Abstract
To assess the association between antiretroviral therapy (ART) and fertility history and desire among HIV-positive Ugandan women, we conducted a cross-sectional study among HIV-positive Ugandan women aged 18–50 years who attended an HIV clinic at Mbarara University in western Uganda between November 1, 2005 and June 6, 2006. Of 538 women approached, 501 were enrolled. ART use was associated with increased odds of fertility desire (AOR 2.99, 95% CI 1.38–6.28), and decreased odds of pregnancy (AOR 0.56, 95% CI 0.33–0.95) and live birth (AOR 0.30, 95% CI 0.13–0.66). ART was associated with an increase in fertility desire, but was not associated with an increase in fertility. Additional studies will be needed to determine if this greater fertility desire among ART-treated women leads to an increase in fertility as ART use expands.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Women of reproductive age comprise 46% of the world’s HIV-infected population (UNAIDS 2006). Although only 10% of the world’s population reside in sub-Saharan Africa, three-quarters of the women infected with HIV live in the region, where approximately 13.2 million women of child-bearing age are HIV-positive (UNAIDS 2006).
Uganda has the second highest total fertility rate in Africa at 7.1, and the fourth highest worldwide (WHO 2006a). However, Uganda’s total fertility rate among women (irrespective of HIV sero-status) has stabilized concurrent with the onset of endemic HIV (UN 1997, 2005). High HIV prevalence is associated with a reduction in fertility by 25–40% among HIV+ women (Zaba and Gregson 1998) in many countries in sub-Saharan Africa. In Uganda specifically, the combined effect of increased mortality among HIV-positive women and a reduction in fertility resulted in 700,000 fewer births between 1980 and 2000 (Lewis et al. 2004). This decline in births has been ascribed to increased fetal loss, reduced conception, and excess mortality among HIV-positive women of reproductive age (Gray et al. 1998; Ross et al. 2004; Zaba and Gregson 1998).
With donor support from the President’s Emergency Plan for AIDS Relief and Global Fund, no-cost combination anti-retroviral therapy (ART) has recently been introduced in Uganda and other resource-limited countries (UNAIDS 2006). Currently 51% of Ugandans with advanced HIV receive ART (WHO 2005). This has led to dramatic reductions in morbidity and mortality among those receiving treatment (Badri et al. 2006; Badri et al. 2002; Braitstein et al. 2006; Mermin et al. 2006). It is unknown, however, whether increased access to ART will reverse the observed HIV-related declines in fertility. One study of U.S. women found that conception rates among HIV+ women remained the same before and after initiation of ART (Massad et al. 2004). A second U.S. study found increased rates of pregnancy among women on HAART relative to women on other anti-retroviral therapy (Blair et al. 2004). Recent reports from Uganda and South Africa suggest that ART may be associated with an increase in unplanned pregnancies (Homsy et al. 2006; Mohohlo et al. 2006). Data on the effect of ART use or decreased viral load on sexual behavior are more extensive, although they have yielded conflicting results. Some studies have found an increase in unprotected sex and number of sex partners—factors that could lead to increased fertility—in association with ART use and viral load decrease (Dukers et al. 2001; Katz et al. 2002; Kelly et al. 1998; Miller et al. 2000; Scheer et al. 2001). Others, including two conducted in resource-limited settings (Cote d’Ivoire and Uganda), have not (Bateganya et al. 2005; Moatti et al. 2003; Wolf et al. 2003). Of note, a recent study in rural Uganda found that ART provision and counseling were associated with a reduction in risk behaviors (Bunnell et al. 2006). However no study to date has explicitly addressed whether access to ART is associated with changes in fertility desire and fertility outcomes. We therefore posed the question: has access to ART changed the fertility and fertility desires of HIV-positive Ugandan women?
We based our study on a conceptual framework proposed by Kaida that details the biological, behavioral, economic, and social factors that may mediate ART’s influence on fertility (Kaida et al. 2006). We hypothesized that ART use may increase fertility and fertility desires among HIV-positive women (compared with those not on therapy) through three mechanisms. First, with improved quality and length of life, women and their partners may anticipate living long enough to raise children, and thus desire more children. Second, improved health status may renew interest in sex, as well as strengthen a woman’s biological ability to conceive and carry a pregnancy to term. Finally, ART use may change a woman’s sexual behavior (increase in number of partners and engaging in unprotected sex), particularly if it changes a woman’s perception of her infectivity. Given the high fertility rate and HIV prevalence in Uganda, elucidating the association between ART and fertility may inform national demographic projections, social policy decisions, and HIV education and family planning programs.
