Abstract
Aim
The objective of this study was to determine risk factors for non-communicable diseases (NCDs) on the basis of socio-demographic characteristics, lifestyle-related determinants, environmental and psychological characteristics, and individual and family disease history among university students in Bangladesh.
Study design
Cross-sectional survey.
Methods
Using the WHO STEPwise approach for NCDs, a cross-sectional study was conducted among 1,140 students. The collected data were analyzed using the Statistical Package for Social Sciences (SPSS) software, version 22.
Results
In all, 29.2% of the respondents (BMI ≥ 23.00 kg/m2) were overweight and/or obese, and almost two-thirds (65%) of them did not take part in any physical activity (PA). A third (33.3%, p = 0.002) of male smokers reported health problems and it was found that environmental tobacco smoke (ETS) was significantly responsible for developing asthma (OR = 0.55; CI = 0.33–0.93). Individual and family history of NCDs was statistically significant for obesity and asthma and considerably increased the odds ratio for heart disease.
Conclusion
This study shows that the number of students suffering from different types of NCDs is not negligible. Their lifestyle and family history of NCDs are responsible for this to a significant extent. Urgent initiatives should be taken to rein in the spread of NCDs among the youth of Bangladesh.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
The prevalence rate of non-communicable diseases (NCDs)–diseases that are not transmitted from person to person, and are of long duration and slow progression (WHO 2017)–is increasing day by day among the youth of Bangladesh, one of the developing countries of the Southeast Asian region. Consequently, the mortality rate from NCDs is rising steadily, both among adults and the young. NCDs are certain types of diseases that are mostly related to risk factors of which four prominent ones are tobacco use, unhealthy diet, physical inactivity and harmful use of alcohol (WHO 2011). These lead to other risk factors that in turn engender more NCDs such as hypertension, hyperglycemia, hyperlipidemia, obesity, poor nutrition, etc. (Go et al. 2014; Nichols et al. 2014; WHO 2013a). Around the world, the increasing trend of NCDs has taken a heavy toll on lives, and it is estimated that deaths from NCDs will rise to 49.7 million by 2020. In 2017, the WHO stated that these NCDs were responsible for 40 million deaths annually, of which almost three quarters (31 million) occurred in low- and middle-income countries (WHO 2017). It also stated that the current mortality percentage per year of NCDs around the world is 70%. The global cost for NCDs was estimated at US $6.3 trillion in 2010, and it is anticipated that this will increase to US $13 trillion by the year 2030 (Atun et al. 2013).
The world is now going ahead with the mission of implementing sustainable development goals (SDGs). The aim of goal 3.4 is to reduce premature mortality from NCDs by one third by the year 2030 (WHO 2015). Therefore, like the rest of the world, we have to put suitable emphasis on NCDs and conscientize people about the colossal detriment they cause to human health because adequate awareness about the issue can play a pivotal role in fighting off the epidemic hazard. This study was conducted among first year university students in order to examine their current health status, lifestyle, family history of diseases, and dietary habits, and to find out the prevalence of risk factors among them and their probability of developing NCDs.
First-year university students are the people who step out of their home into a new environment for education, which is why they go through a nutritional transition. Moreover, they develop the harmful habits of smoking, drinking alcohol, sedentary lifestyle and unhealthy diet during this period, habits which can become permanent as they develop into mature adults. Studies show that in both developing and developed countries university students have poor dietary habits with a low intake of milk, fruit, vegetables, etc. and a high intake of food items rich in fats and carbohydrates (Freedman et al. 1999; Tassitano et al. 2014). For these reasons, it is important to investigate the lifestyle and current health status of these young adults along with their family history of diseases because the roots of many NCDs in adulthood lie in this earlier behavior and lifestyle (Hanan Abo-Elgamelen Ebrahim Essa and El-Shemy 2015).
