several months after the phone interview. Findings from univariate analyses indicated that, although the median number of sexual partners decreased with age, a significant portion of the older MSM sample reported having multiple sexual partners in the past year. For example, 25% of men aged 60–69 reported having nine or more sexual partners within the past year. In examining correlates of high risk sex (UAI with sero-discordant or unknown status partners) among older MSM, researchers reported that moderate substance use was predictive of engaging in unprotected sexual activity, such that 12% of moderate substance users compared to 5% of heavy drug users and <3% of light/non-users reported engaging in UAI. Similarly, moderate drug use was significantly associated with having an HIV positive serostatus, such that 35% of moderate substance users reported being HIV+, as compared to 15% of heavy users, 10% of light users, and 9% of non-users. Similar findings were noted for younger MSM in the sample. Although it may be expected that the heaviest drug users would be more likely to engage in risky sex, the authors propose one possible explanation for the findings. They assert that heavier drug use may inhibit social and sexual functioning, thereby decreasing the chances of persons finding partners at typical gay-associated social venues and, if they do, successfully engaging in sex [8]. Overall, the findings of this study indicate that older MSM continue to have active sexual lives and engage in high risk behaviors, with moderate levels of substance use being associated with increased likelihood of engaging in sexual risk behaviors and seroconverting.
The two remaining global studies performed (Ostrow et al. [9]; Plankey et al. [10]) draw data from the larger longitudinal Multicenter AIDS Cohort Study, with similar analyses performed on the sample during follow-up periods of 1984–2003 and 1998–2008 respectively. In both studies, the authors examined the relationship between substance use and the incidence of UAI and seroconversion. In the earlier study by Plankey et al. [10], MSM aged 46 or older accounted for approximately 10% of the sample (N = 4003) and 5% of seroconverting participants as based on biospecimen testing completed at each 6 month assessment period. In the later examination by Ostrow et al. [9], MSM over the age of 46 accounted for a larger portion of the sample (N = 1667), making up 47% of the total sample and 27% of the men who seroconverted in the follow-up period. Analyses were not conducted separately for older MSM, with overall findings from both studies indicating that that increasing age was actually a protective factor against seroconversion. In Plankey et al. [10] findings from univariate analyses pertaining to the entire MSM sample indicated that increased chance for seroconversion was primarily related to increased numbers of UAI partners, with use of methamphetamine, cocaine, poppers, ecstasy, and alcohol also being independently predictive. Number of UAI partners and use of illicit substances also remained significant in the multivariate model with methamphetamine and popper use increasing the likelihood of seroconversion by 1.5–2 times respectively [10]. Findings from Ostrow et al.’s [9] examination of “sex drug combinations” were similar, with multivariate findings predicting seroconversion indicating that 41% of the model’s variance was accounted for by the number of unprotected anal receptive sex partners (URASP) and 33% was predicted by the use of “sex drug combinations” such as stimulants, poppers, and erectile dysfunction drugs. Given this study’s use of advanced statistical techniques, biomedical testing, and the sample’s significant portion of MSM over the age of 46, findings from Ostrow et al. [9] in particular provide a strong argument for the relationship of substance use to engagement in sexual risk behaviors among older MSM.
Substance Use and Sexual Risk Behavior Among Older MSM: Situational Studies
Three studies assessed substance use and risky sexual behavior at a situational level; that is, the use of alcohol or drugs before or during sexual encounters within a predetermined assessment time frame. The first study, by Dufour et al. [25], was longitudinal in nature and assessed the age-related correlates of risky behavior among HIV-negative MSM in an attempt to corroborate the young age risk effect. Within this study, participant age was categorized as those less than 30 years old (n = 355) and those older than 30 (n = 455), reflecting the pre- and post-AIDS period. Few age-related differences with regard to sexual risk behavior emerged in the univariate analysis, as the rate of UAI with casual partners did not significantly differ between the two age groups. However, the data did show that older MSM reported higher rates of sex in bathhouses and having more than five casual partners in the past 6 months than did their younger counterparts. With regards to UAI with a casual partner, 13% of younger and 12% of older MSM reported this behavior in the past 6 months. For both older and younger MSM, participants who reported frequent use of alcohol or drugs prior to sex were more likely to report engaging in UAI with casual partners in the past 6 months. Among older MSM, additional correlates of UAI with a casual partner were noted, such that those having UAI with a regular partner in the past 6 months, sex with females, ever having UAI with an HIV-positive partner, and perceived invulnerability to AIDS tended to be more likely to have unprotected anal intercourse with casual sex partners.
