Abstract
The prevalence of nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH) has increased rapidly worldwide, making NAFLD/NASH an important global health problem from both a medical and socioeconomic standpoint. NAFLD is also regarded as a liver component of metabolic syndrome and is reported to be associated with the risk factors for metabolic syndrome. It has been suggested that NAFLD/NASH be recognized both as a liver-specific disease and as an early mediator of systemic diseases. Liver biopsy is recommended as the gold standard method for the diagnosis of NASH and for the staging of liver fibrosis in patients with NAFLD. However, because of its high cost, high risk, and high weightage as a healthcare resource, invasive liver biopsy is a poorly suited diagnostic test for such a highly prevalent condition. Therefore, the development of reliable noninvasive methods for the assessment of liver fibrosis has been sought to estimate the risk of progression of NASH to cirrhosis, estimate the risk of cardiovascular events, aid in the surveillance for HCC, and guide therapy in patients with NAFLD/NASH. In this review, we highlight the principles and recent advances in ultrasound elastography techniques (Real-time Tissue Elastography®, vibration-controlled transient elastography, point shear wave elastography, and two-dimensional shear wave elastography) used to evaluate the liver fibrosis stage and steatosis grade in patients with NAFLD.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The prevalence of nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH) has increased rapidly worldwide, along with increases in the prevalence of obesity and type 2 diabetes mellitus (T2DM) [1, 2]. NASH, the progressive form of NAFLD, histologically characterized by lobular inflammation and hepatocyte ballooning, is associated with a more rapid progression to fibrosis, and affects around 1.5–6% of the general population [1, 3]. NAFLD/NASH is now recognized as the most common liver disease worldwide, and the global prevalence of NAFLD is estimated at 25% of the world population, with geographical variability and the highest prevalence in the Middle East and South America [1]. NAFLD/NASH often shows the progression to cirrhosis, and patients with this disease show a higher frequency of development of hepatocellular carcinoma (HCC) [1, 4]. Thus, NAFLD/NASH represents an important global health problem from both a medical and socioeconomic standpoint.
Nonalcoholic fatty liver disease is also regarded as a liver component of metabolic syndrome and is often associated with the risk factors of metabolic syndrome, such as obesity, T2DM, and dyslipidemia [5, 6]. Recently, a growing body of evidence has been collected to support the notion that NAFLD is both a liver-specific disease and an early mediator of systemic diseases. Notably, histological liver fibrosis is recognized as the main predictor of the overall long-term outcomes in patients with NAFLD, including the development of cardiovascular disease and liver-related mortality [7].
Liver biopsy is recommended as the gold standard method for the diagnosis of NASH and the staging of liver fibrosis in patients with NAFLD [8,9,10]. However, because of its increased cost, high risk, and high weightage as a healthcare resource, an invasive liver biopsy is a poorly suited diagnostic test for a condition with such a high prevalence as NAFLD/NASH [11]. Therefore, the development of reliable non-invasive methods for the assessment of liver fibrosis has been sought to estimate the risk of progression of NASH to cirrhosis, estimate the risk of cardiovascular events, aid in the surveillance of HCC, and guide therapy in patients with NAFLD/NASH. In this review, we highlight the recent advances in ultrasound elastography techniques to evaluate the liver fibrosis stage and steatosis grade in patients with NAFLD.
Present issues in the diagnosis of NASH
NASH is defined histologically by the presence of hepatic steatosis and inflammation with hepatocyte injury (hepatocyte ballooning), with or without fibrosis [9, 10]. At present, liver biopsy is recognized as the only procedure that allows reliable differentiation of nonalcoholic fatty liver (NAFL) from NASH [10]. Furthermore, a liver biopsy is the accepted gold standard for the diagnosis and staging of NAFLD in the guidelines of the Japanese Society of Gastroenterology (JSG), guidelines of the American Association for the Study of Liver Disease (AASLD), and guidelines of the European Association for the Study of the Liver (EASL) [9, 10, 12], even though it is an invasive examination, has a selection bias inherent to liver biopsy, and is impractical for repeated assessments of the liver tissue condition. More importantly, liver biopsy cannot be considered as the gold standard for a precise evaluation of the histological features of NAFLD, because the histological staging would be based on examination of biopsy specimens that represent at most 1/50,000 of the total liver mass [13]. Furthermore, the histopathologic diagnosis is mainly determined using liver tissues derived from percutaneous liver biopsies, which are prone to sampling errors and/or inter-observer variability [14, 15]. Furthermore, the characteristic histological features of NAFLD/NASH are often lost in cases of NAFLD with cirrhosis, the so-called “burned-out NASH” [16].
According to a meta-analysis, the estimated prevalence of NAFLD is 27.4% in Asia as a whole [1], and 22.3% in Japan specifically [2], with NASH accounting for 10–20% of the cases. In Japan, at present, there are an estimated 22.6 million patients with NAFLD and 3.76 million patients with NASH, including 660,000 NAFLD patients with advanced fibrosis (F3 + F4) [17]. It is impractical to examine all of these patients by liver biopsy. In actual clinical practice, the performance of liver biopsy is also deterred by patient reluctance to undergo the procedure [18]. Thus, candidates for liver biopsy should be selected on the basis of a careful risk–benefit assessment.
