Abstract
The paradigm of a therapy aimed at inhibiting the formation of blood vessels, which would consequentially deprive cells and tissues of oxygen and nutrients, was born from the concept pioneered by the late Judah Folkman that blood vessel formation is central to the progression and maintenance of diseases which involve cellular metabolism and tissue expansion, and cancer in particular. The prototype targeted angiogenesis inhibitor anti-vascular endothelial growth factor (VEGF) antibody bevacizumab was approved in 2004 for colorectal cancer, and has since been approved for other cancers. Rheumatoid arthritis (RA) is a chronic inflammatory disease, during which inflamed tissue invades and destroys cartilage and bone. The tissue expansion, invasion, expression of cytokines and growth factors and areas of hypoxia which are a feature of RA have resulted in the hypothesis that angiogenesis inhibition may also be beneficial in RA, drawing on the success of bevacizumab. This review focuses on our current understanding of the importance of angiogenesis in RA, and on the lessons which may be learnt from the clinical experiences of angiogenesis blockade, particularly in colorectal cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Development of targeted therapies is the ultimate goal of many academic research units and biotechnology companies. The last 10–20 years have seen exciting advances in the field of targeted therapies, in particular the development of antibody-based approaches. Antibodies which block tumour necrosis factor (TNF) α, namely infliximab, adalimumab, golimumab and certolizumab, are approved for use in rheumatoid arthritis (RA), as well as in other chronic inflammatory disorders, with infliximab leading the way for the original approval of antibody therapy for RA. Just as antibody therapy is now widely accepted in RA, approval of antibody against vascular endothelial growth factor (VEGF) bevacizumab revolutionised treatment of colorectal cancer. At the time of writing, both infliximab and bevacizumab are in the ‘top 5’ list of therapeutic antibodies, and together make up a nearly 20% share of the top 10 best-selling drugs in 2010.
Interestingly, VEGF, described as an angiogenic factor more than a quarter of a century ago [1, 2], is also a potential therapeutic target in RA, and there are many parallels between solid tumours and inflammatory diseases such as RA, such as the involvement of cytokines and hypoxia, and the formation of new blood vessels (angiogenesis). The present review aims to focus on the role of the vasculature in the development and maintenance of RA, and to discuss the prospects for targeted anti-angiogenic therapy in RA, building upon the experiences gained from the use of novel biologicals such as bevacizumab in cancer.
Angiogenesis and RA
RA is a chronic inflammatory disease affecting approximately 1% of the population worldwide, with women 3 times more likely to be affected than men. Up to 30% of RA patients become permanently work-disabled within 3 years of diagnosis if not treated, highlighting the impact of RA on quality of life [3]. For example, it has been documented in a recent study that at the time of first symptoms of RA, 86% of men and 64% of women aged less than 65 years were working. More than one-third (37%) of these patients reported subsequent work disability, and the probabilities of continuing to work were 80 and 68% at 2 and 5 years, respectively [4]. RA may begin at any time from the first few weeks of life until the ninth decade, although the peak time of presentation is 35–45 years of age, with patients presenting with painful, stiff and swollen joints, predominantly the small joints of the hands and wrists, as well as the metatarsophalangeal joints, ankles, knees and cervical spine. In most patients, symptoms appear over weeks to months, starting in one joint and often accompanied by prodromal symptoms including anorexia, weakness, or fatigue.
In RA, the synovial membrane becomes inflamed and increases in thickness, eventually forming an active front or ‘pannus’, which invades and destroys underlying cartilage and bone. Normally 1–2 cell layers thick, the synovium in RA increases to a thickness of several cell layers, due to a combination of cellular hyperproliferation and infiltration by cells derived from the circulation, predominantly T-cells and monocytes. The synovial fluid becomes rich in neutrophils, and increases in volume due to oedema, leading to joint swelling and pain. This synovium invades cartilage and bone, resulting in the destruction of cartilage and bone. In the context of this review, it has been recognized for a number of years that angiogenesis is an important process in the development and maintenance of RA, and that VEGF plays a particularly crucial role [5–8]. The synovial hyperplasia which occurs in RA leads to an increased demand for oxygen and nutrients within the synovium, and hence low oxygen tension. The hypoxic milieu in turn drives expression of hypoxia-sensitive angiogenic factors such as VEGF, and interacts with other inflammatory signalling pathway such as the NFκB cascade. The newly formed blood vessels supply the synovial tissue with oxygen and nutrients necessary for cellular metabolism and division, and bring in leukocytes, as well as cytokines, chemoattractants and growth factors, thus further perpetuating the angiogenic cycle in RA synovium (Fig. 1).
One of the earliest reports suggesting that angiogenesis may be a feature of RA was the description in 1980 that a low molecular weight angiogenesis factor (apparently identical with that derived from tumours but predating the description of VEGF) was present in synovial fluids from RA patients [9]. RA synovial fluids were later shown to induce morphological changes in human endothelial cells, with formation of tubule-like structures and induction of angiogenesis in an in vitro assay [10, 11]. It is now clear that RA synovium is characterised by alterations in synovial vessel density, in areas of diffuse synovitis and in regions of large leukocytic infiltrates with germinal centre-like structures [12]. Alterations in endothelial turnover and apoptosis have been reported, coupled with expression of cycle-associated antigens, consistent with increased vascular proliferation [13, 14]. A recent study has documented the presence of immature blood vessels in RA synovium. Comparison of the staining patterns for CD31 and the pericyte marker α-smooth muscle cell actin revealed a significant fraction of CD31-positive but α-smooth muscle cell actin-negative cells in RA tissue when compared to osteoarthritis (OA) or control tissue [15]. This altered vascular signal in RA synovium has also recently been detected using Doppler ultrasound [16, 17].
Targeting VEGF in models of arthritis
Many studies have reported that expression of angiogenesis-regulating factors is altered in RA. The best characterized growth factor expressed in RA is VEGF, a potent and relatively selective inducer of endothelial cell survival, migration and proliferation [18–21]. More than 10 years ago the groups of Koch and Fava almost simultaneously reported VEGF expression in RA synovial fluids and tissue [22, 23]. In addition to synovial expression of VEGF and its receptors, circulating (serum) levels of VEGF are increased, and correlate with inflammatory response markers such as C-reactive protein and swollen joint counts [24–33]. VEGF levels are increased even in RA patients with disease duration of less than 2 years, and predict subsequent joint destruction, suggesting that angiogenesis may be an early event in RA progression [34]. Serum VEGF levels have also been shown to correlate with blood flow in wrist synovium of patients with RA [35].
The expression of high levels of VEGF in RA was the basis of proposing that targeting angiogenesis may be of therapeutic benefit. Murine collagen-induced arthritis (CIA) is a model widely used for the testing of potential therapeutics for RA, and was utilised to develop TNFα inhibitors as a therapeutic modality for RA [36]. In CIA, expression of VEGF and VEGF receptors has been demonstrated [37–39]. Studies from our own laboratory have shown that CD31-positive blood vessels are visible in both early and advanced stages arthritis, in parallel with synovial expansion/inflammation and expression of VEGF (Fig. 2). Importantly, inhibition of angiogenesis has been shown to be effective in CIA. For example, treatment of CIA in rats with broadly acting angiogenesis inhibitors AGM-1470 or Taxol, or other inhibitors of endothelial proliferation, significantly suppressed disease [40–45]. The data described above prompted studies of the effectiveness of VEGF inhibition as a therapeutic approach for treatment of RA. Anti-VEGF antibody delayed disease onset, but appeared less effective when administered during the chronic phase of disease [37]. In another study, anti-VEGF inhibited synovitis in CIA, as indicated by a reduction in clinical score and paw swelling relative to untreated mice [46]. A soluble form of VEGFR1 has also been shown to significantly suppress established arthritis [47, 48]. A different strategy to limit angiogenesis via the VEGF pathway was to directly target VEGFR in models of arthritis. In a spontaneous model of arthritis in KRN/NOD mice, De Bandt et al. observed that treatment with anti-VEGFR1 (but not anti-VEGFR2) antibody abrogated bone and cartilage destruction. The antibody delayed the onset of arthritis and attenuated the severity of disease [49]. The group of Carmeliet also demonstrated that treatment with antibody against VEGFR1 reduced the incidence of joint disease, whereas antibody specific for VEGFR2 appeared ineffective [50].
