Abstract
Purpose
To evaluate in vitro the feasibility of therapeutic high-intensity-focused ultrasound (HIFU) combined with microbubbles and titanium dioxide (TiO2).
Methods
Oral squamous cell carcinoma cells (HSC-2) were sonicated using a HIFU transducer with a resonant frequency of 3.5 MHz, 30 mm in diameter, and focal length of 50 mm. The ultrasound intensity was 210 W/cm2, and two pulses (0.5 s each) were sonicated for each cell sample (9 × 104 cells per well). Immediately after HIFU, the viable cells were measured by an automated cell counter. The survival rate was measured in the presence of microbubbles (Sonazoid) and peroxo titania-silica (R-P-TS) or anatase titania-silica (R-A-TS) TiO2.
Results
Cell viability immediately following sonication in the presence of TiO2 (R-A-TS) and TiO2 (R-P-TS) was 65.5 ± 0.7 and 59.4 ± 3.3 %, respectively. A marked decrease in cell viability was seen when microbubbles were added to the above cell conditions. Specifically, cell viability decreased to 14.0 ± 0.1 and 4.4 ± 0.9 % when microbubbles were added to samples containing TiO2 (R-A-TS) and TiO2 (R-P-TS), respectively.
Conclusion
Immediate in vitro cell killing was observed with short pulsed duration HIFU sonication with a combination of microbubbles and TiO2. This finding suggests that TiO2 could have caused enhanced mechanical cell destruction by microbubbles.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
High-intensity-focused ultrasound (HIFU) is a novel therapeutic method that has emerged in recent years as a ‘focal’ treatment alternative in which various cancers can be eradicated while greatly reducing the side effects of radical treatment. Although the current clinical strategies employ HIFU exclusively for thermal ablation of the target sites, there is considerable interest in other mechanisms, such as chemical and mechanical tissue damage from focused ultrasound, which have not been thoroughly investigated.
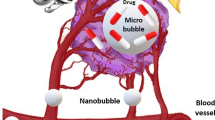
Titanium dioxide (TiO2) is generally known as a photocatalyst, generating reactive oxygen species under ultraviolet irradiation. Interestingly, Ogino et al. [1] discovered an alternative TiO2 activation method that uses ultrasound (US) irradiation instead of ultraviolet irradiation. Additionally, Harada et al. [2] recently demonstrated the cell-killing effect of TiO2 nanoparticles under US irradiation both in vitro and in vivo. The mechanism of cell damage involving use of nanoparticle TiO2 in the medical field has drawn significant attention. On the other hand, in the field of bubble dynamics, it is well known that microbubbles can play a major role in killing cancer cells and also accelerating thrombolysis [3], which mainly involves mechanical energy. This phenomenon is induced by transient bubble disruption that generates shockwaves and microjets [4], and with stable bubble oscillation, acoustic microstreaming [5–7].
To date, there have been no studies on evaluation of ultrasound cell killing in combination with TiO2 and microbubbles in the literature. The aim of the present study was to evaluate in vitro the feasibility of therapeutic HIFU combined with microbubbles and TiO2. Furthermore, experiments were carried out to determine whether the enhancement of microbubble mechanical damage can be achieved by addition of TiO2.
Materials and methods
Cell culture
Cells from an oral squamous cell carcinoma cell line, HSC-2 [purchased from Japanese Collection of Research Bioresources (JCRB) Cell Bank], were maintained in a MEM medium (Wako, Osaka, Japan) with 10 % fetal bovine serum (Invitrogen, Tokyo, Japan) at 37.0 °C in humidified air with 5 % CO2. Immediately before each experiment, HSC-2 cells were collected by Trypsin–EDTA (Gibco, NY, USA) treatment and centrifugation. Cell viability before treatment was always over 98 %.
Aliquots of the final HSC-2 cell line suspension at a volume of 500 μl (9 × 104 cells per well) were placed as a completed medium onto a Lumox® Multiwell (SARSTEDT, Germany) plate with a flat film bottom (50 µ thickness) before each ultrasound treatment.
Titanium dioxide
A titania-silica aqueous solution was used as a sonocatalyst. This solution is sold as a photocatalyst under the name RINKOH (Titania Global Science and Technology LLP, Fukuoka, Japan). RINKOH has an R-P-TS (peroxo titania-silica) type and an R-A-TS (anatase titania-silica) type. RINKOH is a special photocatalyst prepared by coupling of titanium oxide and silicon oxide with hydrogen peroxide. The solid concentration is 1.0 % in water suspension, the hydrogen-ion concentration is 6–9 ppm, nanoparticles are uniform with an average size of about 10–30 nm in diameter, and the color tone is milky. R-P-TS solution contains 0.028–0.030 % peroxide on a hydrogen peroxide conversion basis and 2.8–3.9 % peroxide per solid weight. R-A-TS solution, on the other hand, contains 0.0008–0.0010 % peroxide on a hydrogen peroxide conversion basis, and a maximum of 0.1 % peroxide per solid weight. Comparing the two solutions, R-P-TS has a 30- to 39-fold higher peroxide concentration than R-A-TS per solid weight. Both of these materials were stable and had no tendency of aggregation within biological fluids used in the present experiment. Cell suspension containing a final concentration of 10 % titania-silica solution was used for each experiment.