Because of the situational design of this study, the authors were able to make a stronger argument from their analyses about the relationship between alcohol use and risky sexual behavior than would be possible using a global assessment approach. In this regard, Dufour et al. [25] concluded from their findings that “frequent alcohol or drug use before anal sex with casual partners was strongly predictive of unprotected anal sex” for both younger and older MSM (p. 276). The authors also conclude that that there is little evidence supporting the existence of a young age risk effect, in that younger and older participants in their study demonstrated very few differences in sexual risk behavior.
In a second situational study, Darrow et al. [7] used cross-sectional surveys to assess for recreational drug use and risky sexual behaviors among MSM in Miami (N = 407) with a wide age range of 18–73 (50% over age 37). Among this sample, 77% reported at least one incident of anal intercourse in the past year, with 62% reporting at least one incident of UAI. Descriptive analyses also indicated that 40% of the entire MSM sample reporting using alcohol or recreational drugs during at least one episode of anal intercourse. Although older MSM were not examined separately, univariate analyses indicated that URAI in the past month was significantly associated with younger age (under 35 years) and being HIV positive or having AIDS. Findings also indicated that MSM who reported having anal intercourse while under the influence of alcohol or recreational drugs were significantly more likely to report UAI in the past year (85%) than men who reported having anal intercourse but never under the influence (76%). Because analyses were not conducted separately for older and younger MSM, findings were unable to provide strong support for the association of substance use to risky sexual behavior specifically among older MSM. However, overall findings support this association for MSM in general and indicate that UAI may be a more likely occurrence for younger MSM [7].
A final study by Jimenez [20] also used a situational design, examining the role of minority race status and sexual orientation in relation to risky sexual behaviors among MSM over the age of 50. The author hypothesized that a minority status in these three areas would contribute to a higher degree of marginalization, and, in turn, more risky behavior. Black and Latino MSM (N = 110) over the age of 50 completed self-report questionnaires assessing sexual risk behaviors, drug use, and the HIV-related topics of stigma and risk perception. Of the sexually active participants (90% of the sample), 20% reported engaging in unprotected receptive anal intercourse with a male partner in the past 3 months. In terms of the association between substance use and risky sexual behavior, a significant proportion of participants reported using alcohol (84%), marijuana (59%), poppers/nitrates (23%), crack (20%), and heroin (20%) “just before or during sex” over the past 6 months [20, pp. S223]. However, the risk level associated with sexual activity while using drugs was not assessed, as participants were not asked to distinguish between protected and unprotected sexual intercourse, casual versus regular partners, or specify the serostatus of their sexual partners. Though the participants in this study reported a variety of HIV risk behaviors, 74% believed that they had no chance or a low chance of contracting HIV. In addition, although 95% of MSM in this study knew of an HIV-related community agency, only 54% of the participants ever utilized these services. The results of this study have important implications for older minority MSM. Indeed, their “perception of invulnerability,” combined with their high rate of risk behaviors and lack of HIV-related healthcare utilization may put them at more of a risk than other subgroups of MSM.
