Abstract
Diabetic macular edema (DME) is the most common cause of vision loss among patients with diabetes mellitus (DM), rendering it an important growing challenge in ophthalmology. In the past decades, the management strategies for DME had a few paradigm shifts, and the advent of an expanding number of anti-vascular endothelial growth factor (VEGF) agents also calls for an in-depth examination of the currently available evidence. This article was composed with the intention to provide recommendations for practicing clinicians to improve the management and, through it the outcomes of DME. Drawing from current guideline recommendations, clinical trial findings and local clinical experiences, these consensus recommendations for the management of DME were formed by an expert panel through iterations of discussion and voting. First, the treatment goal of DME is to achieve best visual outcome with edema improvement while minimizing treatment burden. Second, anti-VEGF therapy should be considered as the first-line treatment for patients with center-involving DME causing vision loss. Baseline visual acuity (VA) and central subfield thickness (CST) should be taken into consideration when choosing anti-VEGF agents. Third, early intensive anti-VEGF therapy (at least 3 monthly doses) is important for better patients’ VA and anatomical improvement. In non-responders who have already been treated with 3-5 injections of anti-VEGF agents, it is reasonable to switch to other modalities, such as steroids. Finally, for the follow-up phase, fixed or individualized dosing should be considered based on VA and OCT.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Diabetes mellitus (DM) is a serious and burgeoning metabolic disorder that poses a significant burden to both human health and socioeconomic development in modern time [1]. The global prevalence of adult DM is estimated to surge to 10.4% of the population in 2040, affecting over 640 million people [1]. Diabetes is associated with higher risks of mortality and comorbidities’ development, such as diabetic retinopathy (DR) [2]. Diabetic macular edema (DME), a common complication of DR, is the most prevalent cause of vision loss among diabetic patients, rendering it a primary health concern among the diabetic population [3]. DME also adds burden to the health care system, as its direct medical cost is 3 times greater than the average national health expenditure per person [4]. According to the National Health Insurance Research Database (NHIRD) data of 2004-2009, the diagnosis of DME among the 1.43 million DM population in Taiwan was 7.3% and the treatment of DME associated visual loss was 1.3% [4]. Analysis of the 2005-2011 data from the NHIRD database showed a steady increase in the incident cases of sight-threatening DR and a declining trend in sight-threatening DR prevalence among type 2 diabetic patients [5]. The increasing diabetic population and the excessive medical costs associated with DME are important impetuses for seeking an effective management for DME.
In the past three decades, numerous treatment strategies for DME have been developed and implemented clinically, including laser photocoagulation, corticosteroids, and intravitreal anti-vascular endothelial growth factor (VEGF) injections. The trials’ findings of these treatment measures are summarized herein.
Laser photocoagulation
Laser photocoagulation, including focal and grid laser, has been the gold standard DME treatment since the 1980s [6,7,8]. However, the role of laser has largely diminished with the advent of corticosteroids and anti-VEGF agents. Laser was established as a standard treatment for DME by the Early Treatment Diabetic Retinopathy Study (ETDRS), in which the risk of vision loss (losing ≥15 letters) was shown to be halved among patients with clinically significant macular edema (CSME) in the focal photocoagulation group; however, similar benefits were absent in the non-CSME subgroup [6].
Corticosteroids
Prior to the approval of fluocinolone and dexamethasone for ocular use in 2012, triamcinolone had been commonly used for the treatment of DME. In the randomized, sham-controlled trial of dexamethasone intravitreal implant in patients with diabetic macular edema study (MEAD), trial subjects were randomized to receive dexamethasone implant 0.7 mg, dexamethasone implant 0.35 mg, or sham procedure [9]. After 3 years of follow up, the percentage of patients with ≥15-letter improvement was greatest in the high-dose group [9]. Dexamethasone implant 0.7 mg thus became the standard treatment for the management of DME. However, treatment efficacy could be compromised by cataract formation, as visual acuity (VA) was noted to have decreased among dexamethasone-treated patients after the first year of treatment, but remained consistent in the pseudophakic subgroup [9]. Moreover, the rate of intraocular pressure (IOP) increase requiring treatment was also significantly higher among the dexamethasone-treated patients [9]. Therefore, albeit highly efficacious, the use of corticosteroids may be deterred by safety issues including cataracts and IOP elevation.
