Abstract
Racial disparities in HIV/AIDS are well established and efforts to understand key factors that may explain these differences are needed. Recent evidence suggests that health literacy may contribute to disparities in health behaviors among African American HIV patients. One component of health literacy, numeracy, is emerging as an important skill for successful self management of medications. We therefore tested whether numeracy mediated the effects of race on medication management among HIV seropositive patients. Results showed that poor management of a simulated HIV medication regimen among African Americans and women was mediated by lower numeracy. Poor medication self-management may be a significant root cause for health disparities in African Americans with HIV/AIDS. Whether African American women may be at particular risk requires further study. Interventions to improve HIV medication self-management through addressing numeracy skills may help to narrow the gap in health disparities among African Americans with HIV/AIDS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The HIV/AIDS epidemic has had a devastating impact on the African–American community over the past 25 years. Today, African Americans become infected with and die from HIV/AIDS at a greater rate than any other racial/ethnic group in the United States. Of those diagnosed with AIDS between 1997 and 2004, African Americans had the smallest proportion of individuals still alive after 9 years, compared to all other racial/ethnic groups. Moreover, survival time after an AIDS diagnosis among African Americans is lower than among any racial or ethnic group. Although deaths among Whites with AIDS declined 19% between 2000 and 2004, deaths among African Americans with AIDS declined only 7% during this same period. The reasons for these disparities are not a product of race per se but rather are likely due to barriers experienced by many African Americans [1].
Medical diagnosis and care are essential for reducing morbidity and mortality in any community, and are of particular concern in the African American community living with HIV/AIDS. When a medical patient is also part of a marginalized group, there is a greater likelihood that his or her illness will be poorly controlled, leading to a greater risk of death [2]. As stated by the National Minority AIDS Council, “What marks poor communities of color more than any other set of characteristics is the degree to which the poverty of their residents creates and enforces marginalized social status….Scientific evidence supports the assertion that the overrepresentation of African Americans among those infected with and affected by HIV is linked to marginalized social status” (pp. 12) [2]. One consequence of such marginalization is often poor educational quality and poorer literacy. Sudore et al. [3] found that in an elderly sample, African Americans, individuals with less than a high school education, and people with low income had higher mortality and were much more likely than Whites to have low literacy. Their findings implied that African Americans with adequate literacy had similar mortality rates as Whites. Moreover, low literacy has been linked to poorer disease management, increased hospitalizations, and, in particular, has been related to poor adherence to antiretroviral medications for the treatment of AIDS [4, 5]. No clear consensus on whether African American HIV patients are poorer adherers than other racial/ethnic groups exists and may be largely due to differences in adherence measurement techniques and the existence of multiple comorbidities (e.g., depression, substance abuse) among study participants [6–8].
Osborn et al. [9], conducted the only known study to date to test whether disparities in adherence were a function of health literacy. Findings from this study, that assessed 4-day self-reported adherence to antiretroviral medications, showed that health literacy mediated the effects of race on medication adherence [9]. African American HIV patients were more likely to be classified as non-adherent in this study; however, when literacy was included in the model, the effect of race on HIV-medication adherence diminished to non-significance [9]. This study provides strong support for the argument that limited health literacy may be a possible explanatory link underlying poorer disease outcomes among African Americans with HIV/AIDS and provides a “jumping off point” for further investigation into the root causes of the relationship between health literacy and health disparities among African Americans with HIV/AIDS.
Successful adherence to medications not only relies on the frequency of medication-taking across time but also on accurate understanding and management of prescription instructions. This includes correct identification of pills, understanding the number of pills to be taken at each dose, the timing of doses, determination of missed doses, need for refills and comprehension of warnings and other ancillary instructions (e.g., “take on an empty stomach”) [10]. Earlier studies have shown that low health literacy is a risk factor for incorrect identification of medicines [11], misinterpretation of prescription drug labels [12], and inaccurate comprehension of drug warning labels [13, 14]. Our earlier preliminary study showed that reading literacy for health related information and numeracy, the ability to understand and use numbers in daily life [15], was significantly related to medication management capacity with numeracy having the most robust effect. This study further showed that low numeracy skills mediated the effects of gender on medication management and explained the finding that women had poorer medication management skills than men [16].
