Abstract
Purpose
This study aimed to report the visual and anatomical outcomes of intravitreal anti-VEGF treatment for diabetic macular edema (DME) in a real-world clinical setting from Turkey over 36 months.
Methods
This is a retrospective, multicenter (7 sites) study. The medical records of 1072 eyes (both previously treated and naive eyes) of 706 consecutive patients with visual impairment due to center-involving DME treated with intravitreal anti-VEGF injections between April 2007 and February 2017 were reviewed. The eyes were divided into mutually exclusive three groups based on the duration of follow-up (12, 24, or 36 months). Primary outcome measures were changes in visual acuity (VA) and central macular thickness (CMT) from baseline to final visit in each cohort, frequency of visits and intravitreal anti-VEGF injections. As secondary endpoints, VA outcomes were assessed in subgroups stratified by baseline VA [<70 ETDRS letters and ≥70 ETDRS letters] and loading dose status of anti-VEGF injections.
Results
VA increased by a mean of 8.2 letters (12-month cohort, p < 0.001), 5.3 letters (24-month cohort, p < 0.001), and 4.4 letters (36-month cohort, p = 0.017) at final visits. The eyes with <70 VA letters achieved more significant VA improvement at final visits in all cohorts compared with eyes with >70 VA letters (p < 0.001). The mean decreases in CMT from baseline to last visits at 12-, 24-, and 36- month cohorts were −100.5 µm, −107.7 µm, and −114.3 µm, respectively (p < 0.001). The mean number of injections given were 4.6, 2.3, and 1.8 during years 1 to 3, respectively. Patients who received loading dose showed greater VA gains than those who did not in all follow-up cohorts.
Conclusion
Our study revealed that anti-VEGF treatment improved VA and CMT over a follow-up of 36 months. Although these real-life VA outcomes following anti-VEGF therapy for DME were similar to other real-life studies, they were inferior to those noted in randomized controlled trials, mainly due to undertreatment.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Diabetic macular edema (DME) is a leading cause of vision loss in the working-age population of developed countries, affecting approximately 15% of patients with diabetes [1]. Anti-VEGF agents are recommended as first-line therapy for DME, since vascular endothelial growth factor (VEGF) has been identified as one of the major factors contributing to the blood–retinal barrier breakdown. The efficacy and safety of anti-VEGF drugs in patients with DME have already been proven in landmark randomized controlled trials (RCT) [2,3,4,5,6]. In a comparative effectiveness trial, The Diabetic Retinopathy Clinical Research Network (DRCR.net) Protocol T study compared ranibizumab (Lucentis, Novartis, Genentech, South San Francisco, CA, USA), aflibercept (Eylea, Regeneron Pharmaceuticals, Tarrytown, NY, USA), and bevacizumab (Avastin, Genentech, Roche Group) for the treatment of DME. All three anti-VEGF drugs, dosed according to a protocol-specific algorithm, demonstrated similar mean visual gains at 2 years (+ 12.3, + 12.8, and + 10.0 Early Treatment Diabetic Retinopathy Study [ETDRS] letters for ranibizumab, aflibercept, and bevacizumab, respectively) [2]. However, given the restrictions of a clinical trial setting, such as a smaller and selected patient population, prescribed treatment protocols, and shorter observational periods, these conditions in RCTs do not always represent routine practices in real life. Therefore, evaluating the long-term benefit of intravitreal anti-VEGF therapy for DME in a real clinical practice setting may provide further valuable information for treatment decisions.
Several real-life studies have been conducted to assess the consistency between RCTs and real-life settings, in which patients do not meet RCT inclusion criteria due to diversity in systemic or ocular disease severity. These studies have shown that patients receive less frequent injections and have worse visual outcomes in clinical practice compared with participants in landmark trials [7, 8]. However, there are only limited data on the long-term visual and anatomic outcomes of patients with DME treated with anti-VEGF agents. The purpose of this study was to determine the efficacy and treatment frequency of intravitreal anti-VEGF therapy for DME in real clinical practice in Turkey over a three-year period. This is the first large-scale, observational real-world study of anti-VEGF use for DME in Turkey.
