Abstract
Understanding spinal kinematics is essential, not only for the comprehension and diagnosis of spinal diseases, but also for improving modern tools and software. The sheer volume and complexity of now available information can be overwhelming. We aimed to distil it into a form that facilitates comparison among diverse studies addressing spinal kinematics under healthy and degenerative conditions. We specifically aimed to define a baseline definition of the spectrum of normal spinal kinematics that in turn allows a comparable definition of kinematics of the degenerative lumbar spine. The considered data was obtained by a systematic MEDLINE search including studies on angular/translational segmental motion contribution, range of motion, coupling and center of rotation. As for degenerative conditions, we collected publications on disc degeneration, facet joint osteoarthritis, facet joint tropism, spondylolisthesis, ligament degeneration and paraspinal muscle degeneration. While we could demonstrate repeating motion patterns for some topics, agreement in other fields is limited due to methodological variances and small sample sizes, particularly in publications with highly accurate but complex techniques. Besides, the high frequency of concurrent degenerative processes complicates the association between diseases and subsequent kinematical changes. Despite several substantial gaps, we stand at the precipice of technological breakthroughs that can power future large-scale studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Kinematics of the lumbar spine is a matter of great interest in the field of spinal orthopedics and reason for countless investigations during the last decades. A profound understanding is essential for not only the comprehension and diagnosis of numerous spine diseases, but also for the improvement of tools, such as motion sustaining products and prostheses. Modern implants usually aim at restoring healthy kinematics, which of course requires precise knowledge of these complex relations. The same is true for multibody dynamics software using kinematical data as input for simulations.
Discussing the kinematics of the “healthy” spine inevitably raises the question of its definition and whether it is possible to clearly distinct a healthy spine from a pathologically behaving exemplar by just studying its motion pattern. This could serve as a tool for diagnostics and disease classification. Several approaches in this direction have been taken, for example in order to diagnose spondylolisthesis (SL) by evaluating segmental instability62,104 or to assess the degree of disc degeneration (DD) by measuring the shift of the center of rotation (COR).37,38,103,119 Multiple authors tried to come up with a definition of spinal instability. “Damage at one of the three spinal columns”,40,42 hyper-translational and hyper-angular motion14,48,52,83,126,127,–128 or even a disordered COR22,104,119 were held responsible for a spinal imbalance. However, a useful classification system could not yet be established in the clinical practice. Besides, the applied methods for studying healthy as well as pathological motion patterns of the spine are extremely diverse and range from simple static end-position image comparison to sophisticated techniques like 3D motion reconstructions. Moreover, test procedures as well as experiment parameters are manifold. This adds up to an immense diversity of outcomes within literature, often even contradicting. Some of the widespread, fundamental principles in the field are therefore based on single publications or even originate from in vitro tests, and even though more recent publications indicate contradictory results, these principles are not discarded.
Driven by the lack of clarity in this field, we attempt to clear the fog as far as possible by providing an extensive overview on published literature in the field of spinal kinematics under healthy and degenerative conditions. We further try to find explanations for contradictory results and point out gaps in literature, in order to inspire and motivate research in these fields. In addition, this review shall serve as a reference and foundation for comparisons with any kind of existing or future results. Literature has grown substantially since 1977, when White and Panjabi published a first review on the basics of spinal kinematics.140 Based on their work,140,141 we analysed the literature on the following topics: angular segmental contribution, translational segmental contribution, maximal range of motion (ROM), coupling, COR and phase lag (PL). In addition, we summarized publications on spinal kinematics in DD, facet joint osteoarthritis (FJOA), facet joint tropism (FJT), SL, ligament degeneration (LD) and paraspinal muscle degeneration (PMD). Since most pathologies show the highest prevalence in the lumber spine, we focused on this lower section of the spine.
Materials and Methods
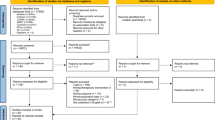
MEDLINE was searched with predefined keywords for each topic individually, leading to 2992 angular/translational segmental motion contribution (Fig. 12), 2992 coupling (Fig. 14), 2992 maximal ROM (Fig. 13), 1054 COR (Fig. 15) and 2992 PL (Fig. 16) hits. Similarly, 763 DD: mechanical stiffness (Fig. 17), 2688 DD: ROM (Fig. 18), 397 FJOA (Fig. 19), 38 FJT (Fig. 20), 283 SL (Fig. 21), 119 LD (Fig. 22) and 157 PMD (Fig. 23) publications were found for our section on pathologies. These results were then narrowed with inclusion and exclusion criteria and supplemented with a reference search. All papers from 1970 to 2016 were included. Cadaver studies were excluded, since they neglect neuromuscular interaction, which is one of the most essential components defining spinal in vivo behavior. However, as indicated there, they were included in the section on COR since no in vivo studies were found for kinematical behavior during lateral bending (LB) and axial rotation (AR).
Eventually, this resulted to a final selection of 36 angular/translational segmental motion contribution (Fig. 12; Table 1), 9 coupling (Fig. 14; Table 3), 11 maximal ROM (Fig. 13; Table 2), 15 COR (Fig. 15; Table 4) and 9 PL (Fig. 16; Table 5) publications. 9 DD: mechanical stiffness (Fig. 17; Table 6), 13 DD: ROM (Fig. 18; Tables 7; 8), 4 FJOA (Fig. 19; Table 9), 1 FJT (Fig. 20; Table 10), 17 SL (Fig. 21; Table 11), 3 LD (Fig. 22; Table 12) and 1 PMD (Fig. 23; Table 13) studies were selected for the part on pathologies. A detailed description of the applied search strategy and precise literature overview is provided in the Appendix.
Results of the final literature selection were brought into a comparable form. All results dealing with segmental contribution were converted into percentages, relative to the overall motion from L1 to S1. When data was missing for certain segmental levels, an average value from all available percental values on that level was taken and visualized with a dashed line. Results that were separated into groups according to age, sex or other factors were averaged. For left and right LB and AR pooled values were used. Additionally, statistical error propagation was considered when pooling standard deviation values.26
Values and plots in the sections on pathologies are normalized to values measured under healthy conditions, in order to allow comparisons.
Healthy Conditions
The lumbar spine is an essential contributor for bending and twisting movements during daily activities. Besides, lumbar joints are also exposed to high loads, leading to increased susceptibility for many degenerative diseases, such as DD or FJOA.114 On these grounds, the most caudal section of the spine is object of numerous investigations and in focus of the spinal research.
As previously mentioned, methodical strategies are various (methodologies are listed in the Appendix), many parameters have to be defined. While load bearing5 does not seem to influence the kinematic and movement direction (forward vs. backward flexion) has an only minor effect,3 movement execution (passive vs. active)24 significantly alters the outcome. Besides, experimental factors like movement velocities (arbitrary vs. prescribed) and ROM (restricted vs. the maximum possible) and body posture need to be investigated as potential influencing factors.
Aside from experimental parameters, patient populations are considerably different amongst the authors. Age seems to have an only minor effect and only age groups above 50 years seem to have an altered kinematics.48,143 Gender23,143 and body weight48 was shown to be inconsequential for motion patterns.
Segmental Motion Contribution
Angular
The lumbar spine covers substantial ROMs during normal daily activities. The overall movement, which will be referred to as 100%, is the sum of smaller movements of all the segments from L1 to S1. The contribution of these segments to the overall movement however varies considerably and depends on the nature of the performed movement.
Angular motion contribution for flexion/extension (FE), LB and AR is discussed in the following, defined as the angular, relative contribution of one segment to the overall movement of the lumbar spine (L1 to S1).
It is derived from calculating the difference of the intervertebral angle between two or more positional frames. In 2D studies (planar X-ray, video fluoroscopy, etc.), the intervertebral angle is measured between the lower endplate of the supraadjacent vertebrae and the upper endplate of the subjacent vertebrae. In 3D, the relative rotation of two vertebras is determined by calculating the rotational matrix that brings a vertebra from one into the other position.
Flexion/Extension
Analyzing spinal movements in the sagittal plane (neutral to flexed) has yielded two major contribution patterns in literature. A cranio-caudally decreasing70,71,127,132,142,143 and a cranio-caudally increasing contribution pattern3,7,56,83,100 with a slight drop at the L5–S1 segment (Fig. 1a).
Angular contribution of the segments. (a) Flexion, (b) extension, (c) lateral bending, and (d) axial rotation. Dashed lines are used when the values for certain levels were not available and an average value was used. Shaded areas indicate a classification according to patterns that are further discussed in the main text. Negative values in (d) represent counter-rotating movement. Complementary to the content of the main text, the studies which used pure biplanar video-fluoroscopic are indicated with (VF) in the legend of plot (a).
These two patterns seem to be completely conflicting at first sight. However, according to our understanding, there are at least two possible explanations:
- Angular Contribution is ROM Dependent All studies printed in blue (decreasing pattern) performed their experiments with a limited ROM of either 35,132 4070,142,143 or 45 degrees of flexion.71 Takayanagi et al.127 did not limit the ROM, they however performed their experiments in a sitting position, which automatically limits the movement. In contrast, all experiments printed in green (increasing pattern) were performed with an unlimited magnitude of flexion.
This finding implies that the angular contribution could be ROM dependent, which is in line with Miyasaka et al.83 They investigated ROM dependent segmental contribution in 90 subjects and documented a higher contribution of the cranial segments at the initial stage of flexion and the typical L4–L5 peak pattern at the maximal magnitude.