Current status of conventional ultrasonography in the management of NAFLD
The findings of conventional ultrasonography (US) in patients with NAFLD are often operator-dependent and include a bright liver, intrahepatic vascular blurring, and deep attenuation [18]. According to a meta-analysis of studies comparing the findings of US with the histopathological findings, abdominal US had a sensitivity of 85% and specificity of 94% for the diagnosis of moderate to the severe fatty liver [19]. On the other hand, it has been reported that it is difficult to make an accurate diagnosis of the fatty liver using the abdominal US alone in patients with morbid obesity or with hepatic steatosis of less than 20% [9, 20, 21]. Therefore, a significant number of patients with fatty liver, which is defined as a liver fat content of at least 5% of the total liver weight, can be missed [22]. In addition, the results of the visual assessment of NAFLD by US show substantial inter-observer variability and limited reproducibility [23]. As methods for early diagnosis of NAFLD, quantitative evaluations, such as calculation by computer-assisted US of the hepatic/renal ratio (H/R) and by the US of the hepatic attenuation rate, have been attempted [24]. Evaluation of inflammation and degrees of fibrosis less than those that define cirrhosis is not possible by conventional B-mode US.
Nevertheless, conventional US is still recommended for the diagnosis of moderate and severe steatosis in the current guidelines, because it is widely available, well established, noninvasive, and relatively inexpensive. Therefore, the US is considered as the first-line imaging technique in patients with clinically suspected NAFLD [9, 10, 12].
Principle and classification of ultrasound elastography
Most cases of NAFLD are asymptomatic until the disease has progressed to cirrhosis, and repeated biopsies to monitor these patients are impractical. Therefore, there is a need to develop useful noninvasively measured biomarkers to monitor disease progression. US elastography is a general term used to describe US-based methods for measuring the elasticity of liver tissue. While various devices have been developed by different companies, the imaging modalities are principally divided into two major types: strain imaging, which is a US method for measuring the liver deformation caused by compression, and shear wave imaging, which is a US method for measuring the velocity of the micro-displacements (shear waves) induced in liver tissue (Table 1). Strain imaging measures liver deformation in response to compression (by cardiac contraction or manual compression) applied to the tissue and then analyzes the images obtained. Strain imaging determines the liver stiffness by measuring the value of ε (extension per unit length) and calculating E (elasticity) = δ/ε. Shear wave imaging measures the velocity of propagation through the liver of a shear wave, which is a transverse wave formed when a vibration wave is transmitted through the liver. The velocity of the shear wave in shear wave imaging is converted into a liver stiffness measurement (LSM) expressed in kilopascals (kPa), using the following formula of E = 3ρ (tissue density) Vs2. Vibration-controlled transient elastography (VCTE, FibroScan®) is the pioneer US-based technique, and is the most widely used worldwide (with over 5100 systems distributed in over 80 countries). Other elastography modalities, such as point shear wave elastography (pSWE), which includes acoustic radiation force impulse imaging (ARFI) or two-dimensional shear wave elastography (2D-SWE) integrated into conventional US systems, are emerging (Fig. 1) [25,26,27].
Illustrations of the principles of each of the available US elastography techniques. a Real-time Tissue Elastography® (RTE) measures the liver deformation caused by compression; b vibration-controlled transient elastography (VCTE: FibroScan®) measures the speed of a mechanical pulse emitted by the probe across the liver; c point shear wave elastogpraphy (pSWE) uses pulsed focused US (acoustic push pulse) to generate a transverse elastic wave (shear wave), and the speed of the transverse wave through the tissue is measured; d two-dimensional shear wave elastography (2D-SWE) involves the combination of a radiation force induced in the tissue by focused US beams
Although both strain imaging and shear wave imaging are referred to as US elastography, the underlying principles of the two methods are different, and they should be considered as completely different procedures (Table 1, Fig. 1).
Ultrasound elastography: strain imaging
Real-time tissue elastography
The first practical use of elastography was an epoch-making event in the staging of fibrosis in patients with chronic hepatitis. Historically, the development of US elastography, beginning in the 1990 s, was aimed at the diagnosis of diseases involving sclerotic changes in tissues, such as cancer and cirrhosis, and the world’s first commercially available US-based elastography system, based on strain imaging [Real-time Tissue Elastography® (RTE)], was introduced in Japan in 2003 (EUB-8500; Hitachi Medical, Kashiwa, Japan).
When a certain external force is applied to tissue, the resulting strain varies according to the stiffness of the tissue. RTE measures the displacement magnitudes in the regions of interest (ROIs) and calculates the relative distortion by performing spatial differentiation (Table 2, Figs. 1a, 2a). Areas with a relatively small distortion (relatively hard tissue) are highlighted in blue, areas with a relatively large distortion (relatively soft tissue) are highlighted in red, and areas with an intermediate level of distortion are highlighted in green. Thus, the liver tissue is displayed as a color map in 256 colors in real time [28, 29]. The measurement methods include the liver elasticity score as a subjective measure, the liver fibrosis index (LFI) as an objective measure (incorporating nine feature values obtained from the images as independent variables into the equation), and the elastic ratio (expressed as the parenchymal to peripheral venous strain ratio of the liver).
Actual images of a Real-time Tissue Elastography® (RTE; Hitachi Healthcare, Japan); b vibration-controlled transient elastography (VCTE: FibroScan®; Echosence, France); c point shear wave elastography (pSWE; Acuson S2000, Siemens, Germany); d two-dimensional shear wave elastography (2D-SWE; Elast Q, Philips, the Netherlands)
Real-time Tissue Elastography® is indicated for various diffuse liver diseases, including viral hepatitis and NAFLD. In a study of patients with NAFLD, Ochi et al. observed a significant correlation between the elastic ratio and liver fibrosis, and a significant difference in the elastic ratios between patients with NAFLD activity score (NAS) 0–4 and ≥ 5 [30].
In the past, RTE used to be performed only with a linear probe. Therefore, in patients with large amounts of subcutaneous, visceral, and intrahepatic fat, these areas were likely to be highlighted in blue due to insufficient penetration, resulting in an overestimation of fibrosis. In recent years, it has become possible to perform RTE using a convex probe, which allows expansion of the observation field in depth, as well as widthwise, from the left to the right. This has made accurate assessment possible even in patients with thick subcutaneous fat, severe obesity, and/or severe fatty liver. In addition, unlike shear wave elastography, RTE has the advantage that the results are less influenced by inflammation, jaundice, congestion, and so forth. In general, however, strain elastography is inferior for the quantification of hepatic fibrosis than shear wave elastography (Table 3).
