Abstract
Background
The optimal extent of thyroidectomy for papillary thyroid cancer (PTC) is controversial. Our objective was to evaluate the effect of total thyroidectomy or partial thyroidectomy on survival in low- and high-risk patients.
Methods
The Surveillance, Epidemiology, and End Results database was used to identify PTC patients who underwent thyroidectomy. The independent effects of age, distant metastases, extrathyroidal extension, tumor size, sex, lymph node metastases, radioactive iodine use, and extent of thyroidectomy on survival were analyzed for low- and high-risk PTC.
Results
There were 4402 (81%) low-risk and 1030 (19%) high-risk patients; 84.9% underwent total thyroidectomy. The 5- and 10-year survival were 95% and 89% in the low-risk patients and 84% and 73% in the high-risk patients, respectively (P = .001). In the low-risk patients, 10-year survival after total thyroidectomy was 89%, compared with 91% after partial thyroidectomy (adjusted hazard ratio for death, 1.73; 95% confidence interval, 1.28–2.33; P < .001); older age, male sex, larger tumor, lymph node metastases, and lack of radioactive iodine were associated with higher mortality. In the high-risk patients, 10-year survival after total thyroidectomy was 72%, compared with 78% after partial thyroidectomy (adjusted hazard ratio for death, 1.46; 95% confidence interval, .89–2.40; P = .14); older age, distant metastases, larger tumors, and lack of radioactive iodine were associated with higher mortality.
Conclusions
Survival of patients with PTC was not significantly influenced by the extent of thyroidectomy. The survival after partial thyroidectomy was similar to total thyroidectomy within both the low- and high-risk prognostic groups.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Prognostic indices have been generated that stratify patients with papillary thyroid cancer (PTC) into low- and high-risk prognostic groups. 1– 7 Most patients with PTC are low risk and have an excellent prognosis; the small proportion of patients who are high risk have a relatively worse survival. The extent of thyroidectomy that provides optimal survival for low-risk and high-risk patients is unknown, because no randomized trial has compared outcomes after total thyroidectomy with those after an operation of lesser extent. One approach that has been suggested is to use a less extensive thyroidectomy, such as thyroid lobectomy and isthmusectomy, on patients with a good prognosis, rather than routinely performing total thyroidectomy on all patients. 2,3,8–12
However, total thyroidectomy has been proposed as the optimal operation for all patients with PTC. It provides advantages such as clearing microscopic contralateral disease, enabling the use of radioactive iodine as an adjuvant therapy, allowing accurate postoperative thyroglobulin surveillance, and, possibly, providing better survival. Proponents of total thyroidectomy recommend performing it on all patients except those with microscopic cancers, regardless of their prognostic grouping.13,14
This population-based study was performed to determine the effect of the extent of thyroidectomy on the survival of patients with low- and high-risk PTC. Our hypotheses were that patients with low-risk PTC have similar survival regardless of the extent of thyroidectomy and that those with high-risk PTC have improved survival if total thyroidectomy is performed.
METHODS
Data Sources and Study Subjects
The Surveillance, Epidemiology, and End Results (SEER) database15 was used to identify people in the United States diagnosed with thyroid cancer (International Classification of Diseases for Oncology code C73.9) in 12 SEER regions between 1988 and 1995. Only those with histological subtypes of PTC (consisting of papillary adenocarcinoma [International Classification of Diseases for Oncology histology code 8260], follicular variant of papillary carcinoma [code 8340], mixed papillary/follicular carcinoma [code 8340], and papillary carcinoma [code 8050]) were included. Patients younger than 20 years and patients in whom data were missing were excluded.
Surgical Procedures
Surgical therapy was determined according to the site-specific thyroid surgery codes, indicating the most extensive surgical procedure performed. Surgical therapy was dichotomized into (1) total thyroidectomy (total, near-total, or subtotal thyroidectomy) and (2) partial thyroidectomy (lobectomy with or without isthmusectomy). Patients who had a biopsy alone without additional surgery and those with an unspecified thyroidectomy were excluded.
