Abstract
Intracranial atherosclerotic disease (ICAD) is one of the most common causes of stroke worldwide and the one with the worst prognosis. In this study, we assessed the hypothesis that the balance of circulating pro- and antiangiogenic factors plays a role in the evolution of the disease and can be used as a potential marker for the disease course and a target for treatment. Seventy-four patients with severe ICAD were enrolled in this prospective observational study, medically optimized, and followed for 6 months. Thirteen pro- and eight antiangiogenic factors were measured in the participants’ serum using a sandwich multiplex ELISA. Angiogenic profiles were calculated using principal component analysis. We tested the association between angiogenic profiles and recurring cerebrovascular events despite intensive medical therapy, disability at 6 months after enrollment, and angiographic neovascularization in patients who failed medical treatment and underwent indirect revascularization surgery. There is a strong association between a functionally antiangiogenic profile and recurrent stroke or TIA in patients with ICAD (OR = 7.2, CI 2.4–34.4). Multivariable regression analysis showed that this antiangiogenic profile was also associated with poor functional status after 6 months (p = 0.002), independent from other clinical features such as history of previous stroke, diabetes, and age. In patients who failed medical management and underwent indirect revascularization surgery, high endostatin and angiostatin levels were also associated with low angiographic neovascularization (p = 0.02). The results of this study point to the striking importance of antiangiogenesis as a determinant of ICAD patient prognosis and suggest a possible new target for therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intracranial atherosclerotic disease (ICAD) is one of the most widespread causes of stroke worldwide [1,2,3]. It accounts for at least 10% of all strokes in the USA [4] and as much as 67% in countries with predominantly Asian, Hispanic, and Black inhabitants, which constitute the majority of the world population [1]. ICAD carries a worse prognosis than other stroke etiologies, with an annual rate of recurrent stroke and death of 15–35% despite intensive medical management [5,6,7]. Recent randomized controlled clinical trials have shown that stenting and bypass surgery fail to improve outcomes in ICAD cases [8,9,10]. The high prevalence, poor prognosis, and lack of treatment options for ICAD necessitate the identification of meaningful markers of the disease evolution and new targets for development of improved therapeutic strategies.
Preliminary work by Arenillas and Navarro-Sobrino has explored angiogenesis as a potential contributor to the pathophysiology of ICAD and acute ischemic stroke [11,12,13]. Arenillas et al. evaluated the proangiogenic vascular endothelial growth factor (VEGF) and the antiangiogenic endostatin in 40 patients with ICAD. They found that a higher ratio of endostatin/VEGF was associated with a higher number of intracranial atherosclerotic lesions and that elevated endostatin increased the risk for recurrent stroke at 13 months. However, this study was restricted to only two of the numerous known angiogenic factors and was conducted before the application of the current standards of intensive medical management. Navarro-Sobrino et al. evaluated 8 proangiogenic and 5 antiangiogenic factors in patients with acute ischemic stroke, showing that an acute antiangiogenic status determined by high endostatin plasma levels was associated with a worse long-term functional outcome. In this study, only 20% (n = 22) of the population included were cases of atherothrombosis, and no conclusions could be defined for that subpopulation.
Despite these important findings, the role of angiogenesis in ICAD has not been established. Determining the role and therapeutic potential of angiogenesis in ICAD requires an investigation of angiogenic molecules beyond VEGF and endostatin, and an evaluation of their relevance and interactions under intensive medical management and novel surgical treatments.
The investigation of numerous angiogenic factors as biomarkers poses several statistical challenges. The inclusion of multiple molecules and pathways generates data with high dimensionality that limits the meaningfulness of traditional inferential analysis. The absence of a full understanding of their correlations and interactions constrains the use of regression models to establish their association with clinical outcomes.
The study we are presenting aimed to determine the association between a broad spectrum of circulating factors and recurrent cerebrovascular events as well as functional outcomes in patients with ICAD. We conducted a prospective cohort study to evaluate the role of 21 circulating angiogenic factors, employing advanced statistical modeling to overcome the challenges mentioned above. Specifically, we tested the hypothesis that angiogenic phenotypes are associated with (1) the response to medical management in terms of stroke and transient ischemic attack (TIA), (2) functional clinical status at 6 months, and (3) angiographic neovascularization after encephaloduroarteriosynangiosis (EDAS) surgery.