Ultrasound elastography: shear wave imaging
Vibration-controlled transient elastography (VCTE)
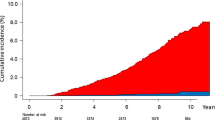
A report on the first elastography system to utilize a shear wave and shear wave speed techniques, known as vibration-controlled transient elastography (VCTE, FibroScan), to estimate liver stiffness was published in 2002 [31] (Table 1). VCTE is mounted with a one-dimensional probe and an ultrasonic transducer. The technology measures the velocity of a 50-MHz shear wave emitted by a probe in the intercostal space into the liver (Figs. 1b, 2b). The velocity is positively related to liver stiffness. The shear elastic wave travels faster through hard tissues and slower through soft tissues (Fig. 3). FibroScan® measures the shear wave velocity and calculates Young’s modulus E (kPa) using the equation, E = 3qVs2 [tissue density, q = 1 g/cm3; shear wave speed, Vs (m/s)] (Figs. 1b, 3). At that time, however, the utility of VCTE for NAFLD was hardly tested, because many hepatologists believed that US elastography was not suitable for obese patients [32]. Yoneda et al. were the first in the world to report the usefulness of VCTE for the staging of fibrosis in patients with NAFLD [33, 34]. Following these reports, VCTE began to be used for the staging of fibrosis in NAFLD patients and was thoroughly validated worldwide. VCTE is the first Food and Drug Administration (FDA)-approved elastography technique, introduced in April 2013 (Tables 1, 2). At present, VCTE is performed using three different probes for measurement under various circumstances: the standard M probe (3.5 MHz) for adults, the XL probe (2.5 MHz) for overweight patients, and the S probe (5.0 MHz) for children. Lower-frequency probes are suitable for patients who have high abdominal adiposity or have a large skin-to-liver surface distance, to reduce wave attenuation [35].
Vibration-controlled transient elastography (VCTE: FibroScan®; Echosence, France) measures the velocity of a 50-MHz shear wave that is emitted by a probe. a The results are displayed with an estimate of the shear wave speed. The distance from the probe is plotted on the y-axis, and the time of the peak of the shear wave is plotted on the x-axis. b The shear wave velocity is positively related to the liver stiffness; it travels faster through hard tissues and slower through soft tissues
The first systematic meta-analysis of VCTE (M probe) based on studies including 854 NAFLD patients was conducted by Kwok et al., which indicated a sensitivity/specificity of this modality for the diagnosis of fibrosis stages F2, F3, and F4 of 0.79/0.75, 0.85/0.85, and 0.92/0.92, respectively [36]. In the most recent meta-analysis of VCTE (M-probe) based on 11 studies and 1753 NAFLD patients, the AUROC for the diagnosis of fibrosis stage F2, F3, and F4 was 0.85, 0.92, and 0.94, respectively [37]. There is one report of a meta-analysis of the usefulness of the XL probe conducted by Xiao et al., involving three studies and 318 NAFLD patients, according to which the AUROC for the diagnosis of fibrosis stages F2, F3, and F4 was 0.82, 0.86, and 0.94, respectively [38].
Technical failure was a common phenomenon ranging in frequency from 6.7 to 27.0% and was primarily related to a high BMI [39, 40]. Because VCTE involves the transmission of a mechanical wave that originates at the skin, obesity is a significant cause of technical failure and unreliable measurements (Tables 2, 3). Lower LSM values appear to reliably exclude advanced fibrosis, but cases with early fibrosis stage could be easily misclassified by VCTE. Although the examination takes a short time and is highly reproducible (Table 2), it has the disadvantage of not allowing reliable measurement in obese patients (Table 3).
Vibration-controlled transient elastography was reported to have an accuracy corresponding to an AUROC of 0.73 for predicting all-cause mortality [41]. It is also reported as a clinically reliable follow-up method for NAFLD patients [42, 43]. The results of VCTE are known to be affected by the presence of inflammation, portal pressure, liver congestion, and mechanic cholestasis [44]. Food intake also increases liver stiffness, probably through an increase in portal blood flow [45, 46]. Other well-characterized causes of spuriously high liver stiffness include congestive heart failure [47], biliary obstruction [48], and amyloidosis [49] (Table 3). Solitary liver lesions, such as hepatic cysts and hemangiomas, have also been shown to be associated with increased LSM values [50].
Recently, the FibroScan-AST (FAST) score, calculated using the LSM and controlled attenuation parameter (CAP) obtained using FibroScan® (Echosens; Paris, France), as well as the serum level of aspartate aminotransferase (AST), was reported as being an effective measure for the identification of NASH [51, 52].
Point shear wave elastography (pSWE)
Virtual Touch™ quantification (VTQ) was the first commercially available pSWE. VTQ involves targeting the anatomic region to be examined for its elastic properties using a ROI cursor while performing real-time B-mode imaging (Table 1). VTQ uses pulsed focused US (acoustic push pulse) to generate a transverse elastic wave (shear wave) and tracking US pulses to measure the shear wave speed, and thereby tissue stiffness (Figs. 1c, 2c). The measured shear wave speed is an intrinsic and reproducible property of tissue. In VTQ, the tissue stiffness is expressed by the shear wave speed, Vs (m/s) = √Ε/2(1 + γ)ρ, where E is Young’s modulus (γ is Poisson’s ratio and ρ is the density). The technique of pSWE was developed by Siemens (Issaquah, WA, USA) and is available on Acuson S2000 and S3000 ultrasound diagnostic imaging devices, and also on the iU22 diagnostic imaging device developed by Philips (Bothell, WA, USA). This quantitative technique provides a single unidimensional measurement of tissue elasticity like the FibroScan®, although the measurement area can be positioned on a two-dimensional B-mode image (Fig. 2c, Table 2).
