Abstract
Purpose
To analyze the effects of mobility of degenerated disc in the lower lumbar discs (L4–5 and L5–S1) on both whole lumbar motion and adjacent segment ROM.
Methods
The kMRIs with disc degeneration at L4–5 or L5–S1 were classified into three groups: the normal group, the motion-preserved (MP) group and the motion-lost (ML) group based on range of motion (ROM) of 5° in the degenerated segment. Each segmental ROM, whole lumbar motion, and the contribution % of the upper lumbar spine (ULS: L1–2–3) and the lower lumbar spine (LLS: L4–5–S1) motion to whole lumbar motion were measured and compared with each of the other groups.
Results
There were 94, 99 and 66 patients in the normal group, MP group and ML group, respectively. The normal group showed no significant difference compared to the MP group in all ROM parameters. The ML group showed significantly less whole lumbar motion, more contribution % in the ULS and less in the LLS than the normal and the MP groups. The ROM in the superior adjacent segment in the ML group was not significantly different between that in the normal and MP group.
Conclusions
Degenerated lumbar discs did not show hypermobility within functional ROM. Loss of segmental ROM from advanced disc degeneration did not cause an increase in the ROM of the superior adjacent segment in vivo. When the LLS had motion-lost, advanced disc degeneration, whole lumbar motion was significantly decreased and compensatory increase in ROM was accomplished by the ULS.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Traditionally, the scientific literature has described the degenerative changes of intervertebral discs (IVDs) in terms of the three sequential stages that were described in a study of autopsy findings by Kirkaldy-Willis and Farfan [1]: (1) temporary dysfunction, (2) unstable phase and (3) stabilization. In other words, the early stages of IVD degeneration produce instability of the segment. This process has been supported by a variety of radiographic findings and biomechanical studies of cadavers [2–4]. Additionally, recent in vivo analyses of the lumbar spine using kinetic magnetic resonance imaging (kMRI), which evaluates segmental range of motion (ROM) in a weight-bearing functional position, have shown that IVD degeneration increases segmental ROM and translation [5–9].
As the degenerative changes progress, however, the IVD space is lost and the instability is reduced by osteophyte formation and hypertrophy of the facet joints, progressively inducing stability. Although this ‘stabilization phase’ could have different influence on the motion of the whole lumbar spine, as well as the adjacent segments, there has been no comparative data available.
The hypothesis of this study is that the whole lumbar motion could show different patterns according to the mobility of the degenerated disc in the lower lumbar spine, and the stabilized segment with advanced disc degeneration may not show compensatory increase of ROM in the adjacent segment in vivo. We aimed to analyze the effects of mobility of degenerated disc in the lower lumbar spine discs (L4–5 and L5–S1) on both whole lumbar motion and adjacent segment ROM.
Materials and methods
Participants
KMRI of the lumbar spine were consecutively obtained over a 6-month period from September 2005 to February 2006 at an MRI institute. In this study, 600 patients (3,000 motion segments) with low back pain (398 men, 202 women) with or without leg pain were enrolled. The mean age was 46.2 years (range 21–76 years). All patients underwent kMRI for segmental motion of the lumbar spine in the 60° flexion, neutral and 20° extension in standing, weight-bearing position. The range of flexion and extension was limited with a control bar. Patients with transitional vertebra, coronal plane deformity, spondylolisthesis, trauma, tumor, infection, or those who had a lumbar spine operation due to any disease were excluded from this study. Each patient was screened by the authors for preexisting lumbar spine pathology or operation history. All the patients signed an approved informed consent form.
Measurement of motion
All examinations were performed on kMRI with a field strength of 0.6 T (Upright Multi-Position; Fonar Corp, New York, NY) using a flexible surface coil. The imaging protocol included sagittal T1-weighted spin-echo sequences (repetition time/echo time, 671/17 ms; slice thickness, 3.0 mm; field of view, 24 cm; matrix, 256 × 200; and number of excitation 2) and T2-weighted fast spin-echo sequences (repetition time/echo time, 3,432/160 ms; slice thickness, 3.0 mm; field of view, 24 cm; and number of excitation 2). Two segmental motions were measured at flexion and extension positions in the sagittal plane. The data obtained from the MR images were recorded on a computer for subsequent measurements and all calculations were automatically performed utilizing a software package (MRI Analyzer Version 3, Truemeric Corp, Bellflower, CA).
