Abstract
Purpose
To examine the prognosis of patients with diabetic macular edema (DME) before Japanese approval of antivascular endothelial growth factor (VEGF).
Methods
This retrospective study included 135 eyes of 115 patients who received treatments (photocoagulation, pharmacological treatments, vitrectomy) for DME between January 2003 and August 2012. The best-corrected visual acuity (BCVA) before and 1, 3, 6, 12, and 24 months after treatment was examined. BCVA was classified based on the decimal value of BCVA before treatment as good (BCVA > 0.7, BCVA = 0.7), moderate (BCVA > 0.7 but <0.2), or poor (BCVA < 0.2, BCVA = 0.2), and each prognosis of BCVA was investigated.
Results
Thirty-five (25.9 %) patients were classified with good BCVA, while 69 (51.1 %) had moderate and 31 (23.0 %) poor BCVA. Following 24 months of treatment, the averaged good BCVA maintained its value (0.0513 ± 0.0954 to 0.0773 ± 0.258). Similarly, the averaged moderate BCVA maintained its value (0.449 ± 0.169 to 0.441 ± 0.431), whereas the averaged poor BCVA significantly improved (1.070 ± 0.291 to 0.879 ± 0.361: p < 0.001). Specifically, the averaged BCVA of patients who initially received vitrectomy increased 0.380 logMAR after 24 months (0.859 ± 0.414 to 0.479 ± 0.549).
Conclusion
DME patients with good BCVA at the time of initial treatment generally maintained the averaged BCVA at 24 months, while patients with moderate BCVA did not significantly improve without a standard regimen of anti-VEGF therapy. However, the results indicate that early vitrectomy is a potential treatment option for DME patients with poor BCVA.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Diabetic macular edema (DME) is a disease associated with diabetic retinopathy that causes irreversible macular changes. Treatment for DME has evolved since 1985, when reports from the early treatment diabetic retinopathy study indicated that macular photocoagulation could reduce the risk of visual loss by 50 % [1, 2]. In the 1990s, vitrectomy was considered an effective treatment for diffuse macular edema [3–5]. In 2000, the effectiveness of intravitreal triamcinolone acetonide (IVTA) was demonstrated, although the associated long-term prognoses have been poor, and related risks of cataracts and high intraocular pressure have been reported [6, 7].
More recently, a large-scale clinical trial involving treatment with antivascular endothelial growth factor (VEGF) antibodies demonstrated better prognoses than laser photocoagulation alone [8]. Consequently, the effectiveness of anti-VEGF for the treatment of DME has been confirmed [8–13]. However, the clinical trials excluded patients with good best-corrected visual acuity (BCVA) without foveal involvement, as well as patients with severe diabetic retinopathy, or severe DME and poor initial BCVA. In addition, over 30 % of the patients received photocoagulation in the anti-VEGF monotherapy group. Therefore, the results of the clinical trials might not reflect the actual complexity of the clinical setting. We believe that the clinical setting should be a factor in the selection of anti-VEGF and other kinds of treatment.
In Japan, limited information exists on the effects of treatment with anti-VEGF antibodies in DME patients because intravitreal anti-VEGF (ranibizumab) injection for DME was only recently approved (February 2014). In the current study, we examined the prognosis of DME patients who received different treatments including vitrectomy, photocoagulation and pharmacological treatments in order to evaluate the efficacy of the various approaches prior to the approval of anti-VEGF therapy in Japan.
Subjects and methods
Subjects
The subjects were 163 consecutive patients (183 eyes) who received treatment for DME at St. Luke’s International Hospital (Tokyo, Japan) from January 2003 to August 2012. The subjects included patients who were followed up for >6 months following the initial day of treatment. Forty-four of 183 eyes were not followed up for >6 months. The number of patients available for follow-up until 6 months was 135, that for up to 12 months was 132, and that for up to 24 months was 114. Because of the potential influence of this on the main outcome of the study, exclusion criteria included the presence of vitreal hemorrhage and severe cataracts (Emery–Little grade >3) before treatment or vitreal hemorrhage and progression of cataracts (Emery–Little grade >3) following treatment. The data of three eyes with vitreous hemorrhage and one eye with severe cataract during the observation period were dropped from the onset of these diseases. Eventually, there were 115 subjects (94 men, 41 women, 135 eyes), and the average age of the patients was 63.4 ± 7.5 years (range 41–80 years). The average duration of follow-up was 22 months (range 6 months–2 years). Patients with macular traction without macular edema were not included, but patients with macular traction with macular edema based on the diabetic vascular abnormality were included.
