Abstract
Purpose
The objective of this study was to evaluate and compare the IOP values in the sitting and supine positions in primary open-angle glaucoma (POAG) and pseudoexfoliation glaucoma (PXG) patients. We also investigated possible relationships between the level of visual field damage and postural IOP change.
Methods
Twenty-nine patients with POAG and 32 patients with PXG were recruited to the study. An Icare PRO tonometer was used to measure IOP in the sitting and supine positions. Intraocular pressure in the sitting position was also measured with a Goldmann applanation tonometer (GAT). Humphrey field analyzer 750 data taken within the previous 3 months were obtained and analyzed.
Results
The mean difference between the GAT and the Icare PRO tonometer readings was 0.12 ± 0.8 mmHg, and the tonometers were in close agreement (r = 0.964; P < 0.0001). The mean Icare PRO IOP in the sitting position was 16.6 ± 3.3 mmHg in the POAG group and 14.9 ± 2.7 mmHg in the PXG group. The average rise was 1.7 ± 1.2 mmHg in the POAG group and 2.9 ± 1.9 mmHg in the PXG group. The difference in IOP between the sitting and supine positions was significant between the groups (P = 0.001). The ∆IOP was negatively correlated with both the mean deviation and the visual field index (P < 0.0001 for both). The ∆IOP and pattern standard deviation were positively correlated (P < 0.0001).
Conclusions
A higher increase in IOP was observed in PXG patients from the sitting to the supine position than in POAG patients. Postural variation in IOP was found to be associated with the severity of visual field damage.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pseudoexfoliation glaucoma (PXG) is the most common secondary open-angle glaucoma. In contrast to primary open-angle glaucoma (POAG), PXG has a more destructive clinical course with higher intraocular pressure (IOP) at onset, faster rate of progression, reduced response to medical therapy, and increased need for surgical intervention [1]. The likelihood of developing glaucomatous optic neuropathy is higher in eyes with PXG than in other forms of glaucoma at comparable IOP values [2]. Significant association of PXG with cerebrovascular and cardiovascular diseases has also been reported [3].
Several studies have investigated the influence of head and body postural change on IOP. Some authors have reported that the difference in posture-induced IOP change was higher in patients with glaucoma than in controls, whereas some other studies disagreed [4, 5]. Studies comparing posture-induced IOP change between patients with advanced glaucoma and those with mild-to-moderate glaucoma reported higher posture-induced IOP increases among patients with advanced glaucoma. Higher IOP variation was also reported in patients with systemic vascular disease than in controls when in the supine position [6].
We hypothesized that posture-induced IOP change in PXG patients may be more pronounced than in POAG patients and may explain the more aggressive clinical course in patients with PXG. To test this hypothesis, we evaluated and compared the IOP values in the sitting and supine positions in POAG and PXG patients. We also investigated the possible relationships between the level of visual field damage and postural IOP change.
Materials and methods
The study was conducted according to the ethical standards stated in the 1964 Declaration of Helsinki and with the approval of the local ethics committee. All patients were fully informed on the procedures, and their written informed consent was obtained before their participation in the study.
This study was conducted at the Cerrahpasa Ophthalmology Glaucoma Clinic between March and May of 2013. A consecutive series of 35 patients with POAG and 32 patients with PXG was recruited. Table 1 lists the patients’ demographic features.
Patient exclusion criteria were a history of ocular surgery, additional ocular disease other than POAG or PXG, more than 6-D of spherical or 3-D of cylindrical refractive error, a narrow angle, and systemic use of beta blockers. If both eyes were suitable, data from the right eye was used for the statistical analysis.
Humphrey Field Analyzer 750 (Carl-Zeiss Meditec, Dublin, CA, USA) data taken within the previous 3 months were obtained and analyzed. The results of the Swedish interactive threshold algorithm (SITA) strategy and the central 30–2 program were used for evaluations. The reliability criteria were false positive and false negative rates of <33 % and fixation losses of <20 %.
Central corneal thickness (CCT), anterior chamber depth (ACD), and axial length were measured in the sitting position with an ultrasound device (US 4000; Nidek, Tokyo, Japan). Primary open-angle glaucoma diagnosis was based on typical glaucomatous optic disc damage (i.e., a vertical cup-to-disc asymmetry between the eyes of 0.2 or more, a vertical cup-to-disc ratio of 0.7 or more, and neuroretinal rim thinning, notching, or nerve fiber layer defects) or glaucomatous visual field defects that were determined by consecutive, repeated abnormal results on visual field testing [i.e., a glaucoma hemifield test that was outside of the normal limits, a pattern standard deviation (PSD) with a P value <0.05, or 3 or more contiguous points with a P value <0.05 (at least one of which had a P value <0.01) in the pattern deviation plot], in the presence of open angles and IOP levels above 21 mmHg.
Pseudoexfoliation glaucoma was diagnosed when slit-lamp findings of pseudoexfoliation material deposition on the anterior lens capsule or at the pupillary border were observed in addition to the above-mentioned POAG criteria.