Anti-VEGF therapy
The role of anti-VEGF agents as the first-line therapy for DME has been consolidated by the well-established disease modifying effects of VEGF inhibition on DME [10, 11]. In the study of ranibizumab injection in subjects with clinically significant macular edema with center involvement secondary to diabetes mellitus study (RISE/RIDE study), trial participants were randomized to receive ranibizumab 0.3 mg, ranibizumab 0.5 mg monthly injections, or monthly sham injections [12]. Compared with the sham control group, ranibizumab-treated patients gained significant visual improvements, peaking as early as 5-6 months after treatment [12]. Treatment responses to ranibizumab were durable and maintained for over 4.5 years, and were associated with central foveal thickness reduction [13, 14]. Nonetheless, it is of note that delayed ranibizumab treatment may offer limited benefits, as seen with the crossover sham control group [13]. While patients in the 2 active treatment groups shared similar efficacy and safety profiles, the risk of stroke appeared to be slightly higher in the 0.5 mg treatment group [14]. In consequence, 0.3 mg was the standard dose for ranibizumab treatment approved by the Federal Drug Administration (FDA).
In the of intravitreal aflibercept injection in patients with diabetic macular edema (VIVID/VISTA) studies, patients were randomized to receive aflibercept 2 mg q4w, aflibercept 2 mg q8w (after 5 monthly doses), or laser photocoagulation [15]. Irrespective of dose, aflibercept-treated patients gained significantly greater visual improvement compared with the laser group [16]. The standard dose for aflibercept was determined to be 2 mg q8w (after 5 monthly doses). Furthermore, aflibercept significantly reduced central subfield thickness (CST) [16]. Visual improvement was less pronounced among patients in the laser group who crossed over to receive aflibercept after week 100, which corroborates the preference of early treatment [16]. No outstanding safety concerns were reported in these trials [15, 16].
In Taiwan, while reimbursement is currently available for ranibizumab (Lucentis), aflibercept (Eylea), and dexamethasone intravitreal implant (Ozurdex), strict conditions are imposed on the eligibility criteria and treatment duration. A total of 8 lifetime anti-VEGF injections per eye are accepted for approved individuals. The 8 doses need to be fully expended within 5 years and switching is prohibited. Reimbursement for these 3 agents is restricted to patients with a decimal VA between 0.5 and 0.05, central retinal thickness (CRT) ≥300 µm, and hemoglobin A1C (HbA1C) <10%. While reimbursement decisions for the initial 5 doses are based on test results including best-corrected visual acuity (BCVA), fluorescein angiography (FA), optical coherence tomography (OCT), color fundus, and HbA1C, only individuals with proven treatment benefits can be reimbursed for the remaining 3 injections. To help deliver optimized care under limited healthcare resources, an expert panel was formed with the hope to develop local consensus for the management of DME. The facets of care covered in this article include treatment goals, treatment options, initial treatment and assessments, and follow-up schedule and criteria for assessment.
Methods
A panel meeting involving 12 experts was held on January 5th, 2019 in Taipei. The ophthalmology experts were convened to review current evidence and develop consensus recommendations for the management of DME. A total of 6 proposed statements and 1 management algorithm were formulated prior to the meeting, based on current guideline recommendations, local health care reimbursement policies, and treatment patterns. Each statement was discussed in depth, followed by a secret ballot. Consensus was considered to be reached when ≥70% experts voted in agreement. Re-iterations of discussion, statement modifications, and voting were carried out until the attainment of consensus.
Recommendations
The consensus recommendations for the management of DME are summarized below (Table 1).
Treatment goal

BCVA is designated as the primary endpoint in major pilot studies of the treatment agents for DME. For example, the proportion of patients gaining >15 letters in BCVA from baseline was opted for the primary endpoint in the study of ranibizumab injection in subjects with clinically significant macular edema with center involvement secondary to DM (RISE/RIDE) [12] and randomized, sham-controlled trial of dexamethasone intravitreal implant in patients with DME (MEAD) [9] studies, whereas the mean change in BCVA from baseline was selected as the primary endpoint in ranibizumab monotherapy or combined with laser versus laser monotherapy for DME resolution (RESTORE) [17], VIVID/VISTA [15], DRCR.net Protocol I [18], as well as DRCR.net Protocol T [19] studies. In the clinical setting, however, VA improvements may be less accurately portrayed, given that the Snellen, not the ETDRS chart, is the commonly used tool for VA testing. In some cases, VA improvement may be absent despite the resolution of macular edema. For these reasons, the experts recommend including improvements in edema as a treatment goal for DME.