However, Aiyangar7 and Ahmadi3 (which both found an increasing pattern with a drop at L5–S1) show their data over the complete ROM from neutral position to the maximal flexion, and in addition some stages in between. In both studies, no difference in contribution patterns between the intermediate stages and the end of the movement could be observed.
- Posture Most studies printed in blue (decreasing pattern) used pure video-fluoroscopic (VF) experiments,70,71,132,142,143 either uni- or biplanar. In contrast, most other studies (increasing pattern) used different experimental techniques (except Ahmadi3). In order to place hands and arms outside of the continuously recorded frame, subjects are usually asked to cross their hands behind their head during videofluoroscopy, which will likely influence the motion pattern. Crawford and Jull19 showed a 50% reduced thoracic extension during bilateral arm elevation. A similar effect can be expected for the lumbar spine. An additional explanation is that the initial (neutral) position is different when arms are elevated (hollow back).
We again detected two patterns for sagittal extension (neutral to extended position): one suggesting roughly uniform contribution (green)66,143 and the other with high contribution of the cranial and caudal segments and a drop at the intermediated levels (blue)56,70,83,100,142 (Fig. 1b). Importantly, Kulig et al.66 (uniform pattern) put their subjects in a prone position and extension was achieved by actively pushing the trunk off the ground. This certainly impacts spinal kinematics. After exclusion of this study, the majority of data supports the parabolic pattern during sagittal extension. A direct ROM dependency as it is assumed for inclination does not seem to exist for extension, a finding that is in line with Miyasaka.83
Lateral Bending
Contribution patterns for LB are relatively consistent among the authors,23,100,112 with the exception of Li et al.71 (Fig. 1c). Otherwise, the findings indicate a contribution increase from L1 to L3, with a peak at the L2–L3 level and a monotonical decrease from L3 to S1 (Fig. 5b). Interestingly, Simon125 showed a similar distribution for the gap between the cartilage endplates of the facet joints. We accordingly presume that LB is primarily limited by the ROM of the facet joints.
Axial Rotation
For AR, again, two patterns occur depending on the ROM (Fig. 1d). Blankenbaker13 and Haughton46 let their subjects rotate from a neutral position to a limited ROM of only 8° (green, increasing pattern). Studies showing a uniform pattern (blue) measured at either 45°31 or 50°,86,87 or even at the maximally possible torsion.71,80,100,112,123 Taken together, this implies that the lower segments mainly perform the initial phase of AR whereas participation of each level is very similar for larger torsions.
Interestingly, facet joint orientation is also parabolically distributing99: the joints of the inferior and superior lumbar segments are more coronally aligned than the joints of the intermediate ones. Coronal alignment, as opposed to more sagittal alignment, is less restricting for AR. Distributions of joint orientation and gap width therefore cause opposing impacts on the ROM: alignment of the joints favors movement in the inferior and superior segments, whereas the increased gap widths of the intermediate segments, as described above, facilitate motion of the levels in between. This could explain the approximately flat curve of the segment contribution during AR.
Translational
Translational contribution is defined as the percental translational movement of a vertebra, in relation to the sum of all lumbar translations. It is measured in anterior–posterior direction for FE and AR, in left–right direction for LB.
In 2D experiments, segmental translation is measured as the difference in horizontal (meaning in direction of the superior endplate of the subadjacent vertebra) distance between the posteroinferior corner of the supraadjacent vertebra and the posterosuperior corner of the subjacent vertebra. In 3D experiments, translation is defined as the motion of the cranial vertebral coordinate system origin (center of vertebra) in the caudal vertebral coordinate system. Therefore, 2D and 3D values are not exactly identical; they will however yield similar results.
Flexion/Extension
Data for translational contribution can be grouped in two motion patterns very similar to the patterns for angular contribution during flexion (Fig. 2a). With the exception of Li et al.,71 the studies either show a monotonically descending curve (blue)127,132 or a slightly ascending graph with a drop at L5–S1 (green).3,7,56 Only one study could be found for extension (Fig. 2b).56
Translational contribution of the segments. (a) Flexion, (b) extension, (c) lateral bending, and (d) axial rotation. Dashed lines are used when the values for certain levels were not available and an average value was used. Shaded areas indicate a classification according to patterns that are further discussed in the main text.
Interestingly, this correlation between angular and transitional contribution in the sagittal plane indicates that intervertebral discs are simultaneously exposed to high angular deflections as well as anteroposterior loads. Such double loads significantly intensify the stress at highly contributing levels (e.g. L4–L5) and might be the reason for the higher prevalence of degenerative changes at these segments.114
Lateral Bending/Axial Rotation
Literature for translational contribution in LB is scarce.23,71 However, some similarity to the pattern for angular contribution (Fig. 1c) can be seen (Fig. 2c). This is not true for AR, showing a cranio-caudally decreasing contribution pattern for translation (Fig. 2d).71,86,87
Maximal Range of Motion
Hayes et al. first published values for lumbar ROM in 1989, and their results are still used as reference values today.48 However, much research has been done in the meantime. For this review, we only considered studies performing end-to-end movements (meaning the maximal possible movement from flexion to extension, from left to right bending and from left to right twisting) in order to retrieve maximal values for the segmental ROM. Results are shown in Fig. 3, illustrating only moderate agreement between different authors.14,23,29,48,71,80,100,112,123,128
Maximal angular ROM for each lumbar segment. (a) Flexion/extension, (b) lateral bending, and (c) axial rotation. Means are weighted averages (in relation to the number of subjects). Error bars represent the standard deviation (error information was not available for all the shown data from Hayes et al.48 and Mimura et al.,80 as well as for the ROM measured by Dvorak et al.23 during lateral bending in the segment L5–S1).
Literature for maximal translational movement is scarce. Again, measuring methods are considerably different and do not allow comparisons between different publications.
Coupled Motion
As already observed in 1966,110 spinal motion around one axis is always accompanied by coupled translational and rotational components around or along other axes. This phenomenon is caused by our spine, whose curvy shape prohibits pure uniaxial motion.
Literature on coupling motion reports very conflicting results, mainly due to differing definitions. For example, it is essential whether rotation is measured around an inertial or a local coordinate system, since coupled motion is rotation that appears during the spinal rotation in primary direction. Besides, since the results usually arise from newer methods with spatial vertebrae tracking, they strongly depend on the convention of rotation order (e.g. Euler formulation, Roll-Nick-Gier, etc.). This information is usually lacking and comparisons are difficult.
Nevertheless, Fig. 4 gives an overview of the published data in literature.31,71,86,87,112,123,145 Interestingly, coupled motion during FE (Fig. 4a) ranges up to 60% (considering the very large values from Li71 as outliers), even though the centers of mass in the coronal plane are approximately aligned above each other and one would therefore not expect to find any substantial motion around other axes.
Coupled motion [as ratio (%) of the maximal ROM of the primary motion]. Negative values appear due to motion to the opposite direction. Values exceeding 100% are larger than movement in the primary direction. (a) Coupled motion during flexion and extension, (b) coupled motion during lateral bending, and (c) coupled motion during axial rotation. Error bars represent the standard deviation.
Coupled motion during LB was measured to be between 40 and 100% of the primary motion (Fig. 4b) and ranged from 100% up to 400% for AR (Fig. 4c). This is comprehensible, given the fact that the centers of mass are not aligned in the sagittal and axial plane.
Center of Rotation
The COR is generally defined as the penetration point of the axis of rotation (AOR) in the plane of motion. Whilst trying to characterize pathological kinematics, several authors suggested the COR to be an important indicator for early progression of spinal diseases.21,38,69,88,111,119 However, its description is challenging and associated with some inaccuracies, such as a large error magnification,93 projection errors due to coupled motion and calculation method dependence in 3D.136
Flexion/Extension
Figure 5 displays the measured CORs from four publications6,88,101,148 in either extension (black), neutral position (grey) or flexion (white). The mean COR of a face joint is usually located in the posterior, upper quarter of the caudal vertebra or in the posterior, lower quarter of the intervertebral disc. It almost completely stays in the intervertebral space for L5–S1.
The COR tends to travel from dorsal to ventral and even slightly from caudal to cranial during inclination. Additionally, two groups showed a loop-shaped COR path at certain levels,6,88 which is in line with an in vitro study by Seligman et al.119
Importantly, all the illustrated CORs are mean values. Pearcy,101 Yoshioka148 and Aiyangar6 illustrated COR spreading on areas sometimes larger than the vertebral body projection.
Lateral Bending
No in vivo study for LB could be found. In vitro studies suggest the COR to be located in the ipsilateral posterior disc region.107,111,141
Axial Rotation
One in vivo study for AR could be detected.146 They calculated the COR for maximal magnitude twisting and found it to be located ventrally of the vertebral body, close to the center of the trunk. As opposed to this, in vitro studies usually indicate the COR in the posterior part of the vertebra, posteriorly shifting with increasing torque.107,117,124,137 Xia assumed that this is because the facet joints are not the motion-limiting factor under in vivo conditions (as it is the case in vitro), but rather the surrounding tissue.146
Phase Lag
The term “phase lag” describes a shift of motion among the vertebras. PL occurs when segments start the initial movement with a certain time delay or arrive at the final position with a certain time offset. Whether this phenomenon exists or not and to what extent it exists is controversy discussed in the literature. Kanayama56 and Harada43 experienced a shifted onset from cranial to caudal. Okawa89 experienced both, a sequential and a simultaneous motion pattern for pathological subjects. Ahmadi3 and Takayanagi127 found onset delay at the caudal L5–S1 level for some subjects. Aiyangar’s7,8 studies imply a varying contribution of the segments at the beginning or end of motion. All other authors do not see (Lee,70 Wong,142 Wong143) or mention (Teyhen132) a sequential pattern.