Methods
Participants
Setting
Data was collected from a study conducted in the semi-urban town of Mbarara, southwestern Uganda at the Immune Suppression Syndrome (ISS) clinic at Mbarara University Hospital. Mbarara University Hospital is the largest public hospital in the region, serving patients from the town of Mbarara, as well as outlying rural areas. The ISS clinic is the hospital’s outpatient adult HIV/AIDS clinic. It is the primary source of no-cost HIV care and anti-retroviral medications in the region.
Study Description
We conducted a cross-sectional study of fertility desire, pregnancy history, and live birth history among HIV+ women (both ART-exposed and ART-naïve) attending the ISS clinic. To recruit the ART-naïve group, research staff approached every third woman in the queue waiting for medical services for potential participation in the study. Recruiters approached the next person in line when individuals either declined or were ineligible. To recruit the ART-exposed group, the pharmacy referred every female patient who was refilling ART medication to the research staff. Eligible women were 18–50 years of age, competent to give consent, and HIV-infected. (The Mbarara University IRB considers adults to be 18 years of age or older, and therefore younger participants were not recruited). We considered women ART-exposed if they had been taking ART continuously for nine or more months. We considered women ART-naïve if they had never taken ART, except for vertical transmission prophylaxis.
After determining eligibility and obtaining written informed consent, the research assistants administered a structured questionnaire in either English or Runyankole (the dominant regional language). The Runyankole questionnaire was translated from the original English version into Runyankole, and then a second translator back-translated the questionnaire into English to ensure consistency between the two languages. CD4 data were collected from medical records. The questionnaire was piloted among forty women. Approximately fifteen participants were interviewed daily over eight months from November 1, 2005–June 6, 2006. Interviews were always conducted in a private space, and were conducted by female nurses trained as research assistants. In the second half of recruitment, ART-naïve participants were over-sampled to achieve balanced ART-exposed and ART-naïve by sampling every sixth ART-exposed participant.
Measures
The primary explanatory variable was self-reported ART use and duration (including specific anti-retroviral agents, as well as the start and end date for each ART regimen). The primary outcomes were self-reported pregnancy and live birth history in the previous three years, including date and whether the pregnancy ended in live birth, stillbirth, induced abortion, or miscarriage. The secondary outcome was fertility desire. Fertility desire was defined by the question: “Are you planning to have (any more) children in the future?” Information collected on potential confounders included: sexual and reproductive history (i.e. age at menarche and sexual debut, number of lifetime pregnancies and live births, number of casual and regular sexual partners in the past three months, frequency of vaginal sex in the past three months, contraceptive use (including condoms, oral contraceptives, sterilization, injections, implants, cervical caps, and diaphragms) among those sexually active in the last three months, HIV status of sexual partners, and disclosure of HIV status to sexual partners), health status (WHO stage of disease (WHO 2006b), CD4 cell count, and years since HIV diagnosis), and socio-demographic factors (age, income, marital status, etc).
We reviewed medical records to confirm ART history, and to obtain clinical diagnoses of WHO stage of disease. The medical record was considered the referent measure for inconsistencies between self-reported and medical record data. Medical records were unavailable for pregnancy and birth history.
Data Analysis
Univariate analyses were performed to assess the relationship between ART use, other covariates of interest, and the primary outcomes: fertility desires and fertility history. Categorical variables are reported as counts and proportions, while continuous variables are reported as means with standard deviations (SD) or medians with interquartile range (IQR). Differences in fertility desire and fertility history between groups are reported using Pearson’s chi-squared test statistic (for categorical variables), Student’s independent t-test (for means), and Wilcoxon test (for medians). All statistical tests were two-sided and considered significant at α = 0.05. We used multiple imputation with ten imputations for missing data. Disclosure of HIV status to the participant’s spouse or sexual partner was imputed for 45 participants, discordance between the participant’s HIV status and that of her spouse or sexual partner was imputed for 43 participants, and CD4 cell count data was imputed for 155 participants.