Risk Stratification
Patients were classified into low- and high-risk groups by using the age, metastases, extent, and size (AMES) risk classification. The low-risk group includes all younger (≤40 years for men and ≤50 years for women) patients with intrathyroidal cancers and all older patients with intrathyroidal cancers <5 cm, without distant metastases.2 The high-risk group includes all younger patients who have cancers with extrathyroidal extension and all older patients who have cancers at least 5 cm in size, any cancer with extrathyroidal extension, or intrathyroidal follicular cancers with major tumor capsular involvement or any patient with distant metastases.2
By using these criteria, the variables age, presence or absence of distant metastases, extrathyroidal extension, and tumor size were used to assign patients into low- or high-risk groups. Age in SEER is categorized in 5-year intervals and was grouped into three categories to allow assignment of an AMES risk grouping for each sex. A SEER extent-of-disease code specifies the local and distant extent of tumor in a hierarchical and mutually exclusive manner.16 Extrathyroidal extension was dichotomized into none (tumor confined to thyroid gland) or contiguous spread into adjacent structures. Distant metastasis was recorded as present or absent. Only one extent-of-disease code is used per patient in the SEER database, and therefore local extension in a patient with synchronous distant disease cannot be determined. Because the presence of distant metastases is a high-risk AMES criterion regardless of local extent, this did not affect our ability to classify subjects into low- and high-risk categories. Tumor size was dichotomized as in AMES with a 5-cm cutoff.
We also assessed the effect of sex, the presence or absence of metastatic thyroid cancer in the regional lymph nodes, and the use of radioactive iodine on survival. Regional nodes include ipsilateral, bilateral, contralateral, midline, or cervical nodes; tracheoesophageal, upper anterior mediastinal, submandi-bular, or submental nodes; or regional nodes not otherwise specified.
Statistical Analysis
Survival time was calculated as the time (in months) from diagnosis until death from any cause, last follow-up, or December 31, 2000, whichever came first. Survival was estimated with the Kaplan-Meier method,17 and survival curves were compared by using the log-rank test. Associations between predictor variables and survival were assessed with Cox proportional hazards modeling.18 We performed stratified analyses according to risk group. Multivariate proportional hazards models estimating survival in the high-risk group included, as independent variables, age (in categories ≤39, 40–49, or ≥50 years), sex, extrathyroidal extension (none or adjacent spread), distant metastases (none or present), tumor size (<5 cm or ≥5 cm), regional lymph node metastases (none or present), radioactive iodine use, and type of thyroidectomy (partial vs. total thyroidectomy); the same variables were analyzed in the low-risk group, except for extrathyroidal extension and distant metastases, because low-risk patients by definition have disease confined to the thyroid gland. The strength of associations between predictor variables and estimated survival was expressed as hazard ratios (HRs) and 95% confidence intervals (CI) for death. An HR of 1 indicates that a variable does not affect the risk of death. For each variable, an HR of <1 indicates that it is associated with a reduction in the risk of death, and an HR of >1 indicates that the variable is associated with a greater risk of death. HRs were considered statistically significant if the 95% CI did not overlap 1.0 or if P values were <.05. The proportional hazards assumption was tested by inspection of log-log survival plots. All P values reported were two tailed. SEER*Stat (National Cancer Institute, Cancer Statistics Branch, Bethesda, MD) was used to extract the data from the SEER database; the data were then exported to SAS Version 8 (SAS Institute, Inc., Cary, NC) statistical software for statistical analyses.
RESULTS
Patient Demographics
There were 5432 patients with PTC available for analysis. Most (59.1%) patients were ≥40 years old, and most (77%) were women (Table 1). A total of 92.5% of tumors were smaller than 5 cm, 85.4% were confined to the thyroid gland, 25.7% had regional lymph node metastases, and 1.2% had distant spread within 4 months of diagnosis. Most patients (81%) had low-risk PTC. Radioactive iodine was used in 43% of patients.
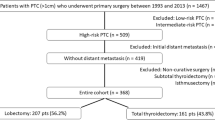
Extent of Thyroidectomy
There were 4612 (84.9%) patients who underwent total or near-total thyroidectomy, and 820 (15.1%) underwent partial thyroidectomy (Table 2). As compared with patients who had partial thyroidectomy, those undergoing total thyroidectomy were more likely to be young, to be male, and to have extrathyroidal extension or regional lymph node metastases. In the low-risk group, 3663 (83.2%) of 4402 had a total thyroidectomy, as compared with 949 (92.1%) of 1030 in the high-risk group (P < .001; Table 3).