An interesting observation is that most studies which experiences PL were performed with hip restriction or hip support. On the other side, in most of the other studies the subjects were free to move. However, this is not true for every case.127,132 Nevertheless, pelvic restriction might be a potential explanation for the occurrence of sequential onset as it could change the initial neutral position.
Flexion/Extension
Kanayama,56 Harada43 and Okawa89 did investigate the sequential onset for forward and backward flexion. They experience that segmental motion during forward flexion starts from the upper cranial levels and sequentially progresses downwards. For backward flexion, they observe the opposite, PLs starting from the most caudal L5/S1 level.
Degenerative Conditions
Degenerative diseases of the lumbar spine are difficult to diagnose, and even more challenging is their classification. Clear associations between diseases or disease stages and certain motion patterns would facilitate both diagnostics and treatment. However, in many cases, spinal pathologies are not isolated phenomena, but are accompanied by other degenerative changes.53,115,120 However, most of the studies classify patients according to the state of their primary disease, neglecting accompanying changes that are also likely to influence the kinematical behavior. Besides, even though structural changes follow a certain progress pattern,32 it is challenging to ambiguously assign them to a certain state of disease. Various grading systems are applied, and depending on the imaging technique, patients are assigned to different progress stages. Comparability is therefore limited.11,12,28,141,149
Disc Degeneration
Despite extensive research, the etiology of lumbar DD is not fully understood. In an extensive review, Hadjipavlou et al.39 conclude that the disease is initiated by a complex, multifactorial combination of stimuli such as ageing, nutrition supply and mechanical factors (vibration, torsion, compression, shear). Details however remain unclear, and kinematics are therefore even more difficult to assess.
Mechanical Stiffness
Even though not directly related, it is conceivable that the mechanical stiffness of the discs plays a role in spinal kinematics. Usually, it is described with a load–deformation curve,94 plotting the moment to the displacement at each time point when bending a functional unit (FU). Load–deformation curves consist of a neutral zone (NZ), where deformation occurs against very little internal resistance, and an elastic zone, where approximately linear resistance occurs (stiffness). Besides, the ROM is shown as the total deformation upon maximal loading. The form of the NZ describes a materials laxity, whereas the ROM is an indicator for the overall stiffness.
We summarized the findings of different in vitro studies in the following, detailed results are listed in the Appendix. However, it has to be taken into account that different grading systems and loading conditions were applied.
Flexion/Extension
Two different patterns could be detected. Some studies found decreasing ROMs for advanced stages of DD, indicating stiffening,60,81,85,150 others showed the often-cited pattern described by Kirkaldy-Willis61: an initially increasing ROM due to instability, followed by a loss of flexibility in the final stage.32,81,141 Tanaka et al.130 found both patterns and suggested level dependency (the decreasing pattern for the cranial levels and the increasing–decreasing one for the caudal levels).
However, most studies agree on a broadening NZ for progressed stages of DD, indicating increased laxity.
Lateral Bending
Associations between FE and LB behavior are frequently seen, implying that DD has similar impacts on both. However, most authors report an initial broadening and subsequent narrowing of the NZ, suggesting a decrease in laxity.
Axial Rotation
Most authors agree on a strong increase for both ROM and laxity during progress of DD.
Taken all together, the data is contradictory and rather implies an arbitrary mechanical behavior than a predetermined pattern. This is not particularly surprising, given that DD is probably a complex set of differently directed processes. Dehydration of the nucleus pulposus, osteophyte formation and diffuse sclerosis are associated with increased stiffness and hence a decrease in flexibility. On the other hand, tendon laxity due to disc height loss and facet joint arthrosis, leading to a worsened ability to guide movement, cause increased segmental mobility.
Beside the complex etiology, Tanaka et al.130 suggested level dependent kinematical behavior, which is otherwise insufficiently investigated to date. However, differing stiffness values between the levels were already shown in 1994.97
We conclude, that it is not exclusively the mechanical properties of a disc that influences the spinal kinematics, but that disc mechanics may alter motion patterns and is therefore worth considering in this context. We could not find any correlation between the measurement results of the different authors and their applied loading conditions, grading system or any other experimental factor. This finding is in line with a previously published review.36
Angular Range of Motion
DD changes the kinematics of the affected levels and it is therefore reasonable to expect differing ROMs.
Flexion/Extension
Figure 6 illustrates the change in segmental ROM in the sagittal plane, depending on the severity of DD. Agreement amongst the authors58,64,67,133 for the individual levels is lacking, however, they almost perfectly coincide when it comes to the overall change in segmental ROM (Fig. 6a). This might be explained by the larger data set of the combined data, which is less sensitive to the spread.
Figure 6a demonstrates that segmental mobility stays relatively constant until the final stage, where mobility drops down to below 50% of the healthy values. Thus the question arises whether and where the lost motion gets compensated, reminiscent of the still on-going debate about how spinal fusions influence spinal kinematics.73 According to Lee et al.,68 although all of the segments somehow participate, the significant part of motion is compensated in the L1–L2 segment (in patients with DD in L4–L5 or L5–S1).
Lateral Bending/Axial Rotation
No literature could be found for LB. For AR, Basques et al.10 was the only group investigating DD-associated ROM change in vivo. According to them, segments slowly lose their ROM during the progress of DD, with the strongest decrease between stages 4 and 5.
Overall ROM
Most studies could not demonstrate any significant change in overall lumbar ROM.30,55,76,108,134 However, Weiner et al.139 found decreased ROM in forward and lateral flexion, and Lee et al.68 demonstrated decreased lumbar ROM for patients with stage 4 or 5 DD and < 5° motion in L4–L5 or L5–S1. This implies that even though lost motion is partly compensated by the other segments (as described above), overall lumbar ROM is also decreased. The reason why many authors could not find significant motion reduction in overall lumbar motion is probably because they classified the segments according to existence or non-existence of DD and did not consider whether the degenerated segments indeed had a reduced mobility.
Translational Range of Motion
Similar as for the angular ROM, consensus between the authors could only be found for the mean segmental change in translational ROM (Fig. 7).9,58,64 After an initial increase at the intermediate stages, mobility drops again at stage 5 to a healthy level. In contrast to the change in angular ROM, translational motion reduction does not take place.
Center of Rotation
Several authors suggested the COR as a tool to recognize the onset of DD at an early stage.37,38,103,119,141 However, to the best of our knowledge, no in vivo studies were published. The cadaveric study from Seligman et al.119 suggests that DD segments start to move with an erratic motion pattern and thus the COR loses stability and its travel path enlarges during sagittal movement. This phenomenon seems to mainly appear during initial and intermediate stages of DD and resolves as soon as ankylosing processes come into play. However, cadaveric studies only permit limited insight into in vivo behavior.
Facet Joint Osteoarthritis
The zygapophyseal joints are essential for load transmission,2 spinal stabilization1,20,41,121 and strongly influence spinal kinematics.4 Just as in other types of diarthrodial joints, FJOA leads to the cartilage degradation and therefore focal and diffuse erosions with sclerosis of subchondral bone.25
It is etiologically related to aging, injury, gender, facet joint orientation and the spinal level.54 Besides, strong association with DD was shown,16,35,41,121 even though the time course of the two diseases is still controversially discussed. Most authors suggest that DD is usually preceding FJOA.34,35,121,135
Range of Motion
Kong et al.64 investigated the change in angular and translational motion in the sagittal plane in relation to the degree of FJOA, using an MRI based grading system as proposed by Fujiwara.35 They illustrated that angular mobility seems to monotonically decrease with progressing FJOA (Fig. 8a). On the other hand, translational ROM increased until grade 3 but dropped at the final stage of FJOA (Fig. 8b).
Angular motion (a) and translational motion (b) for flexion/extension in relation to the degree of facet joint osteoarthritis according to Fujiwara. (c) Male (blue) and female (green) angular motion in all planes according to the degree of subchondral sclerosis, cartilage degeneration and osteophyte formation. Data is normalized to the healthy value (grade 1).
Fujiwara et al.32 divided the pathology of FJOA into three components (subchondral sclerosis, cartilage degeneration, osteophyte formation) and developed a three level grading system to classify each of them (Fig. 8c). Osteophyte formation and cartilage degradation correlate with a ROM pattern proposed by Kirkaldy-Willis: increased angular motion occurs during stage II, which is however reversed to normal ROM values at stage 3. As opposed to this, subchondral sclerosis seems to decrease segmental motion in all planes. A reasonable explanation could be that these are simultaneously ongoing but counteracting processes. Cartilage degeneration loosens the segment, while osteophyte formation and subchondral sclerosis are instantaneously initiated in order to counterbalance segment instability.