Methods
Study area and population
This cross-sectional study, which is descriptive in nature, was carried out among the students of Jahangirnagar University, Dhaka, the only fully residential public university in Bangladesh, between April 10, 2016 and July 28, 2016 (Figure 1). The target population was all the first year students of the university, their total number being about 2,060. Assuming a 2% margin of error, data were collected from 1,140 students.
Measurements
In this study, we followed the WHO STEPwise approach to surveillance (STEPS) of NCD risk factors (WHO 2016a). The total data collection period was divided into two phases. The first phase comprised face-to-face interviews to gather information on socio-demographic characteristics, lifestyle, and individual and family disease history. Following the WHO guidelines, a questionnaire consisting of both open and closed-ended questions was developed prior to the study and used during the interviews. In the second phase, physical measurements were taken from the same subjects. To ensure the data collection quality, standardized protocols were used, and data collectors were provided with proper training before the study. In order to maximize the quality, the filled-out questionnaires were checked immediately after data collection by the quality controllers.
Socio-demographics
Socio-demographic data were collected from all the participants, including their age, gender, ethnicity, study faculty, birth order, family members, parents’ occupation, person bearing educational expenses, and monthly expenditure.
Lifestyle factors
The participants were asked whether they currently smoked cigarettes, were exposed to environmental tobacco smoke, and whether they suffered health problems due to smoke or not. As to physical exercise, they were asked whether they took any physical activity: moderate exercise (walking or meditation/yoga ≥30 min/day), vigorous exercise (jogging, cycling, playing sports or gym workouts ≥60 min/day) or inactivity (occasional or no physical exercise). Students were asked whether they watched movies and spent time on the Internet using social media like Facebook or not. Patterns of watching movies or Internet use were categorized on the basis of hours per day, week and month. To find the risk association of NCDs with dietary patterns, this study focused on the frequency and place of daily meal consumption. The students were asked how many times they ate in a day (e.g. twice, three times, four times or more than four times) and where they took their meals. The questionnaire addressed six places where students usually took their meals such as dining hall, canteen, home, outside (any place off-campus or on-campus other than dining hall, canteen or home), outside and dining hall/canteen, and finally, outside and home.
Individual and family disease history
The participants were asked separate questions for every single chronic condition (physical weakness, asthma, hypertension, heart disease, diabetes, cancer, insomnia, stress/depression and neural disorders) to record whether they had suffered or still suffer from these conditions. Information up to the second degree relationship was collected with regard to family diseases. Both mortality and morbidity data about the NCDs were collected.
Anthropometrics
The ZZJKH-01 weight and height scale was used to measure the weight and height of the participants. Weight was measured in kg and height in cm. At the time of measurement, the students wore light clothing, and their shoes were removed. Body mass index (BMI) was calculated as weight in kg/height in m2. The BMI cut-off points used in this study were BMI < 18.50 kg/m2 for underweight, BMI 18.50 kg/m2–22.99 kg/m2 for normal body weight, BMI 23.00 kg/m2–24.99 kg/m2 for overweight, and BMI ≥ 25 kg/m2 for obese (Jafar et al. 2006; Siddiquee et al. 2015).
Statistical analysis
Descriptive statistics of categorical variables included frequency distribution, proportions, and measuring of central value, and mean and standard deviation were used for the dispersion of the data set. To identify significant relationships between the variables, test statistics such as the Chi-square test, Fisher’s exact test, and t-test were used where appropriate. Variables that were predicted to be associated with NCDs were further analyzed using logistic regression models. All data were analyzed using the Statistical Package for the Social Sciences (SPSS) software for Windows, version 22.0.
Results
Prevalence of overweight/obesity
Rates for underweight, normal weight, overweight and obese were 21.1, 49.7, 14.7 and 14.5% respectively (Table 1). What is alarming is that nearly one third of the study population had a BMI over 23.00 kg/m2, which falls into either the overweight or obese category.