Methods
This study was approved by the Institutional Review Board of St. Luke’s International Hospital Clinical Research Ethics Committee prior to commencing this study.
We performed retrospective chart reviews of patients undergoing microaneurysm photocoagulation, subthreshold micropulse diode laser photocoagulation, grid laser photo coagulation, IVTA, subtenon triamcinolone acetonide (STTA) injection, and vitrectomy with inner limiting membrane peeling combined with phacoemulsification plus intraocular lens implantation, or intravitreal anti-VEGF (bevacizumab) injection as a single or multiple session treatment for DME. At the time of this study, anti-VEGF treatment had not yet been approved in Japan; therefore, only a few patients in this study had received this treatment. Upon approval by the ethical review board, intravitreal injections of bevacizumab were administered.
The following data were extracted from each of the charts: BCVA measurements before the treatment and at 1, 3, 6, 12, and 24 months after initial treatment, treatment history during the observation period, OCT scans performed before the treatment, and any notation of general complications.
The correlation between factors before treatment and the prognosis was examined. The prognosis was defined as the following status. Patients who had at least 0.3 logMAR improvements during the observation period and/or decimal BCVA values greater than 0.7 on the last visit were defined as good and all the others were defined as poor.
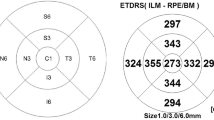
A previous study reported that the BCVA before treatment correlated with the BCVA after treatment in DME [5]. We categorized BCVA before treatment. All subjects were classified into three groups based on the decimal value of BCVA before treatment including good (BCVA > 0.7, BCVA = 0.7), moderate (BCVA > 0.7 but <0.2), and poor (VA < 0.2, BCVA = 0.2). Since receiving a driver’s license in Japan requires a 0.7 or more decimal BCVA, we defined good visual acuity as above this value. Since standard social life requires an approximately 0.2 or more decimal value, we defined moderate as above that value and poor as below. The BCVA decimal value was converted to logMAR units for comparison, and changes in BCVA were evaluated. Charts were reviewed for possible causes of treatment failure. All OCT scans obtained in the horizontal and sagittal plane using a Zeiss Stratus OCT 3000 scanner (until November 2009; Carl Zeiss Meditec Inc., Dublin, CA, USA) or a Cirrus HD-OCT scanner (from November 2009 until August 2012; Carl Zeiss Meditec Inc., Dublin, CA, USA) were analyzed by a single well-trained ophthalmologist (KO). The morphology of macular edema observed on OCT scans was classified into five groups according to Otani’s classification [14]: sponge-like retinal swelling, cystoid macular edema (CME), serous retinal detachment (SRD), a combination of CME and SRD (CME + SRD), and posterior hyaloidal traction with macular edema (Fig. 1). Central macular thickness (CMT) was also measured based on automatic 6 × 6-mm cube data captured with the same OCT instruments. Further, according to a report by Abedi et al. [15], subtracting 60 from CMT values determined by a Cirrus HD-OCT instrument can calculate CMT values equivalent to those determined by the OCT 3000 instrument.
All statistical analyses were performed using SPSS 15.0 J for Windows (SPSS Japan Inc., Tokyo, Japan). The changes in BCVA were compared using the Wilcoxon signed-rank test. For factors before treatment influencing BCVA prognosis, factors with p < 0.2 following univariate analysis were subjected to multivariate analysis, and factors with p < 0.05 were considered statistically significant by the linear recurrence method.
Results
The characteristics of the DME patients included in this study are detailed in Table 1. Mean serum HbA1c levels were 7.05 ± 1.26 %. Forty-three (31.8 %) patients had diabetic kidney disease, and ten (7.4 %) required dialysis. Mean CMT before treatment was 479 ± 173 μm. Fifty-four (38 %) eyes had a CMT > 500 μm, 68 (48 %) had a CMT ≥ 300 μm but ≤500 μm, and 20 (14 %) had a CMT < 300 μm. Macular edema before treatment was categorized as CME in 99 (68 %) eyes, CME + SRD in 18 (12 %) eyes, sponge-like retinal swelling in 12 (8 %) eyes, SRD in 9 (6 %) eyes, and posterior hyaloidal traction in 8 (6 %) eyes.