Numeracy skills are multifaceted and have been grouped into basic, computational, analytical, and statistical numeracy [17]. Health numeracy’s effects on health behaviors are less well known and have, until recently, been overshadowed by work on health literacy [17]. Early evidence in diabetes and anticoagulation control suggest that poor numeracy is a risk for poor health behaviors and outcomes related to management of these diseases [18, 19].
The goal of the present study is to extend our earlier study to test the effects of African American race on medication management, while simultaneously adjusting for the effects of gender and other relevant socioeconomic indicators, and whether numeracy may serve to mediate these effects. We will test the utility of a comprehensive model to explain potential disparities in medication management among HIV positive African American and non-African American men and women. We hypothesize that poorer medication management among African Americans will be explained by low numeracy. Findings from this study will help to identify possible root causes for poorer adherence to HIV medications that can lead to disparities in health outcomes for HIV positive African Americans.
Methods
Participants and Recruitment
A sample of HIV positive African American, Hispanic, and White, inner city dwelling, English- and Spanish-speaking, men and women who had been referred to the University of Miami/Jackson Memorial Hospital Infectious Diseases Clinic or the Miami-Dade County AIDS Drugs Assistance Program (ADAP) were enrolled. Participants were recruited through posted flyers and referral from clinic personnel. Interested participants were either screened in-person by the study recruiter or over the phone.
All participants were either taking antiretroviral therapy (ART) to treat HIV or were medically “in process” for initiating ART at the time of the study. A total of 507 individuals were screened for participation in the study and 207 met eligibility criteria. Study exclusion criteria included reporting any use of heroin, cocaine, or amphetamine in the last year or current alcohol consumption (2 or more drinks) 3 days per week or more (52%); having a history of a psychotic disorder and having head trauma with loss of consciousness for greater than 15 min (26%). Opportunistic infections that were grounds for exclusion include CNS infections such as toxoplasmosis and cytomegalovirus. The remaining non-enrolled individuals were not taking antiretroviral medications and were not scheduled to begin ART in the near future (7%), were lost to follow-up after screening (12%) or were uninterested in participating (3%).
Data and Procedure
Patients who were interested and eligible for the study were enrolled from December 2005 to August 2008. All patients arrived individually to study offices located on the University of Miami, Miller School of Medicine campus to complete a written informed consent form (available in Spanish and English and written at the 6th grade level) before completing an assessment that included demographic questions and measures of reading literacy, numeracy, and HIV medication management (described in detail below). All study materials were available in English and Spanish, and were read aloud to each participant. The estimated time to complete the assessment was 1½ to 2 h. Patients were compensated $50 upon completion of these instruments.
Measures
Demographic Information
Demographic information pertained to patient age, gender, annual income, years of diagnosed HIV, and race.
Numeracy
The Applied Problems subtest of the Woodcock Johnson-III measures quantitative reasoning, math achievement and math knowledge [20]. The Woodcock Johnson-III is a well-known achievement test that has been validated in ethnic minorities and in persons ages 2–90+ years [20]. Low performance on this measure is a function of limited math skills, comprehension difficulties or poor mathematical reasoning abilities. The test has 65 items, but typically not all items are administered. Basal starting levels are based on the respondent’s estimated achievement level as per the guidelines of the test. For example, those estimated to have achieved the level of grade 10 begin with item 35. The basal criterion is met when the individual responds correctly to the six lowest numbered items administered or when Item 1 has been administered. If the basal is not obtained, then the test is administered backward until it is obtained. The ceiling criterion for the test (or the discontinuation of the test) is met when the subject responds incorrectly to the last six consecutively administered items or when the final item is administered. Raw scores on the applied problems test were converted to z-scores with a mean of 0 and a SD of ±1 (based on the test’s published, normative data). The z-score served as a continuous variable in analyses.
Health Literacy
The reading comprehension subtest of the Test of Functional Health Literacy (TOFHLA) [21] was used to measure reading literacy. This test consists of 50 items that assess text comprehension using the modified cloze procedure [22]. Every fifth to seventh word in a health-oriented text passage is omitted and the reader selects the appropriate word from a list of four possible choices. The passages were selected from instructions for an upper gastrointestinal series, the patient rights and responsibilities section of the Medicaid application form and a standard hospital informed consent form. Scores range from 0 to 50 and the percent correct was calculated. Although a short version of the test is available (36 items) the test developers recommend use of the full version in research studies.