Instability
Fujiwara et al.33 and Jang52 investigated the influence of FJOA by defining a translational and angular threshold [max. sagittal ROM: translation > 3 mm, angular motion > 15° (L3–L5)/> 20° (L5–S1)]. Segments exceeding these values were defined as unstable. Fujiwara furthermore divided into anterior and posterior instability. He only found a positive association between FJOA and anterior translatory instability whereas posterior and angular instability were negatively associated. On the other hand, Jang tested instability by complexly correlating DD, FJOA and ligament flavum hypertrophy (LFH). He found angular L4–L5 instability when segments were affected by severe FJOA and LFH. His investigations demonstrate that combined investigations might provide better insight.
Facet Joint Tropism
FJT is defined as asymmetry in orientation of the bilateral facets planes. Kong82 for example determined FJT as an angel difference greater than 7°. To date, it is not clear whether lumbar FJT is congenitally caused or secondary to degeneration. A recent large-scale study within the Asian population however showed that it is age independent, implying that it might be congenital due to a pre-existing phenotype.115
Miyazaki et al.84 investigated the influence of facet orientation and FJT on spinal kinematics (Fig. 9). He grouped the facets according to their sagittal angle (angle between sagittal plane and facet plane in transversal the view): “A” are angles smaller than 38.5° (− 0.5 SD), “B” angles from 38.5° to 49° and “C” angles > 49°. He observed that the orientation (AA, BB, CC represent symmetric facet joints) has a significant impact on the translational motion and non-significant but notable influence on the angular motion (Fig. 9a). As it is expected, more sagittal alignment allows increased movement. Similarly, asymmetry of the facet planes played a role (Fig. 9b). However, the data implies that rather the orientation of the facets than the asymmetry is important.
Angular and translational motion according to the facet orientation (a) and to the facet tropism (b). “A” are angles smaller than 38.5° (− 0.5 SD), “B” angles from 38.5° to 49° and “C” angles > 49°. In a, data is normalized to the BB value, in b to the average of AA, BB and CC. The illustrated data is from Miyazaka.84
Spondylolisthesis
SL is the anterior displacement of a vertebra in relation to the natural curve of the spine. Its severity is oftentimes described with the grading system of Meyerding,78 measuring the percentage of translation of a vertebra relative to its subadjacent vertebra. Grades 1 to 4 represent 0–25, 25–50, 50–75 and 75–100% respectively.
Knutsson et al.62 first investigated the stability of the malaligned segment in 1944.
In the meantime, the kinematics of SL affected lumbar spines has been frequently studied and a better understanding could be established.
Range of Motion
Despite the intuitive belief and some early established theories stating that such segments are hypermobile,62,90 recent literature agrees on normal or even decreased mobility of spondylolisthetic segments.9,75,79,116,144 These authors could not find any sign of instability, as opposed to Penning104 and Knuttson,62 who found hypermobile SL segments.
Figure 10 summarizes all studies providing specific data on the angular motion with and without SL. With the exception of Phan et al.,105 who found a slightly increasing ROM for L4–L5 and L5–S1 SL segments, all authors agree on decreasing mobility in SL affected levels.69,120,141 This loss of motion is attributed to muscle spasm and increased ligament tension due to the slippage between the vertebrae.102 Interestingly, Takayanagi et al.127 distinguished between two stages of SL and found an initially increasing and later decreasing ROM, implying that also the effects of SL depend on the severity.
As opposed to this, the ROM for translational movements seems to slightly increase in SL affected segments. However, Takayanagi et al.127 was the only group who could demonstrate a significant difference.
Whether compensation for increased and decreased motion of SL affected segments occurs in the other segments is not known. Most authors report an overall reduction of the lumber ROM, Yao147 and Phan105 showed tendencies towards decreased ROM for the adjacent levels44 and therefore also for the overall lumbar spine. In line with this, McGregor et al.77 found a decreased overall lumbar ROM.
Even though most of the presented data does not show any significant changes in ROM, several authors describe erratic motion patterns79,88,90,91,127 or even backward slipping during flexion.104,118 Subsequently, we assume that SL alters spinal kinematics in a way that is mainly independent from segmental ROM.
Large-scale studies with dynamical imaging and SL classification according to severity and type (isthmic, degenerative, dysplastic, etc.) are needed for clarification.
Center of Rotation
Penning et al.104 investigated the COR of SL segments and noted an increased spread. In contrast, Schneider et al.22 examined 13 patients and demonstrated backward slipping of the vertebra during flexion in 6 patients. The COR was found to be located cranially of the disc instead of the healthy location within the subadjacent vertebra.
Ligament Degeneration
Spinal ligaments significantly contribute to the stability of the spine.49,50,96 They have been shown to lose tensile strength and elastic modulus with age,50,59 which is associated with decreased stability. Even though LD was related to lower back pain,95 only a few authors investigated the relation between LD and altered spine kinematics.
Range of Motion
Literature is very scarce; we however identified two studies investigating the effects of interspinous ligament (IL) and ligamentum flavum (LF) degeneration on ROM.
Interspinous Ligament
Figure 11 illustrates the results with quite good agreement between the two groups.59,64 ROM is slightly increasing during the initial and only drops at the final stage for the more cranial segments. As opposed to this, ROM constantly decreases for L4–L5 during progress of LD, with the exception of stage 3 in the L5–S1 segments, showing a prominent peak of ROM.
No significant impact on translational motion could be found by either of them.
Ligamentum Flavum
Kong et al.64 investigated spinal kinematics related to hypertrophy of the LF. Whilst finding no significant difference in angular motion, they demonstrated a significant increase in translational motion in LFH affected spines.
Paraspinal Muscle Degeneration
PMD has multiple times be shown to accompany lumbar degenerative diseases like DD122,131 or FJOA.17 Interestingly, it was also observed that animals with degenerative discs, experience a stiffening of the multifidus muscle.15 It is therefore reasonable to assume that degenerative states of these muscles also influence the kinematics of the spine to some extent. To our knowledge, there is however only one study which investigated the relationship between PMD and the spinal kinematics in the lumbar spine, which is the study of Kong et al.63 He investigated 1575 spine units and split them into a hypermobile (defined as angular ROM > 10° or translational ROM > 3 mm) and a normal cohort. He could show that the presence of fatty muscle infiltration was significantly associated with the presence of excessive angular motion. This effect was however not seen for translational hypermobility. Also at the cervical spine, instability related to PMD could not be observed (except at the C3–C4 level).51
Discussion
This review aims at providing a “state of art” collection on the spinal kinematics under healthy and degenerative conditions. Quite some research has been done since the last review of Panjabi and White,95,140 which is however still often referred to as state of the art.
Whilst Panjabi and White had to rely on a small selection of mostly in vitro studies, an immense range of in vivo publications is available today, usually performed with sophisticated measurement techniques. However, despite modern methods, final scientific clarity is widely lacking. Spinal in vivo experiments are highly sensitive to experimental parameters and hence, findings are various and sometimes even contradicting. Additionally, with newer methods allowing spatial 3D-tracking of the vertebras, it has become indispensable to agree on very well-defined conventions of how to evaluate results—and to accurately describe them. We therefore would like to emphasize the importance of a precisely defined and described method for future studies. Moreover, common standards and definitions will facilitate comparisons and establishment of reference values.
Besides, sample sizes usually decrease in studies with a complex experimental setup. More sophisticated and therefore accurate methods are time-consuming and expensive, and accordingly suffer from high sample variance due to a small patient population. On the other hand, simpler methods can be applied to a larger population, but lose quality due to the inaccuracy of the technique. However, immense technical possibilities are given and the diversity of experimental parameters is well known by now. The door is therefore wide open for large-scale studies with great potential to provide clarification of the pressing questions.
We initially asked the question of whether it is possible to define healthy kinematic behavior and clearly distinguish it from the motion pattern of a degenerated spine. In conclusion, the answer has to be: not yet. As summarized in the section on degenerated spines, many diseases are associated with significant differences in kinematical behavior. However, due to high individuality, healthy and pathological ranges largely overlap and a clear distinction is therefore not yet feasible.
An interesting finding is that increasing stiffness of a segment during DD does not immediately produce decreasing motion. ROM is only reduced at the final stage, when severe ankylosing processes come into play. We thus conclude that mechanical stiffness is compensated by increased muscular activity to enable end-positions of certain movements. Cadaveric and also finite element studies, both neglecting muscular components, therefore have very limited power to simulate in vivo behavior.
What remains unclear is to what extent ankylosing processes are involved in restabilization of a segment as described by Kirkaldy-Willis.61 Many figures in this review follow the proposed pattern, suggesting that such mechanisms indeed exists. On the other hand, examples of a monotonically decreasing motion pattern challenge the Kirkaldy-Willis theory and therefore call for more research.
Another essential point to keep in mind is to not only look at degenerative changes as an isolated disease but to incorporate all of the simultaneously ongoing processes. Jang et al.52 could show correlations between kinematical changes and combinations of degenerative diseases. Broadening our perspective accordingly could lead to a better understanding in the field.
We also like to emphasize that more research is required in some of the topics. Particularly, this is LD and PMD. Since, the impact of these degenerative changes are not understood well enough, they are also not involved in the clinical diagnostics nowadays.
In conclusion it can be said that research still is in the middle of investigating extremely complex processes. Hence, direct clinical value in order to use kinematical parameters as a tool to diagnose or to make decisions on surgical interventions is very limited to date. However, we are confident that this will change in the future.
As a limitation of this review, we would like to point out the possibility that some publications were missed by the choice of the key words. We tried to select the keywords very general and also included a subsequent reference search in order to find most of the studies. However, medical and biomechanical terms for the same topics can strongly vary and therefore, we cannot completely exclude that some studies were missed.