Murine collagen-induced arthritis as a model of RA. b CD31 and c VEGF expression in metatarsal sections of mice at different stages of collagen-induced arthritis, with corresponding haematoxylin-eosin sections (a) shown. d High-power images of VEGF expression in early and late arthritis. B = bone, C = cartilage, M = muscle, S = synovium, V = vessels
Taken together, these findings suggest that inhibiting VEGF may be of benefit in RA. However, in parallel with these studies, a wealth of evidence has accumulated about the clinical effectiveness of VEGF blockade in cancer, particularly colorectal cancer, and this will be reviewed in the following section.
Angiogenesis inhibition in cancer: what have we learnt?
The parallels between solid tumours and RA (hypoxia, involvement of cytokines, angiogenesis) have led to suggestions that inhibiting angiogenesis in RA might be of benefit, as has been shown in particular for colorectal cancer, the third most common malignancy in the West and the second most common cause of cancer death.
The idea that new blood vessel formation may be a therapeutic target in solid tumours stemmed from work by Judah Folkman in the early 1970s demonstrating the pivotal role of angiogenesis in the development of tumours. For continued growth, a tumour which exceeds 1–2 mm3 in volume requires its own blood supply, through secretion of factors such as VEGF [51]. The efficacy of bevacizumab (monoclonal anti-VEGF antibody) in metastatic colorectal cancer provided confirmation that targeting angiogenesis has therapeutic benefit in cancer [52, 53]. A number of trials have consistently reported increased response rate, and prolonged progression free survival and overall survival. For example, when used as first-line therapy in addition to irinotecan, fluorouracil (FU) and leucovorin (LV), bevacizumab increased median progression free survival from 6.2 to 10.6 months and median overall survival from 15.6 to 20.3 months [53]. The benefit of VEGF inhibition persists with newer cytotoxic agents. Used as second-line therapy in patients previously treated with cytotoxic agents, bevacizumab improved response rate from 8.6 to 22.7%, progression free survival from 4.7 to 7.3 months and overall survival from 10.8 to 12.9 months when given in addition to the FOLFOX4 regime (oxaliplatin, FU and LV) [54].
However, bevacizumab therapy is associated with adverse events including hypertension, thromboembolic events, bleeding, gastro-intestinal (GI) perforation and proteinuria. For example, studies have reported a bevacizumab-induced five-fold increase in the incidence of severe (Grade 3) hypertension [55]. Hypertension has also been reported in breast cancer, non-small cell lung cancer, renal cell carcinoma and hepatocellular carcinoma [56–59]. Mild, asymptomatic proteinuria has further been reported [60]. According to a recent meta-analysis, in colorectal cancer bevacizumab increases the risk of significant proteinuria by 2.52 [61]. Nephrotic syndrome, characterised by Grade 3 proteinuria plus hypoalbuminaemia leading to gross oedema, has been reported in metastatic breast and pancreatic cancer [57, 62]. Treatment with bevacizumab is moreover associated with risk of serious arterial thromboembolic events [63, 64]. In a pooled analysis of 5 randomised clinical trials (1,745 patients with metastatic colorectal cancer, breast or non-small cell lung cancer), the risk of arterial thromboembolism was doubled (from 1.7% to 3.8; P = 0.031) by addition of bevacizumab to chemotherapy [63]. The evidence for venous thromboembolism (VTE) in the context of bevacizumab therapy is less clear cut. Scappaticci et al. reported no effect on VTE incidence in colorectal cancer [63]. However, a meta-analysis subsequently reported an increase in high-grade (life-threatening) VTE from 4.4 to 7.3% in colorectal cancer [65]. Mucocutaneous bleeding and epistaxis are common adverse effects, reported in up to 24% of bevacizumab treated colorectal cancer patients [60], and an increased incidence of severe bleeding requiring transfusion, primarily of the GI tract, has been reported [54]. There have also been reports of GI perforation [66], and surgical complications including delayed wound healing [67], wound failure (dehiscence or incisional hernias) [68], and anastomotic leak or breakdown [69, 70].
Two recent developments are significant. In the US, the FDA announced withdrawal of approval for bevacizumab in metastatic breast cancer, citing the lack of evidence of sufficient efficacy in light of significant side-effects [71]. In the UK, the National Institute for Health and Clinical Excellence announced (December 2010) that bevacizumab is not recommended for metastatic colorectal cancer, stating that its efficacy does not justify the high costs [72].
Angiogenesis inhibition: prospects for new targets in RA
Alternative growth factor targets
The side-effects of VEGF inhibition in cancer have driven the search to identify alternative angiogenic targets. In RA, growth factors expressed in RA in addition to VEGF include fibroblast growth factor (FGF)-1 and FGF-2 [73], platelet-derived growth factor-B [74, 75] and hepatocyte growth factor [76]. Furthermore, expression of angiopoietins (Ang)-1 and Ang-2 [77, 78] and Ang receptors Tie-1 and Tie-2 [79–81] in RA synovial tissue has been described. For example, Shahrara et al. [80] have shown that Ang-1 immunostaining on synovial lining cells, macrophages and endothelial cells was significantly higher in RA samples compared to osteoarthritis and normal synovial tissue. The use of biologicals to specifically target the Ang-Tie receptors in order to inhibit pathological angiogenesis may offer a novel therapeutic strategy in RA. Soluble Tie-2 receptor was shown to be efficacious in murine CIA [82], and we have shown that administration of a splice variant of Tie-1 demonstrated significant efficacy in CIA. We observed that gene expression levels of Ang1, Ang2, and receptors Tie1 and Tie2 in mouse paws were significantly increased during the progression of CIA, suggesting dysregulation of the Ang-Tie system and highlighting its importance in the angiogenesis that is critical for arthritis development. Administration of Tie-1 produced a significant reduction in disease severity in CIA, together with improvement of joint architecture and reduced CD31-immunopositive staining [83, 84].
Other growth factors expressed in RA include members of the epidermal growth factor (EGF) family. The EGF family (ErbB and human epidermal growth factor receptor, HER) of cell-surface tyrosine kinase receptors, namely EGFR/HER-1/ErbB1, HER-2/ErbB2, HER-3/ErbB3 and HER-4/ErbB4, are activated by a large family of ligands including EGF itself, as well as by transforming growth factor (TGF)-α, heparin-binding EGF like growth factor, amphiregulin (AR), betacellulin, epiregulin, epigen and neuregulins [85–87]. Activation of EGF receptors leads to stimulation of several intracellular pathways, resulting in stimulation of angiogenesis via increased VEGF expression, as well as cell proliferation and inhibition of apoptosis [88]. EGFR over-expression is a feature of colorectal cancer and is associated with decreased survival and response to radiotherapy [89, 90]. Cetuximab and panitumumab, which are in use in colorectal cancer, are monoclonal antibodies directed against EGFR and may act in part by reducing angiogenesis [91]. Other treatments targeting EGF/EGF receptors include the first approved HER therapeutic trastuzumab, a monoclonal antibody that targets HER-2 and has revolutionised the treatment of HER-2-over-expressing, node-positive or node-negative breast cancer [92]. In contrast, lapatinib is a tyrosine kinase inhibitor which interrupts EGFR/HER-1 and HER-2 signalling and has been approved as front-line therapy in triple positive breast cancer and as an adjuvant therapy when patients have progressed on trastuzumab. Erlotinib is used to treat non-small cell lung cancer and pancreatic cancer, and is an inhibitor targeting EGFR/HER-1 [93].
A number of studies suggest that the EGF ligand: receptor family has a role in the development of inflammatory arthritis [94–96]. In addition to the presence of EGF in RA synovium [91], expression of HER-2/ErbB2 has also been reported [95]. Other EGF receptor ligands have also been detected, namely TGF-α and AR [94, 97]. We have demonstrated an inhibitor of the HER family, herstatin, when administered therapeutically to mice with CIA, controlled clinical and histologic signs of disease and reduced the number of joints with severe damage [98]. Since our histological analysis indicated a return to near normal joint architecture, a possible way in which the therapy could be effective is through the reduction of neovascularisation in CIA following EGFR blockade, using approaches such as cetuximab, panitumumab, trastuzumab or new drugs such as lapatinib.