Subjects and methods
Study design
This was a retrospective, observational, multicenter study of consecutive patients with center-involving DME treated with intravitreal anti-VEGF injections between April 2007 and February 2017. The Turkish Social Security Institution issued a new ruling in 2017, stating that three doses of bevacizumab should be administered first in patients who require anti-VEGF treatment, with additional anti-VEGF medicines being used only in resistant and/or unresponsive individuals. Therefore, we did not include the patients with DME in this study since 2017. Twenty-six ophthalmologists from 7 ophthalmology centers in Turkey participated in this study. Patients were treated with intravitreal anti-VEGF injections based on the routine practice of the ophthalmologist. Additional adjunctive treatments could be given at any time point according to ophthalmologist’s discretion.
This study was conducted in compliance with the tenets of the Declaration of Helsinki. The study was approved by the Research Ethics Committee of Gülhane Training and Research Hospital.
Study population
The medical records of patients who were either treatment naïve or previously treated with a diagnosis of center-involving DME were reviewed. Inclusion criteria were: (1) age 18 years or older (2) having at least 1 intravitreal anti-VEGF injection between April 2007 and February 2017 (3) best corrected visual acuity (BCVA) ≥ 20 ETDRS letters (Snellen equivalent 20/400), (4) having a medical record of follow-up of at least 12 months. Exclusion criteria were (1) secondary macular edema from other retinal diseases (2) any concomitant ocular disease that could compromise visual acuity (VA) (3) a history of vitreoretinal surgery (4) intravitreal anti-VEGF and/or steroid injection within three months prior to study inclusion (5) Macular laser photocoagulation within three months before inclusion. If both eyes of a patient were eligible, both were included in the analysis.
Data collection
The medical data of patients at baseline and every visit (every 3 months) up to month 36 were collected. Demographics and clinical characteristics, including type, duration, and stage of diabetes mellitus, ocular history, prior treatments, and other systemic medical diseases, were noted at baseline. At each subsequent visit, BCVA (ETDRS letters), central macular thickness (CMT), intravitreal anti-VEGF injections, concomitant treatments for DME, systemic or ocular adverse events (AEs) related to intravitreal anti-VEGF treatment were recorded.
Snellen VA values converted to approximate ETDRS line scores for analysis and calculated as follows: 85 + 50 × log (Snellen fraction) [9].
Optical coherence tomography (OCT) scans were obtained by spectralis OCT (Heidelberg Engineering, Heidelberg, Germany) or Cirrus OCT (Zeiss, Dublin, CA, USA) depending on the device available at each ophthalmology center. CMT values automatically measured by incorporated machine software were recorded.
Endpoints
The patient eyes were divided into three cohorts: eyes who completed 12 months of follow-up (12-month cohort), those who completed 24 months of follow-up (24-month cohort), and those who completed 36 months of follow-up (36-month cohort), with each cohort being mutually exclusive of the others. All outcomes were calculated on each cohort as a whole.
The primary endpoints were changes in BCVA and CMT from baseline to final visit in each cohort and frequency of visits and intravitreal anti-VEGF injections. As secondary endpoints, VA outcomes were assessed in subgroups stratified by baseline VA [< 70 ETDRS letters (Snellen equivalent 20/40) and ≥ 70 ETDRS letters] and loading dose status of anti-VEGF injections. The patients who received 3 initial injections of ranibizumab at intervals of 4 weeks or 5 initial injections of aflibercept at intervals of 4 weeks were recorded into the subgroups of patients with a loading dose.
Statistical analyses
All statistical analyses were performed using the Statistical Package for the Social Science software version 26 (IBM Corp., SPSS for Windows. Armonk, NY, USA). All analyses were performed on the patient-eye level. For individuals treated in both eyes, each eye was treated independently, and the results were recorded into the appropriate cohort. A value of p < 0.05 was considered statistically significant.