Treatment options

DRCR.net Protocol I shows that the prompt laser group had a gradual improvement in VA, whereas the triamcinolone + prompt laser group experienced a temporary gain in VA prior to cataract formation [18, 20, 21]. Despite surgery, vision improvements in the latter group were very limited. The anti-VEGF group, on the other hand, had rapid (i.e. <3 months) and sustained improvements in VA [18, 20, 21]. Based on the available evidence, the experts agreed that anti-VEGF therapy should be a first-line therapy for patients with center-involving DME with vision loss, in line with the published recommendations of Asian and Japanese experts [2, 11]. For patients with a history of major cardiovascular events, pseudophakic or post-vitrectomy eyes, who are pregnant, or are not able to return for follow up in the first 6 months, experts agree that corticosteroids may be considered as a first choice of treatment [10, 11, 22].

In the Protocol T study, treatment with aflibercept was associated with greater VA improvement at 1 year among patients with poorer baseline VA (i.e. ≤0.4), as compared with treatment with ranibizumab or bevacizumab [19]. However, the level of improvement between aflibercept and ranibizumab at 2 years was comparable [23]. Nonetheless, the improvement in VA area under curve (AUC) over 2 years was significantly greater in the aflibercept group, compared with the other 2 treatment groups [23]. Among patients with mild VA loss at baseline, the amount of improvement was similar across the 3 groups [19, 23]. Of note, the study dose of ranibizumab was 0.3 mg, instead of 0.5 mg.
While VA loss has been central to DME treatment evaluation, the value of CST should not be dismissed. For patients with poor VA but relatively thinner CST, the therapeutic effect of aflibercept might not exceed the other anti-VEGF agents. Subgroup analyses in the Protocol T study affirms that treatment with aflibercept was associated with greater VA improvement in patients with thicker CST (i.e. ≥400 μm) [19]. Therefore, in addition to baseline VA, the experts suggest that CST should also be taken into account in the selection of first-line anti-VEGF therapy.
Initial treatment and assessment

A majority of the experts agree that early, intensified anti-VEGF therapy is critical to VA and anatomical improvement. Most randomized clinical trials of DME treatment with anti-VEGF also administer at least 3 monthly doses in the treatment initiation phase [12, 15, 17,18,19]. As shown in the phase 2 DME and VEGF Trap-Eye investigation of clinical impact (DA VINCI) study, the more intensive dosing regimen (i.e. 2 mg q4w vs 2 mg q8w) after the 3 monthly loading dose was associated with greater numerical improvements in BCVA and CRT [24]. In consequence, subsequent studies such as VIVID/VISTA opted for a loading dose of 5 injections [15], and a post hoc analysis of these studies revealed a continuous improvement in functional and anatomic responses following the 4th and 5th loading injections [25]. Similarly, a decreasing trend in the percentage of eyes with persistent DME over 24 weeks (after 3-6 consecutive monthly injections) was exhibited in a secondary analysis of Protocol T [26]. Although most trials recommend an initial loading dose of anti-VEGF injections, there is evidence suggesting some eyes with DME did well and maintained stable VA at 1 year with a pro re nata (PRN) treatment starting at the first month [27]. In Taiwan, a total of 8 lifetime anti-VEGF injections per eye are reimbursed for eligible patients, and can be applied in two separate phases (e.g. 5 in phase 1 and 3 in phase 2). In practice, Taiwanese physicians generally initiate an early-intense treatment (i.e. 3-5 initial loading injections) to increase patient awareness. In addition, the pre-scheduled series of initial treatments also enhances patients’ adherence and compliance. To reserve room for professional judgment and treatment flexibility, and conforming to the routine practice pattern in Taiwan, experts suggest giving at least 3 loading doses as initial treatment. Of note, the 5-year results from Protocol I demonstrate that the initial vision gains at 1 year were maintained in most eyes treated with ranibizumab + prompt/deferred laser throughout the 5-year period and no more than a median of 2 injections per year were required after the second year [21]. These findings suggest that disease burden may be considerably relieved after 2 years of intensive treatment and close monitoring.