Microbubbles
The microbubble contrast agent used in these experiments was Sonazoid (phospholipid shell encapsulating perfluorobutane gas; Daiichi-Sankyo, Tokyo, Japan). Sonazoid is a clinically approved ultrasound contrast agent with an average diameter of 3.2 µm. Sonazoid microbubbles were diluted with sterilized distilled water for at least 5 min before use. The final volume of Sonazoid was adjusted to 10 % of the medium within each sample cell culture well.
HIFU sonication protocol
Sonication was carried out using an experimental non-clinical laboratory sonicator device for all in vitro studies. An ultrasound generator (SonoPore KTAC-4000, Nepagene, Chiba, Japan) connected to a HIFU Transducer (Nepagene) generated high-intensity-focused ultrasound with a resonant frequency of 3.5 MHz. The diameter of the transducer was 30 mm, the focal length was 50 mm, and the diameter of the focal zone was 1.1 mm in the lateral and 12 mm in the axial directions (full width at half maximum, FWHM). Ultrasound intensity was measured in a separate experiment in a large test tank with a rubber absorber panel facing the transducer to eliminate wave reflection. Ultrasound spatial-average pulse-average intensity (Isapa) was 210 W/cm2, and two pulses (0.5 s each) were sonicated for each cell sample. Aliquots of the final HSC-2 cell line suspension, at a volume of 500 μl (9 × 104 cells per well), were placed as a completed medium onto a 24-well Lumox® Multiwell (SARSTEDT) plate, which has a 50-μm-thick gas permeable bottom. The bottom was also acoustically transparent. The 24-well plate was placed on top of the US transducer. Degassed water was circulated between the transducer surface and the bottom of the plate. Custom-made cylindrical acoustic absorbers (EUA101A, Eastek, Japan, >40 dB at 1 MHz) were used on the opposite side of the US probe in order to reduce ultrasound reflections and eliminate standing waves. No sign of damage to the absorbers that could have led to elution of toxic substances to the cells was observed. After adding the cell suspension to each well, the absorbers were placed in the plate nesting directly on the surface of the cell suspension with no air pockets remaining between them. Temperature measurement of cell suspension immediately before and after treatment by US by a needle thermometer (Tele-Thermometer, Yellow Springs Instrument, OH, USA) showed no significant change. The entire experimental setup is shown in Fig. 1. HIFU intensity was fixed at 210 W/cm2. Immediately after HIFU sonication, the number of viable cells was evaluated by an automated cell counter (TC20, BioRad, USA). A sample volume, 10 μl of 1:1 mixture of cell suspension with Trypan blue dye, was loaded on a dual-chamber slide for cell viability measurements. The viability ratio of cells was calculated using the following formula:
The automated cell counter device uses multi-focal plane analysis for live/dead cell count. Each acoustic and drug condition consisted of at least three identical samples (n = 3). Expression data from this study were analyzed using unpaired t test including Welch’s correction. Results were considered to be significant when the corrected P value was less than 0.05.
Microscope Observation
Optical microscopes were used in order to evaluate the acute morphologic changes to cells immediately after treatment. Cells were extracted from each sonicated or non-sonicated sample and placed inside chamber slides. Observations were started only after the cells gently settled down on the bottom of the slide glass container after 30 min. Cells treated with TiO2 were observed with an inverted microscope (Leica DMI3000 B, Leica Microsystems, Germany) and all-in-one BZ-X700 optical microscope (Keyence, Osaka, Japan).
Results
Cell viability of HSC-2 cells in the presence of TiO2 (R-A-TS) and TiO2 (R-P-TS) was 99.0 ± 1.3 and 86.5 ± 4.5 %, respectively. TiO2 (R-P-TS) alone showed greater cytotoxicity as compared with TiO2 (R-P-TS) alone. No significant cytotoxicity (P < 0.05) was observed with TiO2 (R-A-TS) alone as compared with untreated control cells. Ultrasound alone (210 W/cm2, total duration 1.0 s) to the cells showed cell viability of 94.1 ± 6.5 %. Cytotoxicity of ultrasound exposure in the presence of microbubbles showed a significant decrease in cell viability to 37.6 ± 6.8 %.