Substance Use and Sexual Risk Behavior Among Older MSM: Event-level Studies
Two studies examined substance use in relation to risky sexual behaviors among MSM at the event level, with one concentrating on drug use, and the other on alcohol. The first study by Ober, Shoptaw, Wang, Gorbach, and Weiss [30] investigated factors associated with event-level stimulant (crack and methamphetamine) use during sex to examine the role of drugs in the spread of HIV from high-risk individuals to the general population. Event-level assessment required participants (N = 779 MSM) to recall specific instances of sexual activity with their three most recent partners and report (using ACASI assessment) whether they used drugs in those instances and if sex was unprotected.
Findings indicated that both racial status and age were related to substance use patterns and varying sexual risk behaviors. First, participants who reported crack use during sex (33%) were mostly Black (80%), and participants who reported meth use during sex (22%) were mostly White or Hispanic (74%). Additionally, a subset of participants who used drugs during sex was over the age of 50, such that of those participants who reported using meth during sex, 14% were age 50+, and of those who reported using crack during sex, 21% were age 50+. Bivariate analyses indicated that older age was differentially associated with sexual risk behavior, as a function of the type of drug used. For example, while MSM under 30 had higher odds of meth use during sex than MSM age 40+, MSM in age groups older than 30 had higher odds of crack use during sex than MSM younger than 30. This finding is consistent with that of the multivariate analysis, which showed that older MSM were more likely to use crack and younger MSM were more likely to use meth during sex. Additional analyses suggested that men who had partners of unknown HIV status or HIV-positive partners had higher odds of using meth during sex, a behavior associated with increased likelihood of engaging in unprotected sex. In contrast, crack use was found to occur more often when the partner was believed to be HIV-negative.
Overall, findings from this study indicate that meth users seem to be at a higher risk for contracting HIV than crack users [30]. Indeed, meth use during sex was associated with unprotected sex (when partner HIV status was unknown or positive), having a high number of sexual partners, and being HIV-positive. Because most of the participants who reported meth use were 30 years of age or younger, one possible interpretation of these findings is that younger MSM are at a higher risk than older MSM. However, 14% of meth users were over 50 years old, indicating that a significant subset of older MSM engage in substance-related, sexual risk taking similar to their younger counterparts [30]. In addition, a larger percentage of older MSM reported crack use as compared to younger MSM, a behavior found to be associated with exchanging sex for drugs or money [30].
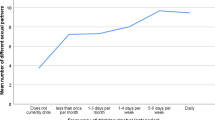
In a study by Mustanski [14], the association of substance use and risky sex was examined among MSM across a wide age range. This online daily diary study examined age and partner type as mediators of the association between alcohol use and risky sex for a period of 30 days. Eligible participants (HIV-negative MSM; N = 143) provided daily reports of number of drinks consumed, number of sexual partners, and specific sexual behaviors with each partner. Composite risk-related variables were created and analyses were conducted using multilevel modeling in order to assess both between and within participant differences in these behavioral outcome variables. Findings strongly and repeatedly supported the association between alcohol use and risky sex, with additional analyses demonstrating the importance of age as a moderator of this relationship. First, no significant age effect was found in regard to alcohol consumption and likelihood of having a sex partner, such that the odds of having a sex partner increase by 18% per drink consumed regardless of age. Similarly, no significant differences were noted between age groups in regards to alcohol consumption and engagement in sexual risk behaviors such as UAI. However, the association between alcohol consumption and sexual risk taking was found to be stronger for older participants (75th percentile, ~37 years old) than for younger participants (25th percentile, ~20 years old). Put simply, when older MSM drank and engaged in sexual activities, they were more likely than their younger counterparts to engage in activities with a high level of risk (as per the composite risk variable). This same effect was seen when more specifically examining the odds of engaging in UAI versus safe sex, such that older participants who consumed alcohol were more likely than younger participants to engage in UAI.