Medication Management
Ability to manage ART medication instructions was assessed using the Medication Management Test (MMT) [23]. The test was developed in response to provider’s seeming lack of awareness of the cognitive basis for patients’ inability to adhere to HIV regimens and in order to identify “…mistakes in dispensing prescriptions and [assess] how well patients can calculate when a new prescription is needed, determine if pills have been missed over the prior week, and identify which medicines need to be taken with food or might make one drowsy” (pp. 122) [23]. In the test development and validation study, the measure was found to be reliable (Chronbach’s alpha = .82) and persons with test scores <60% correct were found to have significantly poorer medication adherence [23].
The test consists of eight items with a total of 16 points. There are five “mock” HIV medications with labels (created for the test) based on typical ART medications and dosing schedules (e.g., zidovudine, lamivudine, and saquinavir; over-the-counter medications such as acetaminophin and vitamins were used in place of actual antiretroviral medications). An example of a medication label is “Take one tablet two times a day – Medication B 150 mg tablet 30 tablets”. Another is “Take two tablets three times a day”. The MMT also has a medication insert for Loperamide, an anti-diarrheal, which contains indications, contraindications, dosing instructions side effects, and warnings.
The test score is then based on answers to questions about the medication labels, the Loperamide insert, and the ability to correctly count out and place a week’s supply of pills in a medication organizer and to determine missed doses and refills. Example questions include “The next few questions are about Medication A. Assume that when you started taking Medication A, you had a seven day supply and that you’ve been taking the medication for three days now. In other words, you should have taken the medication as prescribed for the last three days. Now show me what you would do to determine if you’ve missed any pills so far” and “For medication B, how many days will a new prescription last?” and “Please answer the following questions based on this package insert information for a common diarrhea medication. If you were suddenly experiencing diarrhea and began taking this medication, what’s the maximum number of capsules you should take over a two-day period?” The total percent correct was used in analyses.
Statistical Analyses
Structural equation models (SEM) specifying the relationships between variables were estimated using AMOS, version 17. Advantages of this procedure include the generality and flexibility of model specification and the ability to assess fit of the hypothesized model to the observed data.
Model fit using maximum likelihood estimation can be evaluated through use of the Chi-square (χ2) goodness of fit statistic. A significant χ2 relative to the degrees of freedom indicates the observed and estimated matrices differ. A nonsignificant χ2 value indicates that the two matrices are not statistically different, and the data fit the model. Because sample size may unpredictably influence the evaluation of the fit of the model to the observed data, supplemental indicators of model fit, such as the comparative fit index (CFI) and root mean error of approximation (RMSEA) were also applied [24]. CFI values that exceed 0.90 and RMSEA values below 0.06, and a confidence interval range from 0.00 to 0.08 indicate acceptable model fit [24]. The CFI and the RMSEA are both sensitive to model misspecification and are minimally affected by sample size [24]. Hypotheses regarding the specific structural relations of the constructs in the model were also evaluated through inspection of the direction and magnitude of the path coefficients.
Two structural equation models were estimated with a correlation matrix generated by 207 cases; a sample size considered to be of adequate power to detect small-medium effects [25, 26]. Model 1 tested whether race predicted lower medication management scores after controlling for age, gender, annual income, and number of years of diagnosed HIV. Model 2 tested whether African American race predicted lower numeracy scores; and whether numeracy scores, in turn, predicted lower medication management scores.
Results
Participant Characteristics
A total of 207 participants were enrolled in the study. Table 1 details the demographic characteristics by race (African American vs. non-African American). On average, participants reported taking 4.5 different medications per day (including prophylactics and vitamins in addition to antiretroviral medications) with a total of nearly seven pills per day on average. Participants reported taking their current antiretroviral regimen an average of 3.25 years.
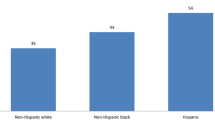
A significantly greater proportion of African American women (92%) than non-African American women (8%) completed the study, χ2(1) = 7.29, P < .001. No other demographic characteristics differed between the groups. African American participants had significantly lower scores on the MMT (t = 2.55, P = 0.01). No differences in health literacy (TOFHLA) were found between African American and non-African Americans; however, significant differences in numeracy (Applied Problems test) were found with African American participants scoring significantly lower than non-African American participants (t = 2.995, P = 0.003). African American participants’ scored more than one standard deviation below the test’s normative mean on average. We therefore chose to focus the present study analyses by testing only the numeracy measure as a mediator between race and medication management.