Yoneda et al. were the first to report the usefulness of pSWE in patients with NAFLD in 2010 [53]. Then, Cassinotto reported the following AUROC values for the diagnosis of various stages of fibrosis in 291 NAFLD patients: 0.77 for fibrosis stage ≥ F2, 0.84 for ≥ F3, and 0.84 for F4 (cirrhosis), which suggest that the ability of pSWE to detect fibrosis in patients with NAFLD/NASH is almost equivalent to that of VCTE [54]. A systematic review of seven studies including 723 NAFLD patients reported a summary sensitivity and specificity of 80.2 and 85.2%, respectively, for the detection of ≥ F2 fibrosis [55]. In 2020, the most recent systematic review and meta-analysis based on 13 studies including 1147 NAFLD patients reported that the AUROC for the diagnosis of fibrosis stages F2, F3, and F4 was 0.89, 0.94, and 0.94, respectively [56]. There are no available data on the follow-up of the severity of fibrosis in NAFLD patients using pSWE.
Like VCTE, the results of pSWE have also been reported to be influenced by other factors, e.g., the presence of inflammation. The focused US pulse, which penetrates subcutaneous fat and ascites, allows measurement even in patients with ascites and obesity [57, 58] (Table 3). Therefore, the reported failure rate of pSWE is quite low (1–2%) [27]. However, the rate of unreliable LSM in obese patients undergoing pSWE was similar or higher than that obtained with SWE or VCTE [54]. Further investigation in NAFLD patients is necessary to confirm these findings.
Although validation studies are fewer as compared to those for VCTE, pSWE is clinically useful because they can be performed together with a regular US examination, which allows structural examination and HCC surveillance.
2D-shear wave elastography (2D-SWE)
The principle underlying 2D-SWE is that the combination of a radiation force induced in tissues by focused US beams and a very high-frame-rate US imaging sequence enables propagation of the resultant shear waves to be captured in real time (Table 1). The radial forces that generate the shear waves are focused at increasing depths, causing a shear wavefront to propagate in the scanned area (Fig. 1). The US system then captures the generated shear waves. The shear wave speed, subsequently estimated by a Doppler-like acquisition over a ROI, is then used to calculate the tissue stiffness. Elasticity is displayed by color mapping of the elasticity encoded pixel by pixel, with the color map image superimposed on the standard B-mode image (Fig. 2d). Stiffer tissues appear in red and softer tissues appear in blue [59, 60]. 2D-SWE was first incorporated into Aixplorer®, manufactured by Supersonic Imagine, and launched in 2010. Thereafter, it was also incorporated into the “LOGIQ” series manufactured by GE Healthcare, Virtual Touch™ Image Quantification manufactured by Siemens, Aplio and Xario manufactured by Canon Medical Systems, and EPIQ and Affiniti manufactured by Philips (Table 1). The operator, assisted by a real-time B-mode US image, places the designated ROI on the color map. A retrospective meta-analysis of 2D-SWE that included 1340 patients with chronic liver disease from 13 centers worldwide reported diagnostic accuracy of 91% (optimal cutoff, 9.2 kPa) and 95% (optimal cutoff, 13.5 kPa) for advanced fibrosis and cirrhosis, respectively [61]. In the subgroup of 172 NAFLD patients, the diagnostic accuracy was 93% and 92% for advanced fibrosis and cirrhosis, respectively, with the same optimal cutoffs as for the overall group. In another study of 291 NAFLD patients, the reported AUROC was 0.86 for fibrosis stage ≥ F2, 0.89 for ≥ F3, and 0.88 for F4 fibrosis (cirrhosis) [54]. For the diagnosis of liver fibrosis in NAFLD patients, it has been reported that 2D-SWE is superior to pSWE and comparable to VCTE in terms of the diagnostic ability for fibrosis stage ≥ F2 [54].
According to a report by Yoneda et al., 2D-SWE showed an almost equivalent diagnostic success rate and diagnostic ability to those of FibroScan® with the XL probe in obese patients [62]. However, SWE is affected by inflammation and jaundice, and 2D-SWE is reportedly influenced by blood stasis, or congestion [63]. Furthermore, the accuracy of 2D-SWE is affected by inter-observer variation and food intake [64]. Therefore, it is recommended that these measurements be performed by very experienced sonographers or radiologists after the patient has fasted for at least 2 h. Just like pSWE, 2D-SWE can also be performed together with a regular US examination for HCC surveillance (Table 3).
Ultrasound-based technologies for grading hepatic steatosis
Controlled attenuation parameter
The controlled attenuation parameter (CAP) is a VCTE-based measure for quantifying the liver fat via evaluation of the US attenuation in the liver, and is expressed in decibels per meter (range of 100–400 dB/m) (Fig. 4). The same radiofrequency data as for determination of the LSM are used for determining the CAP, and the value is only appraised if the acquisition is valid. Similar to the US, CAP measurement is also affected by obesity. Failed examinations are more common in obese patients [63], although this problem has been largely mitigated by the development of the XL probe [65].