Abbreviations
- AOR:
-
Axis of rotation
- AR:
-
Axial rotation
- COR:
-
Center of rotation
- DD:
-
Disc degeneration
- FE:
-
Flexion/extension
- FJOA:
-
Facet joint osteoarthritis
- FJT:
-
Facet joint tropism
- FU:
-
Functional unit
- IL:
-
Interspinous ligament
- LB:
-
Lateral bending
- LD:
-
Ligament degeneration
- LF:
-
Ligamentum flavum
- LFH:
-
Ligamentum flavum hypertrophy
- NZ:
-
Neutral zone
- OA:
-
Osteoarthritis
- PMD:
-
Paraspinal muscle degeneration
- ROM:
-
Range of motion
- SL:
-
Spondylolisthesis
References
Abum, K., M. M. Panjabi, K. M. Kramer, J. Duranceau, T. Oxland, and J. J. Crisco. Biomechanical evaluation of lumbar spinal stability after graded facetectomies. Spine (Phila. Pa. 1976) 15:1142–1147, 1990.
Adams, M. A., and W. C. Hutton. The effect of posture on the role of the apophysial joints in resisting intervertebral compressive forces. J. Bone Jt Surg. Br. 62-B:358–362, 1980.
Ahmadi, A., N. Maroufi, H. Behtash, H. Zekavat, and M. Parnianpour. Kinematic analysis of dynamic lumbar motion in patients with lumbar segmental instability using digital videofluoroscopy. Eur. Spine J. 18:1677–1685, 2009.
Ahmed, A. M., N. A. Duncan, and D. L. Burke. The effect of facet geometry on the axial torque-rotation response of lumbar motion segments. Spine (Phila. Pa. 1976) 15:391–401, 1990.
Aiyangar, A., L. Zheng, W. Anderst, and X. Zhang. Apportionment of lumbar L2–S1 rotation across individual motion segments during a dynamic lifting task. J. Biomech. 48:3709–3715, 2015.
Aiyangar, A., L. Zheng, W. Anderst, and X. Zhang. Instantaneous centers of rotation for lumbar segmental flexion–extension in vivo. J. Biomech. 2016. https://doi.org/10.1016/j.jbiomech.2016.12.021.
Aiyangar, A. K., L. Zheng, S. Tashman, W. J. Anderst, and X. Zhang. Capturing three-dimensional in vivo lumbar intervertebral joint kinematics using dynamic stereo-X-ray imaging. J. Biomech. Eng. 136:011004, 2014.
Aiyangar, A. K., et al. Capturing three-dimensional in vivo lumbar intervertebral joint kinematics using dynamic stereo-X-ray imaging. J. Biomech. Eng. 136:1–9, 2016.
Axelsson, P., R. Johnsson, and B. Stromqvist. Is there increased intervertebral mobility in isthmic adult spondylolisthesis? A matched comparative study using Roentgen stereophotogrammetry. Spine (Phila. Pa. 1976) 25:1701–1703, 2000.
Basques, B. A., A. A. Espinoza Orías, G. D. Shifflett, M. P. Fice, G. B. Andersson, H. S. An, and N. Inoue. The kinematics and spondylosis of the lumbar spine vary depending on the levels of motion segments in individuals with low back pain. Spine (Phila. Pa. 1976) 42:E767–E774, 2017.
Benneker, L. M., P. F. Heini, S. E. Anderson, M. Alini, and K. Ito. Correlation of radiographic and MRI parameters to morphological and biochemical assessment of intervertebral disc degeneration. Eur. Spine J. 14:27–35, 2005.
Bergknut, N., G. Grinwis, E. Pickee, E. Auriemma, A. S. Lagerstedt, R. Hagman, H. A. W. Hazewinkel, and B. P. Meij. Reliability of macroscopic grading of intervertebral disk degeneration in dogs by use of the Thompson system and comparison with low-field magnetic resonance imaging findings. Am. J. Vet. Res. 72:899–904, 2011.
Blankenbaker, D. G., V. M. Haughton, B. P. Rogers, M. E. Meyerand, and J. P. Fine. Axial rotation of the lumbar spinal motion segments correlated with concordant pain on discography: a preliminary study. Am. J. Roentgenol. 186:795–799, 2006.
Boden, S. D., and S. W. Wiesel. Lumbosacral segmental motion in normal individuals. Have we been measuring instability properly? Spine (Phila. Pa. 1976) 15:571–576, 1990.
Brown, S. H. M., D. E. Gregory, J. A. Carr, S. R. Ward, K. Masuda, and R. L. Lieber. ISSLS prize winner: adaptations to the multifidus muscle in response to experimentally induced intervertebral disc degeneration. Spine (Phila. Pa. 1976) 36:1728–1736, 2011.
Butler, D., J. H. Trafimow, G. B. J. Andersson, T. W. McNeill, and M. S. Huckman. Discs degenerate before facets. Spine (Phila. Pa. 1976) 15:111–113, 1990.
Cooley, J. R., B. F. Walker, E. M. Ardakani, T. S. Jensen, and J. J. Hebert. Relationships between paraspinal muscle morphology and neurocompressive conditions of the lumbar spine: a systematic review with meta-analysis. BMC Musculoskelet. Disord. 19:1–21, 2018.
Cossette, J. W., H. F. Farfan, G. H. Robertson, and R. V. Wells. The instantaneous center of rotation of the third lumbar intervertebral joint. J. Biomech. 4:149–153, 1971.
Crawford, H. J., and G. A. Jull. The influence of thoracic posture and movement on range of arm elevation. Physiother. Theory Pract. 9:143–148, 1993.
Cyron, B. M., and W. C. Hutton. Articular tropism and stability of the lumbar spine. Spine (Phila. Pa. 1976) 5:168–172, 1980.
Dimnet, J., A. Pasquet, M. H. Krag, and M. M. Panjabi. Cervical spine motion in the sagittal plane: Kinematic and geometric parameters. J. Biomech. 15:959–969, 1982.
Duda, G. N., M. Heller, J. Albinger, O. Schulz, E. Schneider, and L. Claes. Influence of muscle forces on femoral strain distribution. J. Biomech. 31:841–846, 1998.
Dvorak, J., M. M. Panjabi, D. G. Chang, R. Theiler, and D. Grob. Functional radiographic diagnosis of the lumbar spine. Flexion–extension and lateral bending. Spine (Phila. Pa. 1976) 16:562–571, 1991.
Dvořák, J., M. M. Panjabi, J. E. Novotny, D. G. Chang, and D. Grob. Clinical validation of functional flexion–extension Roentgenograms of the lumbar spine. Spine (Phila. Pa. 1976) 16:943–950, 1991.
Eisenstein, S. M., and C. R. Parry. The lumbar facet arthrosis syndrome. Clinical presentation and articular surface changes. J. Bone Jt Surg. Br. 69:3–7, 1987.
Farrance, I., and R. Frenkel. Uncertainty of measurement: a review of the rules for calculating uncertainty components through functional relationships. Clin. Biochem. Rev. 33:49–75, 2012.
Friberg, O. Instability in spondylolisthesis. Orthopedics 14:463–465, 1991.
Frobin, W., P. Brinckmann, M. Kramer, and E. Hartwig. Height of lumbar discs measured from radiographs compared with degeneration and height classified from MR images. Eur. Radiol. 11:263–269, 2001.
Frobin, W., P. Brinckmann, G. Leivseth, M. Biggemann, and O. Reikeras. Precision measurement of segmental motion from flexion–extension radiographs of the lumbar spine. Clin. Biomech. 11:457–465, 1996.
Frymoyeyr, J., A. Newberg, and M. Pope. Spine radiographs in patients with low back pain. J. Bone Jt Surg. Am. 66:1048–1055, 1984.
Fujii, R., H. Sakaura, Y. Mukai, N. Hosono, T. Ishii, M. Iwasaki, H. Yoshikawa, and K. Sugamoto. Kinematics of the lumbar spine in trunk rotation: in vivo three-dimensional analysis using magnetic resonance imaging. Eur. Spine J. 16:1867–1874, 2007.
Fujiwara, A., T. H. Lim, H. S. An, N. Tanaka, C. H. Jeon, G. B. J. Andersson, and V. M. Haughton. The effect of disc degeneration and facet joint osteoarthritis on the segmental flexibility of the lumbar spine. Spine (Phila. Pa. 1976) 25:3036–3044, 2000.
Fujiwara, A., K. Tamai, H. S. An, T. Kurihashi, T. H. Lim, H. Yoshida, and K. Saotome. The relationship between disc degeneration, facet joint osteoarthritis, and stability of the degenerative lumbar spine. J. Spinal Disord. 13:444–450, 2000.
Fujiwara, A., K. Tamai, H. S. An, T.-H. Lim, H. Yoshida, A. Kurihashi, and K. Saotome. Orientation and osteoarthritis of the lumbar facet joint. Clin. Orthop. Relat. Res. 385:88–94, 2001.
Fujiwara, A., K. Tamai, M. Yamato, H. S. An, H. Yoshida, K. Saotome, and A. Kurihashi. The relationship between facet joint osteoarthritis and disc degeneration of the lumbar spine: an MRI study. Eur. Spine J. 8:396–401, 1999.
Galbusera, F., M. Van Rijsbergen, K. Ito, J. M. Huyghe, M. Brayda-Bruno, and H. J. Wilke. Ageing and degenerative changes of the intervertebral disc and their impact on spinal flexibility. Eur. Spine J. 23:324–332, 2014.
