Abstract
Cartilage and bone tissue engineering has been widely investigated but is still hampered by cell differentiation and transplant integration issues within the constructs. Scaffolds represent the pivotal structure of the engineered tissue and establish an environment for neo-extracellular matrix synthesis. They can be associated to signals to modulate cell activity. In this study, considering the well reported role of hydroxyapatite (HA) in cartilage repair, we focused on the putative chondrogenic differentiation of human mesenchymal stem cells (hMSCs) following culture on membranes of electrospun fibers of poly-l-lactic acid (PLLA) loaded with nanoparticles of HA. hMSCs were seeded on PLLA/HA and bare PLLA membranes and cultured in basal medium, using chondrogenic differentiation medium as a positive control. After 14 days of culture, SOX-9 positive cells could be detected in the PLLA/HA group. Cartilage specific proteoglycan immunostain confirmed the presence of neo-extracellular-matrix production. Co-expression of CD29, a typical surface marker of MSCs and SOX-9, suggested different degrees in the differentiation process. We developed a hydroxyapatite functionalized scaffold with the aim to recapitulate the native histoarchitecture and the molecular signaling of osteochondral tissue to facilitate cell differentiation toward chondrocyte. PLLA/HA nanocomposites induced differentiation of hMSCs in a chondrocyte-like phenotype with generation of a proteoglycan based matrix. This nanocomposite could be an amenable alternative scaffold for cartilage tissue engineering using hMSCs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tissue engineering of bone and cartilage is emerging as a promising therapeutic tool that aims not only to repair impaired tissues but also to fully regenerate them by combining cells, biomaterials mimicking extracellular matrix (scaffolds) and regulatory signals.28 Scaffolds represent the pivotal structure of the engineered tissue and establish an environment for the synthesis of neo-extracellular matrix (ECM). The scaffold component is expected to support cell colonization, migration, growth and differentiation, so that it guides the development of the required tissue. In parallel with tissue formation, the scaffold may undergo degradation through the release of by-products that are both biocompatible and active or can be excreted or subjected to metabolism.9 Addition of biological active signals as ECM components or growth factors to this main backbone have the potency to induce, support or enhance the growth and differentiation of various cell types towards the chondrogenic lineage and to orchestrate tissue repair effectively.64 Both natural and synthetic polymers can be used to create scaffolds that support cells and incorporate cues which guide tissue repair. During native wound healing processes, cells and molecules interact with extracellular matrix (ECM) components such as fibrous proteins and glycosaminoglycans. Several studies demonstrated that the ECM milieu surrounding the cell has physical and structural features in the nanometer scale, and that this arrangement may affect several aspects of cell behavior such as morphology, adhesion, and cytoskeletal arrangements.65,78,81 Thus a great effort has been done to fabricate synthetic materials into nanometer scale structures in attempts to simulate the matrix environment in which seeded cells can be accommodated to proliferate and differentiate towards desired lineages.26,48,56 Electrospinning is one of the approaches that allow the fabrication of synthetic materials into fibrous structures in the micro and nanometer scale.45,55 Electrospun fibers have been shown to mimic the ECM environment to various degrees when cultured with several cell types.7,33,37,49,53,61, 80 Poly(l-lactic acid) (PLLA) has been widely investigated in tissue engineering because of its good biocompatibility63,66,73 and is amenable to be modified with inorganic materials in order to improve its biological properties for tissue engineering purposes.34,35,54,58 In this extent, a variety of calcium phosphates have been used for bone engineering applications. Being similar to the mineral component of natural bone, hydroxyapatite (HA), and other calcium phosphates, e.g., tricalcium phosphate (β-TCP), are considered osteoconductive and bioactive materials allowing new bone formation and have gained wide use as bone substitutes in the clinical arena.6,25,38 Addition of HA in scaffold manufacturing has been largely investigated using different types of materials including natural polymers39,40,82 and synthetic polymers32,52,71 or combination of them.41–43 Ma et al. showed improved proliferation rate and higher expression of bone-specific markers in osteoblasts seeded in PLLA–HA scaffolds.47 These scaffolds of high porosity (>90%) and well-controlled pore architectures were prepared using thermally induced phase-separation (TIPS) techniques and aimed at better mimicking the mineral components and microstructure of natural bone. Wei and Ma pointed out the increased mechanical properties and improved protein adsorption capacity of nano-hydroxyapatite (NHA)–PLLA composite scaffolds.79 Poly-l-lactic acid (PLLA)/hydroxyapatite (HA) hybrid membranes have been fabricated via electrospinning of the PLLA/HA system obtained dispersing nano-powders of HA in a PLLA solution. This nanocomposite demonstrated to promote and facilitate osteoblast cell adhesion capability and growth and therefore to be a potential candidate for bone tissue engineering.22,67 Mineral chondral components, as hydroxyapatite and tricalcium phosphate have been shown to facilitate and promote cartilage regeneration.15,29,70 However, in these studies the effect of biphasic bone/cartilage constructs has been explored mainly obtaining differentiation toward bone rather than cartilage. Other tissue engineering approaches with collagen scaffolds,12 absorbable polymers,18,74 hydroxyapatite,16,68 and even interconnected porous composites of hydroxyapatite/biopolymers fabricated with gel foaming technique,69 have been used for articular cartilage repair. In this extent mature articular cartilage tissues that, owing to their low mitotic activity, cannot heal spontaneously, would better benefit from a stem cell therapy for regeneration purposes and mesenchymal stem cells (MSCs) have elicited substantial attention because they can be readily isolated and expanded ex vivo. However, literature does not provide sufficient evidences supporting their actual advantage over the already accepted treatment with mature chondrocytes. De Bari et al. showed inability of injected in vitro differentiated MSCs only to form ectopic stable cartilage in vivo.21 Indeed, current clinical practice is centered on implantation of autologous mature chondrocyte (ACI) or matrix-associated autologous chondrocyte transplantation/implantation (MACT/MACI), a new operation procedure using a cell seeded collagen matrix, for the treatment of localized full-thickness cartilage defects with effective clinical improvement over a five year period follow up.8 The association of living cells with biomaterials, providing a leading framework for tissue repair, is a potential attractive and effective alternative in the tissue engineering field. MSCs have fueled an increasing amount of research and interest as their amenable culturing and immunologic characteristics and they have been used for in vivo tissue engineering.19,30
Engineered tissue phenotypes from MSCs include osteochondral grafts with both cartilage and bone,1,3,14,31,50,51 adipose tissue,4 tendon and ligaments,57 and skeletal muscle.2,62 However, even if some success has been achieved in the repair of small osteochondral defects, no widely accepted method exists for the complete healing of hyaline cartilage. The cause of the failure lies not in the nature of the biomaterial itself but in its structure, which is not regulated three dimensionally.13,69,77
In the present work we developed a hydroxyapatite functionalized polymeric scaffold by mean of electrospinning with the aim to mimic the native histoarchitecture and the molecular signaling of osteochondral tissue to facilitate the differentiation of MSCs toward chondrocyte. We focused on the putative chondrogenic differentiation of hMSCs after a period of culture upon a membrane of electrospun fibers of poly-l-lactic acid (PLLA) loaded with nanoparticles of HA. This nanocomposite could be an amenable alternative for cartilage tissue engineering using undifferentiated bone marrow MSCs. This functionalized scaffold would provide both a surrogate of the native ECM and the correct sequence of signals to allow a harmonic ongoing lineage-specific differentiation of multipotent precursor cells.