ART Use and Fertility Desire
We compared fertility desire across groups (i.e. ART-exposed vs. ART-naïve HIV-positive women). Unadjusted odds ratios (OR) and 95% confidence intervals (95% CI) were computed to determine the magnitude of the association between independent variables and fertility desire.
Multivariate logistic regression was used to model the association between ART use and the likelihood of fertility desire, while controlling for covariates. A variable was included in the multivariable analysis if its P-value in bivariate analyses was equal to or less than 0.10. We then used backward elimination of variables not significant at alpha = 0.05 to obtain the final adjusted odds ratios (AOR). ART exposure was included in all multivariable analyses regardless of statistical significance as it was the main explanatory variable of interest. WHO stage of disease was also included in all multivariable analyses, as it was the main confounder of interest. We calculated goodness of fit and correlation matrices, and tested for collinearity in the fertility desire model.
ART Use and Fertility History
The relationship between concurrent ART use and the odds of pregnancy and live birth during the three years preceding the interview was examined with generalized estimating equations. The three-year period was retrospectively divided into six-month intervals, and data collected during the cross-sectional interviews (dates of pregnancy and live births, date of HIV diagnosis, ART duration, and other socio-demographic information) were used to retrospectively classify each six-month interval by HIV status and ART treatment status. Thus, a participant was considered ART-exposed during a six-month interval if she was taking ART at any time during that interval. Outcomes were measured for each interval, so that one participant could contribute multiple outcomes, depending on her fertility history. We used the resulting retrospective time intervals to estimate the overall odds of pregnancy and live birth by ART treatment status for the entire three-year period prior to the interview. A three-year period of analysis was used (rather than a lifetime analysis, for example) to highlight the period of potential ART exposure during a period of rapid scale-up. We calculated unstructured correlation matrices and tested for collinearity on the final models. A multivariate generalized estimating equations model was built using the methods described above for the fertility desire analyses.
Results
Recruitment
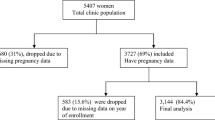
Five hundred thirty-eight women were approached, and of these thirty-seven ART-naïve women declined to participate in the study, yielding a sample of 501 participants. Of 501 participants, oversampling of ART-naïve individuals yielded 223 women (44.5%) taking ART and 278 (55.5%) not taking ART. Participants were excluded from the analyses if both self-reported and medical record data were unavailable.
Baseline Characteristics
Baseline characteristics of the sample are described in Table 1. The ART-exposed group was significantly more likely to be older (P < 0.01), be a member of the Kiga ethnic group (P < 0.01), have advanced education (P < 0.01), and have a higher income (P < 0.01) compared to the ART-naïve group. With regards to HIV/AIDS and health characteristics, the ART-exposed group was more likely to have ever had a WHO stage of 3–4 (P < 0.01), have a lower CD4 nadir (P < 0.01), have had a HIV diagnosis for a longer period of time (P < 0.01), have disclosed her serostatus to her partner if she was sexually active (P < 0.01), and to be concordant with her partner if sexually active (P < 0.01). With regards to sexual and reproductive health characteristics, the ART-exposed group was more likely to have used contraception in the last three months (P < 0.01), have used condoms in the last three months (P < 0.01), have been abstinent in the last three months (P < 0.01), and have been advised by a health care worker to avoid pregnancy (P < 0.01).
ART Use and Fertility Desire
In the bivariate analysis, ART use was not significantly associated with the desire to have more children in the future (OR 0.97, 95% CI 0.59–1.60). However, increased age (OR 0.25, 95% CI 0.16–0.39), being a widow (OR 0.13, 95% CI 0.04–0.39), increased WHO stage (OR 0.55, 95% CI 0.33–0.90), number of lifetime pregnancies (OR 0.38, 95% CI 0.20–0.69) and live births (OR 0.19, 95% CI 0.10–0.38), and number of children alive at one year (OR 0.21, 95% CI 0.11–0.43) were found to be associated with a significant decrease in the odds of fertility desire. Sexually active women (OR 3.03, 95% CI 1.78–5.15) and women who were discordant with their partners (OR 2.31, 95% CI 1.31–4.10) had a significantly increased odds of fertility desire. The remaining variables (ethnicity, education, age at sexual debut, religion, income, marital status, length of time with HIV diagnosis, CD4 cell count, health status, disclosure of sero-status, age at menarche, or advice by a health care worker to avoid pregnancy) fitted in the model had no significant association (Table 2).