Targeting the hypoxia/HIF pathway
Just as low oxygen tension—hypoxia—has been postulated to contribute to tumour angiogenesis, so hypoxia has been suggested to play a role in RA. The regulators of the adaptive response to alterations in oxygen tension are members of the family of transcription factors termed hypoxia-inducible factors (HIFs), which are exquisitely sensitive to changes in oxygen tension [99]. To date, it has been established that approximately 1% of all human genes are regulated by HIF, including genes involved in angiogenesis, apoptosis, vasomotor control, erythropoiesis and energy metabolism. HIF is a heterodimeric transcription factor, composed of α and β subunits [100]. Regulation of HIF-dependent gene expression requires α-subunit accumulation in the cytoplasm and translocation into the nucleus, which enables it to dimerise with HIF-β. HIF heterodimers are then recognised by co-activators and bind to the hypoxia-response elements (HRE) in the target gene to initiate transcription.
The main regulators of HIF-α levels are oxygenases governed by O2, 2-oxoglutarate (2-OG), Fe2+ and ascorbic acid, named HIF prolyl hydroxylase domain (PHD)-containing enzymes and factor inhibiting HIF (FIH-1). HIF-α sub-units encompass an O2-dependent degradation domain (ODD), responsible for hypoxic stabilisation of α-subunits, and two transactivating domains, namely the N-terminal and C-terminal domains (N-TAD and C-TAD, respectively). The C-TAD has been shown to interact with co-activators such as p300/CBP to activate transcription. The PHD enzymes hydroxylate proline residues in the ODD, thus making HIF-α recognisable by the von Hippel Lindau tumour suppressor protein [101], which leads to polyubiquitination and proteolytic destruction of α-subunits by the 26S proteasome. Thus, under conditions where O2 is limiting, HIF-α subunits accumulate and activate transcription of HRE-containing genes.
In RA, as the synovium expands more blood vessels are needed to supply poorly perfused and oxygenated areas distant from the pre-existing blood vessels. A study from our laboratory reported that synovial tissue in RA patients was hypoxic (median O2 2–4%) when compared to patients without RA (9–12%) [102]. These findings complement data obtained more than 30 years ago, which first described synovial hypoxia in RA [103, 104]. A number of factors are believed to interplay to produce the hypoxic environment. The oxygen consumption of the RA synovium is elevated, quite likely as a consequence of the fibroblast hyperproliferation which occurs in RA [105–107]. These findings of an anaerobic and acidic microenvironment with expression of glycolytic enzymes [108] have been supported by magnetic resonance spectroscopy, confirming the presence of low molecular weight metabolites, consistent with hypoxia [109]. A recent study using ultra-sonography to assess synovial thickening also demonstrated increased proliferation and significantly lower synovial fluid pO2 levels in RA compared to non-RA patients [107]. An inverse correlation between synovial oxygen tension and synovitis has been described [110, 111]. Synovial hypoxia in RA is also driven by the accumulation of synovial fluid, which is thought to apply pressure on existing vessels, thereby further compromising oxygen flow to the synovium. In support of this, Richman et al. have shown that oxygen tensions in the synovial fluid vary inversely with volumes of synovial fluid [112]. In RA synovium, HIF-α isoforms (HIF-1α, HIF-2α) are expressed [113–115] and correlate with indices of angiogenesis [27, 116], and HIF expression has also been shown in experimental arthritis models [117, 118]. Of relevance to this review, hypoxia has been shown to upregulate VEGF expression by RA synovial cells and to increase the pro-angiogenic activity of these cells [102, 119]. Other hypoxia/HIF regulated genes in RA are thought to include matrix-degrading enzymes, suggesting that hypoxia might promote synovial invasion of underlying tissue [120].
Inhibition of the hypoxia/HIF-α pathway—in cancer or indeed in RA—represents an alternative therapeutic target because HIF-α downregulation not only affects levels of VEGF but also levels of many other genes that are important in cell metabolism. Indeed, destabilisation of HIF-α by increasing its hydroxylation and degradation through the PHDs, or decreasing transcriptional activation via FIH-1, has become a very popular approach in the fight against cancer. Recent studies have shown that it could be possible to reverse the inhibition of HIF-α regulating enzymes (PHDs/FIH-1) by low oxygen levels (as might be expected to be the case in a hypoxic environment such as that in RA synovium), in order to decrease HIF-α stability in hypoxic conditions. Matsumuto and colleagues have evaluated the effect of 2-OG, an essential co-factor for PHD and FIH-1 hydroxylase activity, on the production of erythropoietin and VEGF in Hep3B cells, and found that 2-OG dose-dependently inhibited HIF-1α, erythropoietin and VEGF protein levels in Hep3B cells in hypoxic conditions, and also dose-dependently inhibited tube formation in in vitro angiogenesis assays, presumably by enhancing PHD/FIH-1 activity [121]. In a more recent study they reported similar results in Lewis lung cancer cells, in both a mouse dorsal air sac assay and a murine tumour xenograft model [122], in which 2-OG was shown to dose-dependently reduce HIF-1α protein and VEGF mRNA. In addition, 2-OG was also shown to reduce tumour size when injected into mice with solid tumours, suggesting that a similar approach—namely upregulating PHD activity—might be of benefit in arthritis.
Other approaches targeting HIFs have been less successful, in that agents which have been reported to inhibit the expression and/or activity of HIF-α are frequently of broad specificity. For example, YC-1 is known to inhibit the expression of HIF-1α at the post-transcriptional level but is also an inhibitor of soluble guanylate cyclase [123]. An inhibitor of histone deacetylase, FK228, also inhbits HIF expression and VEGF induction in RA cells [124]. Shankar et al. have investigated the effect of 2-benzoyl-phenoxy acetamide (BP-1) a synthetic benzophenone analogue, in an experimental arthritis rat model [125]. Benzophenones, obtained from natural sources or synthetically, are potent anti-inflammatory compounds which exhibit significant anti-tumour activity in both in vivo and in vitro. Treatment with BP-1 significantly reduced the increase in paw in arthritic rats in a dose-dependent manner. BP-1-treated synovium was 60% less vascular that the untreated control synovium. Furthermore BP-1 inhibited HIF-1α accumulation and VEGF mRNA expression in vitro and in vivo, suggesting that BP-1 can act as a novel anti-arthritic agent [125].
Considering the unwanted effects of current clinical trials with anti-angiogenic agents, targeting the hypoxia/HIF axis opens the way to design new strategies and to find more successful approaches to inhibit angiogenesis in cancer, as well as in RA.
Conclusions
In 1998, the role of the vasculature in RA and on the prospects for developing vascular-targeted therapies for RA was discussed in this journal [126]. Nearly 10 years later, following approval of bevacizumab for colorectal cancer, it seemed plausible that approval of angiogenesis inhibitors in inflammatory diseases such as RA could rapidly follow [127]. In the intervening period, much has been learnt about the benefits—and possible pitfalls—of angiogenesis inhibition in cancer and more recently in ocular disease. In 2010, Napoleone Ferrara received the Lasker-DeBakey Clinical Medical Research Award for the discovery of VEGF as a mediator of angiogenesis [128] and the development of anti-VEGF therapy for wet macular degeneration, but while there is little doubt that VEGF inhibition using bevacizumab has been shown to be extremely effective, caution needs to be exercised.
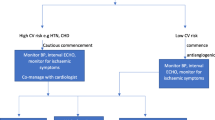
Specifically, whether VEGF inhibition can be extended into RA is currently under debate. As discussed, VEGF inhibition in vivo is associated with side-effects, particularly hypertension and thromboembolic events, and these have clear implications for the potential usefulness in RA of VEGF inhibition. RA is associated with a higher frequency of cardiovascular disease [129–131], with more than 40% of deaths in RA reported to be due to cardiovascular diseases, including ischemic heart disease and heart failure. The standardized mortality ratio for the RA cohort was 2.64 relative to the general population, compared with 0.98 for the control group [132]. A recent study reported that the odds ratio for the risk of all-category stroke in RA was 1.64, and for the risk of ischemic stroke was 2.66 [133]. In another study, which comprised more than 100,000 women free of RA and cardiovascular disease at baseline, the adjusted relative risks of myocardial infarction and stroke in women subsequently diagnosed with RA were 2.00 and 1.48, respectively, when compared to women without RA [134]. A high 10-year risk of cardiovascular disease in newly diagnosed RA patients has been described, with the absolute cardiovascular risk in RA patients similar to that in non-RA subjects who were 5–10 years older [135]. RA patients also have an increased risk of fatality following myocardial infarction (assessed as the 30 day mortality rates following a first acute cardiovascular event) [136]. A recent study reported arterial stiffness to be strongly associated with endothelial dysfunction and overt atherosclerosis in patients with autoimmune diseases such as RA [137].