A meta-analysis of 19 studies of the M probe and including 2735 patients (527 patients with NAFLD) was reported by Karlas et al. [66]. According to the report, the AUROC values were 0.82, 0.81, and 0.78 for the diagnosis of grade ≥ 1, ≥ 2, and 3 steatosis, respectively, with a sensitivity/specificity of 69%/82%, 77%/81%, and 88%/78%, respectively [66]. The cutoff values for diagnosing grade ≥ 1, ≥ 2, and 3 steatosis were proposed to be 248 dB/m, 268 dB/m, and 289 dB/m, respectively. Since the measurement results depend on the distance to the liver surface, the measurement in highly obese patients is performed using the XL probe. In a recent multicenter study of the XL probe conducted in 393 NAFLD patients, the CAP had an AUROC of 0.76 for the detection of steatosis > 5% and a 96% positive predictive value at a cutoff level of 263 db/m [67].
However, the reliability and cutoff values of CAP with the M as compared to the XL probe are also an issue that needs to be debated, because the transmission frequency varies depending on the type of probe. In addition, it should also be noted that the sensitivity is low for livers with only slight fat deposition, and inter-observer variability would be expected.
Because steatosis is a reversible marker reflecting the potential for further liver injury, CAP is a promising investigational tool for clinicians to advise patients on future risks and therapeutic strategies. However, the clinical significance of measuring the degree of hepatic steatosis is unclear [4, 68]. Some studies suggest that the accuracy of CAP for the detection of hepatic steatosis is lower in obese patients [69, 70]. Moreover, significant liver fibrosis may affect the US attenuation and decrease the diagnostic performance of CAP [70]. Recently, a study that followed 4282 patients who had undergone CAP measurement showed that neither the presence nor the severity of hepatic steatosis predicted liver-related events, cancer, or cardiovascular events in the short term, while LSM and the underlying etiology independently predicted liver-related events [71]. Therefore, the results of longitudinal studies are awaited.
Attenuation imaging, attenuation coefficient and ultrasound-guided attenuation parameter
Attenuation imaging (ATI: “Aplio i800” by Canon Medical Systems) is a technique in which the US propagation properties and acoustic transmission characteristics unique to the probe are excluded. After removal of the focus-dependent beam profile and gain-adjusted profile from the echo signals, the rate of attenuation attributable only to the properties of the biological tissue is calculated. Then, tomographic images are reconstructed with the obtained attenuation coefficients, and the result is presented as a color map. ATI allows quantitative assessment of hepatic steatosis by reference to the B-mode images and allows 2D-SWE and ATI without changing the probe. Therefore, blood vessels and structures can be excluded from the map and the measurement area by reference to the B-mode images. This allows the measurement area to be limited to the area of interest. The ATI values increase significantly with increasing steatosis grade. The AUROC for the detection of grade ≥ 1, ≥ 2, and 3 steatosis in NAFLD patients were 0.77, 0.88, and 0.86, respectively [72]. Furthermore, ATI showed high intra- and inter-observer reproducibility for the assessment of hepatic steatosis [73].
Attenuation coefficient (ATT) in the ARIETTA 850® manufactured by Fujifilm (formerly Hitachi) is also a new diagnostic method of US B-mode imaging [74, 75]. US B-mode uses multiple US waves with different frequency components for measurement. ATT estimates hepatic steatosis from differences in attenuation of the received signals in real time. ATT measurement was correlated with histological steatosis grade [74, 75].
Similarly, a tool called Ultrasound-guided Attenuation Parameter (UGAP) has been reported to be available in the LOGIQ series® manufactured by GE Healthcare. The AUROC of UGAP for identifying ≥ S2 and S3 were better than the results obtained with CAP [76]. According to a previous report, the results of assessment using UGAP were strongly correlated with the results of assessment based on the proton density fat fraction (PDFF) measured by MRI [77], and the result of UGAP was weakly affected by liver stiffness [78].
Conclusion
The number of patients with NAFLD/NASH has increased worldwide, with the westernization of lifestyles. Although liver-related events are a relatively minor cause of mortality among NAFLD patients, NAFLD is on the threshold of becoming the most common cause of liver disease and liver-related death globally [79]. Previous studies have reported that the degree of liver fibrosis is an important prognostic factor in patients with NAFLD/NASH, being associated not only with the risk of development of cirrhosis and hepatocellular carcinoma but also with the risk of development of cardiovascular events [80]. The major advantage of US elastography, as compared to liver biopsy, is that it is painless and rapid, is not associated with complications, and is universally accepted by patients. Even in patients in whom the presence of hepatic cirrhosis is obvious, there are two additional benefits of measuring liver stiffness; first, a higher degree of stiffness in patients with cirrhosis could be of diagnostic value for detecting the presence of large varices [81], and second, a greater value of liver stiffness may be predictive of other complications and subsequent liver-related death [82]. US elastography is expected to become an optimal examination for the follow-up of NAFLD patients, and is expected to take its own position as a liver assessment technique, rather than being used only as an alternative to liver biopsy.
Abbreviations
- AASLD:
-
American Association for the Study of Liver Disease
- ALT:
-
ALANINE AMINOTRANSFERASE
- ARFI:
-
Acoustic radiation force impulse
- BMI:
-
Body mass index
- CAP:
-
Controlled attenuation parameter
- EASL:
-
European Association for the Study of the Liver
- FDA:
-
Food and Drug Administration
- HCC:
-
Hepatocellular carcinoma
- JSG:
-
Japanese Society of Gastroenterology
- kPa:
-
Kilopascal
- LSM:
-
Liver stiffness measurement
- NAFL:
-
Nonalcoholic fatty liver
- NAFLD:
-
Nonalcoholic fatty liver disease
- NAS:
-
NAFLD activity score
- NASH:
-
Nonalcoholic steatohepatitis
- pSWE:
-
Point shear wave elastography
- ROI:
-
Region of interest
- 2D-SWE:
-
Two-dimensional shear wave elastography
- T2DM:
-
Type 2 diabetes mellitus
- US:
-
Ultrasonography
- VCTE:
-
Vibration-controlled transient elastography
References
Younossi ZM, Koenig AB, Abdelatif D, et al. Global epidemiology of nonalcoholic fatty liver disease—meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64:73–84.