In multivariate analysis, current ART use (OR 2.99, 95% CI 1.38–6.28) and being married (OR 1.94, 95% CI 1.06–3.53) were significantly associated with increased fertility desire. Increased age (OR 0.33, 95% CI 0.19–0.56), having ever been diagnosed with WHO stage 3–4 (OR 0.46, 95% CI 0.22–0.95), being widowed (OR 0.24, 95% CI 0.08–0.75), and having an increased number of live births (OR 0.35, 95% CI 0.16–0.74) were all significantly associated with a decreased odds of fertility desire (Table 2).
ART Use and Pregnancy in the Previous Three Years
In bivariate analyses, concurrent ART use (OR 0.38, 95% CI 0.22–0.64), increased age (OR 0.36, 95% CI 0.29–0.45), increased education (OR 0.59, 95% CI 0.39–0.89), being a widow (OR 0.46, 95% CI 0.24–0.87), WHO stage of 3–4 (OR 0.50, 95% CI 0.36–0.70), longer length of time since HIV diagnosis (OR 0.66, 95% CI 0.45–0.95), and increased number of children alive at one year of age (OR 0.64, 95% CI 0.43–0.94) were significantly associated with a reduced odds of pregnancy in the previous three years in the bivariable analyses, while being married (OR 2.31, 95% OR 1.56–3.43), being sero-discordant (OR 1.91, 95% CI 1.32–2.77), having a CD4 cell count >500 (OR 1.94, 95% CI 1.13–3.34), being sexually active in the past three months (OR 2.68, 95% CI 1.87–3.84), and contraceptive use in the past three months (OR 1.45, 95% CI 1.01–2.10) were all significantly associated with an increased odds of pregnancy. The remaining variables (religion, income, CD4 cell count ≤500, age at sexual debut and menarche, recent condom use, number of lifetime pregnancies and live births, self-assessed health status, disclosure of HIV status to partner, or concordance of HIV status with partner) fitted in the model had no significant associations (Table 3).
In the multivariate analyses, concurrent ART use (OR 0.56, 95% CI 0.33–0.95) and increased age (OR 0.41, 95% CI 0.31–0.54) were significantly associated with a reduced odds of pregnancy, while being married was significantly associated with an increased odds of pregnancy (OR 2.65, 95% CI 1.76–3.99). The remaining variables (being widowed, higher WHO stage) had no significant associations (Table 3).
ART Use and Live Birth in the Previous Three Years
Results from bivariate analyses showed that concurrent ART use (OR 0.19, 95% CI 0.08–0.43), increased age (OR 0.28, 95% CI 0.22–0.36), being widowed (OR 0.34, 95% CI 0.16–0.71), higher WHO stage (OR 0.52, 95% CI 0.35–0.77), increased time since HIV diagnosis (OR 0.62, 95% CI 0.41–0.93), and number of children alive at one year of age (OR 0.63, 95% CI 0.41–0.98) were significantly associated with decreased odds of live birth in the previous three years, whereas being married (OR 2.03, 95% CI 1.32–3.12), CD4 cell count 301–500 and >500 (OR 2.79, 95% CI 1.16–6.73, and OR 3.29, 95% CI 1.46–7.41, respectively), and being sexually active in the last 3 months (OR 2.13, 95% CI 1.45–3.15) were significantly associated with an increased odds of live birth. The remaining variables (education, ethnicity, religion, income, CD4 cell count of 151–300, self-assessed health status, disclosure, sero-concordance, age at sexual debut and menarche, recent contraceptive use, recent condom use, number of lifetime pregnancies and live births, whether a HCW advised the participant to avoid pregnancy, and disclosure of HIV status to one’s partner) had no significant associations (Table 4).
Multivariable analyses showed that concurrent ART use (OR 0.30, 95% CI 0.13–0.66) and increased age (OR 0.30, 95% CI 0.21–0.43) were significantly associated with decreased odds of live birth, whereas being married (OR 2.39, 95% CI 1.49–3.84) and increased age at sexual debut (OR 1.74, 95% CI 1.14–2.65) were significantly associated with an increased odds of live birth. Being widowed and WHO stage were not significantly associated with the odds of live birth.