Survival
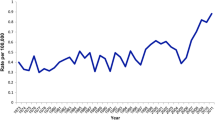
The median follow-up was 7.4 years, with a range of 1 month to 12 years. At the end of follow-up, 608 (11.2%) patients had died. Overall survival in the entire group was 93% (95% CI, 92.2%–93.8%) at 5 years and 86% (95% CI, 85%–87%) at 10 years (Fig. 1). The 5- and 10-year survival was 95% (95% CI, 94.4%–96.1%) and 89% (95% CI, 87.8%–90.2%) in the low-risk patients and 84% (95% CI, 82%–86%) and 73% (95% CI, 69%–77%) in the high-risk patients, respectively (Fig. 2; P < .001). Figure 3 shows the survival in the low- and high-risk patients after either a total thyroidectomy or a partial thyroidectomy. In low-risk patients, 10-year survival was 89% (95% CI, 87.6%–90.4%) after total thyroidectomy and 91% (95% CI, 89%–93%) after partial thyroidectomy (P = .07). In high-risk patients, 10-year survival was 72% (95% CI, 68%–76%) after total thyroidectomy and 78% (95% CI, 68%–88%) after partial thyroidectomy (P = .66).
Survival by extent of thyroidectomy in each risk group. In low-risk patients, the 10-year survival was 89% (95% confidence interval [CI], 87.6%–90.4%) after total thyroidectomy and 91% (95% CI, 89%–93%) after partial thyroidectomy (P = .07). In high-risk patients, the 10-year survival was 72% (95% CI, 68%–76%) after total thyroidectomy and 78% (95% CI, 68%–88%) after partial thyroidectomy (P = .66).
Low-Risk PTC
On univariate analysis of the low-risk patients, those who were aged ≥50 years had a higher risk of death as compared with patients ≤39 years (HR, 16.7; 95% CI, 11.2–25.0; Table 4). Women had a lower risk of death (HR, .53; 95% CI, .43–.66). Other variables evaluated that had no effect on estimated survival were size, lymph node metastasis, and extent of thyroidectomy. With multivariate models to assess for any independent effect on mortality, older age (≥50 vs. ≤39 years: HR, 17.2; 95% CI, 11.3–26.5), larger tumor size (HR, 4.47; 95% CI, 2.00–9.98), regional lymph node metastases (HR, 1.46; 95% CI, 1.10–1.95), and total thyroidectomy (HR, 1.73; 95% CI, 1.28–2.33) were associated with higher mortality, whereas female sex (HR, .67; 95% CI, .54–.84) and radioactive iodine use (HR, .31; 95% CI, .23–.41) were associated with lower mortality (Table 5).
High-Risk PTC
On univariate analysis of the high-risk patients, older age, distant metastasis, and tumors >5 cm were associated with a higher risk of death. Extrathyroidal extension, lymph node metastasis, radioactive iodine use, and female sex were associated with a lower risk of death. Extent of thyroidectomy had no effect on estimated survival (Table 4). In multivariate models, an independent increase in the risk of death was observed for older age (40–49 vs. ≤39 years: HR, 3.03; 95% CI, 1.12–8.21; ≥50 vs. ≤39 years: HR, 15.5; 95% CI, 6.77–35.4), distant metastasis (HR, 8.64; 95% CI, 5.57–13.4), and larger size (HR, 3.17; 95% CI, 2.24–4.48; Table 6). Radioactive iodine use was associated with an independent reduction in the risk of death (HR, .67; 95% CI, .50–.90). After adjustment for all factors, sex, extrathyroidal extension, and lymph node metastasis were no longer associated with mortality (Table 6). Extent of thyroidectomy remained unassociated with estimated survival.
DISCUSSION
This population-based study provides survival data on a large cohort of patients with PTC in different regions across the United States. There was little difference in survival within each risk group whether patients were treated with a partial or a total thyroidectomy. We were surprised to find that the survival of patients with high-risk disease was not improved by the use of total thyroidectomy.