Gertzbein, S. D., J. Seligman, R. Holtby, K. W. Chan, N. Ogston, A. Kapasouri, and M. Tile. Centrode characteristics of the lumbar spine as a function of segmental instability. 1986.
Gertzbein, S. D., J. Seligman, R. Holtby, K. H. Chan, A. Kapasouri, M. Tile, and B. Cruickshank. Centrode patterns and segmental instability in degenerative disc disease. Spine (Phila. Pa. 1976) 10:257–261, 1985.
Hadjipavlou, A. G., M. N. Tzermiadianos, N. Bogduk, and M. R. Zindrick. The pathophysiology of disc degeneration: a critical review. J. Bone Jt Surg. Br. 90:1261–1270, 2008.
Haher, T. R., M. Bergman, M. O’Brien, W. T. Felmly, J. Choueka, D. Welin, G. Chow, and A. Vassiliou. The effect of the three columns of the spine on the instantaneous axis of rotation in flexion and extension. Spine (Phila. Pa. 1976) 16:S319, 1991.
Haher, T. R., M. O’Brien, J. W. Dryer, R. Nucci, R. Zipnick, and D. J. Leone. The role of the lumbar facet joints in spinal stability. Spine (Phila. Pa. 1976) 19:2667–2670, 1994.
Haher, T. R., M. O’Brien, W. T. Felmly, D. Welin, G. Perrier, J. Choueka, V. Devlin, A. Vassiliou, and G. Chow. Instantaneous axis of rotation as a function of the three columns of the spine. Spine (Phila. Pa. 1976) 17:S149–S154, 1992.
Harada, M., K. Abumi, M. Ito, and K. Kaneda. Cineradiographic motion analysis of normal lumbar spine during forward and backward flexion. Spine (Phila. Pa. 1976) 25:1932–1937, 2000.
Hasegewa, K., K. Kitahara, T. Hara, K. Takano, and H. Shimoda. Biomechanical evaluation of segmental instability in degenerative lumbar spondylolisthesis. Eur. Spine J. 18:465–470, 2009.
Hashemirad, F., B. Hatef, S. Jaberzadeh, and N. Ale Agha. Validity and reliability of skin markers for measurement of intersegmental mobility at L2–3 and L3–4 during lateral bending in healthy individuals: a fluoroscopy study. J. Bodyw. Mov. Ther. 17:46–52, 2013.
Haughton, V. M., B. Rogers, M. E. Meyerand, and D. K. Resnick. Measuring the axial rotation of lumbar vertebrae in vivo with MR imaging. Am. J. Neuroradiol. 23:1110–1116, 2002.
Hayashi, T., M. D. Daubs, A. Suzuki, T. P. Scott, K. H. Phan, M. Ruangchainikom, S. Takahashi, K. Shiba, and J. C. Wang. Motion characteristics and related factors of Modic changes in the lumbar spine. J. Neurosurg. Spine 22:1–7, 2015.
Hayes, M. Roentgenographic evaluation of lumbar spine flex-ex in asymptomatic individuals. Spine (Phila. Pa. 1976) 14:327–331, 1989.
Heuer, F., H. Schmidt, Z. Klezl, L. Claes, and H. Wilke. Stepwise reduction of functional spinal structures increase range of motion and change Lordosis angle. J. Biomech. 40:271–280, 2007.
Iida, T., K. Abumi, Y. Kotani, and K. Kaneda. Effects of aging and spinal degeneration on mechanical properties of lumbar supraspinous and interspinous ligaments. Spine J. 2:95–100, 2002.
Inoue, H., S. Montgomery, B. Aghdasi, Y. Tan, H. Tian, X. Jian, R. Terrell, V. Singh, and J. Wang. Analysis of relationship between paraspinal muscle fatty degeneration and cervical spine motion using kinetic magnetic resonance imaging. Glob. Spine J. 02:033–038, 2012.
Jang, S. Y., M. H. Kong, H. J. Hymanson, T. K. Jin, K. Y. Song, and J. C. Wang. Radiographic parameters of segmental instability in lumbar spine using kinetic MRI. J. Korean Neurosurg. Soc. 45:24–31, 2009.
Jaumard, N. V., W. C. Welch, and B. A. Winkelstein. Spinal facet joint biomechanics and mechanotransduction in normal, injury and degenerative conditions. J. Biomech. Eng. 133:071010, 2011.
Kalichman, L., and D. J. Hunter. Lumbar facet joint osteoarthritis: a review. Semin. Arthritis Rheum. 37:69–80, 2007.
Kambin, P., J. E. Nixon, A. Chait, and J. L. Schaffer. Annular protrusion: pathophysiology and Roentgenographic appearance. Spine (Phila. Pa. 1976) 13:671–675, 1988.
Kanayama, M., K. Abumi, K. Kaneda, S. Tadano, and T. Ukai. Phase lag of the intersegmental motion in flexion–extension of the lumbar and lumbosacral spine: an in vivo study. Spine (Phila. Pa. 1976) 21:1416–1422, 1996.
Karadimas, E. J., M. Siddiqui, F. W. Smith, and D. Wardlaw. Positional MRI changes in supine versus sitting postures in patients with degenerative lumbar spine. J. Spinal Disord. Tech. 19:495–500, 2006.
Keorochana, G., C. E. Taghavi, K.-B. Lee, J. H. Yoo, J.-C. Liao, Z. Fei, and J. C. Wang. Effect of sagittal alignment on kinematic changes and degree of disc degeneration in the lumbar spine: an analysis using positional MRI. Spine (Phila. Pa. 1976) 36:893–898, 2011.
Keorochana, G., C. E. Taghavi, S.-T. Tzeng, Y. Morishita, J. H. Yoo, K.-B. Lee, J.-C. Liao, and J. C. Wang. Magnetic resonance imaging grading of interspinous ligament degeneration of the lumbar spine and its relation to aging, spinal degeneration, and segmental motion. J. Neurosurg. Spine 13:494–499, 2010.
Kettler, A., F. Rohlmann, C. Ring, C. Mack, and H. J. Wilke. Do early stages of lumbar intervertebral disc degeneration really cause instability? Evaluation of an in vitro database. Eur. Spine J. 20:578–584, 2011.
Kirkaldy-Willis, W. H., and H. F. Farfan. Instability of the lumbar spine. Spine (Phila. Pa. 1976) 10:253, 1985.
Knutsson, F. The instability associated with disc degeneration in the lumbar spine. Acta radiol. 25:593–609, 1944.
Kong, M. H., H. J. Hymanson, K. Y. Song, D. K. Chin, Y. E. Cho, D. H. Yoon, and J. C. Wang. Kinetic magnetic resonance imaging analysis of abnormal segmental motion of the functional spine unit. J. Neurosurg. Spine 10:357–365, 2009.
Kong, M. H., Y. Morishita, W. He, M. Miyazaki, H. Zhang, G. Wu, H. J. Hymanson, and J. C. Wang. Lumbar segmental mobility according to the grade of the disc, the facet joint, the muscle, and the ligament pathology by using kinetic magnetic resonance imaging. Spine (Phila. Pa. 1976) 34:2537–2544, 2009.
Krismer, M., C. Haid, H. Behensky, P. Kapfinger, F. Landauer, and F. Rachbauer. Motion in lumbar functional spine units during side bending and axial rotation moments depending on the degree of degeneration. Spine (Phila. Pa. 1976) 25:2020–2027, 2000.
Kulig, K., C. Powers, and R. Landel. Segmental lumbar mobility in individuals with low back pain: in vivo assessment during manual and self-imposed motion using dynamic MRI. BMC Musculoskelet. Disord. 10:1–10, 2007.
Lao, L., M. D. Daubs, T. P. Scott, E. L. Lord, J. R. Cohen, R. Yin, G. Zhong, and J. C. Wang. Effect of disc degeneration on lumbar segmental mobility analyzed by kinetic magnetic resonance imaging. Spine (Phila. Pa. 1976) 40:316–322, 2014.
Lee, S. H., S. D. Daffner, J. C. Wang, B. C. Davis, A. Alanay, and J. S. Kim. The change of whole lumbar segmental motion according to the mobility of degenerated disc in the lower lumbar spine: a kinetic MRI study. Eur. Spine J. 24:1893–1900, 2014.
Lee, S. W., E. R. C. Draper, and S. P. F. Hughes. Instantaneous center of rotation and instability of the cervical spine: a clinical study. Eur. Spine J. 22:641–648, 1997.
Lee, S., K. W. N. Wong, M. Chan, H. Yeung, J. L. F. Chiu, and J. C. Y. Leong. Development and validation of a new technique for assessing lumbar spine motion. Spine (Phila. Pa. 1976) 27:E215, 2002.
Li, G., S. Wang, P. Passias, Q. Xia, G. Li, and K. Wood. Segmental in vivo vertebral motion during functional human lumbar spine activities. Eur. Spine J. 18:1013–1021, 2009.
Li, W., S. Wang, Q. Xia, P. Passias, M. Kozanek, K. Wood, and G. Li. Lumbar facet joint motion in patients with degenerative disc disease at affected and adjacent levels: an in vivo biomechanical study. Spine (Phila. Pa. 1976) 36:E629–E637, 2011.