Analysis Excluding Women Taking Efavirenz
Because a substantial minority of women in the ART-exposed group were currently taking efavirenz (which carries a Class D pregnancy rating), we repeated the above analyses while excluding women using regimens containing efavirenz, under the hypothesis that women taking efavirenz may have been more strongly cautioned against becoming pregnant. Of note, health educators at the ISS clinic strongly advise all HIV-positive women not to become pregnant, regardless of their antiretroviral treatment status or specific antiretroviral regimen. Seventy-two women in the ART-exposed group were currently taking efavirenz. When these women were excluded from the analysis, there was no significant change in the odds of fertility desire and birth (adjusted OR for fertility desire was 3.07, 95% CI 1.32–7.18; adjusted OR for live birth was 0.37, 95% CI 0.14–1.00). There was a moderate decrease in effect for pregnancy, but this was non-significant (adjusted OR 0.75, 95% CI 0.38–1.47). These results suggest that use of efavirenz does not account for the associations we found between ART use and fertility desire, pregnancy, or live birth.
Discussion
Concurrent ART use was found to be significantly associated with increased odds of planning to have children in the future in multivariate analysis. Experience elsewhere suggests that desire for children may increase with improved health on ART (Panozzo et al. 2003).
On the other hand, concurrent ART use was found to be significantly associated with decreased odds of pregnancy and live birth in the preceding three years in both bivariate and multivariate analyses. These data suggest that exposure to ART may increase the desire to have additional children, but has not yet increased the odds of pregnancy or live birth among HIV+ Ugandan women attending a HIV clinic in a rural resource-poor setting. The increased desire for HIV+ women to have children in the setting of expanding ART access highlights the importance of incorporating family planning and the prevention of mother-to-child transmission into HIV prevention and treatment programs.
Our observation that ART exposure was associated with a decreased odds of pregnancy and live birth contradicted our original hypothesis (and the results of studies conducted elsewhere (Blair et al. 2004)), but was not altogether surprising. The generalized HIV epidemic in Uganda has stretched the ability of families to care for HIV+ relatives. The recent introduction of ART may have not yet sufficiently improved overall health status to counter act the increased demands of living with HIV and reverse the impact of HIV on childbearing. It is also possible that study participants on ART have more contact with health professionals and health education (where they are counseled to avoid pregnancy), and that this health education is influencing reproductive decisions. Finally, improvements in functional health status may only have been recently realized in many of our participants, such that these improvements are associated with increased fertility desire, but have not yet actually increased fertility.
When interpreting our results, readers should be cautious of the following issues. While births are momentous life events that are easily remembered, we were unable to use medical records to confirm the reproductive histories provided by the participants and therefore cannot exclude differential recall bias of birth history by ART exposure status. However, there is little reason to believe that ART-exposed and ART-naïve women would differently report their fertility history. The total number of pregnancies was probably underreported, as early miscarriages were unlikely to have been recognized and abortion is illegal in Uganda. Because the impact of ART on miscarriage is unknown, it is difficult to fully exclude bias. In addition, while ART-treated women return to the outpatient HIV clinic every three months to refill their prescription, ART-naive individuals may attend the clinic only when ill and requiring treatment. Therefore, women in the ART-naïve arm could have more advanced disease than women in the ART-treated arm, and therefore less able to become pregnant or carry a pregnancy to term. However, the larger percentage of women in the ART-exposed group (relative to the ART-naïve) who had ever been assigned a WHO stage of 3–4 makes this possibility less likely. The generalizability of our results to HIV+ individuals not in medical care is limited, as our study recruited individuals attending an HIV clinic. Selection and survival bias may be a factor as well. While CD4 count and clinical WHO stage determine if a patient is placed on the waiting list for ART at the ISS clinic (at the time of the study, there was a three month wait), social factors influence how fast patients move up the waiting list. Therefore, patients in the ART-exposed group may have more extensive socioeconomic networks that are mediating fertility desire and decisions that could not be controlled for in the analyses. Future qualitative studies are needed to elucidate the socioeconomic factors that mediate how ART impacts fertility decisions. In addition, we were unable to measure how many of the ART-exposed women referred by the pharmacist to the research office actually presented to the research site. This might have introduced selection bias into the study, although the direction of the bias is difficult to predict.
Our results indicate that ART use may be associated with an increase in fertility desire among HIV+ women attending a HIV clinic in a rural resource-limited setting. This increase in fertility desire has not yet translated into an increase in pregnancies or live births. Rather, ART use may be associated with a substantial decrease in fertility among HIV+ Ugandan women. Further study will be necessary to estimate the impact of ART on future fertility patterns in resource-limited settings.