Prevalence of cigarette smoking and exposure to ETS
In this study, 12.9% (147) of all participants—22.0% (146) males and 0.2% (1) females—indulged in smoking (Table 1), while 44.9% (512) of students—63.6% (422) males and 18.9% (90) females—reported being exposed to ETS, with a p-value of <0.001, which is significant. The study showed that 53.5% (610) students—55.1% (366) males and 51.3% (244) females—reported smokers within their family. In this study, the mean age of initiation of smoking was approximately 16 years and the mean continuing period thereafter was 3 (±1.8; Table 2), from which it follows that the smoker students started smoking when they were either at school (class 1–10) or college (class 11–12). The average daily number of cigarettes consumed was 7 for males and 5 for females.
Physical activity
In this study, almost 65% of students were physically inactive. Female students (77%) were more inactive than males (56.5%). This meant that only 1 in every 5 females and 2 in every 5 males took part in some form of physical exercise (Table 1). The difference between male and female students was statistically highly significant (p = 0.001). Of the different types of physical exercise, walking was the most common one, as reported by 19.6% (224) of students—21.4% (142) males and 17.2% (82) females.
Screen-based sedentary behaviors (SBSB)
SBSB like watching movies, playing games on computers and cell phones, as well as spending time on Facebook were found among almost 90% of the participants from both sexes, for more than 16% (17.3% males and 15% females) on a regular basis. The logistic regression analysis showed that students who were involved in daily movie watching had twice the chance (95% CI: 1.36–3.15) of developing overweight/obesity in their lifetime, which is statistically highly significant (p < 0.05; Table 3). It was also found that there were significant differences between male and female participants: the weekly and monthly average time in hours spent watching movies or other SBSB were 6.48 (±8.39) and 28.52 (±34.38) for males, and 5.35 (±8.73) and 24.61 (±37.25) for females (Table 2).
Dietary pattern
The study reported that 12% of the participants consumed food twice a day, whereby generally the morning meal (breakfast) was not taken regularly; 2% of them consumed food more than four times per day; the remaining 65 and 21% of students consumed food three times and four times a day respectively (Table 1). It was also revealed that male students had a higher tendency to take food from outside of the residence than female ones, which is statistically significant (p < 0.001).
Mental health
This study revealed a desolate picture of the mental health state of the participants, as presented in Table 1. More than 69%, both male and female, reported that they had mental stress. Reasons behind the mental stress and illness among the students included study and career-related (29.8%), university culture-related (17.8%), psychological (12.7%), family (5.2%) and financial (3.3%) ones.
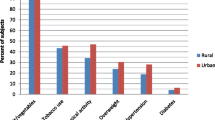
Family morbidity and mortality of NCDs
Of the respondents, a total of 77.5% (883)—74.5% (495) males and 81.5% (338) females—reported NCD patients in their family, with a significant p-value of 0.006 (Table 4). Diabetes was the most prevalent (46.5%) of the top five NCDs, followed by hypertension (37.2%), heart disease (26.3%), asthma (7.2%) and cancer (4.9%).
In the case of NCD mortality, cancer was the most fatal disease (Fig. 2) followed by stroke, heart disease, diabetes, and asthma as the most prevalent causes of mortality among student family members. Other causes of mortality included kidney disease, hypertension and tuberculosis. The results showed that females were more vulnerable to cancer than males, and that the fatality rate of cancer was higher among females than males. As shown in Figure 2, the mortality rates of the respondents’ fathers, mothers, paternal grandfathers, paternal grandmothers, maternal grandfathers, maternal grandmothers, uncles and aunts due to cancer were 21.82, 60, 33.08, 31.87, 32.91, 38, 21.67 and 63.16% respectively. On the other hand, males were more vulnerable to heart disease than females. The rates of mortality due to heart disease were 38.18% for the respondents’ fathers, 10% for their mothers, 22.56% for their paternal grandfathers, 12.1% for their paternal grandmothers, 17.72% for their maternal grandfathers, 14% for their maternal grandmothers, 35% for their uncles and 5.26% for their aunts.