Methods
Scaffold Preparation and Characterization
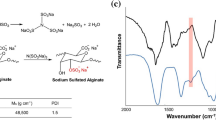
The PLLA/HA nanocomposite was prepared by electrospinning technique, starting from a dispersion of HA nanopowder in a PLLA solution. One gram of PLLA (MW 150 kDa, Aldrich) was dissolved in 5 mL of dichloromethane (Aldrich), and 0.1 g nanosized HA powder (particle size <200 nm Aldrich) was dispersed in the polymer solution under stirring.
The obtained suspension was transferred into a glass syringe, actuated by an infusion pump (KD Scientific) and fed through the needle, which was kept at a high DC voltage (15 kV, Gamma High Voltage generator) with respect to an earthed target facing the needle at a distance of 15 cm. This strong electric field at the tip of the needle caused a charged polymer jet to be extracted from the needle and driven to the collector as a continuous fiber, leading to the formation of a non-woven cloth on the collector surface.
In parallel, bare PLLA patches were obtained with the same experimental conditions to be used as reference.
Microstructure of the obtained membranes was evaluated by Field Emission Scanning Electron Microscopy (FE-SEM, Leo Supra 1535). Autofluorescence analysis on the polymer itself has been performed in order to assess potential biases or artefacts in further processing for immunostaining. Polymers were excited at different time points within a range spanning between 10 ms and 10 s and autofluorescence was detected under fluorescence microscope (Olympus).
Prior to cell culture tests, both PLLA and PLLA/HA patches were sterilized by soaking in absolute ethanol (Aldrich).46 All experiments have been performed in triplicate.
hMSCs Seeding and Culture
Human Mesenchymal Stem Cells (Lonza Biologics Inc.), at passage 2, were used in PLLA/HA sterilized scaffolds and engrafted with a static seeding technique. Similar experiments were performed on bare PLLA patches as a control for differentiation induction. Samples were punched out to disks 8 mm in diameter and placed into a 96-well plate. A standard static seeding was performed at the density of 500 × 103 cell/cm2 as previously described.36 Briefly, droplets of hMSC suspension were seeded and incubated for 6 h. Then 200 μL of the growth medium was added to each well and the constructs were cultured for 14 days either in basal medium (Dulbecco’s minimum essential medium (DMEM) supplemented with 10% fetal bovine serum (FBS), 100 UI/mL penicillin, 100 μg/mL streptomycin) or chondrogenic differentiation medium (Lonza Biologics Inc.). Media were changed every 2 days. Constructs were harvested at 3 days after seeding to assess cell attachment and at 14 days for MSC differentiation analysis. In consideration of the presence of HA, an additional set of experiments was performed for 21 days to evaluate possible osteogenic differentiation.
Cell Engraftment and Biological Assessments
Cell viability, toxicity, attachment, proliferation, and differentiation within the scaffolds have been evaluated by means immunohistology and confocal microscopy. For cell viability assessment a test, Live/Dead assay (Invitrogen), based on cellular membrane intactness was used. Percentage of death and unavailable cells have been calculated counting 200 cells in five randomly chosen microscopic fields at 10× magnification by two independent observers. Upon culturing, patches were fixed with paraformaldehyde (PFA) embedded in O.C.T. cryomatrix, snap frozen, and cut in 15 μm slices. Slides were further processed for Hematoxilin–Eosin staining in order to achieve a morphological analysis. For cell attachment and engraftment assessment was also used confocal microscopy staining cells on the scaffolds for F-Actin with Rhodamine Phalloidin (Molecular Probes) and nuclei using TOTO as nuclear counterstain.
Cell Proliferation and Differentiation Assessments
Fourteen days after seeding the membranes were embedded in O.C.T. cryomatrix, snap frozen, and cut. For cell proliferation slides were immunostained for Ki67 antibody (Neomarkers) and for differentiation with antibodies against CD29 and SOX-9 (Santa Cruz Biotechnology) as previously described.24 Briefly, tissue sections were fixed and permeabilized with 0.1% Triton-X 100 in PBS for 10 min. Non-specific binding of antibodies was blocked by incubating the samples for 45 min with 2% bovine serum albumin. Samples were then incubated 1 h at 37 °C with mouse monoclonal anti-CD29 (at the dilution of 1/100) and rabbit anti-SOX-9 (1/100), primary antibodies. For triple labeling experiments, samples were incubated with Alexa Fluor 488 conjugated secondary anti-mouse IgG and Alexa Fluor 546 conjugated secondary anti-rabbit IgG (Invitrogen) for 30 min at 37 °C. In negative control experiments the incubation with primary antibodies was omitted. Nuclei were counter-stained with TOTO (Invitrogen). The samples were then mounted in Prolong antifade medium (Invitrogen) and viewed under confocal microscopy using an Olympus Fluorview F1000 confocal microscope by two independent blinded observers. Percentage of proliferating cells, CD29 and Sox-9 positive cells and have been calculated counting 200 cells in five randomly chosen microscopic fields at 20× magnification.
Matrix Characterization
To assess matrix formation and cell penetration, Masson’s trichrome staining for collagen, Toluidine blue for proteoglycans and GAGs, and Saflanine O staining for cartilage were performed and samples were imaged under a light microscope (Olympus).
To better characterize neo-ECM, an immunostaining for Aggrecan, one of the major structural component of cartilage, particularly articular cartilage, was performed. Following fixation and permeabilization with 0.1% Triton-X 100 sections were incubated for 45 min with 2% bovine serum to block non-specific binding of antibodies. Samples were then incubated 1 h at 37 °C with monoclonal mouse anti-Aggrecan primary antibody at the dilution of 1/100 (Abcam) followed by an Alexa Fluor 488 conjugated secondary anti-mouse IgG. Additionally, double staining using both mouse anti-Aggrecan and rabbit anti-SOX-9 (1/100) primary antibodies was performed to further demonstrate chondrogenesis. For nuclear visualization, samples were counter-stained with TOTO and further mounted in antifade medium. Slides were imaged under an Olympus Fluorview F1000 confocal microscope by two independent blinded observers.
Intra- and extracellular calcium phosphate (PO4 3−) was detected using a standard von Kossa staining procedure that is typically utilized for the detection of calcium-phosphate mineralization and thus osteogenic differentiation on different biomaterials. Briefly, samples were rinsed with a cacodylic buffer (1 M cacodylic acid and 1 M NaOH in DI water) and then fixed in 2% paraformaldehyde in cacodylic buffer for 10 min at room temperature. Samples were then rinsed twice with DI water followed by exposure to a silver nitrate solution. In von Kossa procedure silver cations are involved in a substitution reaction, forming carbonate or phosphate salts, and then reduced to dark-colored silver metal staining.
Statistical Analysis
Data were processed using SPSS (Statistical Package for Social Sciences) release 13.0 for Windows (SPSS, Chicago). Data are presented as mean ± SD. One-way ANOVA was performed to compare groups with different treatments, followed by multiple pairwise comparison procedure (Tukey test). Assumptions of normality were checked and met. Holm–Sidak method was used to increase the power of the analysis. Pearson’s product-moment r coefficient was calculated to evaluate correlations. Significance was at the .05 level.
Results
Electrospinning Conditions and Scaffold Structural Evaluation
FE-SEM observation on PLLA/HA patches revealed a dispersion of HA nanopowder (particle diameter <200 nm) into the PLLA fibers (Fig. 1).