Baseline characteristics were summarized with descriptive statistics. Quantitative variables were defined as mean ± standard deviation (SD) and qualitative variables as number (n) and percentages (%). The Shapiro–Wilk test was used to evaluate whether the sample came from a normally distributed population. Paired t-test with Bonferroni correction was used to compare the mean changes in VA and CMT from baseline to final visits in each cohort. After dividing the eyes into subgroups according to baseline VA and initial loading dose status, visual outcomes at final visits were also compared between subgroups within each cohort using the Mann–Whitney U test.
The last observation carried forward method (LCOF) was used to replace missing BCVA and CMT data.
Results
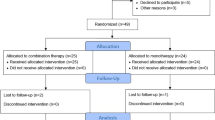
One thousand seventy-two eyes of 706 patients with central-involving DME treated with intravitreal anti-VEGF were included. Of 1072 eyes, there were 495 (46.2%) eyes in the 12-month cohort, 293 (27.3%) eyes in the 24-month cohort, and 284 (26.5%) eyes in the 36-month cohort. Baseline demographics and clinical characteristics of studied eyes are presented in Table 1. The cohorts were similar in terms of demographics and clinical characteristics at inclusion (p > 0.05).
Three hundred sixty-six eyes of 706 (51.8%) patients underwent bilateral treatment during the study period. Overall, the mean age was 60.8 ± 8.5 years and 358 of 706 (50.7%) patients were male. Most patients (93.3%) had type 2 diabetes. The mean duration of diabetes mellitus in patients was 14.5 ± 6.2 years. At baseline, the mean presenting BCVA was 55.6 ± 18.5 ETDRS letters and the mean CMT was 426.5 ± 130.0 µm for the overall patient population. In total, 58.0% of eyes had no previous ocular treatment for visual impairment due to DME.
Visual outcomes
Figure 1 presents the mean monthly changes in ETDRS letters from baseline during follow-up by three cohorts. VA improvements compared to baseline were significant for three cohorts at all follow-ups (p < 0.01). No statistically significant differences in BCVA gain were found between three cohorts at any time point (p > 0.05). In all three cohorts, VA improvement peaked at month 3 (+ 6.0, + 4.7, and + 6.0 ETDRS letters in the 12-, 24-, and 36-month cohorts, respectively, p < 0.001) and continued to improve up to month 12. The visual gains remained relatively stable until month 24 in the 24-month cohort, while visual gains decreased slightly at month 36 in the 36-month cohort. At baseline, the mean BCVA was 55.2 ± 18.2, 55.7 ± 19.9, and 56.0 ± 17.7 ETDRS letters in the 12-, 24-, and 36-month cohorts, respectively (Table 1). The mean increase in BCVA from baseline to month 12 (12-month cohort), month 24 (24-month cohort), and month 36 (36-month cohort) were 8.2 (p < 0.001), 5.3 (p < 0.001), and 4.4 ETDRS letters (p = 0.017), respectively (Fig. 1 and 2).
When stratified by baseline VA, visual outcomes demonstrated ceiling effects, as shown in Fig. 2a–c. In the subgroup of patients with worse baseline VA (< 70 letters), significant VA gains from baseline were demonstrated (+ 11.5, + 9.6, and + 7.7 letters at 12-, 24-, and 36-month, respectively, p < 0.001); while the VA changes from baseline were not statistically significant in the patients with better baseline VA (≥ 70 letters) (+ 0.2, -3.1, and -3.0 letters at 12-, 24-, and 36-month, respectively, p > 0.05). The eyes with < 70 BCVA letters achieved more significant VA improvement at final visits in all cohorts compared with eyes with > 70 BCVA letters (p < 0.001).
Frequency of Anti-VEGF Injections and Clinical Visits
Table 2 indicates the mean number of clinical visits and anti-VEGF injections received in year 1, years 2, and 3 during the study period. The average number of clinical visits and anti-VEGF injections was the highest in the first year (7.4 ± 2.1 visits with 4.6 ± 2.0 injections) and decreased in the second (5.9 ± 2.5 visits with 2.3 ± 1.9 injections) and the third years (5.6 ± 2.3 visits with 1.8 ± 1.8 injections). The patients had on average 13.2 ± 3.8 visits at 24 months and 18.7 ± 5.7 visits at 36 months. The patients received on average 7.1 ± 3.1 injections over 24 months and 8.0 ± 4.2 injections over 36 months.