The findings of this study suggest that older MSM, when drinking alcohol, may be more prone to engaging in risky sexual behavior relative to younger MSM. This contradicts previous studies investigating the effects of alcohol in a heterosexual sample, which concluded that alcohol use has a larger effect on risky sexual behavior in younger samples [31]. Authors suggest several hypotheses for the difference in age-related risk among heterosexual versus MSM populations, including the presence of varying cultural/environmental norms regarding alcohol use, sexuality, and age, as well as the potential impact of “AIDS burnout” among older MSM. However, more research is required in order to fully examine the nature of these possible differences.
Methodological Critique
In reviewing the small body of literature examining the relationship between alcohol and substance use and risky sexual behaviors among MSM over the age of 50, several reoccurring methodological limitations are apparent. To begin, because most of the reviewed studies followed a cross-sectional design, cohort and historical effects as an explanation of age-related outcomes never can be ruled out. Although three longitudinal studies were included in the review, their reported findings typically pertained to one or two specific points of assessment, thus making it difficult to clearly distinguish possible cohort and historical effects from age-related effects. All other critiques and interpretations of the data to follow must be viewed in this limiting context.
Major limitations of the reviewed literature were found to pertain to the (1) operationalization of sexual risk behavior; (2) assessment of alcohol and other drug use; (3) use of self-report assessment methods; (4) inconsistent definition of “younger” versus “older” MSM; and (5) paucity of event level studies of sexual and substance use risk behaviors. In first focusing on risk assessment problems, several studies operationalized sexual risk behavior in ways that were limited in scope, thereby preventing a richer explanation of the relationship between substance use and subsequent experiences of risky sexual behavior. Indeed, in Dufour et al. [25], risky sexual behavior was defined solely as unprotected anal intercourse with a casual partner. Similarly, in Ostrow et al. [9] and Plankey [10] sexual risk was predominately operationalized as number of UAI partners, with a slight improvement by including HIV serostatus (verified by testing) as a risk outcome variable. In Jimenez [20], participants were asked to report experiences in which they used alcohol or other drugs just before or during sex, but they were not asked to distinguish between protected and unprotected sexual intercourse, casual versus regular partners, or to specify the serostatus of their sexual partners. As such, the actual risk level associated with sexual activity while using alcohol or other drugs was not assessed at a high degree of specificity.
There also were limitations in the assessment of alcohol and other drug use. First, only four of the studies considered the importance of quantity of substance use, with Dolcini et al. [8] asking participants to report their frequency of substance use and Ostrow et al. [9], Plankey [10], and Mustanski [14] requiring participants to report the number of alcoholic beverages consumed each day. All other reviewed studies failed to assess for the quantity of the substances ingested, focusing only on whether the use of a substance occurred (e.g. Did you use meth in the past 6 months? Before sex?). Though exact assessments of the quantity of some illicit drugs may be difficult to ascertain based on drug quality and variability in the systems of measurement, the argument can be made that some level of distinction between a “high use” incident and a “low use” incident is warranted to better define the circumstances in which alcohol and substance use might alter the likelihood of risky sexual behavior. Secondly, it would be beneficial if future studies examined a wide range of drugs, rather than limiting the scope to one drug in particular, as done in several of the reviewed studies [29, 30]. As the frequency and type of drug used have been found to differ between age groups in MSM [29, 30], this would allow researchers to determine whether use of a specific drug is associated with the likelihood of risky sexual behavior with respect to a certain age group, and to compare such data across drug type. Studies by Plankey et al. [10] and Ostrow [9] have begun to examine a wide range of substances in addition to drug combinations in relation to sexual risk behavior, and future studies would benefit by building upon their foundation. In sum, for most of the reviewed studies, broadening the range and specificity of the risk behaviors assessed likely would have added to the understanding of the connection between substance use and risky sexual behavior.
