Abstract
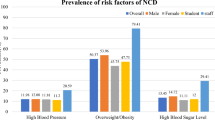
The objective of this study was to assess the prevalence of modifiable risk factors of the major non-communicable diseases (NCDs) among medical students. A cross sectional study was conducted at three randomly selected medical colleges in the Kathmandu Valley in Nepal. All third-year medical students (n = 191) participated in the study. A total of 62.3 % of the respondents were male, and 37.7 % were female. The mean age of the respondents was 21.5 ± 1.0 (SD) years. A total of 20.4 % (n = 39) of the medical students were current tobacco users and 50.8 % (n = 97) have ever consumed alcohol. The majority (85.6 %) of the medical students did not consume the daily recommended amount of fruits and vegetables. A total of 30.9 % (n = 59) of the medical students were involved in low level of physical activity and 42.9 % (n = 82) were involved in moderate level of physical activity. This study showed a high prevalence of risk factors of major NCDs among medical students and interventions are needed to change the unhealthy behaviour of medical students being role models in society.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Globally, non-communicable diseases (NCDs) are the leading cause of mortality accounting for more than 63 % of all deaths [1]. Nearly 55 % of deaths [2] and 44 % of the total burden of diseases in the South-East Asia Region (SEAR) are attributed to NCDs according to the World Health Organization (WHO) [3]. Of the estimated 14.5 million deaths in 2008 in this region, 7.9 million (55 %) were ascribed to NCDs and 34 % of deaths occurred before the age of 60 years [2]. Deaths caused by NCDs are expected to increase by 15 % between 2010 and 2020, and will be most pronounced in low and middle income countries (LMICs) compared to high income countries [1]. In Nepal, NCDs are already the leading cause of outpatient morbidity and mortality [4, 5].
The main contributors to the development of major NCDs are a small number of modifiable risk factors [1, 6, 7]. These modifiable factors include tobacco use, excessive alcohol intake, physical inactivity and an unhealthy diet; these factors are major causes of overweight and obesity, high blood pressure, high blood glucose and dyslipidemia, all important biological risk factors for NCDs [8]. Eliminating these risk factors prevent up to 80 % of heart disease, stroke and type 2 diabetes and more than a third of cancer cases [9].
Medical professionals, who are often viewed as role models in a community, can be crucial change agents to promote healthy behaviour with regard to NCD [10]. Thus, medical students who are future role models as intellectuals in the community should adopt healthy lifestyle practices [11]. Exposure to modifiable risk factors of the major NCDs not only negatively affect quality of life (QoL) in this group but may also lead to poor judgment and irresponsible behaviour and thus failure to render satisfactory health services. The objective of this study was to assess the prevalence of modifiable risk factors for the major NCDs among medical students in the Kathmandu Valley in Nepal. This study is a part of a bigger study exploring the prevalence of risk factors of major NCDs and associated factors among medical students in Nepal; gender differences in clustering of major risk factors have also been studied and results are published elsewhere [12].
Methodology
Study Design and Setting
This was a cross sectional study conducted among third-year medical students in the Kathmandu Valley of Nepal. The Kathmandu Valley comprises Kathmandu, Bhaktapur and Lalitpur districts covering an area of 220 km2 with approximately 2.5 million inhabitants [13, 14]. There are five medical colleges, two public and three private, in the valley, three in the Kathmandu district and two in the Lalitpur district [15]. There are approximately 3200 medical students in the Kathmandu Valley. Approximately a total of 650 medical students are enrolled annually.
Sample Size and Sampling Techniques
A simple random sampling technique was applied to select three medical colleges out of the five resulting in the selection of two private and one public medical college. All the third-year medical students (n = 191) from the selected colleges were invited to participate in the study. A detailed sampling procedure has been described elsewhere [12].
Data Collection
A modified self-administered anonymous questionnaire based on the WHO STEPS Instrument v2.1 was used for data collection [16]. The physical measurements required in step 2 and biochemical measurements required in step 3 of this instrument were not performed due to logistic limitations. Thus, the questionnaire included questions on demographic characteristics of the respondents, tobacco and alcohol consumption, level of physical activity, and fruit and vegetable intake. This questionnaire has been used previously in Nepal [17]. Data were collected during August 2013. One of the co-authors visited the medical colleges and was given permission from the college authorities to enter the classroom. The researcher explained the purpose of the study in detail and distributed the questionnaire to each consenting student. The questionnaire was filled in immediately in the classroom. To ensure confidentiality, the seating was arranged to ensure confidentiality of individual student responses. Only students who were present in class at the time of the visit by the researcher were eligible as respondents.