Materials and methods
Population and study design
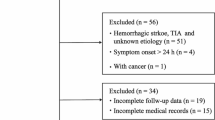
This prospective longitudinal cohort study involved patients diagnosed with ICAD in four hospitals in the Los Angeles metropolitan area where those patients initially presented due to past or current symptoms. Patients aged 25–85 years with a diagnosis of severe ICAD (≥ 70% stenosis) of any intracranial artery as measured by catheter, CT, or MR angiography between 2012 and 2014 were considered for inclusion. Independent vascular neurologists determined patient eligibility, based on the inclusion and exclusion criteria in Table 1. The study received approval from the local institutional review boards, and informed consent was obtained from each participant.
Upon enrollment, medical management was optimized for all patients, and they were followed to determine treatment success. A patient’s phenotype was defined as “non-responder” to medical management if s/he had any signs of ischemic stroke or transient ischemic attack (TIA) events or “responder” if the patient was asymptomatic under medical management. Demographic data, cardiovascular risk-factor history, smoking history, physical activity status, medications, detailed neurological examination, and a modified Rankin score (mRS) score were recorded. Baseline blood chemistry, lipid panel, and HbA1c were obtained.
Patients with recurrent symptoms despite adequate medical management were considered candidates for surgical revascularization and, if eligible, followed the management protocols of the EDAS Revascularization for Symptomatic Intracranial Arterial Stenosis Study (ClinicalTrials.gov identifier: NCT01819597).
Interventions
Medical management
Immediately upon enrollment, all patients underwent intensive medical treatment for primary risk factors (systolic blood pressure and low-density lipoprotein [LDL]), secondary risk factors (diabetes, non-high-density lipoprotein [non-HDL], smoking, obesity, and inadequate exercise) and antiplatelet medications. More specifically, patients with a history of high blood pressure or two or more consecutive measurements of systolic blood pressure > 140 mmHg were treated with at least one antihypertensive medication. Patients with hypercholesterolemia were treated with statin therapy to an LDLc goal of < 70 mg/dl. Patients with diabetes were managed medically to a HbA1c goal of < 6%. Patients were counseled to lose weight, cease smoking, and maintain physical activity with exercise for at least 30 min daily. In addition to the regular office visits, patients were contacted monthly by a research coordinator to promote compliance in medication and lifestyle changes.
Surgical management
The EDAS technique has previously been described in detail [14]. In summary, this is a revascularization procedure in which the superficial temporal artery (STA) is dissected from the scalp, while maintaining its proximal and terminal connections to the external carotid artery and the skin tissues, respectively. Then, the STA is placed under the skull in close proximity to the middle cerebral artery cortical branches. Over time neovascularization from the STA occurs providing flow to the intracranial circulation. Patients eligible for surgery continued intensive medical management with no interruption.
Follow-up
All patients underwent follow-up visits at 2 weeks and 1, 3, and 6 months after optimization. For patients who had an event on medical therapy and therefore underwent EDAS, postoperative visits occurred at 1, 3, and 6 months, with a follow-up catheter angiogram at 6 months. Additional visits were arranged for any patient if a potential TIA or ischemic stroke event was reported between scheduled follow-up visits. Vascular neurologists not involved in the analytical evaluation of the angiogenic factors determined whether TIA or ischemic stroke had occurred and assigned the mRS score for each patient at every evaluation point. The research coordination center monitored patient adherence to the scheduled visits, and transport services were provided to encourage patient adherence to the protocol.
Angiogenic factor measurements
Blood was collected at each visit in EDTA tubes. Serum was immediately separated by centrifugation at 3500 rpm for 15 min at 4 °C and stored in 2 cc cryovials at − 80 °C. Quantitative measurement of human angiogenic factors was taken using an enzyme-linked immunosorbent assay (ELISA Quantikine®, R&D Systems, MN; RayBio®, Raybiotech, GA; and Ciraplex® Aushon Biosystems, MA, USA) to detect the plasma level of vascular endothelial growth factor (VEGF) isoforms 165a and 165b, VEGF-D, soluble VEGF receptor (VEGFR)1, VEGFR2, VEGFR3, platelet-derived growth factor (PDGF)-AA, PDGFF-BB, fibroblast growth factor (FGF) b, hepatocyte growth factor (HGF), heparin-binding epidermal growth factor (HB-EGF), transforming growth factor (TGF) β1, TGF β2, bone morphogenic protein (BMP)-2, BMP-9, stromal cell-derived factor (SDF)-1, interleukin (IL) 4, thrombospondin (TSP)-1, TSP-2, endostatin, and angiostatin. These factors were selected after a review of the literature to obtain a broad representation of pro- and antiangiogenic factors. Each sample was analyzed twice, with the mean of the two values reported as the factor level. The mean intra-assay coefficient of variation (CV) was established with a threshold of less than 20% CV considered valid.