In our study, patients with low-risk PTC had better survival after partial than after total thyroidectomy, which was an unexpected finding. The survival equivalence between total and partial thyroidectomy in high-risk patients may relate to the indolence of most PTC, even in patients with high-risk disease, who have a relatively good survival when compared with patients with other solid tumors. In most other solid tumors, if the recurrence risk is high, more aggressive treatment may be warranted because the absolute reduction in the risk of recurrence is larger, thus offsetting disadvantages related to more aggressive treatment and improving the benefit-risk ratio. In the case of PTC, the generally favorable disease biology seems to make the extent of operation performed less important. In general, as tumor behavior becomes extremely aggressive, local surgical treatment is probably less important because of the high risk of death, as, for example, in the case of anaplastic thyroid cancer. Somewhere in the intermediate spectrum of tumor behavior, more aggressive surgical treatment may be found to have an effect.
There is no reasonable biological explanation of why partial thyroidectomy should be associated with a reduced risk of death in low-risk patients. Therefore, it is possible that bias is contributing to some of our findings in this observational study. Because there seems to be a strong selection bias in favor of the use of total thyroidectomy, it is likely that unmeasured factors may be confounding the associations with survival we are measuring. Our databases lacked clinical detail that might help to explain some of the differences in survival observed between groups of patients treated with different extents of thyroidectomy. Factors unavailable in SEER, such as thyroid-stimulating hormone suppression, or more aggressive histological variants, such as tall cell PTC, may influence the results. If there was a survival benefit associated with the use of more extensive thyroidectomy, however, it must be relatively small, to the extent that it is completely obscured (or reversed) by confounding. The excellent long-term survival observed among all patients with PTC, regardless of risk classification and extent of thyroidectomy, makes it difficult to make a strong recommendation about the use of more aggressive surgery. The fact that partial thyroidectomy was not associated with worse survival regardless of risk classification, however, supports it as an option for patients with PTC.
Our results that extent of thyroidectomy has no effect on survival for low-risk patients can be compared with the results reported by Mazzaferri and Jhiang.5 Their study has the longest follow-up data for patients with PTC—a median follow-up of 15.7 years, compared with 7.4 years in our study. Mazzaferri and Jhiang reported a 30-year mortality of 6% in 698 patients with clinical stage 2 or 3 PTC treated with near-total or total thyroidectomy, compared with 9% in 436 patients treated with less than a near-total thyroidectomy. Most of these were clinical stage 2, similar to our low-risk category, but approximately 20% were clinical stage 3, who would be classified in our study in the high-risk group. Although statistically significant, the absolute difference of 3% between groups is relatively small. That extent of thyroidectomy had little survival influence in low- or high-risk patients in our study may be attributed to the indolent tumor biology of PTC; longer follow-up may produce a small survival difference. As compared with the study by Mazzaferri and Jhiang, our study was four times larger and was representative of a broad population in many regions of the United States. The cohort in the study by Mazzaferri and Jhiang is a highly selected group of patients treated at two institutions, and the study results are subject to the same biases that may be influencing our study.