A third measurement problem noted in four of the reviewed studies [7, 8, 20, 25] pertains to their use of self-report assessment methods that have not been found to encourage the accurate reporting of sensitive information such as drug use and sexual behavior. Specifically, studies tended to rely on paper and pencil questionnaires and/or face-to-face interviews to assess sexual behavior and substance use, rather than use computerized versions of assessment measures that have been found to result in greater perceptions of privacy and subsequently to increase the accuracy of reporting [32]. As such, participants from Darrow et al. [7], Dolcini et al. [8], Dufour et al. [25], and Jimenez [20] may have been more prone to underreport risk behaviors due to social desirability biases, as compared to participants from the other reviewed studies that used ACASI strategies to assess risk behaviors [8, 9, 30]. In addition, only three studies relied on non-self-report strategies to assess for engagement in sexual risk behavior, with Dolcini et al. [8], Ostrow et al.[9], and Plankey et al. [10] incorporating biomedical sample testing to strengthen their study designs. These studies used HIV seroconversion (as verified by testing) as a risk outcome variable in addition to standard assessment procedures, and in doing so, were able to bypass the limitations associated with solely using self-reports including response bias and recall difficulties.
A final measurement problem noted in the reviewed studies pertains to the inconsistent definition of “younger” versus “older” MSM. Although four of the nine studies [8, 20, 29, 30] categorized “older MSM” as those persons 50 and older (similar to CDC distinctions), a large portion of the remaining studies used age intervals that may not capture the experience of men above the age of 50. For example, in Dufour et al. [25], participants 30 years of age and those who were 60 were assigned to the same “older MSM” age category. In Darrow et al. [7] 35 years of age was used as the cutoff. Similarly, in Mustanski [14], participants classified in the youngest quartile of age (~20 years old), were only 17 years younger than those in the 75th quartile (~37 years old), resulting in the classification of persons still in their thirties as “older.” Such inconsistencies in operationalization make it difficult to interpret age-related differences that are reported.
In focusing on study design, another limitation of the literature pertains to the paucity of event level studies of sexual and substance use risk behaviors. Only two of the nine studies [14, 30] examined the relationship of risky sexual behavior and substance use at the event level of specificity, and, of those two, only one was a diary study [14]. The use of daily diary assessment strategies has been considered a “gold standard” in assessing sexual risk and substance use behaviors not only because it addresses the question of social desirability threats by offering extensive privacy in reporting sensitive information, but because it also decreases the chance of recall error and other memory-based concerns. Progress in the field would be advanced considerably if more studies used this assessment strategy. An additional design-based limitation of this small body of literature is the lack of experimental tests of the link between substance use and sexually risky behavior. Although the reviewed event level studies [14, 30] were able to more clearly establish a temporal link between substance use and sexual risk behaviors, causal inferences cannot be drawn from such data.
Conclusions and Future Directions
Each of the reviewed studies represents an effort to explore the association between substance use and risky sex behaviors in older men who have sex with men. Across all studies, findings demonstrated that older MSM are indeed engaging in risky sexual behavior, with the likelihood of engaging in risky sexual activities increasing with the use of alcohol and other drugs. Initial findings also suggest that alcohol and substance use may contribute to higher rates of seroconversion among older MSM. However, although the data suggest that there is an association between substance use and risky sexual behaviors among older MSM, much remains unanswered. In particular, cumulative findings of the reviewed studies offer little clarity with regards to the extent to which older age is associated with increased or decreased sexual risk and alcohol/substance use as compared to younger MSM. Whereas three of the four global level studies [9, 10, 29] provide evidence to support increased sexual and substance-related risk among younger MSM, several situational and event level studies report contrasting findings. The strongest evidence supporting increased risk for older MSM comes from Mustanski [14], whose findings indicated that when older MSM drank and engaged in sexual activities, they were more likely to engage in activities with a high level of risk as compared to younger MSM. Findings from this study demonstrate the importance of specificity in assessment when examining the impact of age on the relationship of alcohol use and risky sex among MSM.