In the entire cohort, the initial anti-VEGF agent was ranibizumab in 749 (69.9%) eyes, aflibercept in 263 (24.5%) eyes, and bevacizumab in 60 (5.6%) eyes (Table 1). Four hundred twenty-two (422 of 1072, 39.4%) eyes received a loading dose of 3 consecutive injections for ranibizumab and 197 (197 of 1072, 18.4%) received a loading dose of 5 consecutive injections for aflibercept. In total, 619 (57.7%) eyes received a loading dose of anti-VEGF drugs. The subgroup of patients who received loading dose showed greater VA gains compared with those who did not in all follow-up cohorts (Fig. 3a–c). In the 12-month cohort, the visual gain was + 10.3 letters in patients who received loading dose compared to + 4.4 letters in those who did not (p < 0.001, Fig. 3a). Similar VA outcomes were found in 24- and 36-month cohorts (p = 0.09 and p = 0.011, respectively), (Fig. 3b and c).
Change in mean BCVA in patients with and without loading doses from baseline to month 12 (a), month 24 (b), and month 36 (c). Numbers on top of columns show mean change in BCVA letters (SD). *For ranibizumab, 3 initial consecutive injections at 4 weekly intervals; for aflibercept, 5 initial consecutive injections at 4 weekly intervals
Anatomical outcomes
Figure 4 presents the mean monthly changes in CMT values from baseline during follow-up by three cohorts. For all cohorts, a significant reduction in CMT compared to baseline was seen at month 3 (−80.4 µm, −72.1 µm, and −81.0 µm in the 12-, 24-, and 36-month cohorts, respectively, p < 0.001) and continued to mildly decrease through months 12, 24, and 36. There was a significant decrease in CMT compared to baseline at all time points (p < 0.001). No statistically significant differences in CMT reduction were found between 3 cohorts at any time point (p > 0.05).
At baseline, the mean CMT was 416.6 ± 120.5 µm, 433.7 ± 131.8 µm, and 436.2 ± 142.7 µm in the 12-, 24-, and 36-month cohorts, respectively (Table 1). The mean decreases in CMT from baseline to month 12 (12-month cohort), month 24 (24-month cohort), and month 36 (36-month cohort) were −100.5 µm, −107.7 µm, and −114.3 µm, respectively (p < 0.001), (Fig. 4).
Adjunctive therapy
During the study period, additional ocular treatments were required in 655 of 1072 (61.1%) eyes at some time point. Additional treatments were as follows: focal or grid macular laser photocoagulation (n = 177, 16.5%), pan-retinal photocoagulation (PRP) (n = 124, 11.6%), intravitreal dexamethasone implant only (n = 144, 13.4%), focal or grid macular laser photocoagulation followed by intravitreal dexamethasone implant (n = 70, 6.5%), subthreshold laser therapy (n = 50, 4.7%), combined focal or grid macular laser photocoagulation and PRP (n = 43, 4.0%), intravitreal dexamethasone implant followed by pars plana vitrectomy (PPV) (n = 39, 3.6%), and PPV only (n = 8, 0.7%).
Forty-six (5.6%) of 827 eyes which were phakic at the time of inclusion to the study had cataract extraction during the study period. All patients received uneventful phacoemulsification surgery, followed by in-the-bag intraocular lens implantation.
Safety outcomes
Over the 36-month period, ocular AEs were registered in 44 of 1072 (4.1%) eyes. Ocular AEs were increased intraocular pressure (2%, n = 22), vitreous hemorrhage (1.3%, n = 14), glaucoma (0.05%, n = 5), traumatic cataract (0.09%, n = 1), and endophthalmitis (0.09%, n = 1). No cases of retinal tears or detachment were observed during the follow-up.