References
Badri, M., Lawn, S. D., & Wood, R. (2006). Short-term risk of AIDS or death in people infected with HIV-1 before antiretroviral therapy in South Africa: A longitudinal study. The Lancet, 368(9543), 1254–1259.
Badri, M., Wilson, D., & Wood, R. (2002). Effect of highly active antiretroviral therapy on incidence of tuberculosis in South Africa: A cohort study. The Lancet, 359(9323), 2059–2064.
Bateganya, M., Colfax, G., Shafer, L. A., Kityo, C., Mugyenyi, P., Serwadda, D., Mayanja, H., & Bangsberg, D. (2005). Antiretroviral therapy and sexual behavior: A comparative study between antiretroviral- naive and -experienced patients at an urban HIV/AIDS care and research center in Kampala, Uganda. AIDS Patient Care and STDS, 19(11), 760–768.
Blair, J. M., Hanson, D. L., Jones, J. L., & Dworkin, M. S. (2004). Trends in pregnancy rates among women with human immunodeficiency virus. Obstetrics and Gynecology, 103(4), 663–668.
Braitstein, P., Brinkhof, M. W., Dabis, F., Schechter, M., Boulle, A., Miotti, P., Wood, R., Laurent, C., Sprinz, E., Seyler, C., Bangsberg, D., Balestre, E., Sterne, J. A., May, M., & Egger, M. (2006). Mortality of HIV-1-infected patients in the first year of antiretroviral therapy: Comparison between low-income and high-income countries. The Lancet, 367(9513), 817–824.
Bunnell, R., Ekwaru, J. P., Solberg, P., Wamai, N., Bikaako-Kajura, W., Were, W., Coutinho, A., Liechty, C., Madraa, E., Rutherford, G., & Mermin, J. (2006). Changes in sexual behavior and risk of HIV transmission after antiretroviral therapy and prevention interventions in rural Uganda. AIDS, 20(1), 85–92.
Dukers, N. H., Goudsmit, J., de Wit, J. B., Prins, M., Weverling, G. J., & Coutinho, R. A. (2001). Sexual risk behaviour relates to the virological and immunological improvements during highly active antiretroviral therapy in HIV-1 infection. AIDS, 15(3), 369–378.
Gray, R. H., Wawer, M. J., Serwadda, D., Sewankambo, N., Li, C., Wabwire-Mangen, F., Paxton, L., Kiwanuka, N., Kigozi, G., Konde-Lule, J., Quinn, T. C., Gaydos, C. A., & McNairn, D. (1998). Population-based study of fertility in women with HIV-1 infection in Uganda. The Lancet, 351(9096), 98–103.
Homsy, J., Bennell, R., King, R., & Mermin, J. (2006). Determinants of Pregnancy Among Women Receiving HAART in Rural Uganda, Abstract 98. Paper presented at the PEPFAR Annual Meeting, 2006 HIV/AIDS Implementer’s Meeting. Durban, South Africa. June 12–15.
Kaida, A., Andia, I., Maier, M., Strathdee, S. A., Bangsberg, D. R., Spiegel, J., Bastos, F. I., Gray, G., & Hogg, R. (2006). The potential impact of antiretroviral therapy on fertility in sub-Saharan Africa. Current HIV/AIDS Reports, 3(4), 187–194.
Katz, M. H., Schwarcz, S. K., Kellogg, T. A., Klausner, J. D., Dilley, J. W., Gibson, S., & McFarland, W. (2002). Impact of highly active antiretroviral treatment on HIV seroincidence among men who have sex with men: San Francisco. American Journal of Public Health, 92(3), 388–394.
Kelly, J. A., Hoffman, R. G., Rompa, D., & Gray, M. (1998). Protease inhibitor combination therapies and perceptions of gay men regarding AIDS severity and the need to maintain safer sex. AIDS, 12(10), F91–F95.
Lewis, J. J., Ronsmans, C., Ezeh, A., & Gregson, S. (2004). The population impact of HIV on fertility in sub-Saharan Africa. AIDS, 18(Suppl 2), S35–S43.