Fibers were porous, with elongated pores characterized by an average pore size of about 100 nm (Fig. 1). Autofluorescence analysis on the polymer itself has been performed in order to assess potential biases or artefacts in further processing for immunostaining. Samples were excited at different time points within a range spanning between 10 ms and 10 s. Scaffolds showed autofluorescence only after 8 ± 0, 4 s.
Cell Viability, Proliferation, Morphology and Differentiation
Live/Dead assay demonstrated a ≥90% cell viability in both PLLA and PLLA/HA scaffolds with the latter showing improved survival and an effective cell engrafting after 48 h culture. In the PLLA/HA samples, a significantly greater percentage of viable cells was detected, in comparison with the bare PLLA, both cultured in basal medium (97 ± 2% vs. 94 ± 1% p < 0.05) (Fig. 2a). Analogously, a significantly higher percentage of viable cells could be detected in the PLLA/HA group with respect to the PLLA one when cultured in chondrogenic medium. (Fig. 2a). Figure 2b shows cell proliferation in the experimental groups. A significant increase in cell proliferation could be noticed in the PLLA/HA functionalized scaffold in both basal and chondrogenic culture conditions in comparison with the matched bare PLLA constructs. Moreover, hMSCs cultured in PLLA/HA nanocomposite exhibited changes in expression of chondrogenic and stem cell markers with respect to PLLA control.
(a) Cell viability analysis by means of Live/Dead Assay (Invitrogen). Percent of viable cells is reported. (b) Cell proliferation analysis. Ki67 positive cells were counted out of 200 cells in five randomly chosen microscopic fields at 20× magnification. Cells have been cultured for 3 days. * Indicates level of significance p < 0.01
Hematoxylin–eosin staining confirmed engrafting, showing elongating cells attached on PLLA/HA fibers (Fig. 3a).
hMSCs cultured on PLLA/HA scaffold for 14 day in basal medium. (a) Haematoxylin Eosin staining revealing elongated cells in contact with PLLA/HA fibers. (b) Confocal microscopy. Staining for Alfa-actin and nuclear counterstain with TOTO. Note the spindled shape of a cell in PLLA/HA scaffold and its interaction with fibers
Three days after seeding, hMSCs were well adhered on the PLLA/HA fibers with a spindled shape (Fig. 3b). Light and confocal microscopy showed elongated cells with rare cytoplasm and a high nucleus/cytoplasm ratio. Nuclei appeared enlarged with loose chromatin and several nucleoli thus indicating conditions of non quiescence (Fig. 3a). After 14 days of culture, cells positive for the chondrogenic transcription factor SOX-9 in both basal and chondrogenic media groups in the PLLA/HA scaffolds, could be detected (Fig. 4). Interestingly, these results were comparable with the PLLA samples cultured with the chondrogenic medium, while culture in basal media failed to show chondrogenic markers expression in the bare PLLA samples (Fig. 4). Aggrecan immunostain localized surrounding cell clumps within the scaffold (Fig. 5). hMSCs were either CD29 positive or negative and double positive CD29-SOX-9 cells were observed, too (Fig. 4). The detected co-expression of CD29, a typical surface marker of hMSCs also expressed in chondrocytes, and SOX-9, a transcription factor associated with chondrogenesis, suggests chondrogenic differentiation.
hMSCs cultured on PLLA/HA scaffold for 14 days in basal medium. Confocal microscopy (a) PLLA alone scaffold cultured for 14 days in basal medium. (b) PLLA/HA scaffold cultured for 14 days in basal medium. Different degrees of hMSC differentiation as shown by co-expression of a mesenchymal stem lineage marker (CD29, green fluorescence) and SOX-9 (red fluorescence), a transcription factor associated with chondrogenesis (arrows). Total undetectable expression of CD29 possibly indicates further advances in the differentiation process (arrow heads) as the loss of expression in a stem cell marker. (c) At bottom, representative graph showing cell differentiation evaluation by means of mesenchymal stem cell (CD29) and chondrogenic (Sox-9) specific markers immunodetection. A significant statistical difference could be observed between PLLA and PLLA/HA samples treated in basal medium, as indicated by the asterisk between the respective column bars. No statistical differences could be found between PLLA/HA samples cultured in basal medium and PLLA alone samples cultured in chondrogenic medium. * Indicates level of significance p < 0.01
Confocal microscopy. Pure PLLA (a), PLLA/HA (b) cultured for 2 weeks in basal media. Co-expression of Aggregan (green fluorescence) and SOX-9 (red fluorescence), a transcription factor associated with chondrogenesis. Nuclear counterstain with TOTO (blue fluorescence). Aggrecan immunostaining demonstrating clumps of hMSCs immersed in a newly formed chondrogenic-related connective environment in the PLLA/HA scaffold (b)
Toluidine blue and Safranin O staining confirmed the presence of neo-extracellular-matrix produced around the cells (Fig. 6). A more intense deposition of proteoglycans and GAGs could be observed in the functionalized scaffold (Figs. 6a and 6c) in comparison to the bare PLLA polymers (Figs. 6b and 6d). To assess possible osteogenic differentiation related to the presence of HA, all samples were cultured for an additional week and stained for von Kossa to reveal presence of calcium phosphates. In all conditions tested, no significant presence of positive staining could be detected (Fig. 7). However, in the PLLA/HA groups, a minimal amount of calcium phosphates could be observed (Figs. 7c and 7d). In light of the fact that this findings could be noticed also in the positive chondrogenic control PLLA/HA samples, and the localization of the staining appeared to be extracellular and in close vicinity of the PLLA/HA fibers, these results are presumably to be referred to the presence of HA residuals on the scaffold itself. A similar experiment performed on the scaffold alone without cell seeding showed similar results (Figs. 7e and 7f).
Safranine O and Toloudine Blue staining for extracellular matrix. (a) Representative section stained with Safranin O of hMSCs seeded upon PLLA/HA and cultured for 2 weeks in basal media. (b) Representative section stained with Safranin O of hMSCs seeded upon PLLA alone and cultured for 2 weeks in basal media. The red staining represents the matrix produced around the cells (blue staining). Arrows indicate a PLLA/HA fiber. (c) Representative section stained with Toloudine Blue of the human MSC seeded upon PLLA/HA and cultured for 2 weeks in basal media. (d) Representative section stained with Safranin O of hMSCs seeded upon PLLA alone and cultured for 2 weeks in basal media. The blue staining represents the matrix produced around the cells (dark blue staining). Arrows indicate a PLLA/HA fiber. A more intense deposition of proteoglycans and GAGs could be observed in the functionalized scaffold (a, c) in comparison to the bare PLLA polymers (b, d)
Von Kossa staining for calcium phospate. (a) PLLA alone scaffold cultured with hMSC in basal medium for 21 days (Mag 400×). (b) PLLA alone scaffold cultured with hMSC in chondrogenic medium for 21 days (Mag 400×). (c) PLLA/HA scaffold cultured with hMSC in basal medium for 21 days (Mag 400×). (d) PLLA/HA scaffold cultured with hMSC in chondrogenic medium for 21 days (Mag 400×). (e) PLLA/HA scaffold not seeded with cells at low magnification (Mag 100×). (f) PLLA/HA scaffold not seeded with cells (Mag 400×). Neither PLLA alone nor PLLA/HA showed a significant presence of calcium phosphate. A minimal presence of staining could be noticed in the PLLA/HA scaffold cultured both in basal and in chondrogenic medium. Localization of the staining is clearly extracellular and adhered to fibers; the presence of calcium in the sample cultured in chondrogenic medium suggests the idea of deposits mainly derived from the scaffold itself, rather than a cellular deposition. Figure (e) and (f) confirm this hypothesis showing minimal amounts of calcium in the bare PLLA scaffold not seeded with cells (see Text)
Discussion
The synthesis of polymer composites with inorganic filler materials is well established; however, it is difficult to produce well-defined structures to increase their regenerative potential because most biomaterials containing inorganic phases are difficult to be manufactured and tailored to host living cells. The architecture of moulded materials, for example, is often detrimental in terms of cells penetration and proliferation. In this extent, electrospinning technology could represent an elective candidate to process natural biomaterials and synthetic biocompatible polymers for biomedical applications. The topology of electrospun scaffolds closely mimics the fibrillar structure of the ECM, and the cell adhesion and proliferation are enhanced on nanostructured scaffolds.