Discussion
The prevalence of overweight/obesity in this study justifies the WHO projection about overweight/obesity of the world population (WHO 2013b). The percentage documented in this study was higher than earlier studies among university students of Bangladesh (Peltzer et al. 2014). Logistic regression analysis in our study showed that overweight/obesity is the fundamental risk factor for developing NCDs in future since almost all other variables were associated with it. For the South Asian region, studies have proved that a high prevalence of obesity was positively related to gender, middle age, higher educational and economic status, physical inactivity and some dietary habits (Jayawardena et al. 2013). In our study, all these variables were also found to be statistically significant for the development of overweight/obesity.
University students are at a high risk of smoking as they are exposed to a greater availability of cigarettes and close association with smoking peers. At the same time, they face additional social, emotional and educational challenges when they enter university (Hossain et al. 2017). A recent study revealed that the prevalence of tobacco smoking among the students of Jahangirnagar University in 2015 was 60.2%, with males smoking at a higher rate than females (68.81 and 19.56% respectively; Hossain et al. 2017). Another study based on demographic and health survey data reported that the prevalence of tobacco smoking among men in Bangladesh was 60% (Sreeramareddy et al. 2014). Although the findings of the present study differ somewhat from the existing smoking-related literature in Bangladesh, they still do not indicate that the rate of cigarette smoking in the country has declined significantly. On the contrary, it is still very high from a public health point of view and comparable with several similar studies from around the world (Babatunde et al. 2012; Deressa and Azazh 2011). As the study subjects were the newly enrolled first year university students, there might be greater chances that the rate of cigarette smoking among them will increase if health interventions are not taken. Again, the results of yet another study revealed that university students are at a high risk of smoking because of the initiating factors of cigarette use (Hossain et al. 2017).
For NCDs, physical inactivity is considered an independent risk factor and one of the ten leading risk factors for global mortality and morbidity which may cause obesity, hypertension, diabetes, coronary heart disease, and breast and colon cancer (WHO 2016b). The results of the current study show considerable similarities with those of other comparable studies among adults and university students in different geographic locations (Peltzer et al. 2014; WHO 2016b). In this study, a significant link between overweight/obesity and physical inactivity was found. A number of studies conducted on dietary patterns both in the developed and developing countries have shown that dietary behaviors of university students are poor, with a low intake of milk, fruit and vegetables, and a high intake of food with excessive fats and carbohydrates (Martinez Alvarez et al. 2015; Pullman et al. 2009). Another study revealed that unhealthy dietary habits, characterized by skipping meals, low consumption of healthy food and high intake of energy and sugar-rich food were prevalent among a relatively large proportion of university students in Bangladesh (Karmakar et al. 2016), which is in agreement with this study.
Mental health is one of the vital parameters for a happy, healthy and productive life; however, mental stress/disorder does not receive enough attention and is not adequately addressed as a public health issue in countries like Bangladesh (WHO 2016c). The findings of this study reported widespread (69.3%) mental stress among university students in Bangladesh, a rate which was much higher than the prevalence in the general adult population (aged 18 years or older) in Bangladesh, which ranges from 6.5 to 31% (Hossain et al. 2014). The occurrence of mental stress (69.3%) in the current study was 4.3 times higher than that (16.1%) found among Bangladeshi adults in 2005 (WHO 2016c); further, the prevalence of mental stress among the Bangladeshi university students, as reported in the current study, was 1.3 times higher than that (54%) among medical (MBBS Year III and IV) students in Bangladesh (Eva et al. 2015). Among the reasons for mental stress reported in the current study, university culture-related and family causes could be especially significant because they have since emerged as new risk factors exacerbating mental pressure and disorders. Previous studies have shown that poor language skills (Kim et al. 2011), financial hardship (Cuthbertson et al. 2004), insomnia (Kaneita et al. 2009), drinking and tobacco use (Beck et al. 2008), and physical inactivity and living conditions (Kono et al. 2015) are well-established factors for determining mental health, which is similar to the findings of the current study.