Massad, L. S., Springer, G., Jacobson, L., Watts, H., Anastos, K., Korn, A., Cejtin, H., Stek, A., Young, M., Schmidt, J., & Minkoff, H. (2004). Pregnancy rates and predictors of conception, miscarriage and abortion in US women with HIV. AIDS, 18(2), 281–286.
Mermin, J., Ekwaru, J. P., Liechty, C. A., Were, W., Downing, R., Ransom, R., Weidle, P., Lule, J., Coutinho, A., & Solberg, P. (2006). Effect of co-trimoxazole prophylaxis, antiretroviral therapy, and insecticide-treated bednets on the frequency of malaria in HIV-1–infected adults in Uganda: A prospective cohort study. The Lancet, 367(9518), 1256–1261.
Miller, M., Meyer, L., Boufassa, F., Persoz, A., Sarr, A., Robain, M., & Spira, A. (2000). Sexual behavior changes and protease inhibitor therapy. SEROCO Study Group. AIDS, 14(4), F33–F39.
Moatti, J. P., Prudhomme, J., Traore, D. C., Juillet-Amari, A., Akribi, H. A., & Msellati, P. (2003). Access to antiretroviral treatment and sexual behaviours of HIV-infected patients aware of their serostatus in Cote d’Ivoire. AIDS, 17(Suppl 3), S69–S77.
Mohohlo, M., Khosa, T., Mohapi L, & Gray, G. (2006). Pregnancy-Related Events in an Antiretroviral Treatment Program, Abstract 113. Paper presented at the PEPFAR Annual Meeting, 2006 HIV/AIDS Implementer’s Meeting, Durban, South Africa. June 12–15.
Panozzo, L., Battegay, M., Friedl, A., & Vernazza, P. L. (2003). High risk behaviour and fertility desires among heterosexual HIV-positive patients with a serodiscordant partner-two challenging issues. Swiss Medical Weekly, 133(7–8), 124–127.
Ross, A., Van der Paal, L., Lubega, R., Mayanja, B. N., Shafer, L. A., & Whitworth, J. (2004). HIV-1 disease progression and fertility: The incidence of recognized pregnancy and pregnancy outcome in Uganda. AIDS, 18(5), 799–804.
Scheer, S., Chu, P. L., Klausner, J. D., Katz, M. H., & Schwarcz, S. K. (2001). Effect of highly active antiretroviral therapy on diagnoses of sexually transmitted diseases in people with AIDS. The Lancet, 357(9254), 432–435.
United Nations. (1997). World fertility patterns 1997 Africa. New York.
United Nations. (2005). Uganda Country Profile. New York.
UNAIDS. (2006). 2006 Report on the global AIDS epidemic. New York.
WHO. (2005). Core Health Indicators. Geneva.
WHO. (2006a). Core Health Indicators. Geneva.
WHO. (2006b). WHO case definitions of HIV for surveillance and revised clinical staging and immunological classification of HIV-related disease in adults and children. Retrieved March 9, 2007, from WHO case definitions of HIV for surveillance and revised clinical staging and immunological classification of HIV-related disease in adults and children. Geneva.
Wolf, K., Young, J., Rickenbach, M., Vernazza, P., Flepp, M., Furrer, H., Bernasconi, E., Hirschel, B., Telenti, A., Weber, R., & Bucher, H. C. (2003). Prevalence of unsafe sexual behavior among HIV-infected individuals: The Swiss HIV Cohort Study. Journal of Acquired Immune Deficiency Syndromes, 33(4), 494–499.
Zaba, B., & Gregson, S. (1998). Measuring the impact of HIV on fertility in Africa. AIDS, 12(Suppl 1), S41–S50.
Acknowledgements
Funding was provided from The Doris Duke Charitable Foundation, NIMH 54907, and NIAAA K-24 015287. The authors thank the Mbarara Hospital ISS clinic and Mbarara Hospital for their administrative support, as well as Drs. Deborah Cohan and John Tercier for their critical review of the manuscript. Finally, the authors thank the study participants for their time and willingness to share personal information with the study team.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Maier, M., Andia, I., Emenyonu, N. et al. Antiretroviral Therapy is Associated with Increased Fertility Desire, but not Pregnancy or Live Birth, among HIV+ Women in an Early HIV Treatment Program in Rural Uganda. AIDS Behav 13 (Suppl 1), 28–37 (2009). https://doi.org/10.1007/s10461-008-9371-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-008-9371-7