One approach that has been suggested for surgical management of PTC is to use partial thyroidectomy for low-risk patients and to reserve total thyroidectomy for high-risk patients, because some studies have shown no survival benefit from more extensive thyroidectomy in low-risk patients.10,12,19,20 Another approach is to perform total thyroidectomy in all patients because of advantages such as removing contralateral microscopic disease, enabling accurate serial postoperative thyroglobulin measurements, allowing radioactive iodine to be administered to ablate any residual thyroid tissue and treat any residual cancer, and possibly decreasing the recurrence rate5,21– 24 and increasing survival. 5,13,14,21–23 Our study does not support either of these approaches, but it supports performing either operation for either risk group; partial thyroidectomy may be a reasonable alternative to total thyroidectomy. The theoretical advantages of total thyroidectomy are not as important if the survival is unaffected. The debate about the optimal extent of thyroidectomy is likely to continue, because no randomized controlled trial has ever been performed on this issue; it is unlikely that such a trial will be completed because of the large sample size required to show a small survival difference.25
Total or near-total thyroidectomy was performed more often than less extensive procedures for our study patients with PTC, whether they were low or high risk according to AMES criteria. Although many patients who were low risk had excellent survival with a partial thyroidectomy, a near-total or total thyroidectomy was performed in most of these patients. Most of all patients in this study (83%) underwent near-total or total thyroidectomy, and most were in the low-risk group. In other large database studies using the National Cancer Data Base and a linked analysis of the National Cancer Data Base and the American College of Surgeons Commission on Cancer Patient Care Evaluation Thyroid Cancer Study, most patients with PTC were treated with total thyroidectomy.19,26 Another study using SEER data revealed that the risk classification of patients with well-differentiated thyroid cancer does not independently determine the choice of thyroidectomy by surgeons in the United States.27 It seems that most patients in the United States undergo near-total or total thyroidectomy regardless of their risk. Our study supports partial thyroidectomy as a reasonable option because it seems to provide similar survival in any risk group.
Age is one of the most important prognostic factors in PTC: older age is associated with a poorer prognosis. Many would argue that more extensive thyroidectomy is warranted in older patients. 5,28– 30 Age was also a powerful influence on survival in our study. After accounting for other variables, including the extent of thyroidectomy, age remained a strong predictor in both low- and high-risk patients. Our study, however, does not support use of a total thyroidectomy over a partial thyroidectomy in older patients.
Radioactive iodine treatment was associated with a decreased mortality in both low- and high-risk patients after adjustment for all other measured variables, including extent of thyroidectomy. Mazzaferri and Jhiang5 found that the 30-year mortality was 9% in patients who did not receive radioactive iodine, compared with 3% in those treated with radioactive iodine, after excluding clinical stage 1 and 4 disease. Taylor et al.28 reported in patients with high-risk PTC, after adjusting for other variables, a benefit from radioactive iodine, which reduced the risk of cancer-specific mortality (risk ratio, .30), but not overall survival, with a short average follow-up of 3 years. Radioactive iodine as an adjuvant therapy seems to be an important adjuvant modality in treating patients with PTC. In fact, in our study, it was more important than the extent of thyroidectomy.
In summary, the survival of patients with PTC is not significantly influenced by the extent of thyroidectomy, whether the patient is in a low- or high-risk group. Patients who have a partial thyroidectomy seem to have long-term survival similar to those who have a total thyroidectomy, even after accounting for their prognostic risk group.