An association between a family history of NCDs and their existence in the offspring generation has been well established by many studies among different populations. This study also confirmed a significant relationship between students’ obesity and a family history of NCDs, specifically hypertension, diabetes and cancer. It can be seen from the multiple logistic regression analysis that the risk of developing obesity among students with a positive family history of NCDs is almost twice as high as among those with no positive family history of NCDs, and that it was statistically significant. Similarly, the risk ratio was 1.68 (95% CI: 1.27–2.22), 1.58 (95% CI: 1.21–2.08), and 1.84 (95% CI: 1.00–3.40) for hypertension, diabetes and cancer respectively. All of these risks were statistically significant. Our results were, to some extent at least, similar to those of other studies (Van der Sande et al. 2001). In the case of asthma, family histories of asthma and cancer were significantly associated (p < 0.05) with the students’ asthma: the risk ratio was 0.31 (95% CI: 0.15–0.62) for students with a family history of asthma, and 0.43 (95% CI: 0.17–1.07) for those with a family history of cancer. Along with some other risk factors like the environmental one, these results modestly agree with those of previous studies conducted to find out the association between parental and offspring asthma (Bjerg et al. 2007; Paaso et al. 2013). In the case of heart disease, although no significant association with family history was reported in this study because of the fewer positive cases of heart disease among students, the logistic model showed that all family histories of NCDs have a positive impact on it. Findings from previous studies suggest that common behavioral determinants and environmental and genetic factors intensify the risk of developing cardiovascular disease among the progeny (Chen et al. 2001; Khoury et al. 2016). All these evidences serve to accentuate the risks of NCDs among the participants of this study.
Limitations of this study
This study has some limitations. One of them is that biochemical assessment of the study subjects was not possible due to insufficient funding. Again, as it was a cross-sectional observation study, establishment of strong causal relationships between various risk factors was not possible, and identified risk factors could not be causally associated with NCDs. Another limitation of this study was self-reported information, which always involves the risk of recall bias. In addition, data relating to family NCD histories was only gathered from the respondents, not from their family members directly; therefore, the results of the study might need to be interpreted with caution.
Conclusions and implications of the findings
To the best of our knowledge, no single study has been conducted in Bangladesh highlighting all the risk factors associated with NCDs among university students. This is the first initiative in Bangladesh to draw a model of multiple risk factors for the causation of NCDs among students. It is of great concern that in recent times, not only the adults, but also the young people of Bangladesh are suffering and even dying from NCDs. As this study reveals, the numbers of young people suffering from different types of NCDs in Bangladesh are not negligible, and the factors responsible for this include family history of NCDs as well as their lifestyle choices, such as physical inactivity, a diet rich in saturated and trans fatty foods, eating less fruit and vegetables, having meals outside of home, smoking, etc. This study provides baseline information to start a discussion about NCDs risks, which could contribute to creating awareness among all the university students of the country, as well as drawing the attention of the country’s public health leaders and policy makers to the issue. Evidence-based health programs and policies should be undertaken for addressing the university students’ health hazards on the basis of the findings of this study so that they can lead an active, healthy and productive life, which will contribute to the country’s sustainable development in the long term. Therefore, the authorities concerned should, without any further delay, embark on programs for consciousness-raising about the detrimental impact of the ever-escalating burden of NCDs on the population in general, and young university students in particular. To conclude, we would like to put forward the following recommendations for mitigating the risks and adverse effects of NCDs among the university population in Bangladesh: (1) the first-year university students need to be conscientized about the causal and impact factors of NCDs because they are more vulnerable to adopting bad habits under the influence of environmental and peer pressure; (2) students should be encouraged to get involved in more physical activities such as exercises and outdoor games that require body movement instead of playing video games on the computer, for example; (3) students should be encouraged to abstain from consuming food items rich in saturated and trans fats as well as to eat those rich in fiber, such as fruits and vegetables; (4) students should be provided with regular counseling so as to enable them to get help with mental disorders like depression, stress, etc. that leads them to cultivate bad habits; (5) a smoking-free campus should be ensured, and students should be discouraged from consuming all tobacco products; and finally, (6) students with a family history of NCDs should be conscientised about the risk factors as well as the detrimental impact of NCDs on human health from the very beginning.