Changes in VA and/or retinal thickness after three consecutive injections are used as primary benchmarks for evaluating anti-VEGF treatment responses [28,29,30]. For example, specific criteria such as failing to gain >5 letters after 3 monthly injections [28] and CST ≥290 μm for women and ≥305 μm for men in Zeiss Cirrus [30], are used to determine poor responses. Having reviewed the relevant publications, the panel concurred that the term ‘non-responders’ throughout these recommendations should pertain to eyes without improvement in VA (VA improvement <5 letters or one line) as well as CST (CST ≥300 μm and reduction <20% from baseline). Responders are eyes obtaining VA improvement >5 letters or one line from the baseline and having a CST <300 μm. Individuals who fail to meet either of the criteria are categorized as inadequate responders. Based on the European Society of Retina Specialists (EURETINA) recommendations [10, 11] and local clinical experience, the experts agreed that other treatments should be sought if VA and CST remain unimproved after 3-5 injections. Subsequent treatment choices should not be confined to corticosteroid, since a variety of treatment modalities are available, including combining laser or vitrectomy [11].
Follow-up schedule and criteria for assessment

Considering the design of the currently available trials [13, 15, 18] and the all-inclusive nature of this statement, the experts did not voice any disagreements. However, the preferred follow-up strategies varied. Under the current medical care in Taiwan, 6 (55%), of the experts showed preference for PRN, 4 (36%) for Treat-and-Extend (T&E), and 1 (9%) for others.
An algorithm for center-involving DME management under the initial and follow-up phases was formulated (Fig. 1). For patients with center-involving DME with vision loss, laser should be reserved as a rescue treatment, instead of a primary treatment option. Given that the mean changes in VA and CST at 2 years in patients with good initial VA (i.e. 20/25 or better) were not significantly different between patients who were initially managed with aflibercept and those in the laser or observation arm who received aflibercept upon the worsening of VA [31], anti-VEGF or observation is recommended for patients with baseline VA greater than 0.5.
Treatment algorithm for center-involving DME. 1Corticosteroids can be considered as the first choice in patients who have a history of major cardiovascular events, with pseudophakic or post-vitrectomy eyes, with pregnancy, or patients who are not able to return for follow-up in the first 6 months. 2Anti-VEGF therapy should be considered as the first-line treatment; baseline VA and CST should be taken into consideration when choosing anti-VEGF agents. 3Early intensive anti-VEGF therapy (at least 3 monthly doses) is important for patients’ VA and anatomical improvement. 4Non-responder: No improvement of VA (VA improvement <5 letters or one line) AND CST (CST ≥300 μm and reduction <20% from baseline). 5Responder: VA improvement >5 letters or one line from the baseline AND CST <300 μm. 6In non-responders who have already been treated with 3–5 injections of anti-VEGF therapy, it is reasonable to switch to other modalities, such as steroids. 7For the follow-up phase, the fixed or individualized dosing should be considered based on VA and OCT. CST: central subfield thickness; DME: diabetic macular edema; FA, fluorescein angiography; FU, follow-up; OCT: optical coherence tomography; VA: visual acuity; VEGF: vascular endothelial growth factor
Conclusions
DME is the most frequent cause of vision impairment among patients with diabetes and it may substantially compromise patients’ quality of life. Moreover, the need for proper management is accentuated by the steadily rising prevalence of DM. Despite the fact that DME management has substantially improved over time, collective efforts of clinicians, health care authorities, and pharmaceutical industry are required to provide patients with highly efficacious and cost-effective treatments. The present document was developed through a careful scrutiny of the published and clinical evidence, and with the intention to support the ophthalmologists in Taiwan with the latest practical guidance for DME treatment. Nevertheless, the recommendations in this article may be subject to or require updates, to remain in adherence to the latest trial results and local public health programs.
References
Ogurtsova K, da Rocha Fernandes JD, Huang Y, Linnenkamp U, Guariguata L, Cho NH, et al. IDF Diabetes Atlas: global estimates for the prevalence of diabetes for 2015 and 2040. Diabetes Res Clin Pract. 2017;128:40–50.
Cheung GC, Yoon YH, Chen LJ, Chen SJ, George TM, Lai TY, et al. Diabetic macular oedema: evidence-based treatment recommendations for Asian countries. Clin Exp Ophthalmol. 2018;46:75–86.
Strain WD, Cos X, Hirst M, Vencio S, Mohan V, Voko Z, et al. Time to do more: addressing clinical inertia in the management of type 2 diabetes mellitus. Diabetes Res Clin Pract. 2014;105:302–12.
Yang MC, Tan EC, Su YJ, Lai CC. PSS2 Epidemiology, treatment patterns and medical expenses of diabetic macular edema in Taiwan: a nationwide claim-based database study. Value Health. 2012;15:A642.
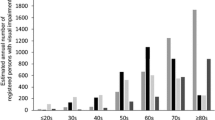
Lin JC, Shau WY, Lai MS. Sex- and age-specific prevalence and incidence rates of sight-threatening diabetic retinopathy in Taiwan. JAMA Ophthalmol. 2014;132:922–8.