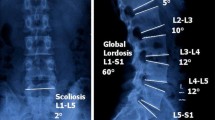
Segmental motion was defined as a sum of two segmental angles between each vertebral body in flexion and extension. This was measured by drawing lines along the superior borders of the upper vertebra of each motion segment and extending them until they cross (Fig. 1). In addition to measuring segmental motion at five spinal levels (L1–2, L2–3, L3–4, L4–5 and L5–S1), the whole lumbar motion which indicates the overall segmental motion from L1 to L5 was defined by the following formula: whole lumbar motion = L1–2 + L2–3 + L3–4 + L4–5 + L5–S1 segmental motion. The proportion of total lumbar motion contributed by each segment of the spine was measured (% of whole lumbar motion): that is, the contributions (% ROM) of the upper lumbar segments (L1–2–3, ULS) and the lower lumbar segments (L4–5–S1, LLS) to whole lumbar motion were measured.
To analyze the interobserver and intraobserver reliability, we analyzed intraclass correlation coefficients (ICC) for the measured value of 30 randomly selected cases by two observers.
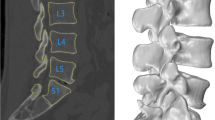
Classification of the groups
Grade 1 and 2 degenerative changes, according to the system of Pfirrmann et al. [10] were classified as normal. IVD graded as 3 or 4, with segmental motion >5°, were classified as motion-preserved (MP) degenerated discs, and IVD of grade 4 or 5 degeneration with segmental motion of <5° were classified as motion-lost (ML) degenerated discs. Of the 600 patients, we excluded 337 patient with multilevel MP degenerated disc without ML disc, multilevel ML disc and single level ML disc with segmental motion >5°. There was no degenerated disc of grade 4 in the ML group.
We classified the final 263 patients into three groups: the normal group, the MP group and the ML group. To be classified into the normal group, all segments must have had normal discs. If a single segment of the LLS (either L4–5 or L5–S1) had a MP disc and the other IVDs were normal, the patient was classified into the L4–5 MP or L5–S1 MP group, and patients in whom a single segment of the LLS was a ML disc and the other IVDs were normal or MP disc were classified into the L4–5 ML or L5–S1 ML group.
The results of the three groups were compared. To analyze the influence of the mobility of each degenerated disc, we compared the normal group, L4–5 MP group and L4–5 ML group first and then compared the normal group with L5–S1 MP and L5–S1 ML group in the next step (Fig. 2).
Next, we analyzed the differences in the segmental motion on superior adjacent segments according to their grade of degeneration in the ML group (L4–5 segmental motion in the L5–S1 ML group and L3–4 segmental motion in the L4–5 ML group, Figs. 3 and 4). Statistical analysis was performed using SPSS software (version 12, SPSS Inc., Chicago, IL). ANOVA with Tukey’s B post hoc analysis was used to compare the three groups, and Student’s t test and Mann–Whitney U test were performed to compare the superior adjacent segment ROM, with a significance level of 0.05.
Results
Interobserver ICC were 0.77 (0.68–0.93), while intraobserver ICC were 0.87 (0.82–0.96). The reliability was excellent (>0.7) for measurement of the segmental motion.
Within the normal group, there were 94 patients (M:F = 50:44, mean age 32.8 years). The MP group consisted of 99 patients (M:F = 67:32, mean age 40 years) and there were 28 L4–5 MP and 71 L5–S1 MP patients. Within the ML group with 66 patients (M:F = 45:21, mean age 50.2 years), there were 17 L4–5 ML and 49 L5–S1 ML patients. There was no significantly different sex ratio in the MP and ML group (p = 0.184), but the mean age was significantly different in all three groups (p < 0.001).