References
Atun R, Jaffar S, Nishtar S, Knaul FM, Barreto ML, Nyirenda M, Banatvala N, Piot P (2013) Improving responsiveness of health systems to non-communicable diseases. Lancet 381(9867):690–697. https://doi.org/10.1016/s0140-6736(13)60063-x
Babatunde OA, Elegbede OE, Ayodele LM, Atoyebi OA, Ibirongbe DO (2012) Cigarette smoking practices and its determinants among university students in southwest Nigeria. J Asian Sci Res 2(2):62–69
Beck KH, Arria AM, Caldeira KM, Vincent KB, O'Grady KE, Wish ED (2008) Social context of drinking and alcohol problems among college students. Am J Health Beh 32(4):420–430. https://doi.org/10.5555/ajhb.2008.32.4.420
Bjerg A, Hedman L, Perzanowski MS, Platts-Mills T, Lundback B, Ronmark E (2007) Family history of asthma and atopy: in-depth analyses of the impact on asthma and wheeze in 7- to 8-year-old children. Pediatrics 120(4):741–748. https://doi.org/10.1542/peds.2006-3742
Chen W, Srinivasan SR, Bao W, Berenson GS (2001) The magnitude of familial associations of cardiovascular risk factor variables between parents and offspring are influenced by age. Ann Epidemiol 11(8):522–528. https://doi.org/10.1016/s1047-2797(01)00228-9
Cuthbertson P, Lauder W, Steele R, Cleary S, Bradshaw J (2004) A comparative study of the course-related family and financial problems of mature nursing students in Scotland and Australia. Nurse Educ Today 24(5):373–381. https://doi.org/10.1016/j.nedt.2004.03.005
Deressa W, Azazh A (2011) Substance use and its predictors among undergraduate medical students of Addis Ababa University in Ethiopia. BMC Public Health 11:660. https://doi.org/10.1186/1471-2458-11-660
Eva EO, Islam MZ, Mosaddek ASM, Rahman MF, Rozario RJ, Iftekhar AFMH, Ahmed TS, Jahan I, Abubakar AR, Dali WPEW, Razzaque MS, Habib RB, Haque M (2015) Prevalence of stress among medical students: a comparative study between public and private medical schools in Bangladesh. BMC Res Notes 8:327. https://doi.org/10.1186/s13104-015-1295-5
Freedman DS, Dietz WH, Srinivasan SR, Berenson GS (1999) The relation of overweight to cardiovascular risk factors among children and adolescents: the Bogalusa heart study. Pediatrics 103:1175–1182
Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Judd SE, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Mackey RH, Magid DJ, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler ER, Moy CS, Mussolino ME, Neumar RW, Nichol G, Pandey DK, Paynter NP, Reeves MJ, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Wong ND, Woo D, Turner MB (2014) Executive summary: heart disease and stroke statistics-2014 update—a report from the American Heart Association. Circulation 129(3):e28–e292. https://doi.org/10.1161/01.cir.0000441139.02102.80
Hanan Abo-Elgamelen Ebrahim E, El-Shemy MBA (2015) Prevalence of lifestyle associated risk factors for non-communicable diseases and its effect on quality of life among nursing students, Faculty of Nursing, Tanta University. Int J Adv Res 3(5):429–446
Hossain MD, Ahmed HU, Chowdhury WA, Niessen LW, Alam DS (2014) Mental disorders in Bangladesh: a systematic review. BMC Psychiatry 14:216. https://doi.org/10.1186/s12888-014-0216-9
Hossain S, Hossain S, Ahmed F, Islam R, Sikder T, Rahman A (2017) Prevalence of tobacco smoking and factors associated with the initiation of smoking among university students in Dhaka, Bangladesh. Central Asian J Global Health 6(1):244. https://doi.org/10.5195/cajgh.2017.244