Li J, Zou B, Yeo YH, et al. Prevalence, incidence, and outcome of non-alcoholic fatty liver disease in Asia, 1999–2019: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2019;4:389–98.
Singh S, Allen AM, Wang Z, et al. Fibrosis progression in nonalcoholic fatty liver vs nonalcoholic steatohepatitis: a systematic review and meta-analysis of paired-biopsy studies. Clin Gastroenterol Hepatol. 2015;13:643–654.e1–9.
Ekstedt M, Hagstrom H, Nasr P, et al. Fibrosis stage is the strongest predictor for disease-specific mortality in NAFLD after up to 33 years of follow-up. Hepatology. 2015;61:1547–54.
Marchesini G, Bugianesi E, Forlani G, et al. Nonalcoholic fatty liver, steatohepatitis, and the metabolic syndrome. Hepatology. 2003;37:917–23.
Angulo P. Nonalcoholic fatty liver disease. N Engl J Med. 2002;346:1221–31.
Dulai PS, Singh S, Patel J, et al. Increased risk of mortality by fibrosis stage in nonalcoholic fatty liver disease: systematic review and meta-analysis. Hepatology. 2017;65(5):1557–65.
Kleiner DE, Brunt EM, Van Natta M, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology. 2005;41:1313–21.
Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67:328–57.
European Association for the Study of the Liver (EASL), European Association for the Study of Diabetes (EASD), European Association for the Study of Obesity (EASO). EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. J Hepatol. 2016;64:1388–402.
Cadranel JF. Good clinical practice guidelines for fine needle aspiration biopsy of the liver: past, present and future. Gastroenterol Clin Biol. 2002;26:823–4.
Watanabe S, Hashimoto E, Ikejima K, et al. Evidence-based clinical practice guidelines for nonalcoholic fatty liver disease/nonalcoholic steatohepatitis. J Gastroenterol. 2015;50:364–77.
Bravo AA, Sheth SG, Chopra S. Liver biopsy. N Engl J Med. 2001;344:495–500.
Bedossa P, Dargere D, Paradise V. Sampling variability of liver fibrosis in chronic hepatitis C. Hepatology. 2003;38:1449–57.
Maharaj B, Maharaj RJ, Leary WP, et al. Sampling variability and its influence on the diagnostic yield of percutaneous needle biopsy of the liver. Lancet. 1986;1:523–5.
Caldwell SH, Lee VD, Kleiner DE, et al. NASH and cryptogenic cirrhosis: a histological analysis. Ann Hepatol. 2009;8:346–52.
Estes C, Anstee QM, Arias-Loste MT, et al. Modeling NAFLD disease burden in China, France, Germany, Italy, Japan, Spain, United Kingdom, and United States for the period 2016–2030. J Hepatol. 2018;69:896–904.
Sanyal AJ. AGA technical review on nonalcoholic fatty liver disease. Gastroenterology. 2002;123:1705–25.
Hernaez R, Lazo M, Bonekamp S, et al. Diagnostic accuracy and reliability of ultrasonography for the detection of fatty liver: a meta-analysis. Hepatology. 2011;54:1082–90.
Xia MF, Yan HM, He WY, et al. Standardized ultrasound hepatic/renal ratio and hepatic attenuation rate to quantify liver fat content: an improvement method. Obesity (Silver Spring). 2012;20:444–52.
Fedchuk L, Nascimbeni F, Pais R, et al. Performance and limitations of steatosis biomarkers in patients with nonalcoholic fatty liver disease. Aliment Pharmacol Ther. 2014;40:1209–22.
Paige JS, Bernstein GS, Heba E, et al. A pilot comparative study of quantitative ultrasound, conventional ultrasound, and MRI for predicting histology-determined steatosis grade in adult nonalcoholic fatty liver disease. AJR Am J Roentgenol. 2017;208:W168–77.
Cengiz M, Sentürk S, Cetin B, et al. Sonographic assessment of fatty liver: intraobserver and interobserver variability. Int J Clin Exp Med. 2014;7:5453–60 (eCollection 2014).
Zhang B, Ding F, Chen T, et al. Ultrasound hepatic/renal ratio and hepatic attenuation rate for quantifying liver fat content. World J Gastroenterol. 2014;20:17985–92.
Dietrich C, Bamber J, Berzigotti A, et al. EFSUMB guidelines and recommendations on the clinical use of liver ultrasound elastography, update 2017 (long version). Eur J Ultrasound. 2017;38:e16–47.
Friedrich-Rust M, Poynard T, Castera L. Critical comparison of elastography methods to assess chronic liver disease. Nat Rev Gastroenterol Hepatol. 2016;13:402–11.
Ferraioli G, Wong VW, Castera L, et al. Liver ultrasound elastography: an update to the world federation for ultrasound in medicine and biology guidelines and recommendations. Ultrasound Med Biol. 2018;44:2419–40.
Matsumura T, Shiina T, Oosaka T, et al. Development of real- time tissue elastography. MEDIX. 2004;41:30–5.
Shiina T, Nightingale KR, Palmeri ML, et al. WFUMB guidelines and recommendations for clinical use of ultrasound elastography: part 1: basic principles and terminology. Ultrasound Med Biol. 2015;41:1126–47.
Ochi H, Hirooka M, Koizumi Y, et al. Real-time tissue elastography for evaluation of hepatic fibrosis and portal hypertension in nonalcoholic fatty liver diseases. Hepatology. 2012;56:1271–8.
Sandrin L, Tanter M, Gennisson JL, et al. Shear elasticity probe for soft tissues with 1-D transient elastography. IEEE Trans Ultrason Ferroelectr Freq Control. 2002;49:436–46.