Eleven of 706 (1.5%) patients suffered systemic AEs that were suspected to be related to anti-VEGF treatment. The systemic AEs were myocardial infarction (0.8%, n = 6) and cerebrovascular accident (0.75%, n = 5).
Discussion
To date, the anti-VEGF injection has become the first-line therapy for center-involved DME in most clinical practices [10]. Nevertheless, due to difficulties in access to healthcare services, higher frequency of co-morbidities, and/or poor adherence to the treatment by older patients, individualized treatment regimens vary substantially in a real-world setting, mainly resulting in fewer injections and fewer clinic visits than those imposed by strictly monitored clinical trials [11, 12]. This current study of Turkey showed that anti-VEGF injections for DME were associated with functional and anatomic improvement in a real-life setting, which was in line with results observed in clinical trials and other real-world studies. The greater improvements in VA were achieved in patients who had a lower baseline VA over three years. It was also observed that the patients who received loading doses showed better VA gains over 36 months of follow-up. However, in the present study, anti-VEGF injections for DME were administered less frequently and less effective than those in clinical trials.
Overall, the visual improvements observed in this study are consistent with real-life studies from other countries, though 12-month BCVA gain (+ 8.2 letters) in the 12-month cohort of our study was better than what has been reported in real-world data [11,12,13,14,15,16]. In the LUMINOUS study, a prospective multicountry analysis of 1063 DME eyes, the country-specific visual gains were between -0.3 and 6.9 letters with an average of 2.2–6.0 injections over one year [13]. In the OCEAN prospective study, which included 1226 eyes in Germany, the mean VA outcome during 12 months was + 4 letters, achieved with a mean of 4.4 injections [12]. In a 1-year Moorfield’s retrospective study of 102 treatment naïve eyes, a mean improvement of 9.9 letters with a mean of 6.9 injections was observed [17]. Our functional results at 12 months were also similar with a slightly fewer number of 4.6 injections. The visual gain was maintained over the second and third year of follow-up in the 24- and 36- month cohorts with mean 7.1 and 8.0 intravitreal injections, respectively (+ 5.3 letters in the 24-month cohort and + 4.4 letters in the 36-month cohort). Consistent with our results, a retrospective study of 3-year outcomes from Thailand showed improvement of 6.8, 4.1, and 3.0 letters with a mean of 6, 8, and 9 injections at 12, 24, and 36 months, respectively [11]. In another real-world BOREAL-DME study conducted at France, Massin et al. reported similar VA gains of 7.4 letters at month 12 and 4.1 letters at month 36 [16].
The real-world DME study outcomes are notably worse than those from RCTs. RCTs have the intensive treatment and follow-up protocol and narrow inclusion and exclusion criteria, leading to better outcomes. In the VISTA&VIVID study, the reported mean gain in BCVA from baseline to 3-year was between + 10.3 and + 11.7 ETDRS letters with 18.1–32 injections [4]. Similar VA improvements were also observed at 36 months in other RCTs, including RESTORE (+ 8 letters) and RISE&RIDE (+ 11 and + 11.4 letters) [6, 18]. The present study suggests a potential role of undertreatment to account for inferior visual outcomes of our DME population. Recent studies have shown that higher visual gains were obtained with more frequent injections in clinical trials than real-world reports [2, 19]. In line with this finding, a retrospective real-world study in the USA has reported that mean VA improvement had a linear relationship with a mean number of anti-VEGF injections at one year, suggesting that intensive treatment strategy in the first year is essential [20]. Another possible explanation for the differences in visual outcomes is varying population characteristics. Chronic DME and previous laser treatment-related structural damage may limit the potential for visual recovery that may account for the differences in long-term results between the studies [3]. Therefore, considering that 42% of our patients had received previous ocular treatments, the chronicity and severity of DME in some of our patients and thus the relative delay in starting anti-VEGF are important factors further contributing to the inferior outcomes.