Defining Variables
Ethnicity was defined as Brahmin/Chhetri, Janajati, Madhesi and other ethnic background based on the classification used by the Central Bureau of Statistics of Nepal [14].
Standard guidelines for each of the modifiable NCD risk factors (smoking, excessive alcohol intake, physical inactivity and inadequate consumption of fruit and vegetables) were adopted from the WHO NCD Risk Factor STEPS 1 and 2 Questionnaires [16].
A person is at risk of NCDs if s/he is a daily tobacco user. Daily tobacco users were respondents who reported smoking cigarettes, bidi, kankat, or hukka using other forms of smokeless tobacco on a daily basis.
The limit for being at risk for alcohol intake was (1) males drinking 15 or more standard drinks a week and (2) women drinking 12 or more standard drinks a week [18]. The criterion for standard drinks of different alcoholic beverages is described elsewhere [17]. Alcohol users who had consumed at least one standard drink (e.g. beer, whiskey, vodka, rum, local alcohol or rakshi, thongba, wine etc.) in the past 30 days prior to the study were classified as current drinkers.
A person has a risk of NCDs if s/he has <600 metabolic equivalent of task (MET) minutes a week of physical activity. Physical activity was related to daily occupation. To determine the level of physical activity the WHO STEPS Survey Manual criteria were used [16]. MET minutes/week was calculated based on number of days and time spent on vigorous and/or moderate physical activities during work, transport, and recreational activities. Vigorous, moderate and low physical activity was recorded based on the criteria in the WHO STEPS Manual.
A person has a risk of NCDs if s/he has consumed less than five servings of fruits and vegetables per day. One serving of vegetables was defined as one cup of raw, leafy green vegetables (spinach, salad, etc.), half a cup of other cooked or raw vegetables (tomatoes, pumpkin, beans etc.) or half a cup of vegetable juice. One serving of fruit was defined as one medium-size piece of fruit (banana, apple, etc.), half of cup of raw, cooked or canned fruit, or half of cup of juice from a fruit (not artificially flavoured) [16, 19].
Data Analysis
We used EpiData 3.1 for data entry and Epi Info 3.5.4 for analysis. Descriptive findings were presented as frequencies and percentages.
Research Ethics
This study was approved by the Department of Community Medicine and Public Health, Institute of Medicine, Nepal. Written informed consent was obtained from all participants.
Results
Demographic Characteristics
In this study, 62.3 % (n = 119) of respondents were male and 37.7 % (n = 72) were female. Among respondents, 61.8 % (n = 118) were Brahmin/Chhetri, 24.6 % (n = 47) were Janajati, 9.4 % (n = 18) were Madhesi and 4.2 % (n = 8) were of other ethnic origin. The mean age of the respondents was 21.5 ± 1.0 (SD) years.
Modifiable Risk Factors
Tobacco Use
One-fifth (n = 39) of the medical students were current tobacco users and 12 % (n = 23) of those were daily users, 11 % (n = 21) were current daily smokers, 3.1 % (n = 6) were current smokeless tobacco users, and three (1.6 %) used both forms of tobacco. The mean age of initiation of smoking was 18.6 ± 1.2 (SD) years and mean duration of smoking was 3.1 ± 1.2 (SD) years (Table 1). All smokers smoked manufactured cigarettes, and the mean number of manufactured cigarettes used by daily smokers was 5.7 ± 1.8 (SD) (Table 2). Brahmin/Chhetri was found to be the ethnic group with the largest number of current tobacco users (n = 30, 25.4 %) compared to other ethnic minority groups.
Alcohol Consumption
Half (n = 97) of the medical students have ever consumed alcohol. One-third (n = 65) of medical students consumed alcohol less than once a month. The mean age of initiation of alcohol use was 18.1 ± 0.6 years (SD) (Table 3). During the past 30 days, the mean number of days of drinking alcohol was 3 ± 0.8 days (SD), and the mean number of drinks consumed on a drinking day was 4.6 ± 0.8 (SD). The mean maximum number of drinks consumed on one occasion during the past 30 days was 6.3 ± 1.2 standard drinks (SD). Over the previous 30 days, the mean number of days for binge drinking was 2.6 ± 1.0 days for males and 1.1 ± 0.8 days for females (Table 4). Only 2.1 % (n = 4) consumed alcohol at a level that constituted a risk for NCDs. Brahmin/Chhetri was found to be the ethnic group with the highest number of current drinkers (n = 40, 33.9 %) compared to other ethnic minority groups.