Recently, fabrication of electrospun PLLA/HA hybrid membranes by HA nanoparticles dispersion in PLLA polymer was attempted for bone tissue regeneration using a human osteoblast cell line with encouraging results in terms of tensile strength, cell adhesion, and growth.67 Cartilage, by contrast, is a non-vascular, turgid network, which supports chondrocytes spaced 10–200 μm apart. Hydrophilic proteoglycans, such as aggrecan, interwoven between networks of collagen II fibers, provide a shock-absorbing matrix. Given its low mitotic activity, mature articular cartilage cannot heal spontaneously, thus mandating for search of a cell type able to both repopulate tissue loss and reconstitute the connectival environment crucial for cartilage function. Nowadays, implantation of autologous mature chondrocyte (ACI), or matrix-associated autologous chondrocyte transplantation/implantation (MACT/MACI), for cartilage repair is well established and allows an effective strategy for cartilage repair. However, it requires highly specialized facilities and a turnaround time of about 4 or 5 weeks to ensure the appropriated cell expansion. Moreover, although the use of chondrocytes in applications of cartilage tissue engineering is still prevalent, concerns associated with donor-site morbidity, cell de-differentiation and limited lifespan of these cells have foreseen the use of MSCs as a potential tool to forefront of such applications.20 MSCs are considered a multipotent cell population endowed with high plasticity and low immunogenic potential that are readily available (i.e., bone marrow aspiration) and easily expandable in in vitro settings. Recent technological advances produced rapid and highly cost-effective systems, allowing for procedures of isolation and injection in the same clinical operative settings. Their low immunogenic profile could also enlighten new avenues on putative non-autologous stem cell therapy.5 Thus, because of their multipotency, easy isolation and culture, highly expansive potential, and immunoregulatory properties, these cells may be an attractive therapeutic tool for repairing purposes, especially for complex osteochondral defects. In fact, MSCs have recently claimed attention of connective tissue engineering and regenerative medicine and have become increasingly considered as a potential alternative cell source for improving well-established methods of osteochondrotic cartilage defect repair, such as the cited Autologous Chondrocyte Transplantation method. Moreover, MSCs are being evaluated as an alternative to patient-derived chondrocytes in combination with newly developed implantable scaffolds or as target/carrier cells in new strategies of regenerative medicine.20
Hydroxyapatite and tricalcium phosphate have been shown to facilitate and promote cartilage regeneration15,29,70 and biomineralization in cartilage and especially in bone tissue engineering approaches has been attempted using collagen composites59 and absorbable polymers by means of gel foaming techniques69 and solid/liquid phase separation.47
However, these methods do not allow production of 3D environment adequate to recapitulate the ECM and this is thought to be at the root of the only partial success of such approaches.13,69,77
Given the reported role of HA in cartilage regeneration, we developed a HA functionalized scaffold by means of electrospinning with the aim to recapitulate the native histoarchitecture and the molecular signaling of osteochondral tissue to facilitate the differentiation of hMSCs toward chondrocyte. In this study we demonstrated the effective engraftment and the induction of chondrogenic differentiation of hMSCs after a period of culture upon a patch of electrospun fibers of poly-l-lactic acid (PLLA) loaded with nanoparticles of HA. Ultrastructural analysis of this scaffold revealed the adequate porosity to promote cell attachment. In the used nanocomposite scaffold, mesh openings matched the required dimensions reported in early studies in which the minimum requirement for pore size was considered to be approximately 50–100 μm, due to cell size, migration requirements, and transport.28 This porosity allows for initial cell attachment and subsequent migration into and through the matrix and for mass transfer of nutrients and metabolites, providing sufficient space for development, and later remodeling, of the organized tissue. In addition, this scaffold showed a hierarchical structure with fibers exhibiting a second degree of organization in pores within the submicron range that enhance both cell attachment and exchange surface area.
Cytotoxicity assay revealed preserved cell viability and correlated with an effective cell engrafting following 48 h culture. Interestingly, cells seeded on the PLLA/HA nanocomposite showed a significantly improved survival. Explanations of this phenomenon could be found in both the biological signaling provided by HA, which may promote cell attachment with further maintenance of a favorable milieu to preserve cell vitality, and the biochemical effect that HA functionalization exerts on the scaffold itself. It has been shown that potential problems of biocompatibility in tissue engineering, by applying degradable and reabsorbable polymer scaffolds, may also be related to biodegradability and bioresorbability.75 It is well known the relevance of exposure of 3D scaffold–cell construct to sufficient quantities of neutral culture medium, especially during the period where the mass loss of the polymer matrix occurs; it has been reported that a high amount of degradation by-products, especially occurring with poly-lactic acid, leads to the death of an entire cell culture.76 In this extent, production of hybrid/nanocomposite materials by incorporation of TCP, HA and basic salts into fast polymer matrix systems, such as PGA and PGA/PLA, could be advantageous. These inorganic fillers allow the tailoring of the resorption kinetics of the polymer matrix.9,64 Additionally, the basic degradation products of HA or TCP would buffer the acidic by-products of the aliphatic polyester and may thereby help to avoid the formation of an unfavorable environment for the cells, due to decreased pH.42,64,75
Our findings suggest an effect of PLLA/HA system on stem cells differentiation. hMSCs were cultured in basal and in chondrogenic media both on functionalized PLLA/HA nanocomposite and on bare PLLA scaffolds. Modifications in both cell morphology and markers expression were more significant in PLLA/HA nanocomposites in comparison with PLLA scaffolds. Three days after seeding, hMSCs were well adhered on the PLLA/HA fibers displaying a spindled morphology. After 14 days of culture cells positive for the chondrogenic transcription factor SOX-9 could be detected in the PLLA/HA nanocomposite in a significantly greater percentage than in the PLLA scaffold. We designed an internal positive control culturing hMSC on bare PLLA scaffold in a chondrogenic medium. Our results suggested a significantly increased expression of chondrogenic markers in the PLLA/HA group when compared with PLLA in basal culture conditions. Addition of chondrogenic medium to the non-functionalized scaffold resulted in findings similar to the PLLA/HA scaffold cultured in basal medium. Interestingly, addition of chondrogenic medium to PLLA/HA did not induce significant changes, but a 5% lower percentage of proliferating cells was reported (Fig. 2b).
The authors acknowledge, among the limitations of the study, the lack of quantitative data on mRNA expression of chondrogenic markers to speculate on the actual degree of differentiation obtained. Thus notwithstanding, the expression of a marker typical of mesenchymal stem cells which is also present in chondrocyte (CD29), associated—or not—in the same construct with the chondrogenic transcription factor SOX-9, could reliably suggest the idea of difference advances in already taken and ongoing differentiation pathway toward chondrogenesis.