Early Treatment Diabetic Retinopathy Study Research Group. Photocoagulation for diabetic macular edema. Early Treatment Diabetic Retinopathy Study report number 1. Arch Ophthalmol. 1985;103:1796–806.
Mohamed Q, Gillies MC, Wong TY. Management of diabetic retinopathy: a systematic review. JAMA. 2007;298:902–16.
Palanker DV, Blumenkranz MS, Marmor MF. Fifty years of ophthalmic laser therapy. Arch Ophthalmol. 2011;129:1613–9.
Boyer DS, Yoon YH, Belfort R Jr, Bandello F, Maturi RK, Augustin AJ, et al. Three-year, randomized, sham-controlled trial of dexamethasone intravitreal implant in patients with diabetic macular edema. Ophthalmology. 2014;121:1904–14.
Schmidt-Erfurth U, Garcia-Arumi J, Bandello F, Berg K, Chakravarthy U, Gerendas BS, et al. Guidelines for the management of diabetic macular edema by the European Society of Retina Specialists (EURETINA). Ophthalmologica. 2017;237:185–222.
Terasaki H, Ogura Y, Kitano S, Sakamoto T, Murata T, Hirakata A, et al. Management of diabetic macular edema in Japan: a review and expert opinion. Jpn J Ophthalmol. 2018;62:1–23.
Nguyen QD, Brown DM, Marcus DM, Boyer DS, Patel S, Feiner L, et al. Ranibizumab for diabetic macular edema: results from 2 phase III randomized trials: RISE and RIDE. Ophthalmology. 2012;119:789–801.
Boyer DS, Nguyen QD, Brown DM, Basu K, Ehrlich JS, Ride, et al. Outcomes with as-needed ranibizumab after initial monthly therapy: long-term outcomes of the phase III RIDE and RISE trials. Ophthalmology. 2015;122:2504–13 e1.
Brown DM, Nguyen QD, Marcus DM, Boyer DS, Patel S, Feiner L, et al. Long-term outcomes of ranibizumab therapy for diabetic macular edema: the 36-month results from two phase III trials: RISE and RIDE. Ophthalmology. 2013;120:2013–22.
Korobelnik JF, Do DV, Schmidt-Erfurth U, Boyer DS, Holz FG, Heier JS, et al. Intravitreal aflibercept for diabetic macular edema. Ophthalmology. 2014;121:2247–54.
Heier JS, Korobelnik JF, Brown DM, Schmidt-Erfurth U, Do DV, Midena E, et al. Intravitreal aflibercept for diabetic macular edema: 148-Week results from the VISTA and VIVID studies. Ophthalmology. 2016;123:2376–85.
Mitchell P, Bandello F, Schmidt-Erfurth U, Lang GE, Massin P, Schlingemann RO, et al. The RESTORE study: ranibizumab monotherapy or combined with laser versus laser monotherapy for diabetic macular edema. Ophthalmology. 2011;118:615–25.
Diabetic Retinopathy Clinical Research N, Elman MJ, Aiello LP, Beck RW, Bressler NM, Bressler SB, et al. Randomized trial evaluating ranibizumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edema. Ophthalmology. 2010;117:1064–77 e35.
Diabetic Retinopathy Clinical Research N, Wells JA, Glassman AR, Ayala AR, Jampol LM, Aiello LP, et al. Aflibercept, bevacizumab, or ranibizumab for diabetic macular edema. N Engl J Med. 2015;372:1193–203.
Diabetic Retinopathy Clinical Research N, Elman MJ, Qin H, Aiello LP, Beck RW, Bressler NM, et al. Intravitreal ranibizumab for diabetic macular edema with prompt versus deferred laser treatment: three-year randomized trial results. Ophthalmology. 2012;119:2312–8.
Elman MJ, Ayala A, Bressler NM, Browning D, Flaxel CJ, Glassman AR, et al. Intravitreal Ranibizumab for diabetic macular edema with prompt versus deferred laser treatment: 5-year randomized trial results. Ophthalmology. 2015;122:375–81.
Kodjikian L, Bellocq D, Bandello F, Loewenstein A, Chakravarthy U, Koh A, et al. First-line treatment algorithm and guidelines in center-involving diabetic macular edema. Eur J Ophthalmol. 2019;1120672119857511.