Within the 49 patients in the L5–S1 ML subgroup, there were 17 with normal L4–5 discs and 32 with degenerated L4–5 discs. Within the 17 patients in the L4–5 ML subgroup, there were 5 with normal L3–4 discs and 12 with degenerated L3–4 discs.
Comparison of the normal group, the L4–5 MP group and the L4–5 ML group (Table 1; Fig. 5)
The mean L4–5 segmental ROM, whole lumbar ROM and mean age was 9.3°, 41.3° and 32.8 years in the normal group, 8.4°, 36.1° and 42.3 years in the L4–5 MP group, and 3°, 25°, 54.2 years in the L4–5 ML group, respectively. The L4–5 segmental ROM and whole lumbar ROM showed no significant difference between the normal and MP group, but significant difference between the normal and ML, MP and ML group (p = 0.003 and <0.001, respectively). Mean age showed significant difference between all three groups (p <0.001).
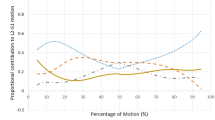
The mean upper (L1–2–3):lower (L4–5–S1) lumbar segmental % ROM was 40.2:36.6 % in the normal group, 38.1:40.1 % in the MP group and 46.3:27.7 % in the ML group. The difference was not significant between the normal and MP group, but significant between the normal and ML, and MP and ML group (p = 0.036 for ULS and 0.006 for LLS respectively). The mean ROM of L1–2 was 7° (17 %) in the normal group, 6.7° (18.8 %) in the MP group and 5.8° (25.3 %) in the ML group. Significant hypermobility of L1–2 was found only in the ML group (p = 0.017).
Comparison of the normal, L5–S1 MP and L5–S1 ML groups (Table 2; Fig. 6)
The mean L5–S1 segmental ROM, whole lumbar ROM and mean age was 6.3°, 41.3° and 32.8 years in the normal group, 6.5°, 39°, 35.8 years in the L5–S1 MP group and 2.2°, 32.2° and 48.8 years in the L5–S1 ML group, respectively. The L5–S1 segmental ROM and whole lumbar motion showed no significant difference between the normal and MP group, but significant difference between the normal and ML, MP and ML groups (p < 0.001 and <0.001 respectively). Mean age showed significant difference between the three groups (p < 0.001).
Comparison of segmental range of motion and percentage of whole lumbar motion between the normal, L5–S1 MP and L5–S1 ML groups. Likewise L4–5 groups, there was no significant difference between the normal and MP group in all parameters. The only significant difference was found in L1–2 and L5–S1 ROM of the ML group
The mean upper:lower lumbar segmental ROM was 40.2:36.6 % in the normal group, 40.3:38.2 % in the MP group and 45.4:31.5 % in the ML group. The difference was only significant between the normal and ML, MP and ML groups (p = 0.037 for ULS and 0.011 for LLS respectively). The mean ROM of L1–2 was 7° (17 %) in the normal group, 6.5° (18 %) in the L5–S1 MP group and 6.7° (22.6 %) in the L5–S1 ML group. There was a significant hypermobility of L1–2 only in the ML group (p = 0.008).
Comparison of ROM in the superior adjacent segment of the degenerated discs
L3–4 of the subgroups with degenerated L4–5 disc (Table 3)
The mean ROM % (proportion % to whole lumbar motion) of the L3–4 showed no significant difference in the three groups: 9.5° (23.2 %) in the normal group, 7.1° (26 %) in the L4–5 MP group and 8.2°(21.8 %) in the L4–5 ML group (p = 0.411). The mean L3–4 ROM in the L4–5 ML group was 7° (23.1 %) when the L3–4 IVD was a normal disc. This result did not differ significantly from the mean L3–4 ROM of 7.1° (26.9 %) when L3–4 was a degenerated disc.