The average number of treatments was 2.36, with 71 eyes (48 %) receiving a single treatment and 77 eyes (52 %) requiring at least one additional treatment during the observation period. Treatments included macular photocoagulation (128 eyes), anti-VEGF (60 eyes), vitrectomy (52 eyes), STTA (40 eyes), and IVTA (39 eyes; Table 2). All patients who received vitrectomy underwent phacoemulsification and intraocular lens implantation simultaneously. Generally, patients with lightly thickened macular edema received focal photocoagulation (including subthreshold micropulse diode laser) if they had good BCVA (BCVA > 0.7, BCVA = 0.7). Grid laser photocoagulation, IVTA, STTA, or anti-VEGF was applied in patients with moderate BCVA (BCVA < 0.7 but >0.2). Grid laser photocoagulation was applied to the patient presenting with diffuse dye leakage, while IVTA was applied (from 2003 to 2007) in patients with severe diffuse macular edema. STTA injection and/or photocoagulation for microaneurysm were performed in patients with moderately thickened macular edema. Vitrectomy was the treatment of choice in patients with poor BCVA (BCVA < 0.2, BCVA = 0.2) and extremely thickened macular edema and in patients with posterior hyaloidal traction. In cases that involved changes in the BCVA grading following treatment, patients received different treatments. Upon approval by the ethical review board, a single intravitreal injection of bevacizumab was administered to steroid responder patients and to patients with diffuse macular edema who had not been responsive to prior treatments. Thirty-eight eyes of 32 patients in which triamcinolone acetonide was administered presented with cataract progression, and 34 eyes of 30 patients underwent vitrectomy combined with phacoemulsification plus intraocular lens implantation between observation periods.
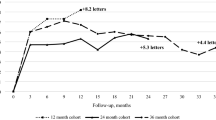
Average BCVA (logMAR) prior to treatment and at 1, 3, 6, 12, and 24 months after treatment was 0.489 ± 0.408, 0.455 ± 0.408, 0.410 ± 0.360, 0.399 ± 0.384, 0.419 ± 0.410, and 0.437 ± 0.465, respectively. Compared to baseline (before treatment) BCVA values, the measurements at 3, 6, and 12 months following treatment improved significantly (p = 0.002, p = 0.001 and p = 0.048, respectively). However, following 24 months of treatment, the difference in BCVA compared to pretreatment values was not significantly different (Fig. 2). BCVA before treatment was moderately correlated with BCVA at 24 months after treatment (Fig. 3).
The results of univariate analyses revealed that BCVA before treatment, HbA1c levels, presence of intraocular lens, and dialysis were factors that potentially influenced BCVA prognosis. Multivariate analysis showed that only dialysis was significantly correlated with prognosis.
Before treatment, there were 35 (25.9 %) patients with good, 69 (51.5 %) with moderate, and 31 (23.0 %) with poor BCVA. At 24 months, there were 41 eyes (36.0 %) with good, 51 eyes (44.7 %) with moderate, and 22 eyes (19.3 %) with poor BCVA.
Patients with averaged good BCVA were maintained (range 0.0513 ± 0.0954 to 0.0773 ± 0.278). Similarly, patients with averaged moderate BCVA were maintained (range 0.449 ± 0.169 to 0.441 ± 0.431). In patients with poor BCVA, significant improvement in BCVA at 1, 3, 6, 12, and 24 months after treatment was 0.970 ± 0.297, 0.894 ± 0.232, 0.835 ± 0.373, 0.848 ± 0.290, and 0.879 ± 0.361, respectively. Further, the differences were significant at 3, 6, 12, and 24 months compared to baseline measurements (p < 0.001 for all comparisons). BCVA at 24 months in the group with poor BCVA prior to treatment was significantly lower than values from the groups with good or moderate BCVA (Fig. 4). In particular, BCVA significantly increased 0.859 ± 0.414 to 0.479 ± 0.549, which corresponded to an average increase of 0.380 in patients who received vitrectomy at first treatment (p < 0.001), while BCVA at 24 months increased 0.369 ± 0.346 to 0.346 ± 0.400 in the patients who received laser photocoagulation and/or pharmacological treatments. Averaged BCVA in patients who had phacoemulsification at 24 months was 0.537 ± 0.491 (n = 61); on the other hand, in those who did not have it, the value was 0.324 ± 0.405 (n = 51). Twenty-three eyes did not have the data at 24 months (Table 3).
An increase of at least 0.3 logMAR after 2 years of treatment was observed in 41 eyes (41.3 %). Conversely, a decrease of approximately 0.3 logMAR was observed in 18 eyes (12.6 %). The causes of the visual loss included nine cases of macular atrophy, four cases of foveal hard exudates, two cases of neovascular glaucoma, and two cases of central retinal vein occlusion.
In the eyes with CME + SRD morphology, BCVA was significantly worse compared with the other groups (p < 0.001). In the CME + SRD group, BCVA was significantly improved at 1 and 3 months (p = 0.039, 0.011) and not significantly improved 24 months after treatment (Fig. 5). BCVA of the sponge-like retinal swelling group at 24 months after treatment was the best (0.347), corresponding to a good BCVA prognosis (Table 4).