Yoneda M, Imajo K, Nakajima A. Non-invasive diagnosis of nonalcoholic fatty liver disease. Am J Gastroenterol. 2018;113:1409–11.
Yoneda M, Yoneda M, Fujita K, et al. Transient elastography in patients with non-alcoholic fatty liver disease (NAFLD). Gut. 2007;56:1330–1.
Yoneda M, Yoneda M, Mawatari H, et al. Noninvasive assessment of liver fibrosis by measurement of stiffness in patients with nonalcoholic fatty liver disease (NAFLD). Dig Liver Dis. 2008;40:371–8.
de Lédinghen V, Vergniol J, Foucher J, et al. Feasibility of liver transient elastography with FibroScan using a new probe for obese patients. Liver Int. 2010;30:1043–8.
Kwok R, Tse YK, Wong GL, et al. Systematic review with meta-analysis: non-invasive assessment of non-alcoholic fatty liver disease–the role of transient elastography and plasma cytokeratin-18 fragments. Aliment Pharmacol Ther. 2014;39:254–69.
Jiang W, Huang S, Teng H. Diagnostic accuracy of point shear wave elastography and transient elastography for staging hepatic fibrosis in patients with non-alcoholic fatty liver disease: a meta-analysis. BMJ Open. 2018;8(8):e021787.
Xiao G, Zhu S, Xiao X, et al. Comparison of laboratory tests, ultrasound, or magnetic resonance elastography to detect fibrosis in patients with nonalcoholic fatty liver disease: a meta-analysis. Hepatology. 2017;66:1486–501.
Wong VW, Vergniol J, Wong GL, et al. Diagnosis of fibrosis and cirrhosis using liver stiffness measurement in nonalcoholic fatty liver disease. Hepatology. 2010;51:454–62.
de Lédinghen V, Vergniol J. Transient elastography (FibroScan). Gastroenterol Clin Biol. 2008;32:58–67.
Boursier J, Vergniol J, Guillet A, et al. Diagnostic accuracy and prognostic significance of blood fibrosis tests and liver stiffness measurement by FibroScan in non-alcoholic fatty liver disease. J Hepatol. 2016;65:570–8.
Kamarajah SK, Chan WK, Mustapha NRN, et al. Repeated liver stiffness measurement compared with paired liver biopsy in patients with non-alcoholic fatty liver disease. Hepatol Int. 2018;12:44–5.
Nogami A, Yoneda M, Kobayashi T, et al. Assessment of 10-year changes in liver stiffness using vibration-controlled transient elastography in non-alcoholic fatty liver disease. Hepatol Res. 2019;49:872–80.
Mueller S, Sandrin L. Liver stiffness: a novel parameter for the diagnosis of liver disease. Hepat Med. 2010;2:49–67.
Mederacke I, Wursthorn K, Kirschner J, et al. Food intake increases liver stiffness in patients with chronic or resolved hepatitis C virus infection. Liver Int. 2009;29:1500–6.
Popescu A, Bota S, Sporea I, et al. The influence of food intake on liver stiffness values assessed by acoustic radiation force impulse elastography-preliminary results. Ultrasound Med Biol. 2013;39:579–84.
Millonig G, Friedrich S, Adolf S, et al. Liver stiffness is directly influenced by central venous pressure. J Hepatol. 2010;52:206–10.
Millonig G, Reimann FM, Friedrich S, et al. Extrahepatic cholestasis increases liver stiffness (FibroScan) irrespective of fibrosis. Hepatology. 2008;48:1718–23.
Loustaud-Ratti VR, Cypierre A, Rousseau A, et al. Non-invasive detection of hepatic amyloidosis: FibroScan, a new tool. Amyloid. 2011;18:19–24.
Wong GL, Kwok R, Wong VW. Huge adrenal hemangioma: a rare cause of deceivingly high liver stiffness measurement by transient elastography. Clin Gastroenterol Hepatol. 2015;13:e37–8.
Newsome PN, Sasso M, Deeks JJ, et al. FibroScan-AST (FAST) score for the non-invasive identification of patients with non-alcoholic steatohepatitis with significant activity and fibrosis: a prospective derivation and global validation study. Lancet Gastroenterol Hepatol. 2020;5:362–73.
Oeda S, Takahashi H, Imajo K, et al. Diagnostic accuracy of FibroScan-AST score to identify non-alcoholic steatohepatitis with significant activity and fibrosis in Japanese patients with non-alcoholic fatty liver disease: comparison between M and XL probes. Hepatol Res. 2020;50:831–9.
Yoneda M, Suzuki K, Kato S, et al. Nonalcoholic fatty liver disease: US-based acoustic radiation force impulse elastography. Radiology. 2010;256:640–7.
Cassinotto C, Boursier J, de Lédinghen V, et al. Liver stiffness in nonalcoholic fatty liver disease: a comparison of supersonic shear imaging, FibroScan, and ARFI with liver biopsy. Hepatology. 2016;63:1817–27.
Liu H, Fu J, Hong R, et al. Acoustic radiation force impulse elastography for the non-invasive evaluation of hepatic fibrosis in non-alcoholic fatty liver disease patients: a systematic review & meta-analysis. PLoS One. 2015;10(7):e0127782.
Lin Y, Li H, Jin C, et al. The diagnostic accuracy of liver fibrosis in non-viral liver diseases using acoustic radiation force impulse elastography: a systematic review and meta-analysis. PLoS One. 2020;15:e0227358.
Friedrich-Rust M, Nierhoff J, Lupsor M, et al. Performance of acoustic radiation force impulse imaging for the staging of liver fibrosis: a pooled meta-analysis. J Viral Hepat. 2012;19:e212–9.