Statistics
Descriptive statistics were computed to summarize demographic and angiogenic factor data. A logarithmic transformation was used to correct for skewness in the angiogenic factor data (transformed angiogenic factor [Tr Angiogenic Factor] = (\( \ell_{n} \) Angiogenic factor + 1). Principal component analysis (PCA) was applied to the angiogenic factors to reduce data dimensionality and derive the equations for composite indexes denominated as angiogenic profiles (APs). Using PCA we were able to reduce the number of predictor variables from twenty-one angiogenic factors to seven principal components (APs) that preserve as much of the whole data variability (i.e., statistical information) as possible. Figure 1 illustrates the reduction of 21 angiogenic factor variables to seven principal components. Each principal component, denominated AP (1–7), contains an eigenvector and an eigenvalue that summarize the initial dataset. As no p values are computed during the creation of the APs, this methodology does not increase the false discovery rate but captures as much of the variability in the original data as possible. The inferential analysis included APs with eigenvalues higher than or equal to 1.0. We selected this threshold because the components with eigenvalues above 1 accounted for 75% of the total variance. The APs were calculated for each subject and constituted predictor variables in the subsequent statistical analyses. If more than one AP was associated with a specific response, the coefficients of the regression were used to resolve the final angiogenic profile associated with the outcome variable.
Vector representation of the initial dataset variability and post-principal component analysis (PCA) resultant angiogenic profiles (APs). This graphic illustrates the use of principal component analysis to reduce the number of variables tested, while maintaining the variability of the data. Instead of testing 21 angiogenic factors, seven angiogenic profiles summarize the information. Each angiogenic factor is represented in a as a vector in space contributing to the total variability of the data. Several angiogenic factors had significant correlations, as shown in detail in Supplementary Fig. 1. Correlations are represented here by their proximity in space and their individual contribution to the data variability by their length and diameter. B represents the principal components, the new variables (APs) resulting from the PCA, which encompasses the whole data variability but in a summarized manner. The final product of the APs direction (eigenvector) and diameter (eigenvalue) represents the complete data variance. A set of the first seven principal components (AP1–AP7) contained in this dataset 75% of the total data variability, allowing for an elimination of their high correlations and a reduction in the number of variables used for the inferential analyses
To evaluate the association of the APs with failure of medical management, a stepwise logistic regression model was built using the APs first as predictor variables. Subsequently, the significantly associated APs were incorporated in a multivariable logistic regression including the relevant clinical predictor variables: age, gender, previous stroke, hypertension, hypercholesterolemia, diabetes, and obesity (defined as a BMI ≥ 30). Each model’s fitness was evaluated using R-square and AUC of the corresponding ROC. An odds ratio was calculated for each variable from the regression parameters with their corresponding 95% confidence intervals.
The association between APs and functional outcomes at 6 months was evaluated with a multivariable ordinal logistic regression model. This model included age, gender, baseline mRS score, and the APs as the predictor variables. The outcome variable was the mRS score at 6 months. Significant findings were further investigated by constructing a prediction profiler using the ordinal model with 5000 simulation runs of random factor settings.
The association between APs and revascularization after surgical management was investigated in individuals failing medical management who underwent EDAS surgery. For this, a “neovascularization index” was defined as the Perren grades [15] plus an additional point if evidence of collaterals in the ASITN grades was observed in cerebral angiography 6 months after surgery. We built a linear regression model using stepwise regression with a minimum BIC stopping rule and backward direction for the outcome variable neovascularization index, including predictor variables: age, diabetes, smoking history, and baseline APs.
Finally, selected by the coefficient composition of the APs significantly associated with clinical outcomes, the main constituent angiogenic factors were compared between the outcome groups with two-sided student’s t test and one-way ANOVA for the transformed data.