Wells JA, Glassman AR, Ayala AR, Jampol LM, Bressler NM, Bressler SB, et al. Aflibercept, bevacizumab, or ranibizumab for diabetic macular edema: two-year results from a comparative effectiveness randomized clinical trial. Ophthalmology. 2016;123:1351–9.
Do DV, Nguyen QD, Boyer D, Schmidt-Erfurth U, Brown DM, Vitti R, et al. One-year outcomes of the DA VINCI Study of VEGF Trap-Eye in eyes with diabetic macular edema. Ophthalmology. 2012;119:1658–65.
Ziemssen F, Schlottman PG, Lim JI, Agostini H, Lang GE, Bandello F. Initiation of intravitreal aflibercept injection treatment in patients with diabetic macular edema: a review of VIVID-DME and VISTA-DME data. Int J Retina Vitreous. 2016;2:16.
Bressler NM, Beaulieu WT, Glassman AR, Blinder KJ, Bressler SB, Jampol LM, et al. Persistent macular thickening following intravitreous aflibercept, bevacizumab, or ranibizumab for central-involved diabetic macular edema with vision impairment: a secondary analysis of a randomized clinical trial. JAMA Ophthalmol. 2018;136:257–69.
James DGP, Mitkute D, Porter G, Vayalambrone D. Visual outcomes following intravitreal ranibizumab for diabetic macular edema in a pro re nata protocol from baseline: a real-world experience. Asia Pac J Ophthalmol (Phila). 2019;8:200–5.
Cicinelli MV, Cavalleri M, Querques L, Rabiolo A, Bandello F, Querques G. Early response to ranibizumab predictive of functional outcome after dexamethasone for unresponsive diabetic macular oedema. Br J Ophthalmol. 2017;101:1689–93.
Khan Z, Kuriakose RK, Khan M, Chin EK, Almeida DR. Efficacy of the intravitreal sustained-release dexamethasone implant for diabetic macular edema refractory to anti-vascular endothelial growth factor therapy: meta-analysis and clinical implications. Ophthalm Surg Lasers Imaging Retina. 2017;48:160–6.
Maturi RK, Glassman AR, Liu D, Beck RW, Bhavsar AR, Bressler NM, et al. Effect of adding dexamethasone to continued ranibizumab treatment in patients with persistent diabetic macular edema: a DRCR Network phase 2 randomized clinical trial. JAMA Ophthalmol. 2018;136:29–38.
Baker CW, Glassman AR, Beaulieu WT, Antoszyk AN, Browning DJ, Chalam KV, et al. Effect of initial management with aflibercept vs laser photocoagulation vs observation on vision loss among patients with diabetic macular edema involving the center of the macula and good visual acuity: a randomized clinical trial. JAMA. 2019;321:1880–94.
Acknowledgements
Writing and editorial assistance in the preparation of this manuscript was provided by Health Care Medical Publishing, Ltd. The content of this article was expressed according to the opinions of authors and the manuscript submission for publication was completed with the final approval of all authors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
J. T. Chen, Consultant fee (Bayer); L.J. Chen, Consultant fee (Bayer, Novartis), Honorarium (Bayer, Novartis); S.N. Chen, Consultant fee (Bayer); W.L. Chen, Consultant fee (Bayer), Honorarium (Bayer, Novartis); C.K. Cheng, Consultant fee (Bayer), Honorarium (Allergan, Bayer, Novartis); S.M. Hsu, Consultant fee (Bayer), Honorarium (Allergan, Bayer, Novartis); S.J. Sheu, Consultant fee (Bayer), Honorarium (Allergan, Bayer, Novartis); W.C. Wu, Consultant fee (Bayer), Honorarium (Allergan, Bayer, Novartis); C.H. Yang, Consultant fee (Bayer), Honorarium (Allergan, Bayer, Novartis); C.M. Yang, Consultant fee (Bayer, Novartis), Honorarium (Bayer, Novartis); L. Yeung, Consultant fee (Bayer, Novartis), Honorarium (Allergan); D. K. Hwang, Consultant fee (Allergan); S. J. Chen, Consultant fee (Bayer, Novartis), Honorarium (Allergan, Bayer Novartis).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Organizer: Mineo Kondo, MD, PhD.
Corresponding Author: Shih-Jen Chen
About this article
Cite this article
Chen, JT., Chen, LJ., Chen, SN. et al. Management of diabetic macular edema: experts’ consensus in Taiwan. Jpn J Ophthalmol 64, 235–242 (2020). https://doi.org/10.1007/s10384-020-00741-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-020-00741-4