HSC-2 cells were exposed to HIFU in the presence of the two types of TiO2 at an intensity of 250 W/cm2 (duration total 1 s). Cell viability immediately following sonication in the presence of TiO2 (R-A-TS) and TiO2 (R-P-TS) was 65.5 ± 0.7 and 59.4 ± 3.3 %, respectively. A marked decrease in cell viability was observed when microbubbles were added to the above cell conditions. Samples containing TiO2 (R-A-TS) and TiO2 (R-P-TS) showed a decrease in cell viability to 14.0 ± 0.1 and 4.4 ± 0.9 %, respectively, in the presence of microbubbles (Fig. 2).
As the automated cell counter cannot detect the cells that completely disappear due to treatment, the cell destruction percentage was estimated by counting the absolute number of Trypan blue-negative live cells before and after treatment. The cell destruction percentage was calculated using the following formula:
The cell destruction percentage of HIFU sonication and/or in the presence of TiOs and/or microbubbles is shown in Fig. 3. The percentage of cell destruction in each ultrasound-sonicated sample was greater in the TiO2 (R-P-TS) + MB groups than in the TiO2 (R-A-TS) + MB groups. Compared to the microbubble only groups, cell destruction showed a two-fold increase in the TiO2 (R-A-TS) group and a three-fold increase in the TiO2 (R-P-TS) group (Fig. 4).
Optical microscope (BZ-X700, Keyence) observation revealed significant cell morphological changes and decrease in the number of cells (Fig. 5), before and after HIFU sonication. Significant changes were most observed in cells treated with HIFU sonication in the presence of microbubbles and TiO2 (R-P-TS). Figure 6 a shows a representative image of cells with severely damaged cell membrane. The absolute number of remaining fragments that had any cell-like structure was least observed in the microbubbles + TiO2 (R-P-TS) group. There were some giant blebs obviously induced immediately after the ultrasound treatment (Fig. 6b). There were brownish-tinted particles believed to be TiO2 on the cell membrane. Cells in the presence of TiO2 (R-A-TS) were at a glance morphologically intact, and few blebs were observed (Fig. 6c).
a Significant numbers of blebbing cell membrane in ultrasound treated group in the presence of microbubble and peroxo titania-silica-type TiO2. b Giant blebbing of cancer cells immediately after ultrasound treatment in the presence of microbubble and peroxo titania-silica-type TiO2. c Images of intact cell cancer cells treated with ultrasound and anatase titania-silica-type TiO2. Notice the brown particles on cell membrane which shows possible TiO2 nanoparticles
Discussion
We investigated the immediate effects of cell killing by a combination of short pulsed duration HIFU sonication with TiO2 and microbubbles in oral squamous cell carcinoma cells (HSC-2) in vitro. The effect of cell killing was more enhanced by the combination of HIFU sonication, TiO2, and microbubbles compared to cells treated without TiO2. These novel findings suggested that TiO2 enhanced the mechanical disruption of cells by ultrasound-induced microbubble collapse.
Titanium dioxide is widely used as a photocatalyst for industrial and medical applications, such as disposal of wastewater [8] and sterilization of bacteria, due to its useful physical and biological properties [9, 10]. It is well known that photo-induced electrons and holes can be generated on the TiO2 surface under exposure to UV light [11, 12]. These excited electrons and holes have strong reduction and oxidation activities that could further react with hydroxyl ions or water. This results in the formation of various reactive oxygen species (ROS), which have been shown to significantly damage cancer cells [13, 14].
While the cytotoxic effects of TiO2 nanoparticles have been under intense investigation, the molecular mechanisms of this cytotoxicity remain unknown [15]. Shimizu et al. [13] have suggested that various reactive oxygen species (ROS) including not less than singlet state molecular oxygen (1O2) and hydroxyl radicals (·OH) can be generated when nano-sized TiO2 powder is irradiated by US. As it has been demonstrated that the presence of TiO2 accelerates the generation of OH radicals in an ultrasonic bath, it is likely that the same phenomenon occurred with the excitation of TiO2 in our experimental setup during HIFU irradiation of oral squamous cell carcinoma cells. We did not conduct experiments to confirm the relationship between increased ROS generation and the degree of cell-killing enhancement. However, the cell destruction rate doubled or tripled only when TiO2 was added during HIFU irradiation, which suggests some kind of effect induced by this particular material. Furthermore, R-P-TS, which includes more hydrogen peroxide than R-A-TS solution, resulted in significantly more cell damage, indirectly suggesting ROS generation involvement. But as to why TiO2 enhanced the mechanical disruption of cells remains to be evaluated in future experiments.