The increased cardiovascular disease in RA, coupled with the increased risk of thromboembolic complications following VEGF blockade in cancer, suggests that other approaches to inhibit angiogenesis might be useful. What might be the advantage of targeting HIFs rather than VEGF, a hypoxia-inducible gene? HIFs regulate a range of other angiogenic growth factors and molecules, including inflammatory cytokines and chemokines. Crucially, although there are many similarities between HIF-1α and HIF-2α, there is growing evidence revealing differences, implying that they have distinct biological roles in different cell types. Microarray-based studies revealed that HIF-2α regulates approximately 13% (36/271) of genes upregulated by hypoxia, and 17% of downregulated genes (37/217) [138]. HIF-1α regulates genes involved in metabolism, regulating glycolysis and glucose uptake [139, 140]. In addition HIF-1α activates angiogenesis, survival, and invasion, most importantly in normal development and in response to stress. Conversely HIF-2α regulates a small group of genes involved specifically in tumourigenesis [141]. It has thus become clear that by having contrasting effects on regulation of HIF-target genes, HIF-1α and HIF-2α may contribute to progression or regression of angiogenesis-dependent diseases such as RA. Understanding how HIF-1α and HIF-2α, both of which are expressed in RA, contribute to synovial angiogenesis, might lead to specific targeting of one or other isoform. Assuming selective inhibitors of HIFs are developed in the future, such an approach might avoid the side-effects seen with bevacizumab.
Nevertheless, it would be premature to discount, for example, combined TNFα and VEGF blockade, or perhaps, combined TNFα and EGF/EGFR blockade, in RA. Anti-TNFα biologicals are associated with an approximately two to fourfold increased risk of serious bacterial infections, including tuberculosis [142–145]. Targeting the TNF pathway together with angiogenesis inhibitors should not, in contrast, result in increased infection rates. The importance of angiogenesis in RA, driven by in part by a combination of hypoxia and VEGF, is undisputed, and angiogenesis inhibition still seems a reasonable therapeutic approach, and is supported by a wealth of animal studies. The non-responder cohort to anti-cytokine therapy, coupled with the increased risk of infections such as tuberculosis, mean that improvements to current treatments in RA are still necessary, and angiogenesis blockade could be a potential therapeutic opportunity.
References
Senger DR, Galli SJ, Dvorak AM, Perruzzi CA, Harvey VS, Dvorak HF (1983) Tumor cells secrete a vascular permeability factor that promotes accumulation of ascites fluid. Science 219:983–985
Senger DR, Perruzzi CA, Feder J, Dvorak HF (1986) A highly conserved vascular permeability factor secreted by a variety of human and rodent tumor cell lines. Cancer Res 46:5629–5632
Barrett EM, Scott DG, Wiles NJ, Symmons DP (2000) The impact of rheumatoid arthritis on employment status in the early years of disease: a UK community-based study. Rheumatology (Oxford) 39:1403–1409
Sokka T, Kautiainen H, Pincus T, Verstappen SM, Aggarwal A, Alten R, Andersone D, Badsha H, Baecklund E, Belmonte M, Craig-Muller J, da Mota LM, Dimic A, Fathi NA, Ferraccioli G, Fukuda W, Geher P, Gogus F, Hajjaj-Hassouni N, Hamoud H, Haugeberg G, Henrohn D, Horslev-Petersen K, Ionescu R, Karateew D, Kuuse R, Laurindo IM, Lazovskis J, Luukkainen R, Mofti A, Murphy E, Nakajima A, Oyoo O, Pandya SC, Pohl C, Predeteanu D, Rexhepi M, Rexhepi S, Sharma B, Shono E, Sibilia J, Sierakowski S, Skopouli FN, Stropuviene S, Toloza S, Valter I, Woolf A, Yamanaka H (2010) Work disability remains a major problem in rheumatoid arthritis in the 2000s: data from 32 countries in the QUEST-RA Study. Arthritis Res Ther 12:R42
Szekanecz Z, Gaspar L, Koch AE (2005) Angiogenesis in rheumatoid arthritis. Front Biosci 10:1739–1753
Szekanecz Z, Koch AE (2008) Targeting Angiogenesis in Rheumatoid Arthritis. Curr Rheumatol Rev 4:298–303
Szekanecz Z, Szegedi G, Koch AE (1998) Angiogenesis in rheumatoid arthritis: pathogenic and clinical significance. J Investig Med 46:27–41
Paleolog EM (2009) The vasculature in rheumatoid arthritis: cause or consequence? Int J Exp Pathol 90:249–261
Brown RA, Weiss JB, Tomlinson IW, Phillips P, Kumar S (1980) Angiogenic factor from synovial fluid resembling that from tumours. Lancet 1:682–685
Semble EL, Turner RA, McCrickard EL (1985) Rheumatoid arthritis and osteoarthritis synovial fluid effects on primary human endothelial cell cultures. J Rheumatol 12:237–241
Kumar P, Erroi A, Sattar A, Kumar S (1985) Weibel-Palade bodies as a marker for neovascularization induced by tumor and rheumatoid angiogenesis factors. Cancer Res 45:4339–4348
Fearon U, Griosios K, Fraser A, Reece R, Emery P, Jones PF, Veale DJ (2003) Angiopoietins, growth factors, and vascular morphology in early arthritis. J Rheumatol 30:260–268
Ceponis A, Konttinen YT, Imai S, Tamulaitiene M, Li TF, Xu JW, Hietanen J, Santavirta S, Fassbender HG (1998) Synovial lining, endothelial and inflammatory mononuclear cell proliferation in synovial membranes in psoriatic and reactive arthritis: a comparative quantitative morphometric study. Br J Rheumatol 37:170–178
Walsh DA, Wade M, Mapp PI, Blake DR (1998) Focally regulated endothelial proliferation and cell death in human synovium. Am J Pathol 152:691–702
Izquierdo E, Canete JD, Celis R, Santiago B, Usategui A, Sanmarti R, Del Rey MJ, Pablos JL (2009) Immature blood vessels in rheumatoid synovium are selectively depleted in response to anti-TNF therapy. PLoS One 4:e8131
Larche MJ, Seymour M, Lim A, Eckersley RJ, Petavy F, Chiesa F, Rioja I, Lukey PT, Binks M, McClinton C, Dolan K, Taylor PC (2010) Quantitative power doppler ultrasonography is a sensitive measure of metacarpophalangeal joint synovial vascularity in rheumatoid arthritis and declines significantly following a 2-week course of oral low-dose corticosteroids. J Rheumatol 37:2493–2501
Taylor PC, Steuer A, Gruber J, Cosgrove DO, Blomley MJ, Marsters PA, Wagner CL, McClinton C, Maini RN (2004) Comparison of ultrasonographic assessment of synovitis and joint vascularity with radiographic evaluation in a randomized, placebo-controlled study of infliximab therapy in early rheumatoid arthritis. Arthritis Rheum 50:1107–1116
Ferrara N, Gerber HP, LeCouter J (2003) The biology of VEGF and its receptors. Nat Med 9:669–676
Ferrara N (2004) Vascular endothelial growth factor: basic science and clinical progress. Endocr Rev 25:581–611
Ho QT, Kuo CJ (2007) Vascular endothelial growth factor: biology and therapeutic applications. Int J Biochem Cell Biol 39:1349–1357
Ferrara N (2009) VEGF-A: a critical regulator of blood vessel growth. Eur Cytokine Netw 20:158–163
Koch AE, Harlow LA, Haines GK, Amento EP, Unemori EN, Wong WL, Pope RM, Ferrara N (1994) Vascular endothelial growth factor. A cytokine modulating endothelial function in rheumatoid arthritis. J Immunol 152:4149–4156