Results
Eighty patients met inclusion criteria between July 2012 and December 2014. Six declined to participate, and 74 enrolled (Table 2). Mean age was 61.8 (SD = 12.3, range 28.6–83.3) years, with 39 females (52.7%). The majority of participants were non-Hispanic Whites. Overall compliance with intensive medical management was 95.9% for antiplatelet medication use, 90.6% for antihypertensive medication use, 94.9% for statins use, and 100% for diabetes management and smoking cessation. At presentation, the most common mRS score was 1.
During the 6-month follow-up period, 29 (39.1%) patients receiving medical therapy had recurrent cerebral ischemic events, including 3 who had only TIAs, 17 who had ischemic strokes without TIAs, and 9 who had both TIAs and ischemic strokes. As Table 2 shows, while non-responders and responders were largely similar in age, gender, race, ethnicity, location of the qualifying lesion, compliance with medical therapy, and general cardiovascular risk factors, non-responders less often had a history of stroke and a worse baseline disability status.
Measurements of all 21 angiogenic factors are given in Table 3 for responders and non-responders to medical therapy. Transformed angiogenic factor values were used to conduct the principal component analysis, which generated seven APs with eigenvalues higher than 1. These APs were named “AP1” to “AP7” in the order of decreasing eigenvalue. Figure 2 illustrates the principal components and their contributing angiogenic factors. The coefficients for each transformed angiogenic factor are provided in Supplementary Table 1.
Graphic representation of the angiogenic profiles (APs) calculated using principal component analysis. This graphic illustrates the new variables summarized as angiogenic profiles (APs) which contain different combinations of the 21 angiogenic factors evaluated. Each AP is shown as a vector. Their lengths represent their eigenvalue as proportion of the data variability accounted per each principal component. The seven APs capture 75% of the overall variance of all the 21 angiogenic factors studied. Each AP is built from a linear regression formula, and the coefficient of the main contributory angiogenic factors is represented as a proportion of its length. Positive coefficients are above the dotted line, and negative coefficients are below the dotted line. Proangiogenic factors are represented in white and antiangiogenic factors in yellow. Angiogenic profiles 4, 6, and 7 are predominantly antiangiogenic
Association of angiogenic profiles and recurrent ischemic events
The logistic regression model evaluating the association between the APs and phenotypic outcomes of responder and non-responder reached statistical significance (p = 0.001, R-square = 0.24, AUC = 0.81, 68.9% sensitivity, 80% specificity). As Table 4 indicates, the only AP significantly associated with the non-responder outcome was AP4 (p = 0.02), odds of non-responder being 2.1 (95% CI 1.2–4.1). AP4 was then evaluated in a multivariable logistic regression including the relevant clinical predictor variables: age, gender, previous stroke, hypertension, hypercholesterolemia, diabetes, and obesity. Table 5 describes the multivariable logistic regression model parameter results and odds ratios. The model reached statistical significance (p < 0.0001, R-square = 0.62, misclassification rate = 0.09, AUC = 0.96, 93.1% sensitivity, 89% specificity). In the multivariable model, AP4 was the only significant predictor parameter, with a p = 0.003, odds of non-responder being 7.2 (95% CI 2.4–34.4). AP4 is characterized by higher levels of HGF and the antiangiogenic factors VEGFR1, endostatin, and angiostatin.
We compared the major angiogenic factor components of AP4 between outcome groups. Figure 3 contrasts in two three-dimensional scatterplots the angiogenic factors data from patients responding to medical management and those not responding. The combination of the AP4 components HGF, angiostatin and endostatin levels generates a clear differentiation between responders and non-responders to medical management. Other factors such as VEGFA 165a, FGF, and PDGFAA, for example, did not permit such clear differentiation.
Three-dimensional scatterplots for the baseline levels of HGF, endostatin, and angiostatin in panel a, and VEGFA 165a, PDGFAA, and FGF in panel b. This graphic illustrates how the combination of the factors identified by PCA as part of the AP4 permits a clear delineation of the population between responders (blue) and non-responders (red). Notice how the combination of higher levels of HGF, angiostatin, and endostatin is associated with failure to medical management (red). Other factors combinations, like the one shown on panel b, do not discern such association
Finally, the mean blood levels of the transformed HGF, VEGFR1, and angiostatin were significantly higher among non-responders to medical management, as shown in Fig. 4. The mean levels of Tr-HGF were 6.27 ± 0.92 pg/mL among non-responders compared to 5.39 ± 0.6 pg/mL in the responders to medical management (p < 0.001). The mean levels of Tr-VEGFR1 were 5.27 ± 0.64 pg/mL among non-responders compared to 4.78 ± 1.6 pg/mL in the responders to medical management (p = 0.01). The levels of Tr-angiostatin were also higher in the non-responders (6.59 ± 0.35 ng/mL) versus responders (6.43 ± 0,23, p = 0.042). There was no statistically significant difference in the levels of Tr-endostatin (2.35 ± 0.12 in the non-responders vs. 2.38 ± 0.15 in the responders to medical management).