As mentioned before, the mean number of injections observed in this study and other real-life studies was relatively lower than that observed in other RCTs. In the landmark trials, the patients have received 7–12 injections in the first year, with over 20 injections at two years [4, 18]. In the present study, the patients received 4.6 injections in the first year, 7.1 and 8.0 injections over 24 and 36 months, reflecting general undertreatment. Similarly, in a recently published real-life study with a 4-year duration, Epstein and Amren have reported 4.7, 1.4, 0.7, and 0.9 injections during years 1–4, respectively [21]. A possible explanation for the low number of anti-VEGF injections in our study may be a high burden of health care visits for patients with DME, and it is likely that missed visits or treatments contributed to reduced injection frequency. The patients had on average 7.4, 13.2, and 18.7 visits at 12, 24, and 36 months, which is notably lower than strictly monitored controlled trials [4, 19]. The poor adherence to the treatment in the current study could be attributed to the need for bilateral treatment, lack of education regarding the need for intensive therapy over a period, interference with work schedules, or other associated patient co-morbidities that often contribute to a burden of hospital visits.
Despite undertreatment, substantial and continuous visual and anatomic improvement were observed through 36 months. Patients with low baseline VA (< 70 letters) and those receiving loading doses showed the highest VA gains during the observation period of our study. In contrast, the patients with baseline VA of ≥ 70 ETDRS letters gained less but maintained higher vision than those with lower baseline VA. Considering similar VA outcomes, recently published Protocol V showed that the eyes with very good baseline VA (≥ 80 ETDRS letters) could be managed by observation only instead of starting intravitreal anti-VEGF treatment. Close monitoring rather than proactive treatment may help decrease the burden of clinics and the initial cost of the treatment [22, 23]. Furthermore, results from our study highlight that patients who had a loading dose gained better VA gains than those who did not. Similarly, in a real-world study from Thailand, the authors revealed that the more remarkable mean VA improvement at 12 months was observed in eyes receiving three initial monthly loading injections compared to eyes with non-loading injections [11]. These findings confirm the benefits of receiving loading treatment in a real-life setting.
The incidence of ocular AEs (4.1%) observed in this study was lower than that observed in the RCTs, possibly because of under-reporting in this retrospective observational setting. There was only 1 case of endophthalmitis reported in the study. There were no retinal tears or retinal detachments during the study period. Overall, the safety results observed in this study were consistent with the known safety profile of anti-VEGF agents demonstrated in clinical trials of anti-VEGF therapy in patients with DME [4, 24, 25].
The strength of this current study is that this is the first largest population-based real-world study of anti-VEGF use for DME in Turkey. The study enrolled patients with a variety of demographics and baseline characteristics, including co-morbidities which may have excluded patients from RCTs. Therefore, our study could provide additional information to guide management in patients who are more representative of a typical real-life population. Besides, the multicenter nature of the current study could help to obtain more generalized data. Additionally, the results of this study depend on the sample that consists of 3 mutually exclusive cohorts, each of which differs in terms of both the number of patients and their characteristics. This could allow us to control for any potential impact of the loss to follow-up on visual and anatomic outcomes in this real-life study.
This study has several potential drawbacks, typically associated with its retrospective nature, such as missing data and patients lost to follow-up. Lack of defined treatment criteria and non-standardized VA assessment among study centers could partially account for shortcomings of our real-world data. Furthermore, we did not have information on the course of DME in the individual eyes before the inclusion of the study, which might have also influenced the outcome results. Lastly, the results for three different anti-VEGF agents without considering anti-VEGF switching in the treatment were taken together as a whole. In some studies, such as protocol T, some differences in visual outcomes were found between three drugs, which might influence or explain some of the data in the present study [2].
In conclusion, anti-VEGF therapy for DME over a three-year period was associated with improved functional and anatomic outcomes despite generally low injection numbers in real-life conditions. Baseline VA scores and a loading regimen for anti-VEGF injections seem to be essential factors in achieving better VA outcomes through 3-year follow-up.