Fava RA, Olsen NJ, Spencer-Green G, Yeo KT, Yeo TK, Berse B, Jackman RW, Senger DR, Dvorak HF, Brown LF (1994) Vascular permeability factor/endothelial growth factor (VPF/VEGF): accumulation and expression in human synovial fluids and rheumatoid synovial tissue. J Exp Med 180:341–346
Kikuchi K, Kubo M, Kadono T, Yazawa N, Ihn H, Tamaki K (1998) Serum concentrations of vascular endothelial growth factor in collagen diseases. Br J Dermatol 139:1049–1051
Paleolog EM, Young S, Stark AC, McCloskey RV, Feldmann M, Maini RN (1998) Modulation of angiogenic vascular endothelial growth factor by tumor necrosis factor alpha and interleukin-1 in rheumatoid arthritis. Arthritis Rheum 41:1258–1265
Ikeda M, Hosoda Y, Hirose S, Okada Y, Ikeda E (2000) Expression of vascular endothelial growth factor isoforms and their receptors Flt-1, KDR, and neuropilin-1 in synovial tissues of rheumatoid arthritis. J Pathol 191:426–433
Brouwer E, Gouw AS, Posthumus MD, van Leeuwen MA, Boerboom AL, Bijzet J, Bos R, Limburg PC, Kallenberg CG, Westra J (2009) Hypoxia inducible factor-1-alpha (HIF-1alpha) is related to both angiogenesis and inflammation in rheumatoid arthritis. Clin Exp Rheumatol 27:945–951
Lee SS, Joo YS, Kim WU, Min DJ, Min JK, Park SH, Cho CS, Kim HY (2001) Vascular endothelial growth factor levels in the serum and synovial fluid of patients with rheumatoid arthritis. Clin Exp Rheumatol 19:321–324
Giatromanolaki A, Sivridis E, Athanassou N, Zois E, Thorpe PE, Brekken RA, Gatter KC, Harris AL, Koukourakis IM, Koukourakis MI (2001) The angiogenic pathway “vascular endothelial growth factor/flk-1(KDR)-receptor” in rheumatoid arthritis and osteoarthritis. J Pathol 194:101–108
Pufe T, Petersen W, Tillmann B, Mentlein R (2001) Splice variants VEGF121 and VEGF165 of the angiogenic peptide vascular endothelial cell growth factor are expressed in the synovial tissue of patients with rheumatoid arthritis. J Rheumatol 28:1482–1485
Sone H, Sakauchi M, Takahashi A, Suzuki H, Inoue N, Iida K, Shimano H, Toyoshima H, Kawakami Y, Okuda Y, Matsuo K, Yamada N (2001) Elevated levels of vascular endothelial growth factor in the sera of patients with rheumatoid arthritis correlation with disease activity. Life Sci 69:1861–1869
Kuryliszyn-Moskal A, Klimiuk PA, Sierakowski S, Ciolkiewicz M (2006) A study on vascular endothelial growth factor and endothelin-1 in patients with extra-articular involvement of rheumatoid arthritis. Clin Rheumatol 25:314–319
Kurosaka D, Hirai K, Nishioka M, Miyamoto Y, Yoshida K, Noda K, Ukichi T, Yanagimachi M, Furuya K, Takahashi E, Kingetsu I, Fukuda K, Yamada A (2010) Clinical significance of serum levels of vascular endothelial growth factor, angiopoietin-1, and angiopoietin-2 in patients with rheumatoid arthritis. J Rheumatol 37:1121–1128
Ballara SC, Taylor PC, Reusch P, Marmé D, Feldmann M, Maini RN, Paleolog EM (2001) Raised serum vascular endothelial growth factor levels are associated with destructive change in inflammatory arthritis. Arthritis Rheum 44:2055–2064
Kurosaka D, Hirai K, Nishioka M, Miyamoto Y, Yoshida K, Takahashi E, Ukichi T, Noda K, Yanagimachi M, Furuya K, Fukuda K, Yamada A (2009) Correlation between synovial blood flow signals and serum vascular endothelial growth factor levels in patients with refractory rheumatoid arthritis. Mod Rheumatol 19:187–191
Williams RO, Paleolog E, Feldmann M (2007) Cytokine inhibitors in rheumatoid arthritis and other autoimmune diseases. Curr Opin Pharmacol 7:412–417
Lu J, Kasama T, Kobayashi K, Yoda Y, Shiozawa F, Hanyuda M, Negishi M, Ide H, Adachi M (2000) Vascular endothelial growth factor expression and regulation of murine collagen-induced arthritis. J Immunol 164:5922–5927
Thornton S, Sowders D, Aronow B, Witte DP, Brunner HI, Giannini EH, Hirsch R (2002) DNA microarray analysis reveals novel gene expression profiles in collagen-induced arthritis. Clin Immunol 105:155–168
Hermann LM, Pinkerton M, Jennings K, Yang L, Grom A, Sowders D, Kersten S, Witte DP, Hirsch R, Thornton S (2005) Angiopoietin-like-4 is a potential angiogenic mediator in arthritis. Clin Immunol 115:93–101
de Bandt M, Grossin M, Weber AJ, Chopin M, Elbim C, Pla M, Gougerot-Pocidalo MA, Gaudry M (2000) Suppression of arthritis and protection from bone destruction by treatment with TNP-470/AGM-1470 in a transgenic mouse model of rheumatoid arthritis. Arthritis Rheum 43:2056–2063
Arsenault AL, Lhotak S, Hunter WL, Banquerigo ML, Brahn E (1998) Taxol involution of collagen-induced arthritis: ultrastructural correlation with the inhibition of synovitis and neovascularization. Clin Immunol Immunopathol 86:280–289
Peacock DJ, Banquerigo ML, Brahn E (1992) Angiogenesis inhibition suppresses collagen arthritis. J Exp Med 175:1135–1138
Peacock DJ, Banquerigo ML, Brahn E (1995) A novel angiogenesis inhibitor suppresses rat adjuvant arthritis. Cell Immunol 160:178–184
Bainbridge J, Madden L, Essex D, Binks M, Malhotra R, Paleolog EM (2007) Methionine aminopeptidase-2 blockade reduces chronic collagen-induced arthritis: potential role for angiogenesis inhibition. Arthritis Res Ther 9:R127
Brahn E, Banquerigo ML, Lee JK, Park EJ, Fogler WE, Plum SM (2008) An angiogenesis inhibitor, 2-methoxyestradiol, involutes rat collagen-induced arthritis and suppresses gene expression of synovial vascular endothelial growth factor and basic fibroblast growth factor. J Rheumatol 35:2119–2128
Sone H, Kawakami Y, Sakauchi M, Nakamura Y, Takahashi A, Shimano H, Okuda Y, Segawa T, Suzuki H, Yamada N (2001) Neutralization of vascular endothelial growth factor prevents collagen-induced arthritis and ameliorates established disease in mice. Biochem Biophys Res Commun 281:562–568
Miotla J, Maciewicz R, Kendrew J, Feldmann M, Paleolog E (2000) Treatment with soluble VEGF receptor reduces disease severity in murine collagen-induced arthritis. Lab Invest 80:1195–1205
Afuwape AO, Feldmann M, Paleolog EM (2003) Adenoviral delivery of soluble VEGF receptor 1 (sFlt-1) abrogates disease activity in murine collagen-induced arthritis. Gene Ther 10:1950–1960
de Bandt M, Ben Mahdi MH, Ollivier V, Grossin M, Dupuis M, Gaudry M, Bohlen P, Lipson KE, Rice A, Wu Y, Gougerot-Pocidalo MA, Pasquier C (2003) Blockade of vascular endothelial growth factor receptor I (VEGF-RI), but not VEGF-RII, suppresses joint destruction in the K/BxN model of rheumatoid arthritis. J Immunol 171:4853–4859
Luttun A, Tjwa M, Moons L, Wu Y, Angelillo-Scherrer A, Liao F, Nagy JA, Hooper A, Priller J, De Klerck B, Compernolle V, Daci E, Bohlen P, Dewerchin M, Herbert JM, Fava R, Matthys P, Carmeliet G, Collen D, Dvorak HF, Hicklin DJ, Carmeliet P (2002) Revascularization of ischemic tissues by PlGF treatment, and inhibition of tumor angiogenesis, arthritis and atherosclerosis by anti-Flt1. Nat Med 8:831–840
Folkman J (1971) Tumor angiogenesis: therapeutic implications. N Engl J Med 285:1182–1186
Kabbinavar F, Hurwitz HI, Fehrenbacher L, Meropol NJ, Novotny WF, Lieberman G, Griffing S, Bergsland E (2003) Phase II, randomized trial comparing bevacizumab plus fluorouracil (FU)/leucovorin (LV) with FU/LV alone in patients with metastatic colorectal cancer. J Clin Oncol 21:60–65