L4–5 of the subgroups with degenerated L5–S1 disc (Table 3)
The mean ROM (proportion % to whole lumbar motion) of the L4–5 showed no significant difference in the three groups: 9.3° (21.6 %) in the normal group, 8.7° (22 %) in the MP group and 8.1° (23.8 %) in the ML group (p = 0.173). The mean L4–5 ROM in the L5–S1 ML group was 8.7° (25.1 %) when the L4–5 IVD was a normal disc and did not differ significantly from the mean L4–5 ROM of 7.8° (23.1 %) when L4–5 was a degenerated disc.
Discussion
To date, most studies of degenerative changes and segmental spinal motion have focused on degenerated discs with low signal intensity, with or without partial loss of disc height and segmental instability [2–9] (i.e., dysfunction or unstable phase by Kirkaldy-Willis and Farfan [1]). However, the mobility of degenerated disc could be variable; there has been no study comparing the normal and degenerated segments with variable degree of mobility. In addition, the traditional radiographs in lateral recumbent, maximal flexion–extension position may not be helpful in determining ROM in a weight-bearing, functional position, taking into consideration the tension on the paraspinal muscles and ligaments [11–15]. Previous studies examining cadavers or maximal flexion–extension radiographs of lumbar spines have demonstrated that range of segmental motion in the lumbar spine becomes larger in the lower segments (L4–5, L5–S1) as compared to upper segments (L1–2, 2–3) [16, 17]. On the contrary, the results of studies based on the weight-bearing, functional position or kMRI reported larger ROM in the upper or mid lumbar segments (L2–3, 3–4) than LLS (L4–5 or L5–S1) [18, 19]. This is the background of the present comparative study using kMRI.
Although the ROM required for functional status or for activities of daily living (ADLs) has not been clearly delineated, the maximal ROM of the lumbar spine is not required in most cases. Additionally, existing biomechanical studies have reported that in the initial 60° of lumbar flexion, an increase in the tension of the gluteus maximus muscle limited flexion of the hip joint. However, advancing lumbar flexion beyond 60° causes hip flexion, which contributes to flexion of the whole trunk [20, 21]. Thus, we inferred that a motion of 60° trunk flexion and 20° extension in a weight-bearing standing position would be able to reflect the amount of functional lumbar motion required for ADLs.
In the present study, there was no significant difference between the normal group and the MP group in all ROM parameters, and only the ML group showed significantly less whole lumbar motion, more ROM % in the ULS and less ROM % in the LLS than the other groups. The ROM in the superior adjacent segment in the ML group was not significantly different between that in the normal and the MP group regardless of the degenerative change of the superior adjacent segments
In previous studies on the influence of disc degeneration on segmental ROM, degenerative discs have been reported to experience instability initially and then become more stable in later stages [2–9, 22]. Other studies, however, have shown opposite results. For example, Nachemson et al. [23] found that segmental ROM was not related to the degree of degenerative change. Interestingly, while most studies suggesting a contribution of disc degeneration to biomechanical instability were performed on cadavers, most studies suggesting that there are no correlations between degenerative changes and segmental motion have been conducted utilizing in vivo radiographs, biomechanical study using follower load or kMRI [19, 24, 25].
The first important finding of our study was the difference in whole lumbar ROM between the normal group and the ML group. The normal group had a whole lumbar ROM of 41.3°, which was significantly more than the ROM of 25.1° seen in the L4–5 ML group and the ROM of 32.2° seen in the L5–S1 ML group. The mean age also differed significantly, implying that aging and local degenerative changes in the lumbar spine act together to decrease whole lumbar motion. These differences indicate that the lumbar spine does not inherently compensate for the lost ROM associated with degenerative changes with hypermobility of the adjacent segment, but rather reduced lumbar motion could be compensated by the segmental motion close to the thoracolumbar junction or ROM at the hip joints to produce the same amount of trunk motion.