SOX-9 is a member of the Sox (Sry-type HMG box) gene family, which is predominantly expressed in mesenchymal condensation and cartilage,72 and has been shown to activate type II collagen and aggrecan, playing an early chondrogenic inductive role especially in 3D culture systems.11 This is in line with the report of SOX-9 mRNA expression in MSCs in the initial stage of chondrogenic differentiation followed by high transcription of chondrocyte specific genes, as reported by Bosnakovski et al., in a quantitative analysis of changes in gene profile during chondrogenesis.10 In our study we evaluated, in a semiquantitative assay, the expression of chondrogenic markers showing the induction exerted by the functionalized biomaterial of a relative increase in SOX-9 with respect to the control group. Even if this finding is not supported by contextual gene expression quantitative analysis, these results are in agreement with other works showing up to 25-fold increase of SOX-9 during different protocols of chondrogenic differentiation with respect to a basal level of expression.10,17,23 The expression of SOX-9, was coupled with the presence of a highly expressed surface marker of mesenchymal stem cells27—that is present on chondrocytes as well—and with the production of aggrecan, reliably suggests the idea of different degrees down in the chondrogenic differentiation pathway.
These findings were associated with reported enhancement in cartilage specific extracellular matrix components deposition, as demonstrated by Toluidine blue and Safranin O staining and Aggrecan immunostain in the PLLA/HA nanocomposite in basal conditions. Of note, the latter appeared to be localized within the scaffold surrounding cell clumps. Cells were immersed in this connective atmosphere mainly constituted by neo-produced cartilage-specific proteoglycans. Since HA is known to have osteoinductive properties,44 the chondrogenic phenotype acquired by the MSCs, induced by the PLLA/HA, may be either stable over time or an intermediate stage toward the endochondral bone formation process. In order to investigate this issue, another set of experiments has been performed to assess potential osteogenic differentiation induced by the scaffold. Accordingly to Saldana and collaborators’ protocols, both HA-functionalized and bare PLLA scaffolds were cultured for 21 days in both basal and chondrogenic medium and assayed for calcium phosphate deposition.60 This experiment was also useful to obtain a deeper insight on the significance of HA as a buffering system and/or as main source of calcium for the cells, further explaining the results obtained in terms of increased cell proliferation in the PLLA/HA nanocomposite. No significant calcium deposition was found in all the conditions tested, suggesting a non-osteogenic activity exerted by the scaffold. Moreover, the presence of a minimal amount of calcium phosphate detectable on the PLLA/HA scaffold cultured in the internal positive control of chondrogenic medium, together with the localization of the deposits in the vicinity of the fibers (Figs. 7c and 7d), suggest that the presence of calcium should be referred to HA residual on the scaffold itself. To confirm this hypothesis, a PLLA/HA scaffold not seeded with cells was stained for von Kossa, showing presence of calcium deposits on the scaffold. This strengthens the idea of absence of neo-formation of calcium phosphate salts promoted by the construct and, interestingly, allows to consider the minimal amount of detected staining on the seeded scaffold as a calcium residual following its active use by the system.
Conclusion
We demonstrated that electrospun PLLA/HA nanocomposites can induce differentiation of hMSCs in chondrocyte-like cells that produce proteoglycan based matrix. This nanocomposite could be an amenable alternative for cartilage tissue engineering in combination with bone marrow hMSCs. This functionalized scaffold would provide both a surrogate of the native ECM and the correct sequence of signals to allow a harmonic ongoing lineage-specific differentiation of multipotent precursor cells.
References
Alhadlaq, A., J. H. Elisseeff, L. Hong, C. G. Williams, A. I. Caplan, B. Sharma, R. A. Kopher, S. Tomkoria, D. P. Lennon, A. Lopez, J. J. Mao. (2004), Adult stem cell driven genesis of human-shaped articular condyle. Ann Biomed Eng. 32(7):911-23 doi:10.1023/B:ABME.0000032454.53116.ee
Alhadlaq, A. and J. J. Mao 2004 Mesenchymal stem cells: isolation and therapeutics. Stem Cells Dev 13(4): 436-48. doi:10.1089/scd.2004.13.436
Alhadlaq, A., J. J. Mao. 2005. Tissue-engineered osteochondral constructs in the shape of an articular condyle. J Bone Joint Surg Am 87(5): 936-44. doi:10.2106/JBJS.D.02104
Alhadlaq, A., M. Tang, J. J. Mao. 2005. Engineered adipose tissue from human mesenchymal stem cells maintains predefined shape and dimension: implications in soft tissue augmentation and reconstruction. Tissue Eng 11(3-4): 556-66. doi:10.1089/ten.2005.11.556
Amado, L. C., A. P. Saliaris, K. H. Schuleri, M. St John, J. S. Xie, S. Cattaneo, D. J. Durand, T. Fitton, J. Q. Kuang, G. Stewart, S. Lehrke, W. W. Baumgartner, B. J. Martin, A. W. Heldman, J. M. Hare. 2005. Cardiac repair with intramyocardial injection of allogeneic mesenchymal stem cells after myocardial infarction. Proc Natl Acad Sci U S A 102(32): 11474-9. doi:10.1073/pnas.0504388102
Auclair-Daigle, C., M. N. Bureau, J. G. Legoux, L. Yahia. 2005. Bioactive hydroxyapatite coatings on polymer composites for orthopedic implants. J Biomed Mater Res A 73(4): 398-408. doi:10.1002/jbm.a.30284
Badami, A. S., M. R. Kreke, M. S. Thompson, J. S. Riffle and A. S. Goldstein. 2006. Effect of fiber diameter on spreading, proliferation, and differentiation of osteoblastic cells on electrospun poly(lactic acid) substrates. Biomaterials 27(4): 596-606. doi:10.1016/j.biomaterials.2005.05.084
Behrens, P., T. Bitter, B. Kurz, M. Russlies. 2006. Matrix-associated autologous chondrocyte transplantation/implantation (MACT/MACI)–5-year follow-up. Knee 13(3): 194-202. doi:10.1016/j.knee.2006.02.012
Bonzani, I. C., J. H. George, M. M. Stevens. 2006. Novel materials for bone and cartilage regeneration. Curr Opin Chem Biol. 10(6): 568-75. doi:10.1016/j.cbpa.2006.09.009
Bosnakovski, D., M. Mizuno, G. Kim, S. Takagi, M. Okumur, T. Fujinag. 2006. Gene expression profile of bovine bone marrow mesenchymal stem cell during spontaneous chondrogenic differentiation in pellet culture system. Jpn J Vet Res 53(3-4): 127-39.
Bosnakovski, D., M. Mizuno, G. Kim, S. Takagi, M. Okumura and T. Fujinaga. 2006. Chondrogenic differentiation of bovine bone marrow mesenchymal stem cells (MSCs) in different hydrogels: influence of collagen type II extracellular matrix on MSC chondrogenesis. Biotechnol Bioeng 93(6): 1152-63. doi:10.1002/bit.20828
Buma, P., J. S. Pieper, T. van Tienen, J. L. van Susante, P. M. van der Kraan, J. H. Veerkamp, W. B. van den Berg, R. P. Veth and T. H. van Kuppevelt. 2003. Cross-linked type I and type II collagenous matrices for the repair of full-thickness articular cartilage defects–a study in rabbits. Biomaterials 24(19): 3255-63. doi:10.1016/S0142-9612(03)00143-1
Butnariu-Ephrat, M., D. Robinson, D. G. Mendes, N. Halperin, and Z. Nevo. Resurfacing of goat articular cartilage by chondrocytes derived from bone marrow. Clin. Orthop. Relat. Res. (330):234–243, 1996. doi:10.1097/00003086-199609000-00031.