As noted, differences in methodology, sampling, and definitions of “younger” versus “older” in this small body of literature make it difficult to draw strong conclusions regarding whether the sexual risk behaviors of older MSM are comparable to younger MSM, and the extent to which alcohol and drug use may differentially contribute to engagement in sexual risk-taking as a function of age. In order to fully assess the relationship among age, substance use, and risky sexual behavior in MSM, future studies should evaluate event level occurrences of a variety of drugs in conjunction with sex. Assessment strategies of future studies should meet or exceed standards set by Mustanski [14] by using an event level design to address concerns related to privacy and social desirability threat, as well as decrease the chance of recall error. Through the use of event level designs and experimental designs (the latter presently absent in the literature), researchers would be able determine with more accuracy the age-specific correlates of substance use and risky sexual behavior among older and younger MSM, as well as the unique ways in which alcohol and substance use affects engagement in sexual risk behavior among MSM age 50 and older. Future research would also benefit from more longitudinal studies, which are capable of identifying correlates and mediators of substance use and sexual risk among MSM over time. Such studies would allow researchers to see the possibly changing influence alcohol and other substances have on the sexual risk behaviors of this population across the lifespan. In doing so, research may better inform the development of efficacious interventions to lower the risk of HIV infection among substance-using MSM by tailoring prevention efforts to meet the needs of men of varying ages. It is hoped that future research will lead to a more thorough understanding of the factors associated with behaviors that risk the health of MSM and inform the development of more effective prevention methods to reduce incidence of HIV and other sexually transmitted diseases.
References
CDC. Questions and answers: the 15% increase in HIV diagnoses from 2004 to 2007 in 34 states and general surveillance report questions [Internet]. 2009 [Cited 2010 Jan 15]. http://www.cdc.gov/hiv/topics/surveillance/resources/qa/surv_rep.htm.
CDC. Estimates of new HIV infections in the United States [Internet]. 2008 [Cited 2010 Jan 15]. http://www.cdc.gov/hiv/topics/surveillance/resources/factsheets/incidence.htm.
Dingle GA, Oei TPS. Is alcohol a cofactor of HIV and AIDS? Evidence from immunological and behavioral studies. Psychol Bull. 1997;122(1):56–71.
Steele CM, Josephs RA. Alcohol myopia: its prized and dangerous effects. Am Psychol. 1990;45(8):921–33.
Horvath P, Zuckerman M. Sensation seeking, risk appraisal, and risky behavior. Pers Individ Differ. 1993;14(1):41–52.
Woolf SE, Maisto SA. Alcohol use and risk of HIV infection among men who have sex with men. AIDS Behav. 2009;13(4):757–82.
Darrow WW, Biersteker S, Geiss T, et al. Risky sexual behaviors associated with recreational drug use among men who have sex with men in an international resort area: challenges and opportunities. J Urban Health. 2005;82:601–9.
Dolcini MM, Catania JA, Stall RD, Pollack L. The HIV epidemic among older men who have sex with men. J AIDS. 2003;33:S115–21.
Ostrow DG, Plankey MW, Cox C, et al. Specific sex drug combinations contribute to the majority of recent HIV seroconversions among msm in the MACS. J AIDS. 2009;51:349–55.
Plankey MW, Ostrow DG, Stall R, et al. The relationship between methamphetamine and popper use and risk of HIV seroconversion in the multicenter AIDS cohort study. J AIDS. 2007;45:85–92.
Global HIV Prevention Working Group. Behavior change and HIV prevention: (re)considerations for the 21st century [Internet]. 2008 [Cited 2010 Jan 15]. http://www.globalhivprevention.org/pdfs/PWG_behavior%20report_FINAL.pdf.
McAuliffe TL, Kelly JA, Sikkema KJ, et al. Sexual HIV risk behavior levels among young and older gay men outside of AIDS epicenters: findings of a 16-city sample. AIDS Behav. 1999;3(2):111–9.
Stall R, Barrett D, Bye L, et al. A comparison of younger and older gay men’s HIV risk taking behavior: the communication technologies 1989 cross sectional survey. J AIDS. 1992;5:682–7.