Hurwitz H, Fehrenbacher L, Novotny W, Cartwright T, Hainsworth J, Heim W, Berlin J, Baron A, Griffing S, Holmgren E, Ferrara N, Fyfe G, Rogers B, Ross R, Kabbinavar F (2004) Bevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. N Engl J Med 350:2335–2342
Giantonio BJ, Catalano PJ, Meropol NJ, O’Dwyer PJ, Mitchell EP, Alberts SR, Schwartz MA, Benson AB (2007) Bevacizumab in Combination With Oxaliplatin, Fluorouracil, and Leucovorin (FOLFOX4) for Previously Treated Metastatic Colorectal Cancer: Results From the Eastern Cooperative Oncology Group Study E3200. J Clin Oncol 25:1539–1544
Kabbinavar FF, Schulz J, McCleod M, Patel T, Hamm JT, Hecht JR, Mass R, Perrou B, Nelson B, Novotny WF (2005) Addition of bevacizumab to bolus fluorouracil and leucovorin in first-line metastatic colorectal cancer: results of a randomized phase II trial. J Clin Oncol Official J Am Soc Clin Oncol 23:3697–3705
Llovet JM, Ricci S, Mazzaferro V, Hilgard P, Gane E, Blanc J-F, de Oliveira AC, Santoro A, Raoul J-L, Forner A, Schwartz M, Porta C, Zeuzem S, Bolondi L, Greten TF, Galle PR, Seitz J-F, Borbath I, Häussinger D, Giannaris T, Shan M, Moscovici M, Voliotis D, Bruix J (2008) Sorafenib in advanced hepatocellular carcinoma. N Engl J Med 359:378–390
Miller KD, Chap LI, Holmes FA, Cobleigh MA, Marcom PK, Fehrenbacher L, Dickler M, Overmoyer BA, Reimann JD, Sing AP, Langmuir V, Rugo HS (2005) Randomized phase III trial of capecitabine compared with bevacizumab plus capecitabine in patients with previously treated metastatic breast cancer. J Clin Oncol Official J Am Soc Clin Oncol 23:792–799
Sandler A, Gray R, Perry MC, Brahmer J, Schiller JH, Dowlati A, Lilenbaum R, Johnson DH (2006) Paclitaxel-carboplatin alone or with bevacizumab for non-small-cell lung cancer. N Engl J Med 355:2542–2550
Escudier B, Eisen T, Stadler WM, Szczylik C, Oudard S, Siebels M, Negrier S, Chevreau C, Solska E, Desai AA, Rolland F, Demkow T, Hutson TE, Gore M, Freeman S, Schwartz B, Shan M, Simantov R, Bukowski RM (2007) Sorafenib in advanced clear-cell renal-cell carcinoma. N Engl J Med 356:125–134
Chen HX, Cleck JN (2009) Adverse effects of anticancer agents that target the VEGF pathway. Nature Rev Clin Oncol 6:465–477
Wu S, Kim C, Baer L, Zhu X (2010) Bevacizumab increases risk for severe proteinuria in cancer patients. J Am Soc Nephrol 21:1381–1389
George BA, Zhou XJ, Toto R (2007) Nephrotic syndrome after bevacizumab: case report and literature review. Am J Kidney Dis 49:e23–e29
Scappaticci FA, Skillings JR, Holden SN, Gerber H-P, Miller K, Kabbinavar F, Bergsland E, Ngai J, Holmgren E, Wang J, Hurwitz H (2007) Arterial thromboembolic events in patients with metastatic carcinoma treated with chemotherapy and bevacizumab. J Natl Cancer Inst 99:1232–1239
Schutz FA, Je Y, Azzi GR, Nguyen PL, Choueiri TK (2010) Bevacizumab increases the risk of arterial ischemia: a large study in cancer patients with a focus on different subgroup outcomes. Ann Oncol. doi:10.1093/annonc/mdq587
Nalluri SR, Chu D, Keresztes R, Zhu X, Wu S (2008) Risk of venous thromboembolism with the angiogenesis inhibitor bevacizumab in cancer patients. J Am Med Assoc 300:2277–2285
Hapani S, Chu D, Wu S (2009) Risk of gastrointestinal perforation in patients with cancer treated with bevacizumab: a meta-analysis. Lancet Oncol 10:559–568
Hochster HS, Hart LL, Ramanathan RK, Childs BH, Hainsworth JD, Cohn AL, Wong L, Fehrenbacher L, Abubakr Y, Saif MW, Schwartzberg L, Hedrick E (2008) Safety and efficacy of oxaliplatin and fluoropyrimidine regimens with or without bevacizumab as first-line treatment of metastatic colorectal cancer: results of the TREE study. J Clin Oncol Official J Am Soc Clin Oncol 26:3523–3529
Allegra CJ, Yothers G, O’Connell MJ, Sharif S, Colangelo LH, Lopa SH, Petrelli NJ, Goldberg RM, Atkins JN, Seay TE, Fehrenbacher L, O’Reilly S, Chu L, Azar CA, Wolmark N (2009) Initial safety report of NSABP C-08: a randomized phase III study of modified FOLFOX6 with or without bevacizumab for the adjuvant treatment of patients with Stage II or III colon cancer. J Clin Oncol 27:3385–3390
August DA, Serrano D, Poplin E (2008) “Spontaneous”, delayed colon and rectal anastomotic complications associated with bevacizumab therapy. J Surg Oncol 97:180–185
Bège T, Lelong B, Viret F, Turrini O, Guiramand J, Topart D, Moureau-Zabotto L, Giovannini M, Gonçalves A, Delpero JR (2009) Bevacizumab-related surgical site complication despite primary tumor resection in colorectal cancer patients. Ann Surg Oncol 16:856–860
FDA (2010) FDA begins process to remove breast cancer indication from Avastin label. United States Food and Drug Administration; [updated 2010; cited 2010 16th December]. Available from http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm237172.htm
NICE (2010) Colorectal cancer (metastatic)—bevacizumab. National Institute for Health and Clinical Excellence; [updated 2010; cited]. Available from http://www.nice.org.uk/guidance/index.jsp?action=byID&o=13291
Sano H, Forough R, Maier JA, Case JP, Jackson A, Engleka K, Maciag T, Wilder RL (1990) Detection of high levels of heparin binding growth factor-1 (acidic fibroblast growth factor) in inflammatory arthritic joints. J Cell Biol 110:1417–1426
Sano H, Engleka K, Mathern P, Hla T, Crofford LJ, Remmers EF, Jelsema CL, Goldmuntz E, Maciag T, Wilder RL (1993) Coexpression of phosphotyrosine-containing proteins, platelet-derived growth factor-B, and fibroblast growth factor-1 in situ in synovial tissues of patients with rheumatoid arthritis and Lewis rats with adjuvant or streptococcal cell wall arthritis. J Clin Invest 91:553–565
Remmers EF, Sano H, Lafyatis R, Case JP, Kumkumian GK, Hla T, Maciag T, Wilder RL (1991) Production of platelet derived growth factor B chain (PDGF-B/c-sis) mRNA and immunoreactive PDGF B-like polypeptide by rheumatoid synovium: coexpression with heparin binding acidic fibroblast growth factor-1. J Rheumatol 18:7–13
Koch AE, Halloran MM, Hosaka S, Shah MR, Haskell CJ, Baker SK, Panos RJ, Haines GK, Bennett GL, Pope RM, Ferrara N (1996) Hepatocyte growth factor. A cytokine mediating endothelial migration in inflammatory arthritis. Arthritis Rheum 39:1566–1575
Scott BB, Zaratin PF, Colombo A, Hansbury MJ, Winkler JD, Jackson JR (2002) Constitutive expression of angiopoietin-1 and -2 and modulation of their expression by inflammatory cytokines in rheumatoid arthritis synovial fibroblasts. J Rheumatol 29:230–239
Gravallese EM, Pettit AR, Lee R, Madore R, Manning C, Tsay A, Gaspar J, Goldring MB, Goldring SR, Oettgen P (2003) Angiopoietin-1 is expressed in the synovium of patients with rheumatoid arthritis and is induced by tumour necrosis factor alpha. Ann Rheum Dis 62:100–107
DeBusk LM, Chen Y, Nishishita T, Chen J, Thomas JW, Lin PC (2003) Tie2 receptor tyrosine kinase, a major mediator of tumor necrosis factor alpha-induced angiogenesis in rheumatoid arthritis. Arthritis Rheum 48:2461–2471
Shahrara S, Volin MV, Connors MA, Haines GK, Koch AE (2002) Differential expression of the angiogenic Tie receptor family in arthritic and normal synovial tissue. Arthritis Res 4:201–208