Fruit and Vegetable Intake
The mean number of days/week where medical students consumed fruits was 3 ± 0.3 days/week and for vegetables it was 6.5 ± 0.2 days/week. On average, they consumed 3.3 ± 0.2 servings of fruits and vegetables a day. All respondents had at least one serving of fruits and vegetables daily. More than half of respondents (59.2 %) had 3–4 servings of fruits and vegetables a day followed by 1–2 servings (26.7 %) and 5–9 servings (14.1 %) (Table 5).
Physical Activity
More than two-thirds (n = 141) of the medical students were involved in low or moderate physical activity; and 26.2 % (n = 50) were involved in vigorous physical activity (Table 6). The mean duration of physical activity was 103 ± 15 min/day (inter quartile range 30–150).
Discussion
This study showed that nearly one in every five students in selected Katmandu Valley medical colleges were current tobacco users, and half of them have ever consumed alcohol. These results are consistent with the findings in other studies among medical students in Nepal [12, 20–23]. We found a higher prevalence of alcohol use among medical students than among the general Nepali youth [17]. This may be explained by anxiety during studies, confinement during academic activities, absence of parental supervision, being economically advantaged, and the frequent habitual social drinking among medical students [20–22, 24]. The mean age of initiation of smoking was late in medical students (18.6 years) compared to 15.1 years in the general youth between 15 and 24 years [17]. The mean age of initiation of smoking was approximately similar to age of entry into medical college; this suggests that medical students start smoking and consuming alcohol at the time of entry to medical school. A similar finding was found among medical students in the Kathmandu valley [20]. Contrary to this, Croen et al. [25] found a decrease in substance use among students after entering medical school. The mean age of initiation of alcohol consumption was lower in females than males, which was also found in the general population of Nepali youth [17].
This study found that a high proportion of medical students (higher than among general Nepali youth) had a lower than recommended consumption of fruits and vegetables [17]. A similar result was found in India [11]. This finding is comparable to consumption of fruits and vegetables in medical students in Greece, USA and China [26–28]. A possible explanation could be that canteens of medical colleges in Nepal do not provide adequate selection of vegetables and fruits nor students get adequate selection of vegetables and fruits in home. Dietary habits are poorly monitored, and the quality of food is rarely scrutinized in Nepal.
This study found that more than two-thirds of respondents were involved in low or moderate physical activity, and similar results were found among Egyptian, Saudi and Indian medical students [29, 30]. Medical students spent less time on physical activities daily than the general Nepali youth [17]. A systematic review showed that 74.6 % of Nepali males and 91.2 % of Nepali females (25–64 years) were physically inactive [31]. Lack of time (60.5 %), laziness (61.8 %) and exhaustion from academic activities (42 %) were identified as important obstacles among medical students who did not participate in physical activities [32]. Low physical activity among medical students in this study may be because they have to spend more time on sedentary activities such as studying, completing assignments, surgical procedures and other academically related activities. Medical students become less active in medical college when compared with levels of activity undertaken prior to embarking on their graduate training [33]. A study among graduate students enrolled in different degree programmes found that medical students was the largest group of students with a low level of physical activity (26 %) [34]. In the Kathmandu Valley, ample opportunities to engage in physical exercise are absent. Open parks, open spaces, side-walks, bike-lanes and affordable gyms are either lacking or inadequate [35].
Although this study presents important information about the prevalence of modifiable risk factors among medical students, it has some limitations. The study solely depended upon the information provided by the respondents; thus, the authors cannot disregard conscious underreporting of information by participants. Our study suggests that physical and biochemical measurements of risk factors for major NCDs are necessary. Further studies are needed including behavioural, physical and biological measurements to make a more precise estimate of NCD risk factors.
Medical students are presumed to be more health conscious due to their knowledge acquired from attending medical college. On the contrary, a high prevalence of the modifiable risk factors among the medical students may imply that they do not believe in the fundamental aspects of preventive medicine. Medical faculties need to address unhealthy behaviour to the benefit of their students as well as to maintain medical students as role models to their future patients [36]. This study suggests interventions to promote healthy lifestyle and behaviour and to inspire medical students to become tomorrow’s prevention-oriented doctors.