Comparative box plots for the levels of transformed HGF (a), VEGFR1 (b), angiostatin (c), and endostatin (d) between non-responders (red) and responders to medical management (blue). The figure illustrates the specific angiogenic factors, selected by the PCA, that were associated with no response to medical management. The levels of transformed HGF, VEGFR1, and angiostatin were significantly lower (p < 0.001 [***], p < 0.01 [**], and p < 0.05 [*], respectively) among the responders to intensive medical management. The levels of endostatin were not significantly different (NS)
Association of angiogenic profiles and functional outcomes at 6 months
The multivariable model evaluating the association between the APs at baseline and functional outcomes in terms of mRS score at 6 months after enrollment reached significance with a p = 0.01, R-square = 0.23, and a minimum AUC = 0.82. As described in Table 6, there was a significant association between the AP4 at baseline and the 6-month mRS score (p = 0.002), independently of age, gender, and baseline mRS score. No other predictor variable had a significant association with the functional outcomes. The association between AP4 and the individual mRS scores at 6 months was further investigated using a prediction profiler. Figure 5 shows the association of the AP4 with dichotomized functional outcomes at 6 months. Patients with poor functional outcomes (mRS ≥ 4) had significantly higher levels of the AP4 (p = 0.004).
The comparison of the angiogenic factor components of AP4, Tr-HGF and Tr-angiostatin, between functional outcomes groups at 6 months, revealed significant higher levels of HGF on individuals with poor functional performance than in those with good functional outcome (1276.1 ± 1312.6 pg/mL vs. 327.6 ± 324.7 pg/ml, respectively, p = 0.017). The levels of angiostatin were also higher in those with poor functional outcome (818.5 ± 200 ng/mL vs. 655.7 ± 201.3), but such difference was not statistically significant (p = 0.1) Fig. 6.
Association of angiogenic profiles and angiographic neovascularization after EDAS at 6 months
Among the 29 patients who failed medical management, 15 underwent EDAS revascularization. Five were male and 10 female, with a mean age of 60.7 (SD ± 12.7, range 32.1–83.3) years. Eleven patients completed angiographic follow-up 6 months after surgery. The stepwise regression model evaluating the predictor variables described in Table 7 and the neovascularization index outcome variable reached statistical significance (p = 0.02, R-square = 0.93). Significant predictors of the degree of revascularization included age, diabetes, and APs 1 to 6 at baseline. The regression formula solution for the significant AP components revealed a strong negative association with the antiangiogenic factors endostatin and angiostatin. Figure 7 illustrates the resolved formula coefficients for all angiogenic factors from the significant APs in association with the neovascularization index. Parameters between 1 and − 1 account for little of the variance. Endostatin and angiostatin are the most important.
Association between the level of the individual angiogenic factors and neovascularization after EDAS surgery as calculated from the solution of the regression coefficients of the APs. The graphic indicates that high levels of endostatin and angiostatin were negatively associated with revascularization rates at 6 months after EDAS
Discussion
This study included 74 patients with confirmed ICAD of at least 70% of intracranial vessels who underwent strict medical management. Twenty-nine (39.1%) of these patients had recurrent cerebral ischemic events during the 6-month follow-up despite intensive medical management. This higher than expected proportion of non-responders can be attributed to several factors. We included TIAs as criteria of failure to medical management, the majority of patients in the current study were older than 60, and 30% had a stenosis in the internal carotid artery. These last two factors have been previously associated with an increased risk for recurrent events [5].