Uchida T, Nakashima M, Hirota Y, Miyazaki Y, Tsukazaki T, Shindo H (2000) Immunohistochemical localisation of protein tyrosine kinase receptors Tie-1 and Tie-2 in synovial tissue of rheumatoid arthritis: correlation with angiogenesis and synovial proliferation. Ann Rheum Dis 59:607–614
Chen Y, Donnelly E, Kobayashi H, Debusk LM, Lin PC (2005) Gene therapy targeting the Tie2 function ameliorates collagen-induced arthritis and protects against bone destruction. Arthritis Rheum 52:1585–1594
Jin P, Zhang J, Sumariwalla PF, Ni I, Jorgensen B, Crawford D, Phillips S, Feldmann M, Shepard HM, Paleolog EM (2008) Novel splice variants derived from the receptor tyrosine kinase superfamily are potential therapeutics for rheumatoid arthritis. Arthritis Res Ther 10:R73
Malik NM, Jin P, Raatz Y, Sumariwalla PF, Kiriakidis S, Shepard M, Feldmann M, Paleolog EM (2010) Regulation of the Angiopoietin-Tie ligand-receptor system with a novel splice variant of Tie1 reduces the severity of murine arthritis. Rheumatology 49:1828–1839
Yarden Y (2001) The EGFR family and its ligands in human cancer. Signalling mechanisms and therapeutic opportunities. Eur J Cancer 37(Suppl 4):S3–S8
Yarden Y, Sliwkowski MX (2001) Untangling the ErbB signalling network. Nat Rev Mol Cell Biol 2:127–137
Huang Z, Brdlik C, Jin P, Shepard HM (2009) A pan-HER approach for cancer therapy: background, current status and future development. Expert Opin Biol Ther 9:97–110
Scaltriti M, Baselga J (2006) The epidermal growth factor receptor pathway: a model for targeted therapy. Clin Cancer Res Official J Am Assoc Cancer Res 12:5268–5272
Spano JP, Lagorce C, Atlan D, Milano G, Domont J, Benamouzig R, Attar A, Benichou J, Martin A, Morere JF, Raphael M, Penault-Llorca F, Breau JL, Fagard R, Khayat D, Wind P (2005) Impact of EGFR expression on colorectal cancer patient prognosis and survival. Ann Oncol 16:102–108
Zlobec I, Vuong T, Hayashi S, Haegert D, Tornillo L, Terracciano L, Lugli A, Jass J (2007) A simple and reproducible scoring system for EGFR in colorectal cancer: application to prognosis and prediction of response to preoperative brachytherapy. Br J Cancer 96:793–800
Shiozawa S, Shiozawa K, Tanaka Y, Morimoto I, Uchihashi M, Fujita T, Hirohata K, Hirata Y, Imura S (1989) Human epidermal growth factor for the stratification of synovial lining layer and neovascularisation in rheumatoid arthritis. Ann Rheum Dis 48:820–828
Di Cosimo S, Baselga J (2008) Targeted therapies in breast cancer: where are we now? Eur J Cancer 44:2781–2790
Johnston JB, Navaratnam S, Pitz MW, Maniate JM, Wiechec E, Baust H, Gingerich J, Skliris GP, Murphy LC, Los M (2006) Targeting the EGFR pathway for cancer therapy. Curr Med Chem 13:3483–3492
Hallbeck AL, Walz TM, Briheim K, Wasteson A (2005) TGF-alpha and ErbB2 production in synovial joint tissue: increased expression in arthritic joints. Scand J Rheumatol 34:204–211
Satoh K, Kikuchi S, Sekimata M, Kabuyama Y, Homma MK, Homma Y (2001) Involvement of ErbB-2 in rheumatoid synovial cell growth. Arthritis Rheum 44:260–265
Schreiber AB, Winkler ME, Derynck R (1986) Transforming growth factor-alpha: a more potent angiogenic mediator than epidermal growth factor. Science 232:1250–1253
Yamane S, Ishida S, Hanamoto Y, Kumagai K, Masuda R, Tanaka K, Shiobara N, Yamane N, Mori T, Juji T, Fukui N, Itoh T, Ochi T, Suzuki R (2008) Proinflammatory role of amphiregulin, an epidermal growth factor family member whose expression is augmented in rheumatoid arthritis patients. J Inflamm (Lond) 5:5
Sumariwalla PF, Jin P, Zhang J, Ni I, Crawford D, Shepard HM, Paleolog EM, Feldmann M (2008) Antagonism of the human epidermal growth factor receptor family controls disease severity in murine collagen-induced arthritis. Arthritis Rheum 58:3071–3080
Semenza GL (2009) Regulation of oxygen homeostasis by hypoxia-inducible factor 1. Physiology (Bethesda) 24:97–106
Wang GL, Jiang BH, Rue EA, Semenza GL (1995) Hypoxia-inducible factor 1 is a basic-helix-loop-helix-PAS heterodimer regulated by cellular O2 tension. Proc Natl Acad Sci USA 92:5510–5514
Maxwell PH, Wiesener MS, Chang GW, Clifford SC, Vaux EC, Cockman ME, Wykoff CC, Pugh CW, Maher ER, Ratcliffe PJ (1999) The tumour suppressor protein VHL targets hypoxia-inducible factors for oxygen-dependent proteolysis. Nature 399:271–275
Sivakumar B, Akhavani MA, Winlove CP, Taylor PC, Paleolog EM, Kang N (2008) Synovial hypoxia as a cause of tendon rupture in rheumatoid arthritis. J Hand Surg [Am] 33:49–58
Lund-Olesen K (1970) Oxygen tension in synovial fluids. Arthritis Rheum 13:769–776
Treuhaft PS, McCarty D (1971) Synovial fluid pH, lactate, oxygen and carbon dioxide partial pressure in various joint diseases. Arthritis Rheum 14:475–484
Blake DR, Merry P, Unsworth J, Kidd BL, Outhwaite JM, Ballard R, Morris CJ, Gray L, Lunec J (1989) Hypoxic-reperfusion injury in the inflamed human joint. Lancet 1:289–293
Naughton D, Whelan M, Smith EC, Williams R, Blake DR, Grootveld M (1993) An investigation of the abnormal metabolic status of synovial fluid from patients with rheumatoid arthritis by high field proton nuclear magnetic resonance spectroscopy. FEBS Lett 317:135–138
Lee YA, Kim JY, Hong SJ, Lee SH, Yoo MC, Kim KS, Yang HI (2007) Synovial proliferation differentially affects hypoxia in the joint cavities of rheumatoid arthritis and osteoarthritis patients. Clin Rheumatol 26:2023–2029
Naughton DP (2003) Hypoxia-induced upregulation of the glycolytic enzyme glucose-6-phosphate isomerase perpetuates rheumatoid arthritis. Med Hypotheses 60:332–334
Hitchon CA, El-Gabalawy HS, Bezabeh T (2009) Characterization of synovial tissue from arthritis patients: a proton magnetic resonance spectroscopic investigation. Rheumatol Int 29:1205–1211
Biniecka M, Kennedy A, Fearon U, Ng CT, Veale DJ, O’Sullivan JN (2010) Oxidative damage in synovial tissue is associated with in vivo hypoxic status in the arthritic joint. Ann Rheum Dis 69:1172–1178
Ng CT, Biniecka M, Kennedy A, McCormick J, Fitzgerald O, Bresnihan B, Buggy D, Taylor CT, O’Sullivan J, Fearon U, Veale DJ (2010) Synovial tissue hypoxia and inflammation in vivo. Ann Rheum Dis 69:1389–1395
Richman AI, Su EY, Ho G Jr (1981) Reciprocal relationship of synovial fluid volume and oxygen tension. Arthritis Rheum 24:701–705
Hitchon C, Wong K, Ma G, Reed J, Lyttle D, El-Gabalawy H (2002) Hypoxia-induced production of stromal cell-derived factor 1 (CXCL12) and vascular endothelial growth factor by synovial fibroblasts. Arthritis Rheum 46:2587–2597
Hollander AP, Corke KP, Freemont AJ, Lewis CE (2001) Expression of hypoxia-inducible factor 1alpha by macrophages in the rheumatoid synovium: implications for targeting of therapeutic genes to the inflamed joint. Arthritis Rheum 44:1540–1544
Giatromanolaki A, Sivridis E, Maltezos E, Athanassou N, Papazoglou D, Gatter KC, Harris AL, Koukourakis MI (2003) Upregulated hypoxia inducible factor-1alpha and -2alpha pathway in rheumatoid arthritis and osteoarthritis. Arthritis Res Ther 5:R193–R201