RINKOH technology, which we used to stabilize TiO2, may have contributed to the enhancement of killing cancer cells by microbubbles. As this technology is used for sterilization, deodorization, dirt prevention, decomposition of toxic materials, air quality control, water quality control, and mist prevention of mirrors and elsewhere, a titania-silica aqueous solution of this kind may affect the environment around the cell membrane, which could lower the cavitation threshold. It is a special photocatalyst prepared by coupling of titanium oxide and silicon oxide with hydrogen peroxide. With the conventional technology, if a solution containing anatase titania is left to stand for a long time, the titania may be aggregated in the solution so that a high dispersion state of titania cannot be maintained. This problem was overcome in the present experiment, thus increasing damage to the cell membrane. The cytotoxicity results obtained in our experiments, especially in TiO2 (R-P-TS) containing hydrogen peroxide, suggest a relationship based on the above view. Considering the optical observation results of our study, the cell membrane might have become susceptible to peroxide in TiO2 (R-P-TS), resulting in increased damage to cells and induction of cell blebbing.
Our findings provide a rational basis for possible development of an effective TiO2 nanoparticle activation method by HIFU sonication, especially in the presence of microbubbles. This is the first report demonstrating the combination of TiO2 and microbubbles for the treatment of cancer cells in vitro. This technique may offer a new a noninvasive therapy for localized oral cancers in the near future.
References
Ogino C, Shibata N, Sasaki R, et al. Construction of protein-modified TiO2 nanoparticles for use with ultrasound irradiation in a novel cell injuring method. Bioorg Med Chem Lett. 2010;20:5320–5.
Harada Y, Ogawa K, Irei Y, et al. Ultrasound activation of TiO2 in melanoma tumors. J Control Release. 2011;149:190–5.
Tachibana K, Tachibana S. Albumin microbubble echo-contrast material as an enhancer for ultrasound accelerated thrombolysis. Circulation. 1995;92:1148–50.
Ohl CD, Arora M, Ikink R, et al. Sonoporation from jetting cavitation bubbles. Biophys J. 2006;91:4285–95.
Abe N, Nakamoto H, Suzuki T, et al. Ex vivo evaluation of high-intensity focused ultrasound with ultrasonic-induced cavitation bubbles. J Med Ultrasonics. 2014;41:3–9.
Wu J. Shear stress in cells generated by ultrasound. Prog Biophys Mol Biol. 2007;93:363–73.
Nejad SM, Hosseini SHR, Akiyama H, et al. Optical observation of cell sonoporation with low intensity ultrasound. Biochem Biophys Res Commun. 2011;413:218–23.
Esquivel K, Arriaga L, Rodríguez F, et al. Development of a TiO2 modified optical fiber electrode and its incorporation into a photoelectrochemical reactor for wastewater treatment. Water Res. 2009;43:3593–603.
Tsuang YH, Wu J, Zhang Z, et al. Studies of photokilling of bacteria using titanium dioxide nanoparticles. Artif Organs. 2008;32:167–74.
Cheng CL, Sun D, Chu W, et al. The effects of the bacterial interaction with visible-light responsive titania photocatalyst on the bactericidal performance. J Biomed Sci. 2009;16:7.
Zubkov T, Stahl D, Thompson TL, et al. Ultraviolet light-induced hydrophilicity effect on TiO2(110)(1 × 1). Dominant role of the photooxidation of adsorbed hydrocarbons causing wetting by water droplets. J Phys Chem B. 2005;109:15454–62.
Wang J, Go Y, Liu B, et al. Detection and analysis of reactive oxygen species (ROS) generated by nano-sized TiO2 powder under ultrasonic irradiation and application in sonocatalytic degradation of organic dyes. Ultrason Sonochem. 2011;18:177–83.
Shimizu N, Ogino C, Derider MF, et al. Sonocatalytic facilitation of hydroxyl radical generation in the presence of TiO2. Ultrason Sonochem. 2008;15:988–94.
Chihara Y, Fujimoto K, Konod M, et al. Anti-tumor effects of liposome-encapsulated titanium dioxide in nude mice. Pathobiology. 2007;740:353–8.
Zhu YL, Eaton JW, Li C. Titanium Dioxide (TiO2) nanoparticles preferentially induce cell death in transformed cells in a Bak/Bax-independent fashion. PLoS One. 2012;7:e50607.
Acknowledgments
This study was supported in part by the Japanese Society of Ultrasound in Medicine 2013 Research Grant.
Conflict of interest
Katsuro Tachibana, Hitomi Endo, Loreto Feril, Seyedeh Moosavi Nejad, Hiromasa Takahashi, Kyoichi Narihira, and Toshihiro Kikuta all declare that they have no conflict of interest.
Ethical standard
This article does not contain any experiments with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Tachibana, K., Endo, H., Feril, L.B. et al. Enhanced mechanical damage to in vitro cancer cells by high-intensity-focused ultrasound in the presence of microbubbles and titanium dioxide. J Med Ultrasonics 42, 449–455 (2015). https://doi.org/10.1007/s10396-015-0626-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10396-015-0626-4