Mustanski B. Moderating effects of age on the alcohol and sexual risk taking association: an online daily diary study of men who have sex with men. AIDS Behav. 2008;12(1):118–26.
Vincke J, Bolton R, Miller M. Younger versus older gay men: risks, pleasures and dangers of anal sex. AIDS Care. 1997;9(2):217–25.
Chen SY, Weide D, McFarland W. Are the recent increases in sexual risk behavior among older or younger men who have sex with men? Answer: both. AIDS. 2003;17(6):942–3.
Crepaz N, Marks G, Mansergh G, Murphy S, Miller LC, Appleby PR. Age-related risk for HIV infection in men who have sex with men: examination of behavioral, relationship, and serostatus variables. AIDS Educ Prev. 2000;12(5):405–15.
Anderson G. HIV prevention and older people. SEICUS Rep. 1994;23(2):18–20.
Harry J. Sampling gay men. J Sex Res. 1986;22(1):21–34.
Jimenez AD. Triple jeopardy: targeting older men of color who have sex with men. J AIDS. 2003;33(Suppl. 2):S222–5.
Berger RM, Kelly JJ. What are older gay men like? An impossible question? J Gay Lesbian Soc Serv. 2001;13(4):55–65.
CDC. HIV/AIDS Surveillance Report, vol. 19. Atlanta (GA): US Department of Health and Human Services; 2007.
Salomon EA, Mimiaga MJ, Husnik MJ, et al. Depressive symptoms, utilization of mental health care, substance use, and sexual risk among young men who have sex with men in EXPLORE: implications for age-specific interventions. AIDS Behav. 2009;13(4):811–21.
Murray J, Adam BD. Aging, sexuality, and HIV issues among older gay men. Can J Hum Sex. 2001;10(3/4):75–90.
Dufour A, Alary M, Otis J, et al. Correlates of risky behaviors among younger and older men having sexual relations with men in Montreal, Quebec, Canada. Omega study group. J AIDS. 2000;23:272–8.
Johnston S, de Wit JBF, Janssen M, Coutinho RA, van Griensven GJP. Do today’s young homosexual men practice safer sex than today’s older homosexual men did when they were young? An analysis of sexual behavior change across cohorts in Amsterdam. AIDS Behav. 1999;3(1):75–81.
Chaikelson JS, Arbuckle TY, Lapidus S, Gold DP. Measurement of lifetime alcohol consumption. J Stud Alcohol. 1994;55:133–40.
NIAAA. Five year strategic plan FY07-11: alcohol across the lifespan. US Department of Health and Human Services, National Institutes of Health [Internet]. 2007 [Cited 2010 June 15]. http://pubs.niaaa.nih.gov/publications/StrategicPlan/NIAAASTRATEGICPLAN.htm.
Klitzman RL, Greenberg JD, Pollack LM, Dolezal C. MDMA (‘ecstasy’) use, and its association with other high risk behaviors, mental health, and other factors among gay/bisexual men in New York City. Drug Alcohol Depend. 2002;66:115–25.
Ober A, Shoptaw S, Wang P, Gorbach P, Weiss RE. Factors associated with event-level stimulant use during sex in a sample of older, low-income men who have sex with men in Los Angeles. Drug Alcohol Depend. 2009;102(1–3):122–9.
Cooper ML. Alcohol use and risky sexual behavior among college students and youth: evaluating the evidence. J Stud Alcohol. 2002;14:101–17.
Schroder KE, Carey MP, Vanable PA. Methodological challenges in research on sexual risk behavior: II accuracy of self-reports. Ann Behav Med. 2003;26(2):104–23.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Heath, J., Lanoye, A. & Maisto, S.A. The Role of Alcohol and Substance Use in Risky Sexual Behavior Among Older Men Who Have Sex With Men: A Review and Critique of the Current Literature. AIDS Behav 16, 578–589 (2012). https://doi.org/10.1007/s10461-011-9921-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-011-9921-2