We measured 13 proangiogenic and 8 antiangiogenic factors and evaluated their association with failure of medical management over 6 months. We also measured their correlation with functional status at 6 months, and, in those patients receiving EDAS surgery after failed medical management, with angiographic neovascularization. To reduce the data dimensionality and avoid the limiting effects of strong correlations between angiogenic factors for statistical analysis, we defined APs that summarize these factors using PCA [16]. Among the seven angiogenic profiles identified to explain the variance between angiogenic factors, AP4 was the most antiangiogenic, based on its PCA coefficients. This functionally antiangiogenic profile and its components (HGF, VEGFR1, angiostatin and endostatin) were stronger predictor of recurrent cerebral ischemic events than other clinical features, including a history of previous stroke, diabetes, and age, raising the odds of recurrent events sevenfold. They were also predictors of poor functional status independent of baseline mRS score and age. Lastly, digital subtraction angiographic evaluation of patients who received an indirect revascularization with EDAS showed a negative correlation between neovascularization and endostatin and angiostatin. Altogether, the results of this study point to the striking importance of antiangiogenesis as a determinant of ICAD patient prognosis.
Angiogenesis has been studied in peripheral vascular disease and myocardial ischemia [17, 18]. However, only limited evaluations of angiogenesis’s role in stroke and intracranial atherosclerosis have been conducted by Arenillas et al. [11] and Navarro-Sobrino et al. [12, 13], as previously discussed. Our use of PCA in the current study allowed us to concurrently probe multiple pro- and antiangiogenic factors, despite the complex biology of their interactions and roles in response to cerebral ischemia in ICAD. The statistical approach revealed high correlations among different inhibitors of angiogenesis that constituted AP4: endostatin, angiostatin, and VEGFR1. In addition, when more than one AP was significantly associated with an outcome, as with the neovascularization index, the model’s solution revealed a predominant correlation between endostatin and angiostatin and a strong negative association with neovascularization. Our study confirms the previously suggested association between endostatin and the disease’s progression and reveals that ICAD has a complex antiangiogenic profile dependence also involving angiostatin and VEGFR1.
AP4 also had an important component of elevated HGF. A link between elevated HGF and stroke has been observed by Rajpathak et al. [19] The underlying mechanism of this association is unknown, but a role for angiogenesis in large artery atherosclerotic plaques has been advocated [20]. However, the actual role of proangiogenesis in the small intracranial arteries has been questioned [11]. One reason for the reported association between elevated HGF and risk for stroke may be that hypoperfusion results in an increased proangiogenic signaling that leads to increased HGF but remains unmet due to prevailing antiangiogenic factors. In this case, the elevated levels of HGF would indicate a persistent but unmet need for collaterals. Unfortunately, no antiangiogenic factors were measured by Rajpathak et al. [19]. Another possible reason may be found in HGF’s molecular structure. That is, HGF is an αβ heterodimer, which is proangiogenic in its heterodimeric form only. Naturally occurring and artificially produced fragments of the α subunit, however, are antiangiogenic in function [21,22,23]. It may therefore be that apparent increases in HGF result from increased concentrations of the antiangiogenic α subunit fragments NK1 and NK2, which would fit with our observation that increases in antiangiogenic molecules predict poorer outcomes. We cannot rule out that the methodology used to quantify HGF detected those fragments, since epitope mapping of the antibody and cross-testing with NK1 and NK2 have not been performed.
Several treatment strategies for ICAD have been assessed, including medical management, reduction of the stenosis via stenting, direct revascularization via bypass, and indirect revascularization via EDAS. Of these, strict medical management appears to reduce the risk of embolism, but not progression of the stenosis or the effects of the resulting hypoperfusion [24]. As of now, strategies to directly reduce the stenosis or its resulting hypoperfusion via stenting or bypass have not proven successful in clinical trials [8,9,10]. The induction of neovascularization via EDAS surgery [24, 25], which relies on angiogenesis, has yielded encouraging initial results [14] and is under investigation. Pharmacological control of angiogenesis in the brain, however, still remains to be assessed and may present a promising alternative for mitigating the poststenotic hypoperfusion. The results of the present study suggest that controlling the antiangiogenic factors could be particularly effective. Notably, this observed association was independent of conventional risk factors such as age, smoking history, hypercholesterolemia, diabetes, obesity, or hypertension. This indicates that antiangiogenesis is an unappreciated risk factor for stroke and adverse outcomes.