Calvert, J. W., K. G. Marra, L. Cook, P. N. Kumta, P. A. DiMilla and L. E. Weiss. 2000. Characterization of osteoblast-like behavior of cultured bone marrow stromal cells on various polymer surfaces. J Biomed Mater Res 52(2): 279-84. doi:10.1002/1097-4636(200011)52:2<279::AID-JBM6>3.0.CO;2-8
Chajra, H., C. F. Rousseau, D. Cortial, M. C. Ronziere, D. Herbage, F. Mallein-Gerin and A. M. Freyria. 2008. Collagen-based biomaterials and cartilage engineering. Application to osteochondral defects. Biomed Mater Eng. 18(1 Suppl): S33-45.
Chiroff, R. T., R. A. White, E. W. White, J. N. Weber, D. Roy. 1977. The restoration of the articular surfaces overlying Replamineform porous biomaterials. J Biomed Mater Res 11(2): 165-78. doi:10.1002/jbm.820110203
Ciavarella, S., F. Dammacco, M. De Matteo, G. Loverro, and F. Silvestris. Umbilical cord mesenchymal stem cells: role of regulatory genes in their differentiation to osteoblasts. Stem Cells Dev. 2009 [Epub ahead of print].
Cohen, S. B., C. M. Meirisch, H. A. Wilson, D. R. Diduch. 2003. The use of absorbable co-polymer pads with alginate and cells for articular cartilage repair in rabbits. Biomaterials 24(15): 2653-60. doi:10.1016/S0142-9612(03)00058-9
Colter, D. C., I. Sekiya and D. J. Prockop. 2001. Identification of a subpopulation of rapidly self-renewing and multipotential adult stem cells in colonies of human marrow stromal cells. Proc Natl Acad Sci U S A 98(14): 7841-5. doi:10.1073/pnas.141221698
Csaki, C., P. R. Schneider and M. Shakibaei. 2008. Mesenchymal stem cells as a potential pool for cartilage tissue engineering. Ann Anat 190(5): 395-412. doi:10.1016/j.aanat.2008.07.007
De Bari, C., F. Dell’Accio and F. P. Luyten. 2004. Failure of in vitro-differentiated mesenchymal stem cells from the synovial membrane to form ectopic stable cartilage in vivo. Arthritis Rheum 50(1): 142-50. doi:10.1002/art.11450
Deng, X. L., G. Sui, M. L. Zhao, G. Q. Chen and X. P. Yang. 2007. Poly(L-lactic acid)/hydroxyapatite hybrid nanofibrous scaffolds prepared by electrospinning. J Biomater Sci Polym Ed. 18(1): 117-30. doi:10.1163/156856207779146123
Finger, A. R., C. Y. Sargent, K. O. Dulaney, S. H. Bernacki and E. G. Loboa. 2007. Differential effects on messenger ribonucleic acid expression by bone marrow-derived human mesenchymal stem cells seeded in agarose constructs due to ramped and steady applications of cyclic hydrostatic pressure. Tissue Eng. 13(6): 1151-8. doi:10.1089/ten.2006.0290
Genovese, J. A., C. Spadaccio, J. Langer, J. Habe, J. Jackson and A. N. Patel. 2008. Electrostimulation induces cardiomyocyte predifferentiation of fibroblasts. Biochem Biophys Res Commun 370(3): 450-5. doi:10.1016/j.bbrc.2008.03.115
J. M. Gomez-Vega, E. Saiz, A. P. Tomsia, G. W. Marshall, and S. J. Marshall (2000). Bioactive glass coatings with hydroxyapatite and Bioglass particles on Ti-based implants 1 Processing. Biomaterials 21(2):105–111. doi:10.1016/S0142-9612(99)00131-3
He, W., T. Yong, Z. W. Ma, R. Inai, W. E. Teo and S. Ramakrishna. 2006. Biodegradable polymer nanofiber mesh to maintain functions of endothelial cells. Tissue Eng 12(9): 2457-66. doi:10.1089/ten.2006.12.2457
Hung, S. C., D. M. Yang, C. F. Chang, R. J. Lin, J. S. Wang, L. Low-Tone Ho and W. K. Yang. 2004. Immortalization without neoplastic transformation of human mesenchymal stem cells by transduction with HPV16 E6/E7 genes. Int J Cancer 110(3): 313-9. doi:10.1002/ijc.20126
Hutmacher, D. W., J. T. Schantz, C. X. Lam, K. C. Tan and T. C. Lim. 2007. State of the art and future directions of scaffold-based bone engineering from a biomaterials perspective. J Tissue Eng Regen Med 1(4): 245-60. doi:10.1002/term.24
Ito, Y., N. Adachi, A. Nakamae, S. Yanada, M. Ochi. 2008. Transplantation of tissue-engineered osteochondral plug using cultured chondrocytes and interconnected porous calcium hydroxyapatite ceramic cylindrical plugs to treat osteochondral defects in a rabbit model. Artif Organs 32(1): 36-44.
Jiang, Y., B. N. Jahagirdar, R. L. Reinhardt, R. E. Schwartz, C. D. Keene, X. R. Ortiz-Gonzalez, M. Reyes, T. Lenvik, T. Lund, M. Blackstad, J. Du, S. Aldrich, A. Lisberg, W. C. Low, D. A. Largaespada and C. M. Verfaillie. 2002. Pluripotency of mesenchymal stem cells derived from adult marrow. Nature. 418(6893): 41-9. doi:10.1038/nature00870
Johnstone, B., T. M. Hering, A. I. Caplan, V. M. Goldberg and J. U. Yoo. 1998. In vitro chondrogenesis of bone marrow-derived mesenchymal progenitor cells. Exp Cell Res 238(1): 265-72. doi:10.1006/excr.1997.3858
Kaito, T., A. Myoui, K. Takaoka, N. Saito, M. Nishikawa, N. Tamai, H. Ohgushi and H. Yoshikawa. 2005. Potentiation of the activity of bone morphogenetic protein-2 in bone regeneration by a PLA-PEG/hydroxyapatite composite. Biomaterials 26(1): 73-9. doi:10.1016/j.biomaterials.2004.02.010
Kidoaki, S., I. K. Kwon and T. Matsuda. 2005. Mesoscopic spatial designs of nano- and microfiber meshes for tissue-engineering matrix and scaffold based on newly devised multilayering and mixing electrospinning techniques. Biomaterials 26(1): 37-46. doi:10.1016/j.biomaterials.2004.01.063
Kikuchi, M., Y. Koyama, K. Takakuda, H. Miyairi, N. Shirahama and J. Tanaka. 2002. In vitro change in mechanical strength of beta-tricalcium phosphate/copolymerized poly-L-lactide composites and their application for guided bone regeneration. J Biomed Mater Res 62(2): 265-72. doi:10.1002/jbm.10248
Kikuchi, M., Y. Koyama, T. Yamada, Y. Imamura, T. Okada, N. Shirahama, K. Akita, K. Takakuda and J. Tanaka. 2004. Development of guided bone regeneration membrane composed of beta-tricalcium phosphate and poly (L-lactide-co-glycolide-co-epsilon-caprolactone) composites. Biomaterials 25(28): 5979-86. doi:10.1016/j.biomaterials.2004.02.001