Test of Structural Models
Model 1 included five predictor variables: age, gender (male or female), annual income, years of diagnosed HIV, and race (African American or non-African American); and one outcome variable: HIV medication management. In this just identified model, female gender was associated with lower medication management scores (r = −0.16, P < 0.05). More years of diagnosed HIV was marginally associated with lower medication management scores (r = −0.13, P = 0.06) After controlling for gender and other potential covariates in the model, African American race was associated with lower medication management scores (r = −0.14, P < 0.05). Female gender and African American race accounted for 9% of the variability in this outcome (see Fig. 1).
In Model 2 (full model), numeracy (Applied Problems test) was introduced into the model as a potential mediator (or explanatory factor) in the pathway from female gender to medication management, and African American race, to medication management. As indicated in Fig. 2, the estimated model demonstrated excellent data fit, χ2 (3, N = 207) = 2.70, P = 0.44, CFI = 1.00, RMSEA = 0.00 (90% CI: 0.00–0.11). Female gender predicted lower numeracy scores (r = −0.32, P < 0.001), and African American race predicted lower numeracy scores (r = −0.18, P < 0.01). Female gender and African American race explained 15% of the variability in numeracy scores. The inclusion of numeracy in Model 2 reduced the association between African American race and poor medication management to non-significance. Numeracy also mediated the effect of female gender on poor medication management. Numeracy scores were significantly related to medication management (r = 0.67, P < 0.001), as was fewer years of diagnosed HIV (r = −0.11, P < 0.05). Both numeracy and years of diagnosis explained 45% of the variability in the medication management score.
Model 2 (full version): numeracy mediates the relationship between female gender, African American race and medication management. Coefficients are standardized path coefficients. Overall model fit, χ2(3, N = 207) = 2.70, P = 0.44, CFI = 1.00, RMSEA = 0.00 (90% CI: 0.00–0.11). For tests of significance of individual paths, * P < 0.05, ** P < 0.01, and *** P < 0.001
Discussion
Understanding the reason for pervasive health disparities across race and ethnicity is a major research, practice, and policy goal in the US [27]. To provide new insights into the pathways that lead to health disparities, we examined whether numeracy skills explain racial disparities in the management of HIV medications. Consistent with our predictions, African American race was initially related to poor medication management, but when numeracy skills were accounted for, the effect of race was reduced to non-significance. Likewise, as in our earlier study, the finding that women’s lower medication management scores were mediated by numeracy skill was further supported here. Based on our findings of patient’s “theoretical” understanding of medication management, these results suggest that HIV positive African Americans and women with deficient numeracy may be at particular risk for poor management of their personal prescriptions. Medication non-adherence, measured as the frequency of taking one’s medicines, has not been clearly associated with either race or gender in previous studies [6–8]. By focusing on the accuracy of understanding and following prescription instructions rather than medication-taking frequency, the present study highlights an important component of medication adherence previously uninvestigated as a potential cause of health disparities in HIV.
In prior work, limited literacy skills explained the association between African American race and poor HIV medication adherence [27]. The present study adds to that knowledge by highlighting the importance of numeracy skills in relation to medication management. While the role of numeracy skills in predicting health behaviors and explaining disparities is novel in the HIV literature, it is consistent with studies in other chronic disease contexts. Specifically, Osborn et al. recently showed that African American race predicted poor glycemic control, and numeracy skills explained this relationship [28]. Limited numeracy skills have also been linked to compromised disease management practices [15, 18], including poor adherence to self-care recommendations and lower disease management self-efficacy [18].
While numeracy appears to be an important component to medication management, clearly other factors contribute to one’s capacity to manage medications. In our study, the longer one had been diagnosed with HIV, the more problems one had with the medication management task on average. The precise relation between disease duration and medication management is unclear and does not support an “intuitive” assumption that those who have been diagnosed longer, and presumably have been taking medications longer, would be more skilled at managing those medicines. Whether disease duration may serve as a proxy representing HIV disease related cognitive decline (e.g., slowed information processing) associated with HIV infection remains to be tested [29–32]. Others [11] found general cognitive status in the elderly to be related to understanding prescription instructions and in HIV, problem solving and other neurocognitive processing capacities have been associated with this outcome [33]. These findings at a minimum suggest that living with HIV longer may not necessarily lead to better medication management supporting the findings of others that health behaviors may diminish over time with chronic illness [34].