Conclusions
Medical students in the Katmandu Valley in Nepal were at risk of developing NCDs due to low intake of fruits and vegetables, physical inactivity, tobacco use, and high alcohol consumption. Considering the evidence that more risk factors put them at higher risk of NCDs, interventions are needed to change unhealthy behaviour among medical students.
References
World Health Organization. (2011). Global status report on noncommunicable diseases. Geneva: WHO.
WHO South-East Asia Region. (2011). Noncommunicable diseases in the South-East Asia Region. India: WHO SEARO.
World Health Organization. (2002). Health situation in the South-East Asia region 1998–2000. SEA/HS/222. New Delhi: WHO Regional Office for South-East Asia.
Neupane, D., & Kallestrup, P. (2013). Non-communicable diseases in Nepal: Challenges and opportunities. Journal of Nepal Health Research Council, 11(24), 225–228.
Bhandari, G. P., Angdembe, M. R., Dhimal, M., Neupane, S., & Bhusal, C. (2014). State of non-communicable diseases in Nepal. BMC public health, 14(1), 23.
Lopez, A. D., Mathers, C. D., Ezzati, M., Jamison, D. T., Murray, C., Haisma, H., et al. (2006). Global burden of disease and risk factors (pp. 2945–2951). Washington, DC: World Bank.
Mokdad, A. H., Marks, J. S., Stroup, D. F., & Gerberding, J. L. (2004). Actual causes of death in the United States, 2000. JAMA, the Journal of the American Medical Association, 291(10), 1238–1245.
Li, Y., Wang, L., Jiang, Y., Zhang, M., & Wang, L. (2013). Risk factors for noncommunicable chronic diseases in women in China: surveillance efforts. Bulletin of the World Health Organization, 91(9), 650–660.
World Health Organization. (2008). 2008–2013 action plan for the global strategy for the prevention and control of noncommunicable diseases: Prevent and control cardiovascular diseases, cancers, chronic respiratory diseases and diabetes. Geneva: World Health Organization.
Talwar, K., Grover, A., & Thakur, J. (2011). Role of medical education in preventing and control of noncommunicable diseases in India? Indian Journal of Community Medicine : Official Publication of Indian Association of Preventive and Social Medicine, 36(Suppl 1), S63–S66.
Naidana, P. S., & Addanki, S. P. K. (2013). A comparative study on lifestyle pertaining to risk of chronic non-communicable diseases between the students of two professional colleges. International Journal of Medical and Health Sciences, 2(1), 36–41.
Shakya, A., Mishra, S. R., Giri, S., Paudel, K. & Neupane, D. (2015). Gender differences and clustering of modifiable risk factors of non-communicable diseases among medical students: A cross sectional study in Nepal. Journal of Community Health, 40, 147–152.
Slusser, M. S., & Slusser, M. (1982). Nepal mandala: A cultural study of the Kathmandu Valley. Princeton: Princeton University Press.
Central Bureau of Statistics. (2011). National population and housing census 2011. Kathmandu: CBS.
Medical Colleges in Nepal. (2013). List of medical colleges in Nepal [cited 2014]. http://www.medicalcollegesnepal.com/category/list-of-colleges/page/3/.
World Health Organization. (2008). WHO steps instrument question-by-question guide (core and expanded). Geneva: World Health Organization.
Ministry of Health and Population (DoHS), Society for Local Integrated Development Nepal (SOLID Nepal), & WHO. (2008). Nepal non-communicable disease risk factor survey. Kathmandu: MoHP, SOLID Nepal and WHO.
Medline Plus. (2013). Alcoholism and alcohol abuse [cited 2014]. http://www.nlm.nih.gov/medlineplus/ency/article/000944.htm.
Oli, N., Vaidya, A., & Thapa, G. (2013) Behavioural risk factors of noncommunicable diseases among Nepalese Urban poor: A descriptive study from a Slum Area of Kathmandu. Epidemiology Research International, 2013
Budhathoki, N., Shrestha, M. K., Acharya, N., & Manandhar, A. (2010). Substance use among third year medical students of Nepal. Journal of Nepal Health Research Council, 8(1), 15–18.