Discussion
A previous clinical trial involving consecutive injections of anti-VEGF antibodies over a period of 2 years demonstrated promising results in DME patients [10]. However, in this study, overall BCVA after 2 years of treatment was not significantly improved after treatment with anti-VEGF antibodies. A possible explanation for this result is that anti-VEGF therapy was not administered according to the standard regimen, but also that the subjects included severe cases that would otherwise not be included in clinical trials. In addition, patients with good BCVA had only marginal room for improvement compared to patients with moderate or poor BCVA.
Approximately 60 % of patients with good BCVA in this study received laser treatment alone or in conjunction with an additional treatment modality. It became clear that patients who started the treatment for DME while BCVA measurements were still good had a favorable long-term prognosis, which indicates the importance of early treatment. Ohkoshi et al. [16] reported that BCVA was maintained for 1 year by performing subthreshold micropulse diode laser treatment for DME, while Othman et al. [17] reported the usefulness of subthreshold micropulse diode laser treatment for CSME. In the current study, a shift from high- to low-intensity laser therapy made it possible for us to start treatment at an earlier time point.
However, in the moderate BCVA group, BCVA was not significantly improved. The RESTORE study reported that patients with an initial BCVA of approximately Swollen equivalent 20/30–20/160 who received ranibizumab monotherapy could read 6.1 letters (approximately 0.12 logMAR) 1 year after treatment [8]. Similarly, the RISE and RIDE studies, which included patients with an initial BCVA of 20/40 to 20/320, reported that the gain of letters from baseline to 2 years after treatment was approximately 0.2 logMAR [10]. Therefore, considering the reported results of large clinical trials, we believe that anti-VEGF therapy could be useful in some cases.
In our study, BCVA significantly improved in the group of patients with poor BCVA. Further, BCVA in patients who were initially treated with vitrectomy improved significantly by 0.380 logMAR. We postulate that the BCVA in patients who received laser photocoagulation and/or pharmacological treatments did not significantly improve because this group mostly included patients who had good VA at the initial stage. Kumagai et al. [5] reported that patients with an average initial BCVA of 0.19 logMAR who received vitrectomy improved approximately 0.20 logMAR within 1 year following surgery, which indicates that vitretomy was an effective treatment for severe DME. The number of anti-VEGF injections per patient was approximately 7–12 in the overseas clinical study [8–10]. In the current study, the average number of total treatments per patient was 1.94 in the good BCVA group, 2.60 in the moderate BCVA group, and 2.35 in the poor BCVA group. As for patients who underwent vitrectomy as initial treatment, the average number of total treatments was 1.28 times. Also because of potential increases in the patients’ medical expenses, reducing the total number of required treatments is recommended.
Approximately 12.6 % of the patients exhibited a >0.3 logMAR decrease in BCVA. The pathogenesis for a poor BCVA prognosis is macular atrophy for longstanding macular edema, hard exudates to the central fovea, neovascular glaucoma, and central retinal vascular occlusion. Patients with neovascular glaucoma or central retinal vein obstruction had markedly deteriorated BCVA. Further, patients in the SRD + CME group had significantly poor BCVA before treatment and did not improve at 24 months, even though they had a significant improvement until 3 months. These were the most severe cases of DME; therefore, the prognosis for the SRD + CME group was poor even if there was a temporary improvement.
This study had several limitations. First, the different treatments were not randomly assigned to the patients. The ideal study would have only included patients undergoing the same therapy, but the examination of a variety of therapies might mimic the clinical setting more closely and could make our results more universally applicable. Second, anti-VEGF injections were not administered using a standard treatment regimen, but as needed, which does not entirely reflect treatments before the anti-VEGF era. However, the prophylactic use of anti-VEGF is important for achieving the desired effect. Third, we performed vitrectomy with phacoemulsification and intraocular implantation simultaneously because the rate of cataract progression following vitreous surgery is typically high. In addition, the improvement of cataracts might affect BCVA after treatment. However, we excluded patients who had severe cataracts (Emery-Little grade >3). Finally, the most important limitation of this study was the retrospective case series design. Consequently, the same OCT devices were not used; therefore, we could not evaluate the status of macular edema and assess prognosis. Given the opportunity in the future, we would like to repeat the study using a prospective design. In the current study, DME patients with good BCVA at the initiation of therapy generally had a good prognosis. DME patients with poor BCVA who underwent vitrectomy likewise exhibited good results. Consequently, the results indicate that treatment options other than anti-VEGF therapy for patients with DME do exist.