There are limitations in our study that should be acknowledged. First, although structural equation modeling proposes a causal relationship between variables, the current study measured all variables cross-sectionally and, thus, can most appropriately speak to associations between variables observed at a single point in time, not causality. Future research is needed to investigate the longitudinal effects of these variables on changes in medication management over time, and to relate numeracy and poor medication management to subsequent adherence and disease progression. Second, a general health numeracy assessment tool that is comparable to health literacy instruments is currently unavailable. The measure used to assess numeracy in this study has not been applied in such a context previously and so requires further validation. Thirdly, this study used a simulated medication regimen rather than patients’ actual prescriptions. Further study is needed to determine the validity of these findings with patients’ actual prescriptions and whether other factors within the broader social context may confer additional risk or protection against poor management of HIV medications among African Americans. The link between the MMT and subsequent medication adherence [23] suggests that our findings may be replicable with individual personal medications.
Finally, it should be noted that the present study was not designed to detect effects by race and gender interactively but rather to test whether race and gender considered together in a model were each related to medication management skill. Our sample consisted of a relatively small number of non-African Americans (16%). Thus, generalizing these findings to a larger population would be erroneous. These findings require replication in larger representative samples of African American and non-African American HIV positive individuals to separate out the unique effects of race and gender.
Limited numeracy skills present a wide-reaching barrier to successful disease management that is potentially modifiable. The development of educational programs and adaptive tools designed to facilitate effective patient-provider communication and accommodate patients with limited numeracy skills could potentially be a useful approach to improving patients’ ability to self manage their medication. In addition, these improvements may help decrease subsequent medication non-adherence and, ultimately, also contribute to reducing racial disparities in disease progression and related mortality [1]. Future research should explore the role of numeracy-focused interventions to reduce racial differences in medication-taking and, potentially, other relevant health behaviors.
References
CDC. HIV/AIDS surveillance report, Vol. 17, Rev. ed. US Department of Health and Human Services; 2007.
Fullilove RE. African Americans, health disparities and HIV/AIDS—recommendations for confronting the epidemic in Black America. Washington, DC: National Minority AIDS Council; 2006.
Sudore RL, Yaffe K, Satterfield S, et al. Limited literacy and mortality in the elderly: the health, aging, and body composition study. J Gen Intern Med. 2006;21(8):806–12.
Kalichman SC, Benotsch E, Suarez T, et al. Health literacy and health-related knowledge among persons living with HIV/AIDS. Am J Prev Med. 2000;18(4):325–31.
Kalichman SC, Rompa D. Functional health literacy is associated with health status and health-related knowledge in people living with HIV-AIDS. J Acquir Immune Defic Syndr. 2000;25(4):337–44.
Arnsten JH, Demas PA, Grant RW, et al. Impact of active drug use on antiretroviral therapy adherence and viral suppression in HIV-infected drug users. J Gen Intern Med. 2002;17(5):377–81.
Miller LG, Liu H, Hays RD, et al. Knowledge of antiretroviral regimen dosing and adherence: a longitudinal study. Clin Infect Dis. 2003;36(4):514–8.
Stone VE, Hogan JW, Schuman P, et al. Antiretroviral regimen complexity, self-reported adherence, and HIV patients’ understanding of their regimens: survey of women in the her study. J Acquir Immune Defic Syndr. 2001;28(2):124–31.
Osborn CY, Paasche-Orlow MK, Davis TC, Wolf MS. Health literacy: an overlooked factor in understanding HIV health disparities. Am J Prev Med. 2007;33(5):374–8.
MacLaughlin EJ, Raehl CL, Treadway AK, et al. Assessing medication adherence in the elderly: which tools to use in clinical practice? Drugs Aging. 2005;22(3):231–55.
Kripalani S, Henderson LE, Chiu EY, et al. Predictors of medication self-management skill in a low-literacy population. J Gen Intern Med. 2006;21(8):852–6.
Wolf MS, Davis TC, Shrank W, et al. To err is human: patient misinterpretations of prescription drug label instructions. Patient Educ Couns. 2007;67(3):293–300.