Another interesting point is that the segment just superior and adjacent to the ML segment did not exhibit a significant increase in ROM. The L4–5 ML group and the normal group did not differ significantly in the contribution of L3–4 to lumbar motion of the whole spine and the absolute value for L3–4 ROM with L4–5 ML was actually smaller. Similarly, the ROM of the L4–5 segment in the L5–S1 ML group was not increased. On the other hand, a comparison of L1–2 ROM in the ML group with the normal and MP groups revealed that ROM was increased in all cases of the ML group. This result suggests that the upper lumbar spine compensates for decreases in whole lumbar ROM, rather than simply the superior adjacent segments. This result might be contrary to the results of various existing biomechanical studies which showed increased segmental motion adjacent to motion-lost segment and their contribution of the development of adjacent segment disease [26–28].
Several limitations of this study should be noted. Although this study is the first to analyze the effects of the mobility of degenerated disc on the whole lumbar motion, there is no established criteria of ‘motion-lost’ segment. We used 5° of ROM to define the ML segment. This is a commonly used radiological criterion to assess lumbar fusion or progression of deformity; however, these results cannot be universally applied to cases where motion is lost as a result of surgical fusion. Secondly, we noted a significant age difference between the ML group and the other groups. Although it is not surprising that older individuals would have more advanced degeneration, we did not account for other degenerative findings such as facet degeneration or ligamentum flavum hypertrophy, which could also affect the lumbar motion segment. Nonetheless, these other degenerative findings often go hand in hand with disc degeneration and therefore are independent of age.
The result of the present study provides baseline information in understanding the characteristics of total lumbar motion based on segmental mobility of degenerated discs and should be considered when planning for lumbar fusion or motion-preserving surgery.
Conclusions
Unlike previous in vitro studies, degenerated lumbar discs did not show hypermobility within functional ROM. Loss of segmental ROM from advanced disc degeneration did not cause an increase in the ROM of the superior adjacent segment in vivo. When the LLS had motion-lost, advanced disc degeneration, whole lumbar motion was significantly decreased and compensatory increase in ROM was accomplished by the ULS.
References
Kirkaldy-Willis WH, Farfan HF (1982) Instability of the lumbar spine. Clin Orthop 165:110–123
Fujiwara A, Lim TH, An HS, Tanaka N, Jeon CH, Andersson GB, Haughton VM (2000) The effect of disc degeneration and facet joint osteoarthritis on the segmental flexibility of the lumbar spine. Spine 25:3036–3044
Rohlmann A, Zandera T, Schmidta H, Wilke HJ, Bergmann G (2006) Analysis of the influence of disc degeneration on the mechanical behaviour of a lumbar motion segment using the finite element method. J Biomech 39:2484–2490
Zhao F, Pollintine P, Hole BD, Dolan P, Adams MA (2005) Discogenic origins of spinal instability. Spine 30:2621–2630
Karamidas EJ, Sidduqui M, Smith FW, Wardlaw D (2000) Positional MRI changes in supine versus sitting postures in patients with degenerative lumbar spine. J Spinal Dis 13:444–450
Jinkins JR, Dworkin JS, Damadian RV (2005) Upright, weight-bearing, dynamic–kinetic MRI of the spine: initial results. Eur Rad 15:1815–1825
Kong MH, Morishita Y, He W, Miyazaki M, Zhang H, Wu G, Hymanson HJ, Wang JC (2009) Lumbar segmental mobility according to the grade of the disc, the facet joint, the muscle, and the ligament pathology by using kinetic magnetic resonance imaging. Spine 34:2537–2544
Kong MH, Hymanson HJ, Song KY, Chin DK, Cho YE, Yoon DH, Wang JC (2009) Kinetic magnetic resonance imaging analysis of abnormal segmental motion of the functional spine unit. J Neurosurg Spine 10(4):357–365