Malakoutian, M., D. Volkheimer, J. Street, M. F. Dvorak, H. J. Wilke, and T. R. Oxland. Do in vivo kinematic studies provide insight into adjacent segment degeneration? A qualitative systematic literature review. Eur. Spine J. 24:1865–1881, 2015.
Mansour, M., S. Spiering, C. Lee, H. Dathe, A. K. Kalscheuer, D. Kubein-Meesenburg, and H. Nägerl. Evidence for IHA migration during axial rotation of a lumbar spine segment by using a novel high-resolution 6D kinematic tracking system. J. Biomech. 37:583–592, 2003.
McGregor, A. H., L. Anderton, W. M. W. Gedroyc, J. Johnson, and S. P. F. Hughes. The use of interventional open MRI to assess the kinematics of the lumbar spine in patients with spondylolisthesis. Spine (Phila. Pa. 1976) 27:1582–1586, 2002.
McGregor, A. H., H. R. Cattermole, and S. P. Hughes. Spinal motion in lumbar degenerative disc disease. J. Bone Jt Surg. Br. 80:1009–1013, 1998.
McGregor, A. H., H. R. Cattermole, and S. P. Hughes. Global spinal motion in subjects with lumbar spondylolysis and spondylolisthesis: does the grade or type of slip affect global spinal motion? Spine (Phila. Pa. 1976) 26:282–286, 2001.
Meyerding, H. W. Spondylolisthesis. Surg. Gynecol. Obstet. 54:371, 1932.
Miao, J., S. Wang, Z. Wan, W. M. Park, Q. Xia, K. Wood, and G. Li. Motion characteristics of the vertebral segments with lumbar degenerative spondylolisthesis in elderly patients. Eur. Spine J. 22:425–431, 2013.
Mimura, M. Rotational instability of the lumbar spine—a three-dimensional motion study using bi-plane X-ray analysis system. Nippon Seikeigeka Gakkai Zasshi 64:546–559, 1990.
Mimura, M., et al. Disc degeneration affects the multidirectional flexibility of the lumbar spine. Spine (Phila. Pa. 1976) 19:1371–1380, 1993.
Min, H. K., W. He, Y. D. Tsai, N. F. Chen, G. Keorochana, D. H. Do, and J. C. Wang. Relationship of facet tropism with degeneration and stability of functional spinal unit. Yonsei Med. J. 50:624–629, 2009.
Miyasaka, K., K. Ohmori, K. Suzuki, and H. Inoue. Radiographic analysis of lumbar motion in relation to lumbosacral stability. Investigation of moderate and maximum motion. Spine (Phila. Pa. 1976) 25:732–737, 2000.
Miyazaki, M., Y. Morishita, C. Takita, T. Yoshiiwa, J. C. Wang, and H. Tsumura. Analysis of the relationship between facet joint angle orientation and lumbar spine canal diameter with respect to the kinematics of the lumbar spinal unit. J. Spinal Disord. Tech. 23:242–248, 2010.
Muriuki, M. G., R. M. Havey, L. I. Voronov, G. Carandang, M. R. Zindrick, M. A. Lorenz, L. Lomasney, and A. G. Patwardhan. Effects of motion segment level, Pfirrmann intervertebral disc degeneration grade and gender on lumbar spine kinematics. 1–10, 2016. https://doi.org/10.1002/jor.23232.
Ochia, R. S., N. Inoue, S. M. Renner, E. P. Lorenz, T. Lim, G. B. J. Andersson, and H. S. An. Three-dimensional in vivo measurement of lumbar spine segmental motion. Spine (Phila. Pa. 1976) 31:2073–2078, 2006.
Ochia, R. S., N. Inoue, R. Takatori, G. B. J. Andersson, and H. S. An. In vivo measurements of lumbar segmental motion during axial rotation in asymptomatic and chronic low back pain male subjects. Spine (Phila. Pa. 1976) 32:1394–1399, 2007.
Ogston, N.G. Centrode patterns in the lumbar spine. 1985.
Okawa, A., K. Shinomiya, H. Komori, T. Muneta, Y. Arai, and O. Nakai. Dynamic motion study of the whole lumbar spine by videofluoroscopy. Spine (Phila. Pa. 1976) 23:1743–1749, 1998.
Olsson, T. H., G. Selvik, and S. Willner. Vertebral motion in spondylolisthesis. Acta Radiol. Diagn. (Stockh.) 17:861–868, 1976.
Otani, K., A. Okawa, K. Shinomiya, and O. Nakai. Spondylolisthesis with postural slip reduction shows different motion patterns with video-fluoroscopic analysis. J. Orthop. Sci. 10:152–159, 2005.
Oxland, T. R., T. Lund, B. Jost, P. Cripton, K. Lippuner, P. Jaeger, and L. P. Nolte. The relative importance of vertebral bone density and disc degeneration in spinal flexibility and interbody implant performance: an in vitro study. Spine (Phila. Pa. 1976) 21:2558–2569, 1996.
Panjabi, M. M. Centers and angles of rotation of body joints: a study of errors and optimization. J. Biomech. 12:911–920, 1979.
Panjabi, M. M. The stabilizing system of the spine. Part II. Neutral zone and instability hypothesis. J. Spinal Disord. 5:390–397, 1992.
Panjabi, M. M. A hypothesis of chronic back pain: ligament subfailure injuries lead to muscle control dysfunction. Eur. Spine J. 15:668–676, 2006.
Panjabi, M. M., V. K. Goel, and K. Takata. Physiologic strains in the lumbar spine ligaments. Spine (Phila. Pa. 1976) 7:192–203, 1982.
Panjabi, M. M., T. R. Oxland, I. Yamamoto, and J. J. Crisco. Mechanical behavior of the human lumbar and lumbosacral spine as shown by three-dimensional load–displacement curves. J. Bone Jt Surg. Am. 76:413–424, 1994.
Passias, P. G., S. Wang, M. Kozanek, Q. Xia, W. Li, B. Grottkau, K. B. Wood, and G. Li. Segmental lumbar rotation in patients with discogenic low back pain during functional weight-bearing activities. J. Bone Jt Surg. Am. 93:29–37, 2011.
Patel, M. M., D. V. Gohil, and T. C. Singel. Orientation of superior articular facets from C3 to S1 vertebrae. J. Anat. Soc. India 53:35–39, 2004.
Pearcy, M. J. Stereoradiography of lumbar spine motion. Acta Orthop. Scand. 212(Suppl):1–45, 1985.
Pearcy, M. J., and N. Bogduk. Instantaneous axes of rotation of the lumbar intervertebral joints. pdf., 1988.
Pearcy, M., and J. Shepherd. Is there instability in spondylolisthesis? Spine (Phila. Pa. 1976) 10:175–177, 1985.
Pennal, G. F., G. S. Conn, G. McDonald, G. Dale, and H. Garside. Motion studies of the lumbar spine—a preliminary report. J. Bone Jt Surg. 54 B:442–452, 1972.
Penning, L., and J. R. Blickman. Instability in lumbar spondylolisthesis: a radiologic study of several concepts. Am. J. Roentgenol. 1979. https://doi.org/10.2214/ajr.134.2.293.
Phan, K. H., M. D. Daubs, A. I. Kupperman, T. P. Scott, and J. C. Wang. Kinematic analysis of diseased and adjacent segments in degenerative lumbar spondylolisthesis. Spine J. 15:230–237, 2015.
Plamondon, A., M. Gagnon, and G. Maurais. Application of a stereoradiographic method for the study of intervertebral motion. Spine (Phila. Pa. 1976) 13:1027–1032, 1988.
Pope, M. H., D. G. Wilder, R. E. Matteri, and J. W. Frymoyer. Experimental measurements of vertebral motion under load. Orthop. Clin. N. Am. 8:155–167, 1977.
Quack, C., P. Schenk, T. Laeubli, S. Spillmann, J. Hodler, B. A. Michel, and A. Klipstein. Do MRI findings correlate with mobility tests? An explorative analysis of the test validity with regard to structure. Eur. Spine J. 16:803–812, 2007.
Quint, U., and H. J. Wilke. Grading of degenerative disk disease and functional impairment: imaging versus patho-anatomical findings. Eur. Spine J. 17:1705–1713, 2008.
Rolander, S. D. Motion of the lumbar spine with special reference to the stabilizing effect of posterior fusion: an experimental study on autopsy specimens. 1966. https://doi.org/10.3109/ort.1966.37.suppl-90.01.
Rousseau, M. A., D. S. Bradford, T. M. Hadi, K. L. Pedersen, and J. C. Lotz. The instant axis of rotation influences facet forces at L5/S1 during flexion/extension and lateral bending. Eur. Spine J. 15:299–307, 2006.
Rozumalski, A., M. H. Schwartz, R. Wervey, A. Swanson, D. C. Dykes, and T. Novacheck. The in vivo three-dimensional motion of the human lumbar spine during gait. Gait Posture 28:378–384, 2008.
Sakamaki, T., S. Katoh, and K. Sairyo. Normal and spondylolytic pediatric spine movements with reference to instantaneous axis of rotation. Spine (Phila. Pa. 1976) 27:141–145, 2002.
Saleem, S., H. M. Aslam, M. A. K. Rehmani, A. Raees, A. A. Alvi, and J. Ashraf. Lumbar disc degenerative disease: disc degeneration symptoms and magnetic resonance image findings. Asian Spine J. 7:322–334, 2013.