In summary, this prospective cohort study of patients with severe ICAD identified a circulating angiogenic profile characterized by a high correlation between factors HGF, endostatin, angiostatin, and VEGFR-1, which was independently and significantly associated with failure of medical management and poor functional status after 6 months. Moreover, the study showed that elevated levels of endostatin and angiostatin were significantly associated with reduced neovascularization after EDAS surgery. Altogether, these findings identify antiangiogenesis as a key component of ICAD failure under medical management and suggest the benefit of defining new pharmaceutical strategies centered on regulating endogenous antiangiogenesis to protect against stroke.
References
Gorelick PB, Wong KS, Bae H-J, Pandey DK (2008) Large artery intracranial occlusive disease a large worldwide burden but a relatively neglected frontier. Stroke 39(8):2396–2399
De Silva DA, Woon F-P, Lee M-P, Chen CP, Chang H-M, Wong M-C (2007) South Asian patients with ischemic stroke intracranial large arteries are the predominant site of disease. Stroke 38(9):2592–2594
Wong LK (2006) Global burden of intracranial atherosclerosis. Int J Stroke 1(3):158–159
Sacco RL, Kargman D, Gu Q, Zamanillo M (1995) Race-ethnicity and determinants of intracranial atherosclerotic cerebral infarction: the Northern Manhattan Stroke Study. Stroke 26(1):14–20
Derdeyn CP, Chimowitz MI, Lynn MJ, Fiorella D, Turan TN, Janis LS, Montgomery J, Nizam A, Lane BF, Lutsep HL (2014) Aggressive medical treatment with or without stenting in high-risk patients with intracranial artery stenosis (SAMMPRIS): the final results of a randomised trial. Lancet 383(9914):333–341
Chimowitz MI, Lynn MJ, Howlett-Smith H, Stern BJ, Hertzberg VS, Frankel MR, Levine SR, Chaturvedi S, Kasner SE, Benesch CG, Sila CA, Jovin TG, Romano JG (2005) Comparison of warfarin and aspirin for symptomatic intracranial arterial stenosis. N Engl J Med 352(13):1305-1316. doi:352/13/1305 [pii] 10.1056/NEJMoa043033
Wityk R, Lehman D, Klag M, Coresh J, Ahn H, Litt B (1996) Race and sex differences in the distribution of cerebral atherosclerosis. Stroke 27(11):1974
Chimowitz MI, Lynn MJ, Derdeyn CP, Turan TN, Fiorella D, Lane BF, Janis LS, Lutsep HL, Barnwell SL, Waters MF (2011) Stenting versus aggressive medical therapy for intracranial arterial stenosis. N Engl J Med 365:993–1003
Awad I, Furlan AJ, Little JR (1984) Changes in intracranial stenotic lesions after extracranial-intracranial bypass surgery. J Neurosurg 60(4):771–776
Powers WJ, Clarke WR, Grubb RL Jr, Videen TO, Adams HP Jr, Derdeyn CP (2011) Extracranial-intracranial bypass surgery for stroke prevention in hemodynamic cerebral ischemia. JAMA, J Am Med Assoc 306(18):1983–1992
Arenillas JF, Alvarez-Sabin J, Montaner J, Rosell A, Molina CA, Rovira A, Ribo M, Sanchez E, Quintana M (2005) Angiogenesis in symptomatic intracranial atherosclerosis: predominance of the inhibitor endostatin is related to a greater extent and risk of recurrence. Stroke 36(1):92–97. doi:10.1161/01.STR.0000149617.65372.5d
Navarro-Sobrino M, Rosell A, Hernandez-Guillamon M, Penalba A, Boada C, Domingues-Montanari S, Ribo M, Alvarez-Sabin J, Montaner J (2011) A large screening of angiogenesis biomarkers and their association with neurological outcome after ischemic stroke. Atherosclerosis 216(1):205–211. doi:10.1016/j.atherosclerosis.2011.01.030
Massot A, Navarro-Sobrino M, Penalba A, Arenillas JF, Giralt D, Ribo M, Molina CA, Alvarez-Sabin J, Montaner J, Rosell A (2013) Decreased levels of angiogenic growth factors in intracranial atherosclerotic disease despite severity-related increase in endothelial progenitor cell counts. Cerebrovasc Dis 35(1):81–88. doi:10.1159/000346097