Keorochana G, Taghavi CE, Lee KB, Yoo JH, Liao JC, Fei Z, Wang JC (2011) Effect of sagittal alignment on kinematic changes and degree of disc degeneration in the lumbar spine. Spine 36:893–898
Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N (2001) Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine 26:1873–1878
Barker PJ, Guggenheimer KT, Grkovic I, Briggs CA, Jones DC, Thomas CD, Hodges PW (2006) Effects of tensioning the lumbar fasciae on segmental stiffness during flexion and extension. Spine 31:397–405
Botsford DJ, Esses SI, Ogilvie-Harris DJ (1994) In vivo diurnal variation in intervertebral disc volume and morphology. Spine 19:935–940
Quint U, Wilke HJ, Shirazi-Adl A, Parnianpour M, Löer F, Claes LE (1998) Importance of the intersegmental trunk muscles for the stability of the lumbar spine: a biomechanical study in vitro. Spine 23:1937–1945
Hodges P, Kaigle HA, Holm S, Ekström L, Cresswell A, Hansson T, Thorstensson A (2003) Intervertebral stiffness of the spine is increased by evoked contraction of transversus abdominis and the diaphragm: in vivo porcine studies. Spine 28:2594–2596
Cunningham BW, Kotani Y, McNulty PS, Cappuccino A, McAfee PC (1997) The effect of spinal destabilization and instrumentation on lumbar intradiscal pressure: an in vitro biomechanical analysis. Spine 22:2655–2663
Hayes MA, Howard TC, Gruel CR, kopta JA (1989) Roentgenographic evaluation of lumbar spine in asymptomatic individuals. Spine 14:327–332
White AA, Panjabi MM (1990) Clinical biomechanics of the spine, 2nd edn. Lippincott Williams and Wilkins, Philadelphia
Miyasaka K, Ohmori K, Suzuki K, Inoue H (2000) Radiographic analysis of lumbar motion in relation to lumbosacral stability; Investigation of moderate and maximum motion. Spine 25:732–737
Tan Y, Aghdasi BG, Montgomery SR, Inoue H, Lu C, Wang JC (2012) Kinetic magnetic resonance imaging analysis of lumbar segmental mobility in patients without significant spondylosis. Eur Spine J 21:2673–2679
Clayson SJ, Newman IM, Debevec DF, Anger RW, Skowlund HV, Kottke F (1962) Evaluation of mobility of hip and lumbar vertebrae of normal young women. Arch Phys Med 43:1–8
Esola MA, McClure PW, Fitzgerald GK, Siegler S (1996) Analysis of lumbar spine and hip motion during forward bending in subjects with and without a history of low back pain. Spine 21:71–78
Rohlman A, Neller S, Bergmann G, Graichen F, Claes L, Wilke HJ (2001) Effect of an internal fixator and a bone graft on intersegmental spinal motion and intradiscal pressure in the adjacent regions. Eur Spine J 10:301–308
Nachemson A, Schultz AB, Berkson MH (1979) Mechanical properties of human lumbar spine motion segments. Part II: influence of age, sex, disc level, and degeneration. Spine 4:1–8
Simpson AK, Biswas D, Emerson JW, Lawrence BD, Grauer JN (2008) Quantifying the effects of age, gender, degeneration, and adjacent level degeneration on cervical spine range of motion using multivariate analyses. Spine 33:183–186
Zirbel SA, Stolworthy DK, Howell LL, Bowden AE (2013) Intervertebral disc degeneration alters lumbar spine segmental stiffness in all modes of loading under a compressive follower load. Spine J 13:1134–1147
Chow DHK, Luk KDK, Evans JH, Leong JCY (1996) Effects of short anterior lumbar interbody fusion on biomechanics of neighboring unfused segments. Spine 21:549–555
Guigui P, Lambert P, Lassale B, Deburge A (1997) Long-term outcome at adjacent levels of lumbar arthrodesis. Rev Chir Orthop Reparatrice Appar Mot 83:685–696
Nakai S, Yoshizawa H, Kobayashi S (1999) Long-term follow-up study of posterior lumbar interbody fusion. J Spinal Disord 12:293–299
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, SH., Daffner, S.D., Wang, J.C. et al. The change of whole lumbar segmental motion according to the mobility of degenerated disc in the lower lumbar spine: a kinetic MRI study. Eur Spine J 24, 1893–1900 (2015). https://doi.org/10.1007/s00586-014-3277-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-014-3277-z