Frulio N, Trillaud H. Ultrasound elastography in liver. Diagn Interv Imaging. 2013;94:515–34.
Muller M, Gennisson JL, Deffieux T, et al. Quantitative viscoelasticity mapping of human liver using supersonic shear imaging: preliminary in vivo feasibility study. Ultrasound Med Biol. 2009;35:219–29.
Bercoff J, Tanter M, Fink M. Supersonic shear imaging: a new technique for soft tissue elasticity mapping. IEEE Trans Ultrason Ferroelectr Freq Control. 2004;51:396–409.
Herrmann E, de Lédinghen V, Cassinotto C, et al. Assessment of biopsy-proven liver fibrosis by two-dimensional shear wave elastography: an individual patient data-based meta-analysis. Hepatology. 2018;67:260–72.
Yoneda M, Thomas E, Sclair SN, et al. Supersonic shear imaging and transient elastography with the XL probe accurately detect fibrosis in overweight or obese patients with chronic liver disease. Clin Gastroenterol Hepatol. 2015;13(1502–9):e5.
Wong GL, Wong VW, Chim AM, et al. Factors associated with unreliable liver stiffness measurement and its failure with transient elastography in the Chinese population. J Gastroenterol Hepatol. 2011;26:300–5.
Furlan A, Tublin ME, Yu L, et al. Comparison of 2D shear wave elastography, transient elastography, and MR elastography for the diagnosis of fibrosis in patients with nonalcoholic fatty liver disease. AJR Am J Roentgenol. 2020;214(1):W20–6.
Wong VW, Vergniol J, Wong GL, et al. Liver stiffness measurement using XL probe in patients with nonalcoholic fatty liver disease. Am J Gastroenterol. 2012;107:1862–71.
Karlas T, Petroff D, Sasso M, et al. Individual patient data meta-analysis of controlled attenuation parameter (CAP) technology for assessing steatosis. J Hepatol. 2017;66:1022–30.
Siddiqui MS, Vuppalanchi R, Van Natta ML, et al. Vibration-controlled transient elastography to assess fibrosis and steatosis in patients with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2019;17(156–163):e2.
Younossi ZM, Stepanova M, Rafiq N, et al. Pathologic criteria for nonalcoholic steatohepatitis: interprotocol agreement and ability to predict liver-related mortality. Hepatology. 2011;53:1874–82.
Chan WK, Nik Mustapha NR, Mahadeva S. Controlled attenuation parameter for the detection and quantification of hepatic steatosis in nonalcoholic fatty liver disease. J Gastroenterol Hepatol. 2014;29:1470–6.
Fujimori N, Tanaka N, Shibata S, et al. Controlled attenuation parameter is correlated with actual hepatic fat content in patients with non-alcoholic fatty liver disease with none-to-mild obesity and liver fibrosis. Hepatol Res. 2016;46:1019–27.
Liu K, Wong VW, Lau K, et al. Prognostic value of controlled attenuation parameter by transient elastography. Am J Gastroenterol. 2017;112:1812–23.
Tada T, Iijima H, Kobayashi N, et al. Usefulness of attenuation imaging with an ultrasound scanner for the evaluation of hepatic steatosis. Ultrasound Med Biol. 2019;45:2679–87.
Yoo J, Lee JM, Joo I, et al. Reproducibility of ultrasound attenuation imaging for the noninvasive evaluation of hepatic steatosis. Ultrasonography. 2020;39:121–9.
Tamaki N, Koizumi Y, Hirooka M, et al. Novel quantitative assessment system of liver steatosis using a newly developed attenuation measurement method. Hepatol Res. 2018;48:821–8.
Koizumi Y, Hirooka M, Tamaki N, et al. New diagnostic technique to evaluate hepatic steatosis using the attenuation coefficient on ultrasound B mode. PLoS One. 2019;14:e0221548.
Fujiwara Y, Kuroda H, Abe T, et al. The B-mode image-guided ultrasound attenuation parameter accurately detects hepatic steatosis in chronic liver disease. Ultrasound Med Biol. 2018;44:2223–32.
Tada T, Kumada T, Toyoda H, et al. Utility of attenuation coefficient measurement using an ultrasound-guided attenuation parameter for evaluation of hepatic steatosis: comparison with MRI-determined proton density fat fraction. AJR Am J Roentgenol. 2019;212:332–41.
Tada T, Kumada T, Toyoda H, et al. Liver stiffness does not affect ultrasound-guided attenuation coefficient measurement in the evaluation of hepatic steatosis. Hepatol Res. 2020;50:190–8.
Rinella M, Charlton M. The globalization of nonalcoholic fatty liver disease: prevalence and impact on world health. Hepatology. 2016;64:19–22.
Angulo P, Kleiner DE, Dam-Larsen S, et al. Liver fibrosis, but no other histologic features, is associated with long-term outcomes of patients with nonalcoholic fatty liver disease. Gastroenterology. 2015;149(389–97):e10.
Berzigotti A, Seijo S, Arena U, et al. Elastography, spleen size, and platelet count identify portal hypertension in patients with compensated cirrhosis. Gastroenterology. 2013;144:102–11.
Vergniol J, Foucher J, Terrebonne E, et al. Noninvasive tests for fibrosis and liver stiffness predict 5-year outcomes of patients with chronic hepatitis C. Gastroenterology. 2011;140:1970–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Ethical statements
All procedures followed were in accordance with the ethical standards of the responsible committees for human experimentation (institutional and national) and in compliance with the principles laid down in the Helsinki Declaration adopted in 1964 and its later versions.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Yoneda, M., Honda, Y., Nogami, A. et al. Advances in ultrasound elastography for nonalcoholic fatty liver disease. J Med Ultrasonics 47, 521–533 (2020). https://doi.org/10.1007/s10396-020-01040-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10396-020-01040-8