References
DP Byar SB Green P Dor et al. (1979) ArticleTitleA prognostic index for thyroid carcinoma: a study of the EORTC Thyroid Cancer Cooperative Group Eur J Cancer 15 1033–41 Occurrence Handle510341 Occurrence Handle1:STN:280:DyaL3c%2FmvV2qtg%3D%3D
B Cady R Rossi (1988) ArticleTitleAn expanded view of risk-group definition in differentiated thyroid carcinoma Surgery 104 947–53 Occurrence Handle1:STN:280:DyaL1M%2FlvVyhsg%3D%3D Occurrence Handle3194846
ID Hay CS Grant WF Taylor WM McConahey (1987) ArticleTitleIpsilateral lobectomy versus bilateral lobar resection in papillary thyroid carcinoma: a retrospective analysis of surgical outcome using a novel prognostic scoring system Surgery 102 1171–8
ID Hay E Bergstrahl J Goellner J Ebersold CS Grant (1993) ArticleTitlePredicting outcome in papillary thyroid carcinoma: development of a reliable prognostic scoring system in a cohort of 1779 patients surgically treated at one institution during 1940 through 1989 Surgery 114 1050–7 Occurrence Handle1:STN:280:DyaK2c%2FnvVantA%3D%3D Occurrence Handle8256208
EL Mazzaferri SM Jhiang (1994) ArticleTitleLong-term impact of initial surgical and medical therapy on papillary and follicular thyroid cancer Am J Med 97 418–28 Occurrence Handle1:STN:280:DyaK2M%2FmvVSgtA%3D%3D Occurrence Handle7977430
InstitutionalAuthorNameAmerican Joint Committee on Cancer. (1997) Thyroid gland ID Fleming JS Cooper DE Henson (Eds) et al. AJCC Cancer Staging Manual EditionNumber5 Lippincott-Raven Philadelphia
SI Sherman JD Brierley M Sperling et al. (1998) ArticleTitleProspective multicenter study of thyroid carcinoma treatment: initial analysis of staging and outcome Cancer 83 1012–21 Occurrence Handle10.1002/(SICI)1097-0142(19980901)83:5<1012::AID-CNCR28>3.0.CO;2-9 Occurrence Handle1:STN:280:DyaK1cvgtVKgsA%3D%3D Occurrence Handle9731906
KH Cohn M Backdahl G Forsslund et al. (1984) ArticleTitleBiologic considerations and operative strategy in papillary thyroid carcinoma: arguments against the routine performance of total thyroidectomy Surgery 96 957–71 Occurrence Handle6505969 Occurrence Handle1:STN:280:DyaL2M%2Fms1eksQ%3D%3D
JL Pasieka LE Rotstein (1993) ArticleTitleConsensus conference on well-differentiated thyroid cancer: a summary Can J Surg 36 298–301 Occurrence Handle8370008 Occurrence Handle1:STN:280:DyaK3sznvF2gsA%3D%3D
AR Shaha JP Shah TR Loree (1997) ArticleTitleLow-risk differentiated thyroid cancer: the need for selective treatment Ann Surg Oncol 4 328–33 Occurrence Handle9181233 Occurrence Handle1:STN:280:DyaK2szisFWltg%3D%3D
B Cady (1997) ArticleTitleHayes Martin Lecture. Our AMES is true: how an old concept still hits the mark—or, risk group assignment points the arrow to rational therapy selection in differentiated thyroid cancer Am J Surg 174 462–8 Occurrence Handle9374215 Occurrence Handle1:STN:280:DyaK1c%2FktVeksw%3D%3D
H Wanebo M Coburn D Teates B Cole (1998) ArticleTitleTotal thyroidectomy does not enhance disease control or survival even in high-risk patients with differentiated thyroid cancer Ann Surg 227 912–21 Occurrence Handle1:STN:280:DyaK1c3pvFKlug%3D%3D Occurrence Handle9637555
OH Clark (1982) ArticleTitleTotal thyroidectomy: the treatment of choice for patients with well-differentiated thyroid cancer Ann Surg 196 361–70 Occurrence Handle7114941 Occurrence Handle1:STN:280:DyaL383ot12ntQ%3D%3D
E Kebebew OH Clark (2000) ArticleTitleDifferentiated thyroid cancer: “complete” rational approach World J Surg 24 942–51 Occurrence Handle10865038 Occurrence Handle1:STN:280:DC%2BD3cvitlGltA%3D%3D
Surveillance, Epidemiology, and End Results Program (http://www.seer.cancer.gov) SEER*Stat Database: Incidence— SEER 12 Regs Public-Use, Nov 2002 Sub (1973-2000), National Cancer Institute, DCCPS, Surveillance Research Program, Cancer Statistics Branch, released April 2003, based on the November 2002 submission