Jafar TH, Chaturvedi N, Pappas G (2006) Prevalence of overweight and obesity and their association with hypertension and diabetes mellitus in an Indo-Asian population. Can Med Assoc J 175(9):1071–1077. https://doi.org/10.1503/cmaj.060464
Jayawardena R, Byrne NM, Soares MJ, Katulanda P, Hills AP (2013) Prevalence, trends and associated socio-economic factors of obesity in South Asia. Obes Facts 6(5):405–414. https://doi.org/10.1159/000355598
Kaneita Y, Yokoyama E, Harano S, Tamaki T, Suzuki H, Munezawa T, Nakajima H, Asai T, Ohida T (2009) Associations between sleep disturbance and mental health status: a longitudinal study of Japanese junior high school students. Sleep Med 10(7):780–786. https://doi.org/10.1016/j.sleep.2008.06.014
Karmakar P, Jahan N, Banik S, Das A, Rahman K, Kundu S, Sattar M (2016) Food habits, obesity and nutritional knowledge among the university students in Noakhali region of Bangladesh: a cross-sectional study. J Food Nutr Dis 5(4). https://doi.org/10.4172/2324-9323.1000201
Khoury M, Manlhiot C, Gibson D, Chahal N, Stearne K, Dobbin S, McCrindle BW (2016) Universal screening for cardiovascular disease risk factors in adolescents to identify high-risk families: a population-based cross-sectional study. BMC Pediatr 16:11. https://doi.org/10.1186/s12887-016-0548-3
Kim G, Aguado Loi CX, Chiriboga DA, Jang Y, Parmelee P, Allen RS (2011) Limited english proficiency as a barrier to mental health service use: a study of Latino and Asian immigrants with psychiatric disorders. J Psychiatr Res 45(1):104–110. https://doi.org/10.1016/j.jpsychires.2010.04.031
Kono K, Eskandarieh S, Obayashi Y, Arai A, Tamashiro H (2015) Mental health and its associated variables among international students at a Japanese university: with special reference to their financial status. J Immigr Minor Health 17(6):1654–1659. https://doi.org/10.1007/s10903-014-0100-1
Martinez Alvarez JR, Garcia Alcon R, Villarino Marin A, Marrodan Serrano MD, Serrano Morago L (2015) Eating habits and preferences among the student population of the Complutense University of Madrid. Public Health Nutr 18(14):2654–2659. https://doi.org/10.1017/S1368980015000026
Nichols M, Townsend N, Scarborough P, Rayner M (2014) Cardiovascular disease in Europe 2014: epidemiological update. Eur Heart J 35(42):2950–2959. https://doi.org/10.1093/eurheartj/ehu299
Paaso EM, Jaakkola MS, Lajunen TK, Hugg TT, Jaakkola JJ (2013) The importance of family history in asthma during the first 27 years of life. Am J Respir Crit Care Med 188(5):624–626. https://doi.org/10.1164/rccm.201212-2236LE
Peltzer K, Pengpid S, Samuels TA, Ozcan NK, Mantilla C, Rahamefy OH, Wong ML, Gasparishvili A (2014) Prevalence of overweight/obesity and its associated factors among university students from 22 countries. Int J Environ Res Public Health 11(7):7425–7441. https://doi.org/10.3390/ijerph110707425
Pullman AW, Masters RC, Zalot LC, Carde LE, Saraiva MM, Dam YY, Randall Simpson JA, Duncan AM (2009) Effect of the transition from high school to university on anthropometric and lifestyle variables in males. Appl Physiol Nutr Metab 34(2):162–171. https://doi.org/10.1139/H09-007
Siddiquee T, Bhowmik B, Da Vale Moreira NC, Mujumder A, Mahtab H, Khan AK, Hussain A (2015) Prevalence of obesity in a rural Asian Indian (Bangladeshi) population and its determinants. BMC Public Health 15:860. https://doi.org/10.1186/s12889-015-2193-4
Sreeramareddy CT, Pradhan PM, Mir IA, Sin S (2014) Smoking and smokeless tobacco use in nine south and southeast Asian countries: prevalence estimates and social determinants from demographic and health surveys. Popul Health Metrics 12:22. https://doi.org/10.1186/s12963-014-0022-0