Westra J, Molema G, Kallenberg CG (2010) Hypoxia-inducible factor-1 as regulator of angiogenesis in rheumatoid arthritis—therapeutic implications. Curr Med Chem 17:254–263
Peters CL, Morris CJ, Mapp PI, Blake DR, Lewis CE, Winrow VR (2004) The transcription factors hypoxia-inducible factor 1alpha and Ets-1 colocalize in the hypoxic synovium of inflamed joints in adjuvant-induced arthritis. Arthritis Rheum 50:291–296
Kim HL, Cho YS, Choi H, Chun YS, Lee ZH, Park JW (2009) Hypoxia-inducible factor 1alpha is deregulated by the serum of rats with adjuvant-induced arthritis. Biochem Biophys Res Commun 378:123–128
Akhavani MA, Madden L, Buysschaert I, Sivakumar B, Kang N, Paleolog EM (2009) Hypoxia upregulates angiogenesis and synovial cell migration in rheumatoid arthritis. Arthritis Res Ther 11:R64
Ahn JK, Koh EM, Cha HS, Lee YS, Kim J, Bae EK, Ahn KS (2008) Role of hypoxia-inducible factor-1alpha in hypoxia-induced expressions of IL-8, MMP-1 and MMP-3 in rheumatoid fibroblast-like synoviocytes. Rheumatology (Oxford) 47:834–839
Matsumoto K, Imagawa S, Obara N, Suzuki N, Takahashi S, Nagasawa T, Yamamoto M (2006) 2-Oxoglutarate downregulates expression of vascular endothelial growth factor and erythropoietin through decreasing hypoxia-inducible factor-1alpha and inhibits angiogenesis. J Cell Physiol 209:333–340
Matsumoto K, Obara N, Ema M, Horie M, Naka A, Takahashi S, Imagawa S (2009) Antitumor effects of 2-oxoglutarate through inhibition of angiogenesis in a murine tumor model. Cancer Sci 100:1639–1647
Yeo EJ, Chun YS, Cho YS, Kim J, Lee JC, Kim MS, Park JW (2003) YC-1: a potential anticancer drug targeting hypoxia-inducible factor 1. J Natl Cancer Inst 95:516–525
Manabe H, Nasu Y, Komiyama T, Furumatsu T, Kitamura A, Miyazawa S, Ninomiya Y, Ozaki T, Asahara H, Nishida K (2008) Inhibition of histone deacetylase down-regulates the expression of hypoxia-induced vascular endothelial growth factor by rheumatoid synovial fibroblasts. Inflamm Res 57:4–10
Shankar J, Thippegowda PB, Kanum SA (2009) Inhibition of HIF-1alpha activity by BP-1 ameliorates adjuvant induced arthritis in rats. Biochem Biophys Res Commun 387:223–228
Paleolog EM, Miotla JM (1998) Angiogenesis in arthritis: role in disease pathogenesis and as a potential therapeutic target. Angiogenesis 2:295–307
Khong TL, Larsen H, Raatz Y, Paleolog E (2007) Angiogenesis as a therapeutic target in arthritis: learning the lessons of the colorectal cancer experience. Angiogenesis 10:243–258
Ferrara N, Carver-Moore K, Chen H, Dowd M, Lu L, O’Shea KS, Powell-Braxton L, Hillan KJ, Moore MW (1996) Heterozygous embryonic lethality induced by targeted inactivation of the VEGF gene. Nature 380:439–442
Gonzalez-Gay MA, Gonzalez-Juanatey C, Martin J (2005) Rheumatoid arthritis: a disease associated with accelerated atherogenesis. Semin Arthritis Rheum 35:8–17
Kaplan MJ (2006) Cardiovascular disease in rheumatoid arthritis. Curr Opin Rheumatol 18:289–297
Van Doornum S, Brand C, King B, Sundararajan V (2006) Increased case fatality rates following a first acute cardiovascular event in patients with rheumatoid arthritis. Arthritis Rheum 54:2061–2068
Sihvonen S, Korpela M, Laippala P, Mustonen J, Pasternack A (2004) Death rates and causes of death in patients with rheumatoid arthritis: a population-based study. Scand J Rheumatol 33:221–227
Nadareishvili Z, Michaud K, Hallenbeck JM, Wolfe F (2008) Cardiovascular, rheumatologic, and pharmacologic predictors of stroke in patients with rheumatoid arthritis: a nested, case-control study. Arthritis Rheum 59:1090–1096
Solomon DH, Karlson EW, Rimm EB, Cannuscio CC, Mandl LA, Manson JE, Stampfer MJ, Curhan GC (2003) Cardiovascular morbidity and mortality in women diagnosed with rheumatoid arthritis. Circulation 107:1303–1307
Kremers HM, Crowson CS, Therneau TM, Roger VL, Gabriel SE (2008) High ten-year risk of cardiovascular disease in newly diagnosed rheumatoid arthritis patients: a population-based cohort study. Arthritis Rheum 58:2268–2274
Solomon DH, Goodson NJ, Katz JN, Weinblatt ME, Avorn J, Setoguchi S, Canning C, Schneeweiss S (2006) Patterns of cardiovascular risk in rheumatoid arthritis. Ann Rheum Dis 65:1608–1612
Soltesz P, Der H, Kerekes G, Szodoray P, Szucs G, Danko K, Shoenfeld Y, Szegedi G, Szekanecz Z (2009) A comparative study of arterial stiffness, flow-mediated vasodilation of the brachial artery, and the thickness of the carotid artery intima-media in patients with systemic autoimmune diseases. Clin Rheumatol 28:655–662
Warnecke C, Weidemann A, Volke M, Schietke R, Wu X, Knaup KX, Hackenbeck T, Bernhardt W, Willam C, Eckardt KU, Wiesener MS (2008) The specific contribution of hypoxia-inducible factor-2alpha to hypoxic gene expression in vitro is limited and modulated by cell type-specific and exogenous factors. Exp Cell Res 314:2016–2027
Carroll VA, Ashcroft M (2006) Role of hypoxia-inducible factor (HIF)-1alpha versus HIF-2alpha in the regulation of HIF target genes in response to hypoxia, insulin-like growth factor-I, or loss of von Hippel-Lindau function: implications for targeting the HIF pathway. Cancer Res 66:6264–6270
Sowter HM, Raval RR, Moore JW, Ratcliffe PJ, Harris AL (2003) Predominant role of hypoxia-inducible transcription factor (Hif)-1alpha versus Hif-2alpha in regulation of the transcriptional response to hypoxia. Cancer Res 63:6130–6134
Raval RR, Lau KW, Tran MG, Sowter HM, Mandriota SJ, Li JL, Pugh CW, Maxwell PH, Harris AL, Ratcliffe PJ (2005) Contrasting properties of hypoxia-inducible factor 1 (HIF-1) and HIF-2 in von Hippel-Lindau-associated renal cell carcinoma. Mol Cell Biol 25:5675–5686
Bongartz T, Sutton AJ, Sweeting MJ, Buchan I, Matteson EL, Montori V (2006) Anti-TNF antibody therapy in rheumatoid arthritis and the risk of serious infections and malignancies: systematic review and meta-analysis of rare harmful effects in randomized controlled trials. JAMA 295:2275–2285
Bongartz T, Warren FC, Mines D, Matteson EL, Abrams KR, Sutton AJ (2009) Etanercept therapy in rheumatoid arthritis and the risk of malignancies: a systematic review and individual patient data meta-analysis of randomised controlled trials. Ann Rheum Dis 68:1177–1183
Furst DE (2008) The risk of infections with biologic therapies for rheumatoid arthritis. Semin Arthritis Rheum 39:327–346
Tubach F, Salmon D, Ravaud P, Allanore Y, Goupille P, Breban M, Pallot-Prades B, Pouplin S, Sacchi A, Chichemanian RM, Bretagne S, Emilie D, Lemann M, Lorthololary O, Mariette X (2009) Risk of tuberculosis is higher with anti-tumor necrosis factor monoclonal antibody therapy than with soluble tumor necrosis factor receptor therapy: the three-year prospective french research axed on tolerance of biotherapies registry. Arthritis Rheum 60:1884–1894
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Thairu, N., Kiriakidis, S., Dawson, P. et al. Angiogenesis as a therapeutic target in arthritis in 2011: learning the lessons of the colorectal cancer experience. Angiogenesis 14, 223–234 (2011). https://doi.org/10.1007/s10456-011-9208-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10456-011-9208-2