References
Sakamoto T, Shimura M, Kitano S, et al (2022) Impact on visual acuity and psychological outcomes of ranibizumab and subsequent treatment for diabetic macular oedema in Japan (MERCURY). Graefes Arch Clin Exp Ophthalmol 260:477–487. https://doi.org/10.1007/s00417-021-05308-8
Wells JA, Glassman AR, Ayala AR, et al (2016) Aflibercept Aflibercept, bevacizumab or ranibizumab for diabetic macular edema: Two-year results from a comparative effectiveness randomized clinical trial. Ophthalmology 123:1351–1359. https://doi.org/10.1016/j.ophtha.2016.02.022
Bressler SB, Glassman AR, Almukhtar T, et al (2016) Five-year outcomes of ranibizumab with prompt or deferred laser versus laser or triamcinolone plus deferred ranibizumab for diabetic macular edema. Am J Ophthalmol 164:57–68. https://doi.org/10.1016/j.ajo.2015.12.025
Heier JS, Korobelnik JF, Brown DM, et al (2016) Intravitreal aflibercept for diabetic macular edema: 148-Week results from the VISTA and VIVID studies. Ophthalmology 123:2376–2385. https://doi.org/10.1016/j.ophtha.2016.07.032
Boyer DS, Nguyen QD, Brown DM, et al (2015) Outcomes with as-needed ranibizumab after initial monthly therapy: Long-term outcomes of the phase III RIDE and RISE trials. Ophthalmology 122:2504–2513. https://doi.org/10.1016/j.ophtha.2015.08.006
Schmidt-Erfurth U, Lang GE, Holz FG, et al (2014) Three-year outcomes of individualized ranibizumab treatment in patients with diabetic macular edema the RESTORE extension study. Ophthalmology 121:1045–1053. https://doi.org/10.1016/j.ophtha.2013.11.041
Kiss S, Liu Y, Brown J, et al (2014) Clinical utilization of anti-vascular endothelial growth-factor agents and patient monitoring in retinal vein occlusion and diabetic macular edema. Clin Ophthalmol 8:1611–1621. https://doi.org/10.2147/OPTH.S60893
VanderBeek BL, Shah N, Parikh PC, Ma L (2016) Trends in the care of diabetic macular edema: Analysis of a national cohort. PLoS ONE 11: e0149450. https://doi.org/10.1371/journal.pone.0149450
Gregori NZ, Feuer W, Rosenfeld PJ (2010) Novel method for analyzing snellen visual acuity measurements. Retina 30:1046–1050. https://doi.org/10.1097/IAE.0b013e3181d87e04
Schmidt-Erfurth U, Garcia-Arumi J, Bandello F, et al (2017) Guidelines for the management of diabetic macular edema by the European Society of Retina Specialists (EURETINA). Ophthalmologica 237:185–222. https://doi.org/10.1159/000458539
Choovuthayakorn J, Phinyo P, Tantraworasin A, et al (2021) Intravitreal anti-vascular endothelial growth factor therapy for diabetic macular edema in clinical practice of single center: three-year outcomes. Ophthalmic Res 64:483–493. https://doi.org/10.1159/000512300
Ziemssen F, Wachtlin J, Kuehlewein L, et al (2018) Intravitreal ranibizumab therapy for diabetic macular edema in routine practice: two-year real-life data from a non-interventional, multicenter study in Germany. Diabetes Ther 9:2271–2289. https://doi.org/10.1007/s13300-018-0513-2
Mitchell P, Sheidow TG, Farah ME, et al (2020) Effectiveness and safety of ranibizumab 0.5 mg in treatment-naive patients with diabetic macular edema: Results from the real-world global LUMINOUS study. PLoS One 15:e0233595. https://doi.org/10.1371/journal.pone.0233595
Korobelnik JF, Daien V, Faure C, et al (2020) Real-world outcomes following 12 months of intravitreal aflibercept monotherapy in patients with diabetic macular edema in France: results from the APOLLON study. Graefes Arch Clin Exp Ophthalmol 258:521–528. https://doi.org/10.1007/s00417-019-04592-9