References
Early Treatment Diabetic Retinopathy Study research group. Photocoagulation for diabetic macular edema. Early Treatment Diabetic Retinopathy Study report number 1. Arch Ophthalmol. 1985;103:1796–806.
Early Treatment Diabetic Retinopathy Study Research Group. Treatment techniques and clinical guidelines for photocoagulation of diabetic macular edema. Early Treatment Diabetic Retinopathy Study report number 2. Ophthalmology. 1987;94:761–74.
Lewis H, Abram GW, Blumenkranz MS, Campo RV. Vitrectomy for diabetic macular traction and edema associated with posterior hyaloidal traction. Ophthalmology. 1992;99:753–9.
Yamamoto T, Akabane N, Takeuchi S. Vitrectomy for diabetic macular edema: the role of posterior vitreous detachment and epimacular membrane. Am J Ophthalmol. 2001;132:369–77.
Kumagai K, Furukawa M, Ogino N, Larson E, Iwaki M, Tachi N. Long-term follow-up of vitrectomy for diffuse nontractional diabetic macular edema. Retina. 2009;29:464–72.
Martidis A, Ducker JS, Greenberg PB, Rogers AH, Puliafito CA, Reichel E, et al. Intravitreal triamcinolone for refractory diabetic macular edema. Ophthalmology. 2002;109:920–7.
Beck RW, Edwards AR, Aiello LP, Bressler NM, Ferris F, Glassman AR, et al. Three-year follow-up of a randomized trial comparing focal/grid photocoagulation and intravitreal triamcinolone for diabetic macular edema. Arch Ophthalmol. 2009;127:245–51.
Mitchell P, Bandello F, Schmidt-Erfurth U, Lang GE, Massin P, Schlingemann RO. The RESTORE study: ranibizumab monotherapy or combined with laser versus laser monotherapy for diabetic macular edema. Ophthalmology. 2011;118:615–25.
Do DV, Nguyen QD, Khwaja AA, Channa R, Sepah YJ, Sophie R, et al. Ranibizumab for edema of the macula in diabetes study: 3-year outcomes and the need for prolonged frequent treatment. JAMA Ophthalmol. 2013;131:139–45.
Brown DM, Nguyen QD, Marcus DM, Boyer DS, Patel S, Feiner L, et al. Long-term outcomes of ranibizumab therapy for diabetic macular edema: the 36-month results from two phase III trials: RISE and RIDE. Ophthalmology. 2013;120:2013–22.
Nguyen QD, Shah SM, Heir JS, Boyer DS, Patel S, Feiner L, et al. Primary End Point (six months) Results of the Ranibizumab for Edema of the macula in diabetes (READ-2) study. Ophthalmology. 2009;116(2175–81):e1.
Massin P, Bandello F, Garweg JG, Hansen LL, Harding SP, Larsen M, et al. Safety and efficacy of ranibizumab in diabetic macular edema (RESOLVE Study): a 12-month, randomized, controlled, double-masked, multicenter phase II study. Diabetes Care. 2010;33:2399–405.
Research Diabetic Retinopathy Clinical, Network Elman ML, Qin H, Aillo LP, Beck RW, Bressler NM, et al. Intravitreal ranibizumab for diabetic macular edema with prompt versus deferred laser treatment: three-year randomized trial results. Ophthalmology. 2012;119:2312–8.
Otani T, Kishi S, Maruyama Y. Patterns of diabetic macular edema with optical coherence tomography. Am J Ophthalmol. 1999;127:688–93.
Abedi G, Patal P, Doros G, Subramanian ML. Transitioning from stratus OCT to cirrus OCT: a comparison and a proposed equation to convert central subfield macular thickness measurements in healthy subjects. Graefes Arch Clin Exp Ophthalmol. 2011;249:1353–7.
Ohkoshi K, Yamaguchi T. Subthreshold micropulse diode laser photocoagulation for diabetic macular edema in Japanese patients. Am J Ophthalmol. 2010;149:133–9.
Othman IS, Eissa SA, Kotb MS, Sadek SH. Subthreshold diode-laser micropulse photocoagulation as a primary and secondary line of treatment in management of diabetic macular edema. Clin Ophthalmol. 2014;8:653–9.
Conflicts of interest
S. Serizawa, None; K. Ohkoshi, None; Y. Minowa, None; O. Takahashi, None.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Serizawa, S., Ohkoshi, K., Minowa, Y. et al. Prognosis of patients with diabetic macular edema before Japanese approval of anti-vascular endothelial growth factor. Jpn J Ophthalmol 59, 244–251 (2015). https://doi.org/10.1007/s10384-015-0384-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-015-0384-2