Kim, B. S., A. J. Putnam, T. J. Kulik and D. J. Mooney. 1998. Optimizing seeding and culture methods to engineer smooth muscle tissue on biodegradable polymer matrices. Biotechnol Bioeng 57(1): 46-54. doi:10.1002/(SICI)1097-0290(19980105)57:1<46::AID-BIT6>3.0.CO;2-V
Kim, T. G. and T. G. Park. 2006. Biomimicking extracellular matrix: cell adhesive RGD peptide modified electrospun poly(D,L-lactic-co-glycolic acid) nanofiber mesh. Tissue Eng 12(2): 221-33. doi:10.1089/ten.2006.12.221
Lee, T. M., C. Y. Yang, E. Chang and R. S. Tsai. 2004. Comparison of plasma-sprayed hydroxyapatite coatings and zirconia-reinforced hydroxyapatite composite coatings: in vivo study. J Biomed Mater Res A 71(4): 652-60. doi:10.1002/jbm.a.30190
Li, Z., L. Yubao, Y. Aiping, P. Xuelin, W. Xuejiang and Z. Xiang. 2005. Preparation and in vitro investigation of chitosan/nano-hydroxyapatite composite used as bone substitute materials. J Mater Sci Mater Med 16(3): 213-9. doi:10.1007/s10856-005-6682-3
Liao, S., M. Ngiam, F. Watari, S. Ramakrishna, C. K. Chan. 2007. Systematic fabrication of nano-carbonated hydroxyapatite/collagen composites for biomimetic bone grafts. Bioinspir Biomim 2(3): 37-41. doi:10.1088/1748-3182/2/3/001
Liao, S., W. Wang, M. Uo, S. Ohkawa, T. Akasaka, K. Tamura, F. Cui and F. Watari 2005 A three-layered nano-carbonated hydroxyapatite/collagen/PLGA composite membrane for guided tissue regeneration. Biomaterials. 26(36): 7564-71. doi:10.1016/j.biomaterials.2005.05.050
Liao, S. S. and F. Z. Cui 2004 In vitro and in vivo degradation of mineralized collagen-based composite scaffold: nanohydroxyapatite/collagen/poly(L-lactide). Tissue Eng. 10(1-2): 73-80. doi:10.1089/107632704322791718
Liao, S. S., F. Z. Cui, W. Zhang and Q. L. Feng 2004 Hierarchically biomimetic bone scaffold materials: nano-HA/collagen/PLA composite. J Biomed Mater Res B Appl Biomater. 69(2): 158-65. doi:10.1002/jbm.b.20035
Lin, L., K. L. Chow, and Y. Leng 2009 Study of hydroxyapatite osteoinductivity with an osteogenic differentiation of mesenchymal stem cells. J Biomed Mater Res A 89(2): 326-35.
Liu, Y., S. Sagi, R. Chandrasekar, L. Zhang, N. E. Hedin and H. Fong 2008 Preparation and characterization of electrospun SiO2 nanofibers. J Nanosci Nanotechnol. 8(3): 1528-36. doi:10.1166/jnn.2008.043
Luong-Van, E., L. Grondahl, K. N. Chua, K. W. Leong, V. Nurcombe and S. M. Cool 2006 Controlled release of heparin from poly(epsilon-caprolactone) electrospun fibers. Biomaterials. 27(9): 2042-50. doi:10.1016/j.biomaterials.2005.10.028
Ma, P. X., R. Zhang, G. Xiao and R. Franceschi 2001 Engineering new bone tissue in vitro on highly porous poly(alpha-hydroxyl acids)/hydroxyapatite composite scaffolds. J Biomed Mater Res. 54(2): 284-93. doi:10.1002/1097-4636(200102)54:2<284::AID-JBM16>3.0.CO;2-W
Ma, Z., W. He, T. Yong and S. Ramakrishna 2005 Grafting of gelatin on electrospun poly(caprolactone) nanofibers to improve endothelial cell spreading and proliferation and to control cell Orientation. Tissue Eng. 11(7-8): 1149-58. doi:10.1089/ten.2005.11.1149
Ma, Z., M. Kotaki, R. Inai and S. Ramakrishna 2005 Potential of nanofiber matrix as tissue-engineering scaffolds. Tissue Eng. 11(1-2): 101-9. doi:10.1089/ten.2005.11.101
Mackay, A. M., S. C. Beck, J. M. Murphy, F. P. Barry, C. O. Chichester and M. F. Pittenger 1998 Chondrogenic differentiation of cultured human mesenchymal stem cells from marrow. Tissue Eng. 4(4): 415-28. doi:10.1089/ten.1998.4.415
Martin, I., V. P. Shastri, R. F. Padera, J. Yang, A. J. Mackay, R. Langer, G. Vunjak-Novakovic and L. E. Freed 2001 Selective differentiation of mammalian bone marrow stromal cells cultured on three-dimensional polymer foams. J Biomed Mater Res. 55(2): 229-35. doi:10.1002/1097-4636(200105)55:2<229::AID-JBM1009>3.0.CO;2-Q
McManus, A. J., R. H. Doremus, R. W. Siegel and R. Bizios 2005 Evaluation of cytocompatibility and bending modulus of nanoceramic/polymer composites. J Biomed Mater Res A. 72(1): 98-106. doi:10.1002/jbm.a.30204
Mo, X. M., C. Y. Xu, M. Kotaki and S. Ramakrishna 2004 Electrospun P(LLA-CL) nanofiber: a biomimetic extracellular matrix for smooth muscle cell and endothelial cell proliferation. Biomaterials. 25(10): 1883-90. doi:10.1016/j.biomaterials.2003.08.042
Montjovent, M. O., L. Mathieu, B. Hinz, L. L. Applegate, P. E. Bourban, P. Y. Zambelli, J. A. Manson and D. P. Pioletti 2005 Biocompatibility of bioresorbable poly(L-lactic acid) composite scaffolds obtained by supercritical gas foaming with human fetal bone cells. Tissue Eng. 11(11-12): 1640-9. doi:10.1089/ten.2005.11.1640
Nair, L. S., S. Bhattacharyya and C. T. Laurencin 2004 Development of novel tissue engineering scaffolds via electrospinning. Expert Opin Biol Ther. 4(5): 659-68. doi:10.1517/14712598.4.5.659
Noh, H. K., S. W. Lee, J. M. Kim, J. E. Oh, K. H. Kim, C. P. Chung, S. C. Choi, W. H. Park and B. M. Min 2006 Electrospinning of chitin nanofibers: degradation behavior and cellular response to normal human keratinocytes and fibroblasts. Biomaterials. 27(21): 3934-44. doi:10.1016/j.biomaterials.2006.03.016
Noth, U., K. Schupp, A. Heymer, S. Kall, F. Jakob, N. Schutze, B. Baumann, T. Barthel, J. Eulert and C. Hendrich 2005 Anterior cruciate ligament constructs fabricated from human mesenchymal stem cells in a collagen type I hydrogel. Cytotherapy. 7(5): 447-55. doi:10.1080/14653240500319093
Oh, T., M. M. Rahman, J. H. Lim, M. S. Park, D. Y. Kim, J. H. Yoon, W. H. Kim, M. Kikuchi, J. Tanaka, Y. Koyama and O. K. Kweon 2006 Guided bone regeneration with beta-tricalcium phosphate and poly L-lactide-co-glycolide-co-epsilon-caprolactone membrane in partial defects of canine humerus. J Vet Sci. 7(1): 73-7.