Hodzic-Hadzibegovic D, Sander BA, Monberg TJ, Larsen M, Lund-Andersen H (2018) Diabetic macular oedema treated with intravitreal anti-vascular endothelial growth factor - 2–4 years follow-up of visual acuity and retinal thickness in 566 patients following Danish national guidelines Acta Ophthalmol 96:267–278. https://doi.org/10.1111/aos.13638
Massin P, Creuzot-Garcher C, Kodjikian L, et al (2019) Real-world outcomes with Ranibizumab 0.5 mg in patients with visual impairment due to diabetic macular edema: 12-month results from the 36-month BOREAL-DME study. Ophthalmic Res 62:101–110. https://doi.org/10.1159/000497406
Lukic M, Williams G, Shalchi Z, et al (2020) Intravitreal aflibercept for diabetic macular oedema: Moorfields' real-world 12-month visual acuity and anatomical outcomes. Eur J Ophthalmol 30:557–562. https://doi.org/10.1177/1120672119833270
Brown DM, Nguyen QD, Marcus DM, et al (2013) Long-term outcomes of ranibizumab therapy for diabetic macular edema: the 36-month results from two phase III trials: RISE and RIDE. Ophthalmology 120:2013–2022. https://doi.org/10.1016/j.ophtha.2013.02.034
Nguyen QD, Brown DM, Marcus DM, et al (2012) Ranibizumab for diabetic macular edema: results from 2 phase III randomized trials: RISE and RIDE. Ophthalmology 119:789–801. https://doi.org/10.1016/j.ophtha.2011.12.039
Ciulla TA, Pollack JS, Williams DF (2021) Visual acuity outcomes and anti-VEGF therapy intensity in diabetic macular oedema: a real-world analysis of 28 658 patient eyes. Br J Ophthalmol 105:216–221. https://doi.org/10.1136/bjophthalmol-2020-315933
Epstein D, Amren U (2018) Long-time outcome in patients treated with ranibizumab for diabetic macular edema: a 4-year study. Retina 38:183–186. https://doi.org/10.1097/IAE.0000000000001501
Hutton DW, Glassman AR, Stein JD, Bressler NM, Sun JK, Network DR (2021) Costs of managing diabetic macular edema with good visual acuity with aflibercept, laser, or observation: DRCR Retina Network Protocol. V Am J Ophthalmol 230:297–302. https://doi.org/10.1016/j.ajo.2021.02.033
Glassman AR, Baker CW, Beaulieu WT, et al (2020) Assessment of the DRCR Retina Network approach to management with initial observation for eyes with center-involved diabetic macular edema and good visual acuity: A secondary analysis of a randomized clinical trial. JAMA Ophthalmol 138:341–349. https://doi.org/10.1001/jamaophthalmol.2019.6035
Mitchell P, Bandello F, Schmidt-Erfurth U, et al (2011) The RESTORE study: ranibizumab monotherapy or combined with laser versus laser monotherapy for diabetic macular edema. Ophthalmology 118:615–625. https://doi.org/10.1016/j.ophtha.2011.01.031
Nguyen QD, Shah SM, Heier JS, et al (2009) Primary end point (six months) results of the ranibizumab for edema of the macula in diabetes (READ-2) study Ophthalmology 116:2175–2181. https://doi.org/10.1016/j.ophtha.2009.04.023
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed equally to this work. All authors have approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethics approval
This study was conducted in compliance with the tenets of the Declaration of Helsinki. The study was approved by the Research Ethics Committee of Gulhane Training and Research Hospital.
Consent to publish
The authors declare and confirm that this research article is original and has neither been published nor been sent or publication in any other journal.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Durukan, A.H., Unlu, N., Onen, M. et al. Anti-vascular endothelial growth factor therapy in diabetic macular edema: real-life outcomes from a multicenter study in Turkey over 36 months. Int Ophthalmol 42, 3777–3787 (2022). https://doi.org/10.1007/s10792-022-02375-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-022-02375-6