Tassitano RM, Dumith SC, Chica DAG, Tenório MCM (2014) Aggregation of the four main risk factors to non-communicable diseases among adolescents. Rev Bras Epidemiol 17(2):465–478
Van der Sande MA, Walraven GE, Milligan PJ, Banya WA, Ceesay SM, Nyan OA, McAdam KP (2001) Family history: an opportunity for early interventions and improved control of hypertension, obesity and diabetes. Bull World Health Organ 79(4):321–328
WHO (2011) WHO global status report on non-communicable diseases 2010: description of the global burden of NCDs: their risk factors and determinants. WHO, Geneva. http://apps.who.int/iris/bitstream/10665/44579/1/9789240686458_eng.pdf. Accessed 24 Mar 2016
WHO (2013a) WHO global action plan for the prevention and control of non-communicable diseases: 2013–2020. WHO, Geneva. http://www.who.int/global-coordination-mechanism/publications/global-actionplan-ncds-eng.pdf. Accessed 8 Apr 2017
WHO (2013b) What are the health consequences of being overweight? WHO, Geneva. http://www.who.int/features/qa/49/en/. Accessed 23 Apr 2017
WHO (2015) WHO report on UN Sustainable Development Summit 2015: health-related SDGs targets. WHO, Geneva. http://www.who.int/mediacentre/events/meetings/2015/un-sustainable-development-summit/en/. Accessed 8 Apr 2017
WHO (2016a) WHO STEPwise approach to surveillance (STEPS). WHO, Geneva. http://www.who.int/chp/steps/en/. Accessed 24 Mar 2016
WHO (2016b) Global Health Observatory (GHO) data: prevalence of insufficient physical activity. WHO, Geneva. http://who.int/gho/ncd/risk_factors/physical_activity_text/en/. Accessed 30 Mar 2016
WHO (2016c) Mental health and substance abuse. WHO, Geneva. http://www.searo.who.int/bangladesh/areas/substanceabuse/en/. Accessed 3 Apr 2016
WHO (2017) WHO fact sheet on non-communicable diseases. WHO, Geneva. http://www.who.int/mediacentre/factsheets/fs355/en/. Accessed 4 Aug 2017
Funding
This study was financially supported by the Research Grant Program 2016 of the Jahangirnagar University Science Club (JUSC), Savar, Dhaka-1342, Bangladesh.
Author information
Authors and Affiliations
Contributions
S.H. conceived the study, was responsible for the implementation, analysis and interpretation of data and wrote the manuscript. M.S.H. supervised the study and critically revised the manuscript. A.A. and F.A. contributed to the implementation of the study, data processing and manuscript development. M.F.H. critically reviewed the statistical analysis section of the paper. M.E.U. critically reviewed and edited the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was conducted while maintaining ethical standards to the highest possible extent. The research proposal was approved by the Department of Public Health and Informatics, Jahangirnagar University, Bangladesh. International ethical guidelines for biomedical research involving human subjects were followed throughout the study. All participants read, understood, and signed a written consent form. The ethical clearance for data collection was given by the respective faculty and department heads.
Rights and permissions
About this article
Cite this article
Hossain, S., Hossain, M.S., Anjum, A. et al. Risk modeling of non-communicable diseases using socio-demographic characteristics, lifestyle and family disease history among university students in Bangladesh. J Public Health (Berl.) 26, 531–543 (2018). https://doi.org/10.1007/s10389-018-0895-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10389-018-0895-7