Rodrigues, C. V., P. Serricella, A. B. Linhares, R. M. Guerdes, R. Borojevic, M. A. Rossi, M. E. Duarte and M. Farina 2003 Characterization of a bovine collagen-hydroxyapatite composite scaffold for bone tissue engineering. Biomaterials. 24(27): 4987-97. doi:10.1016/S0142-9612(03)00410-1
Saldana, L., S. Sanchez-Salcedo, I. Izquierdo-Barba, F. Bensiamar, L. Munuera, M. Vallet-Regi, and N. Vilaboa 2009 Calcium phosphate-based particles influence osteogenic maturation of human mesenchymal stem cells. Acta Biomater. 5(4): 1294-305.
Schindler, M., I. Ahmed, J. Kamal, E. K. A. Nur, T. H. Grafe, H. Young Chung and S. Meiners 2005 A synthetic nanofibrillar matrix promotes in vivo-like organization and morphogenesis for cells in culture. Biomaterials. 26(28): 5624-31. doi:10.1016/j.biomaterials.2005.02.014
Siepe, M., P. Akhyari, A. Lichtenberg, C. Schlensak and F. Beyersdorf 2008 Stem cells used for cardiovascular tissue engineering. Eur J Cardiothorac Surg. 34(2): 242-7. doi:10.1016/j.ejcts.2008.03.067
Simon, C. G., Jr., N. Eidelman, S. B. Kennedy, A. Sehgal, C. A. Khatri and N. R. Washburn 2005 Combinatorial screening of cell proliferation on poly(L-lactic acid)/poly(D,L-lactic acid) blends. Biomaterials. 26(34): 6906-15. doi:10.1016/j.biomaterials.2005.04.050
Sohier, J., L. Moroni, C. V. Blitterswijk, K. D. Groot and J. Bezemer 2008 Critical factors in the design of growth factor releasing scaffolds for cartilage tissue engineering. Expert Opin Drug Deliv. 5(5): 543-566. doi:10.1517/17425247.5.5.543
Stevens, M. M. and J. H. George 2005 Exploring and engineering the cell surface interface. Science. 310(5751): 1135-8. doi:10.1126/science.1106587
Su, S. H., K. T. Nguyen, P. Satasiya, P. E. Greilich, L. Tang and R. C. Eberhart 2005 Curcumin impregnation improves the mechanical properties and reduces the inflammatory response associated with poly(L-lactic acid) fiber. J Biomater Sci Polym Ed. 16(3): 353-70. doi:10.1163/1568562053654077
Sui, G., X. Yang, F. Mei, X. Hu, G. Chen, X. Deng and S. Ryu 2007 Poly-L-lactic acid/hydroxyapatite hybrid membrane for bone tissue regeneration. J Biomed Mater Res A. 82(2): 445-54. doi:10.1002/jbm.a.31166
Suominen, E., A. J. Aho, E. Vedel, I. Kangasniemi, E. Uusipaikka and A. Yli-Urpo 1996 Subchondral bone and cartilage repair with bioactive glasses, hydroxyapatite, and hydroxyapatite-glass composite. J Biomed Mater Res. 32(4): 543-51. doi:10.1002/(SICI)1097-4636(199612)32:4<543::AID-JBM7>3.0.CO;2-R
Tamai, N., A. Myoui, M. Hirao, T. Kaito, T. Ochi, J. Tanaka, K. Takaoka and H. Yoshikawa 2005 A new biotechnology for articular cartilage repair: subchondral implantation of a composite of interconnected porous hydroxyapatite, synthetic polymer (PLA-PEG), and bone morphogenetic protein-2 (rhBMP-2). Osteoarthritis Cartilage. 13(5): 405-17. doi:10.1016/j.joca.2004.12.014
Tanaka, T., H. Komaki, M. Chazono and K. Fujii 2005 Use of a biphasic graft constructed with chondrocytes overlying a beta-tricalcium phosphate block in the treatment of rabbit osteochondral defects. Tissue Eng. 11(1-2): 331-9. doi:10.1089/ten.2005.11.331
Tancred, D. C., A. J. Carr and B. A. McCormack 2001 The sintering and mechanical behavior of hydroxyapatite with bioglass additions. J Mater Sci Mater Med. 12(1): 81-93. doi:10.1023/A:1026773522934
Tsuchiya, H., H. Kitoh, F. Sugiura and N. Ishiguro 2003 Chondrogenesis enhanced by overexpression of sox9 gene in mouse bone marrow-derived mesenchymal stem cells. Biochem Biophys Res Commun. 301(2): 338-43. doi:10.1016/S0006-291X(02)03026-7
Tsuji, H., M. Ogiwara, S. K. Saha and T. Sakaki 2006 Enzymatic, alkaline, and autocatalytic degradation of poly(L-lactic acid): effects of biaxial orientation. Biomacromolecules. 7(1): 380-7. doi:10.1021/bm0507453
Ushida, T., K. Furukawa, K. Toita and T. Tateishi 2002 Three-dimensional seeding of chondrocytes encapsulated in collagen gel into PLLA scaffolds. Cell Transplant. 11(5): 489-94.
Vert, M., S. Li and H. Garreau 1992 New insights on the degradation of bioresorbable polymeric devices based on lactic and glycolic acids. Clin Mater. 10(1-2): 3-8. doi:10.1016/0267-6605(92)90077-7
Vert, M., G. Schwach, R. Engel and J. Coudane 1998 Something new in the field of PLA/GA bioresorbable polymers? J Control Release. 53(1-3): 85-92. doi:10.1016/S0168-3659(97)00240-X
Wakitani, S., T. Goto, S. J. Pineda, R. G. Young, J. M. Mansour, A. I. Caplan and V. M. Goldberg 1994 Mesenchymal cell-based repair of large, full-thickness defects of articular cartilage. J Bone Joint Surg Am. 76(4): 579-92.
Wan, Y., Y. Wang, Z. Liu, X. Qu, B. Han, J. Bei and S. Wang 2005 Adhesion and proliferation of OCT-1 osteoblast-like cells on micro- and nano-scale topography structured poly(L-lactide). Biomaterials. 26(21): 4453-9. doi:10.1016/j.biomaterials.2004.11.016
Wei, G. and P. X. Ma 2004 Structure and properties of nano-hydroxyapatite/polymer composite scaffolds for bone tissue engineering. Biomaterials. 25(19): 4749-57. doi:10.1016/j.biomaterials.2003.12.005
Xu, C., R. Inai, M. Kotaki and S. Ramakrishna 2004 Electrospun nanofiber fabrication as synthetic extracellular matrix and its potential for vascular tissue engineering. Tissue Eng. 10(7-8): 1160-8.
Yim, E. K., R. M. Reano, S. W. Pang, A. F. Yee, C. S. Chen and K. W. Leong 2005 Nanopattern-induced changes in morphology and motility of smooth muscle cells. Biomaterials. 26(26): 5405-13. doi:10.1016/j.biomaterials.2005.01.058
Zhang, S. M., F. Z. Cui, S. S. Liao, Y. Zhu and L. Han 2003 Synthesis and biocompatibility of porous nano-hydroxyapatite/collagen/alginate composite. J Mater Sci Mater Med. 14(7): 641-5. doi:10.1023/A:1024083309982
Acknowledgments
This work was in part supported by the University of Pittsburgh Medical Center Heart, Lung & Esophageal Surgery Institute.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Spadaccio, C., Rainer, A., Trombetta, M. et al. Poly-l-Lactic Acid/Hydroxyapatite Electrospun Nanocomposites Induce Chondrogenic Differentiation of Human MSC. Ann Biomed Eng 37, 1376–1389 (2009). https://doi.org/10.1007/s10439-009-9704-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-009-9704-3