Gonzalez NR, Dusick JR, Connolly M, Bounni F, Martin NA, Van de Wiele B, Liebeskind DS, Saver JL (2015) Encephaloduroarteriosynangiosis for adult intracranial arterial steno-occlusive disease: long-term single-center experience with 107 operations. J Neurosurg. doi:10.3171/2014.10.JNS141426
Perren F, Horn P, Vajkoczy P, Schmiedek P, Meairs S (2005) Power Doppler imaging in detection of surgically induced indirect neoangiogenesis in adult moyamoya disease. J Neurosurg 103(5):869–872. doi:10.3171/jns.2005.103.5.0869
Sainani KL (2014) Introduction to principal components analysis. PMR 6(3):275–278. doi:10.1016/j.pmrj.2014.02.001
Rajagopalan S, Mohler ER 3rd, Lederman RJ, Mendelsohn FO, Saucedo JF, Goldman CK, Blebea J, Macko J, Kessler PD, Rasmussen HS, Annex BH (2003) Regional angiogenesis with vascular endothelial growth factor in peripheral arterial disease: a phase II randomized, double-blind, controlled study of adenoviral delivery of vascular endothelial growth factor 121 in patients with disabling intermittent claudication. Circulation 108(16):1933–1938. doi:10.1161/01.CIR.0000093398.16124.29
Abo-Auda W, Benza RL (2003) Therapeutic angiogenesis: review of current concepts and future directions. J Heart Lung Transpl 22(4):370–382. doi:10.1016/s1053-2498(02)00665-4
Rajpathak SN, Wang T, Wassertheil-Smoller S, Strickler HD, Kaplan RC, McGinn AP, Wildman RP, Rosenbaum D, Rohan TE, Scherer PE, Cushman M, Ho GYF (2010) Hepatocyte growth factor and the risk of ischemic stroke developing among postmenopausal women: results from the women’s health initiative. Stroke 41(5):857–862. doi:10.1161/strokeaha.109.567719
Chen XY, Wong KS, Lam WW, Zhao HL, Ng HK (2008) Middle cerebral artery atherosclerosis: histological comparison between plaques associated with and not associated with infarct in a postmortem study. Cerebrovasc Dis 25(1–2):74–80. doi:10.1159/000111525
Date K, Matsumoto K, Shimura H, Tanaka M, Nakamura T (1997) HGF/NK4 is a speci¢c antagonist for pleiotrophic actions of hepatocyte growth factor. FEBS J 420:1–6
Kuba K, Matsumoto K, Date K, Shimura H, Tanaka M, Nakamura T (2000) HGF/NK4, a four-kringle antagonist of hepatocyte growth factor, is an angiogenesis inhibitor that suppresses tumor growth and metastasis in mice. Cancer Res 60:6737–6743
Mizuno S, Nakamura T (2013) HGF-MET cascade, a key target for inhibiting cancer metastasis: the impact of NK4 discovery on cancer biology and therapeutics. Int J Mol Sci 14(1):888–919. doi:10.3390/ijms14010888
Gonzalez NR, Liebeskind DS, Dusick JR, Mayor F, Saver J (2013) Intracranial arterial stenoses: current viewpoints, novel approaches, and surgical perspectives. Neurosurg Rev 36(2):175–184. doi:10.1007/s10143-012-0432-z discussion 184–175
Dusick JR, Liebeskind DS, Saver JL, Martin NA, Gonzalez NR (2012) Indirect revascularization for nonmoyamoya intracranial arterial stenoses: clinical and angiographic outcomes. J Neurosurg 117(1):94–102. doi:10.3171/2012.4.JNS111103
Acknowledgements
This work was supported by grants from the American Heart Association (12PILT12760011 and 14ISA20870000), the NIH (K23 NS079477-01A1), as well as the Stotter Chair Endowment to NRG. We are grateful to Robert Elashoff, PhD, for statistical revision, as well as the UCLA Stroke Center members (Neal Rao, Lucas Restrepo, Jason Hitman, and Neil Martin) and the Cedars Sinai Stroke Center members (Patrick Lyden, Konrad Schlick, and Shlee Song) for their support and continuous collaboration. Also, we warmly thank the research coordination team led by Antoinette Anderson.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors do not declare any competing interests.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Gonzalez, N.R., Liou, R., Kurth, F. et al. Antiangiogenesis and medical therapy failure in intracranial atherosclerosis. Angiogenesis 21, 23–35 (2018). https://doi.org/10.1007/s10456-017-9578-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10456-017-9578-1