Davis TC, Wolf MS, Bass PFIII, et al. Low literacy impairs comprehension of prescription drug warning labels. J Gen Intern Med. 2006;21(8):847–51.
Davis TC, Wolf MS, Bass PFIII, et al. Literacy and misunderstanding prescription drug labels. Ann Intern Med. 2006;145(12):887–94.
Rothman RL, Housam R, Weiss H, et al. Patient understanding of food labels: the role of literacy and numeracy. Am J Prev Med. 2006;31(5):391–8.
Waldrop-Valverde D, Jones DL, Jayaweera D, et al. Gender differences in medication management capacity in HIV infection: the role of health literacy and numeracy. AIDS Behav. 2009;13(1):46–52.
Golbeck AL, Ahlers-Schmidt CR, Paschal AM, Dismuke SE. A definition and operational framework for health numeracy. Am J Prev Med. 2005;29(4):375–6.
Cavanaugh K, Huizinga MM, Wallston KA, et al. Association of numeracy and diabetes control. Ann Intern Med. 2008;148(10):737–46.
Estrada CA, Martin-Hryniewicz M, Peek BT, Collins C, Byrd JC. Literacy and numeracy skills and anticoagulation control. Am J Med Sci. 2004;328(2):88–93.
Woodcock R, McGrew K, Mather N. Woodcock Johnson III tests of achievement. Itasca, IL: Riverside; 2001.
Parker RM, Baker DW, Williams MV, Nurss JR. The test of functional health literacy in adults: a new instrument for measuring patients’ literacy skills. J Gen Intern Med. 1995;10(10):537–41.
Taylor WS. Cloze procedure: a new test for measuring readability. Journal Q. 1953;38:632–7.
Albert SM, Weber CM, Todak G, et al. An observed performance test of medication management ability in HIV: relation to neuropsychological status and medication adherence outcomes. AIDS Behav. 1999;3(2):121–8.
Ridgon E. CFI versus RMSEA: comparison of two fit indexes for structural equations modeling. Struct Equ Model. 1996;3:369–79.
Kline R. Principles and practice of structural equation modeling. New York: Guilford; 2004.
Loehlin JC. Latent variable models: an introduction to factor, path, and structural analysis. Hillsdale, NJ: Lawrence Erlbaum; 1992.
IOM. Health literacy: a prescription to end confusion. Washington, DC; 2004.
Osborn CY, Cavanaugh K, Wallston KA, White RO, Rothman RL. Diabetes numeracy mediates the association between African American race and poor glycemic control. Diabetes Care. 2009, in press.
Grant I, Atkinson JH, Hesselink JR, et al. Evidence for early central nervous system involvement in the acquired immunodeficiency syndrome (AIDS) and other human immunodeficiency virus (HIV) infections. Studies with neuropsychologic testing and magnetic resonance imaging. Ann Intern Med. 1987;107(6):828–36.
Martin EM, Robertson LC, Edelstein HE, et al. Performance of patients with early HIV-1 infection on the Stroop Task. J Clin Exp Neuropsychol. 1992;14(5):857–68.
Peavy G, Jacobs D, Salmon DP, et al. Verbal memory performance of patients with human immunodeficiency virus infection: evidence of subcortical dysfunction. The HNRC Group. J Clin Exp Neuropsychol. 1994;16(4):508–23.
Wilkie FL, Goodkin K, van Zuilen MH, et al. Cognitive effects of HIV-1 infection. CNS Spectr. 2000;5(5):33–51.
Waldrop-Valverde D, Rodriguez A, Ownby RL. Health literacy and medication management among HIV positive African Americans. NIH Summit: The Science of Eliminating Health Disparities. National Harbor, MD; 2008.
Chesney MA. Factors affecting adherence to antiretroviral therapy. Clin Infect Dis. 2000;30(Suppl 2):S171–6.
Acknowledgments
We would like to thank Raymond L. Ownby, M.D., Ph.D. for his invaluable guidance and suggestions on this manuscript. This study was supported by funding from the National Institute of Mental Health grant number MH74664 to the lead author, D. Waldrop-Valverde.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Waldrop-Valverde, D., Osborn, C.Y., Rodriguez, A. et al. Numeracy Skills Explain Racial Differences in HIV Medication Management. AIDS Behav 14, 799–806 (2010). https://doi.org/10.1007/s10461-009-9604-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-009-9604-4