Khanal, P., Ghimire, R. H., Gautam, B., Dhungana, S. K., Parajuli, P., Jaiswal, A. K., et al. (2010). Substance use among medical students in Kathmandu valley. JNMA: Journal of the Nepal Medical Association, 50(180), 267–272.
Shyangwa, P. M., Joshi, D., & Lal, R. (2007). Alcohols and other substance use/abuse among junior doctors and medical students in a teaching institute. JNMA: Journal of the Nepal Medical Association, 46(167), 126–129.
Kumar, S., Pokharel, B., Nagesh, S., & Yadav, B. K. (2006). Alcohol use among physicians in a medical school in Nepal. Kathmandu University Medical Journal (KUMJ), 4(4), 460–464.
Giri, S., Sharma, S. R., Timalsina, S., Yadav, V., Koirala, S., Kumar, A., et al. (2012). Cardiovascular health risk behavior among medical students in a teaching hospital. Journal of Nepal Health Research Council, 10(22), 187–191.
Croen, L. G., Woesner, M., Herman, M., & Reichgott, M. (1997). A longitudinal study of substance use and abuse in a single class of medical students. Academic Medicine : Journal of the Association of American Medical Colleges, 72(5), 376–381.
Bertsias, G., Linardakis, M., Mammas, I., & Kafatos, A. (2005). Fruit and vegetables consumption in relation to health and diet of medical students in Crete, Greece. International Journal for Vitamin and Nutrition Research Internationale Zeitschrift fur Vitamin- und Ernahrungsforschung Journal international de vitaminologie et de nutrition, 75(2), 107–117.
Spencer, E. H., Frank, E., Elon, L. K., Hertzberg, V. S., Serdula, M. K., & Galuska, D. A. (2006). Predictors of nutrition counseling behaviors and attitudes in US medical students. The American Journal of Clinical Nutrition, 84(3), 655–662.
Sakamaki, R., Toyama, K., Amamoto, R., Liu, C.-J., & Shinfuku, N. (2005). Nutritional knowledge, food habits and health attitude of Chinese university students—A cross sectional study. Nutrition Journal, 4(1), 4.
Anand, T., Tanwar, S., Kumar, R., Meena, G. S., & Ingle, G. K. (2011). Knowledge, attitude, and level of physical activity among medical undergraduate students in Delhi. Indian Journal of Medical Sciences, 65(4), 133–142.
El-Gilany, A.-H., & El-Masry, R. (2011). Physical inactivity among Egyptian and Saudi Medical Students. TAF Preventive Medicine Bulletin, 10(1), 35–44.
Ranasinghe, C. D., Ranasinghe, P., Jayawardena, R., & Misra, A. (2013). Physical activity patterns among South-Asian adults: A systematic review. The International Journal of Behavioral Nutrition and Physical Activity, 10, 116.
Rao, C. R., Darshan, B., Das, N., Rajan, V., Bhogun, M., & Gupta, A. (2012). Practice of physical activity among future doctors: A cross sectional analysis. International Journal of Preventive Medicine, 3(5), 365–369.
Gnanendran, A., Pyne, D. B., Fallon, K. E., & Fricker, P. A. (2011). Attitudes of medical students, clinicians and sports scientists towards exercise counselling. Journal of Sports Science and Medicine, 10(3), 426.
Dabrowska-Galas, M., Plinta, R., Dabrowska, J., & Skrzypulec-Plinta, V. (2013). Physical activity in students of the Medical University of Silesia in Poland. Physical Therapy, 93(3), 384–392.
Pandey, S. (2014). Getting active-challenges in a developing country UK: Exercise works [cited 2014]. http://www.exercise-works.org/latest-news/2014/3/5/getting-active-challenges-in-a-developing-country.html.
Van der Veer, T., Frings-Dresen, M. H., & Sluiter, J. K. (2011). Health behaviors, care needs and attitudes towards self-prescription: A cross-sectional survey among Dutch medical students. PLoS One, 6(11), e28038.
Acknowledgments
The authors would like to thank all the students and medical colleges that participated in the study. This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mishra, S.R., Neupane, D., Shakya, A. et al. Modifiable Risk Factors for Major Non-communicable Diseases Among Medical Students in Nepal. J Community Health 40, 863–868 (2015). https://doi.org/10.1007/s10900-015-0012-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10900-015-0012-6