Fritz A, Ries L, eds. SEER Extent of Disease 1998, Codes and Coding Instructions (No. T-899; Pub. No. 98-4354). 3rd ed. Bethesda, MD: Cancer Statistics Branch, Surveillance Program, Division of Cancer Control and Population Sciences, National Cancer Institute, US Department of Health and Human Services, Public Health Service, National Institutes of Health, 1998:1, 7
EL Kaplan P Meier (1958) ArticleTitleNonparametric estimation from incomplete observations J Am Stat Assoc 53 457–81
DR Cox (1972) ArticleTitleRegression models and life-tables J R Stat Soc B 34 187–220
SA Hundahl ID Fleming AM Fremgen HR Menck (1998) ArticleTitleA National Cancer Data Base report on 53,856 cases of thyroid carcinoma treated in the U.S. 1985-1995 Cancer 83 2638– 48 Occurrence Handle10.1002/(SICI)1097-0142(19981215)83:12<2638::AID-CNCR31>3.0.CO;2-1 Occurrence Handle1:STN:280:DyaK1M%2FovFylug%3D%3D Occurrence Handle9874472
LE Sanders B Cady (1998) ArticleTitleDifferentiated thyroid cancer: reexamination of risk groups and outcome of treatment Arch Surg 133 419–25 Occurrence Handle1:STN:280:DyaK1c3isVOqtw%3D%3D Occurrence Handle9565123
ID Hay CS Grant EJ Bergstralh GB Thompson JA Van Heerden JR Goellner (1998) ArticleTitleUnilateral total lobectomy: is it sufficient surgical treatment for patients with AMES low-risk papillary thyroid carcinoma? Surgery 124 958–66 Occurrence Handle10.1067/msy.1998.91825 Occurrence Handle1:STN:280:DyaK1M%2FntFOgsQ%3D%3D Occurrence Handle9854569
LJ DeGroot EL Kaplan M McCormick FH Straus (1990) ArticleTitleNatural history, treatment, and course of papillary thyroid carcinoma J Clin Endocrinol Metab 71 414–24 Occurrence Handle10.1210/jcem-71-2-414 Occurrence Handle2380337 Occurrence Handle1:STN:280:DyaK3czjvVeisQ%3D%3D
NA Samaan PN Schultz RC Hickey et al. (1992) ArticleTitleThe results of various modalities of treatment of well differentiated thyroid carcinomas: a retrospective review of 1599 patients J Clin Endocrinol Metab 75 714–20 Occurrence Handle1517360 Occurrence Handle1:STN:280:DyaK38zovVenug%3D%3D
EL Mazzaferri RL Young (1981) ArticleTitlePapillary thyroid carcinoma: a 10 year follow-up report of the impact of therapy in 576 patients Am J Med 70 511–8 Occurrence Handle7211893 Occurrence Handle1:STN:280:DyaL3M7lslaqug%3D%3D
R Udelsman E Lakatos P Ladenson (1996) ArticleTitleOptimal surgery for papillary thyroid carcinoma World J Surg 20 88–93 Occurrence Handle1:STN:280:DyaK287kvVemuw%3D%3D Occurrence Handle8588420
SA Hundahl B Cady MP Cunningham et al. (2000) ArticleTitleInitial results from a prospective cohort study of 5583 cases of thyroid carcinoma treated in the United States during 1996: an American College of Surgeons Commission on Cancer patient care evaluation study Cancer 89 202–17 Occurrence Handle10.1002/1097-0142(20000701)89:1<202::AID-CNCR27>3.0.CO;2-A Occurrence Handle1:STN:280:DC%2BD3czlslSlsg%3D%3D Occurrence Handle10897019
PI Haigh DR Urbach LE Rotstein (2004) ArticleTitleAMES prognostic index and extent of thyroidectomy for well-differentiated thyroid cancer in the United States Surgery 136 609–16 Occurrence Handle15349109
T Taylor B Specker J Robbins et al. (1998) ArticleTitleOutcome after treatment of high-risk papillary and non-Hurthle cell follicular thyroid carcinoma Ann Intern Med 129 622–7 Occurrence Handle9786809 Occurrence Handle1:STN:280:DyaK1cvkt12gsw%3D%3D
InstitutionalAuthorNameBritish Thyroid Association and Royal College of Physicians. (2002) Guidelines for the Management of Thyroid Cancer in Adults Royal College of Physicians London
L Vini SL Hyer J Marshall R A’Hern C Harmer (2003) ArticleTitleLong-term results in elderly patients with differentiated thyroid carcinoma Cancer 97 2736–42 Occurrence Handle12767085
ACKNOWLEDGMENT
Dr. Urbach is a Career Scientist of the Ontario Ministry of Health and Long-Term Care, Health Research Personnel Development Program, Ontario, Canada.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Haigh, P.I., Urbach, D.R. & Rotstein, L.E. Extent of Thyroidectomy Is Not a Major Determinant of Survival in Low- or High-Risk Papillary Thyroid Cancer. Ann Surg Oncol 12, 81–89 (2005). https://doi.org/10.1007/s10434-004-1165-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10434-004-1165-1