Samartzis, D., et al. Is lumbar facet joint tropism developmental or secondary to degeneration? An international, large-scale multicenter study by the AOSpine Asia Pacific Research Collaboration Consortium. Scoliosis Spinal Disord. 11:9, 2016.
Saraste, H., L. A. Brostrom, and T. Aparisi. Prognostic radiographic aspects of spondylolisthesis. Acta Radiol. Diagn. (Stockh.) 25:427–432, 1984.
Schmidt, H., F. Heuer, L. Claes, and H. J. Wilke. The relation between the instantaneous center of rotation and facet joint forces—a finite element analysis. Clin. Biomech. 23:270–278, 2008.
Schneider, G., M. J. Pearcy, and N. Bogduk. Abnormal motion in spondylolytic spondylolisthesis. Spine (Phila. Pa. 1976) 30:1159–1164, 2005.
Seligman, J. V., S. D. Gertzbein, M. Tile, and A. Kapasouri. Computer analysis of spinal segment motion in degenerative disc disease with and without axial loading. Spine (Phila. Pa. 1976) 9:566–573, 1984.
Serena S. Hu, MD, Clifford B. Tribus, MD, Mohammad Diab, MD, and Alexander J. Ghanayem, M. Spondylolisthesis and Spondylolysis. Pain 57:655–671, 2007.
Serhan, H. A., G. Varnavas, A. P. Dooris, A. Patwadhan, and M. Tzermiadianos. Biomechanics of the posterior lumbar articulating elements. Neurosurg. Focus 22:E1, 2007.
Shahidi, B., J. C. Hubbard, M. C. Gibbons, S. Ruoss, V. Zlomislic, R. T. Allen, S. R. Garfin, and S. R. Ward. Lumbar multifidus muscle degenerates in individuals with chronic degenerative lumbar spine pathology. J. Orthop. Res. 35:2700–2706, 2017.
Shin, J. H., S. Wang, Q. Yao, K. B. Wood, and G. Li. Investigation of coupled bending of the lumbar spine during dynamic axial rotation of the body. Eur. Spine J. 22:2671–2677, 2013.
Shirazi-Adl, A., A. M. Ahmed, and S. C. Shrivastava. Mechanical response of a lumbar motion segment in axial torque alone and combined with compression. 1986.
Simon, P., A. A. E. Orías, G. B. J. Andersson, H. S. An, and N. N. Inoue. In vivo topographic analysis of lumbar facet joint space width distribution in healthy and symptomatic subjects. Spine (Phila. Pa. 1976) 37:1058–1064, 2012.
Stokes, I. A., and J. W. Frymoyer. Segmental motion and instability. Spine (Phila. Pa. 1976) 12:688–691, 1987.
Takayanagi, K., K. Takahashi, M. Yamagata, H. Moriya, H. Kitahara, and T. Tamaki. Using cineradiography for continuous dynamic-motion analysis of the lumbar spine. Spine (Phila. Pa. 1976) 26:1858–1865, 2001.
Tallroth, K., H. Alaranta, and A. Soukka. Lumbar mobility in asymptomatic individuals. J. Spinal Disord. 5:481–484, 1992.
Tan, Y., B. G. Aghdasi, S. R. Montgomery, H. Inoue, C. Lu, and J. C. Wang. Kinetic magnetic resonance imaging analysis of lumbar segmental mobility in patients without significant spondylosis. Eur. Spine J. 21:2673–2679, 2012.
Tanaka, N., H. S. An, T. H. Lim, A. Fujiwara, C. H. Jeon, and V. M. Haughton. The relationship between disc degeneration and flexibility of the lumbar spine. Spine J. 1:47–56, 2001.
Teichtahl, A. J., D. M. Urquhart, Y. Wang, A. E. Wluka, R. O’Sullivan, G. Jones, and F. M. Cicuttini. Lumbar disc degeneration is associated with Modic change and high paraspinal fat content—a 3.0T magnetic resonance imaging study. BMC Musculoskelet. Disord. 17:1–7, 2016.
Teyhen, D. S., T. W. Flynn, J. D. Childs, T. R. Kuklo, M. K. Rosner, D. W. Polly, and L. D. Abraham. Fluoroscopic video to identify aberrant lumbar motion. Spine (Phila. Pa. 1976) 32:E220–E229, 2007.
Thomopoulos, C., G. Parati, and A. Zanchetti. Effects of blood pressure lowering on outcome incidence in hypertension: 7. Effects of more vs. less intensive blood pressure lowering and different achieved blood pressure levels - Updated overview and meta-analyses of randomized trials. J. Hypertens. 34:613–622, 2016.
Torgerson, W. R., and W. E. Dotter. Comparative Roentgenographic study of the asymptomatic and symptomatic lumbar spine. J. Bone Jt Surg. Am. 58:850–853, 1976.
Vernon-Roberts, B., and C. J. Pirie. Degenerative changes in the intervertebral discs of the lumbar spine and their squeletae. Rheumatol. Rehabil. 16:13–21, 1977.
Volkheimer, D., M. Malakoutian, T. R. Oxland, and H. J. Wilke. Limitations of current in vitro test protocols for investigation of instrumented adjacent segment biomechanics: critical analysis of the literature. Eur. Spine J. 24:1882–1892, 2015.
Wachowski, M. M., T. Hawellek, J. Hubert, A. Lehmann, M. Mansour, C. Dumont, J. Dörner, B. W. Raab, D. Kubein-Meesenburg, and H. Nägerl. Migration of the instantaneous axis of motion during axial rotation in lumbar segments and role of the zygapophysial joints. Acta Bioeng. Biomech. 12:39–46, 2010.
Wang, S., P. Passias, G. Li, G. Li, and K. Wood. Measurement of Vertebral Kinematics Using Noninvasive Image Matching Method – Validation and Application. Spine (Phila Pa 1976) 33:355–361, 2008.
Weiner, D. K., B. Distell, S. Studenski, S. Martinez, L. Lomasney, and D. Bongiorni. Does radiographic osteoarthritis correlate with flexibility of the lumbar spine? J. Am. Geriatr. Soc. 42:257–263, 1994.
White 3rd, A. A., and M. M. Panjabi. The basic kinematics of the human spine. A review of past and current knowledge. Spine (Phila Pa 1976) 3:12–20, 1978.
White, A. A., and M. Panjabi. Clinical Biomechanics of the Spine, 2nd ed. Philadelphia: Lippincott 2:18–20, 1990.
Wong, K., K. Luk, J. Leong, S. Wong, and K. Wong. Continuous Dynamic Spinal Motion Analysis. Spine (Phila. Pa. 1976). 31:414–419, 2006.
Wong, K. W. N., J. C. Y. Leong, M. Chan, K. D. K. Luk, and W. W. Lu. The flexion-extension profile of lumbar spine in 100 healthy volunteers. Spine (Phila. Pa. 1976). 29:1636–1641, 2004.
Wood, K. B., C. A. Popp, E. E. Transfeldt, and A. E. Geissele. Radiographic evaluation of instability in spondylolisthesis. Spine (Phila. Pa. 1976). 19:1697–703, 1994.
Wu, M., S. Wang, S. J. Driscoll, T. D. Cha, K. B. Wood, and G. Li. Dynamic motion characteristics of the lower lumbar spine: implication to lumbar pathology and surgical treatment. Eur. Spine J. 23:2350–2358, 2014.
Xia, Q., S. Wang, M. Kozanek, P. Passias, K. Wood, and G. Li. In-vivo motion characteristics of lumbar vertebrae in sagittal and transverse planes. J. Biomech. 43:1905–1909, 2010.
Yao, Q., S. Wang, J. Shin, G. Li, and K. B. Wood. Lumbar facet joint motion in patients with degenerative spondylolisthesis. J. Spinal Disord. Tech. 26:E19–E27, 2013.
Yoshioka, T., H. Tsuji, N. Hirano, and S. Sainoh. Motion characteristic of the normal lumbar spine in young adults: instantaneous axis of rotation and vertebral center motion analyses. J. Spinal Disord. Tech. 3:103–113, 1990.
Zhang, Y. H., C. Q. Zhao, L. S. Jiang, X. D. Chen, and L. Y. Dai. Modic changes: a systematic review of the literature. Eur. Spine J. 17:1289–1299, 2008.
Zirbel, S. A., D. K. Stolworthy, L. L. Howell, and A. E. Bowden. Intervertebral disc degeneration alters lumbar spine segmental stiffness in all modes of loading under a compressive follower load. Spine J. 13:1134–1147, 2013.
Acknowledgment
The authors gratefully acknowledge Maria-Rosa Fasser’s contribution in editorial assistance.
Conflict of interest
No potential conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Dan Elson oversaw the review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
(Angular/Translational) Segmental Motion Contribution
Maximal Range of Motion
Coupling
Center of Rotation
Phase Lag
Disc Degeneration
Mechanical Stiffness
Segmental and overall ROM
See Fig. 18 and Tables 7 and 8.
Facet Joint Osteoarthrosis
Facet Joint Tropism
Spondylolisthesis
Ligament Degeneration
Paraspinal Muscle Degeneration
Rights and permissions
About this article
Cite this article
Widmer, J., Fornaciari, P., Senteler, M. et al. Kinematics of the Spine Under Healthy and Degenerative Conditions: A Systematic Review. Ann Biomed Eng 47, 1491–1522 (2019). https://doi.org/10.1007/s10439-019-02252-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-019-02252-x