An Icare PRO tonometer (Icare Finland Oy, Vantaa, Finland) was used to measure the IOP in the sitting and supine positions. This tonometer is based on the rebound measuring principle, in which a very light-weight magnetized probe is used to make a momentary contact with the eye [7]. The probe is thrown against the eye using a coil system. That coil system detects the motion parameters. Advanced software analyzes the deceleration and contact times of the probe while it touches the cornea to calculate the IOP.
Each patient first underwent a detailed ophthalmologic examination that included slit-lamp examination, IOP measurement with Goldmann applanation tonometry (GAT), gonioscopy, and evaluation of the ocular fundus. After a 10-min resting period, IOP in the sitting position was measured with the Icare PRO tonometer. Then, the patient was instructed to lie on a bed. The IOP measurement with the Icare PRO tonometer was repeated 30 min later with the patient in the supine position.
All statistical evaluations were performed using Medcalc (version 12.3.0.0; MedCalc Software, Ostend, Belgium). A paired t-test was used to compare the sitting-position IOP measurements with the GAT and the Icare PRO tonometers and the IOP alterations induced by changes in posture. The Pearson product moment correlation was used to evaluate correlation between the 2 tonometers. The Bland–Altman plot was used to analyze the level of agreement between the tonometers. The Mann–Whitney and Fisher exact tests were used to compare the demographic findings of the 2 groups. Probability values of <0.05 were considered to indicate significance.
Results
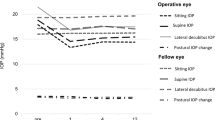
The correlation between the GAT and the Icare PRO tonometer in the sitting position is shown in Fig. 1. The mean difference between the 2 tonometers was 0.12 ± 0.8 mmHg. The Bland–Altman plot in Fig. 2 shows the difference between the GAT and the Icare PRO tonometer. Both tonometers were in close agreement, with a correlation coefficient of 0.964 (P < 0.0001).
The mean Icare PRO IOP in the sitting position was 16.6 ± 3.3 (range: 9.3–21.7 mmHg) for the POAG group and 14.9 ± 2.7 (range: 9.8–20.5 mmHg) for the PXG group (Table 2). In both groups, the mean supine IOPs were higher than the mean sitting IOPs. The average rise was 1.7 ± 1.2 in the POAG group and 2.9 ± 1.9 in the PXG group. The difference in IOP between the sitting and supine positions (∆IOP) was significant in both groups (P = 0.001). The antiglaucoma medications being used by the patients are shown in Table 3. No correlation was found between the number of drops being used and the ∆IOP (r = 0.016; P = 0.89). The number of antiglaucoma medications being used, axial length, ACD, and CCT did not differ between the groups (Table 2). Correlations between the ∆IOP and both the axial length and the ACD were not significant (r = 0.071, P = 0.58 and r = 0.106, P = 0.39, respectively).
The mean MD value of the POAG group (−6.8 ± 6.1) was lower than that of the PXG group (−7.4 ± 6.4), but the difference was not significant (P = 0.34). The mean PSD value of the POAG group (4.5 ± 2.4) was higher than that of the PXG group (4.3 ± 2.2). However, this difference was not significant (P = 0.66). The mean visual field index (VFI) value of the POAG group (76.1 ± 11.8 %) was higher than that of the PXG group (68.2 ± 14.1 %), and this difference was significant (P = 0.02). The ∆IOP and PSD were positively correlated (r = 0.479; P < 0.0001). The ∆IOP was negatively correlated with both the MD and the VFI. The correlation coefficient for the MD (r = −0.591) was higher than that for the VFI (r = −0.778 and P < 0.0001 for both) (Fig. 3).
Discussion
This study has yielded three main findings. First, we observed a good correlation between the GAT and Icare PRO measurements in patients with POAG and in patients with PXG. Second, we observed a higher IOP increase with postural change, from the sitting to the supine position, in patients with PXG than in patients with POAG. Third, we observed a positive correlation between the magnitude of postural IOP change and both the MD (r = 0.591) and the PSD (r = 0.479), and a negative and more forceful correlation between the magnitude of the postural IOP change and the VFI (r = −0.778).
The Icare PRO is a new tonometer that entered clinical practice in 2010. So far, few reports have been published on the correlation between the Icare PRO tonometer and the GAT [8, 9]. Jablonski et al. [8] reported a good correlation (r = 0.951) between the two tonometers in patients with glaucoma. Likewise, Kim et al. [9] reported a good correlation (r = 0.972) between the tonometers. The mean difference between the Icare Pro tonometer and the GAT was reported to be 0.29 mmHg in that study. We obtained similar results: we also found a good correlation (r = 0.964) between the two tonometers, and the mean difference between them was 0.12 mmHg.
We did not observe any significant correlation between the ∆IOP and either the axial length or the ACD. The relationship between the use of antiglaucoma medications and posture-induced IOP changes is debated in the literature. Kiuchi et al. investigated the influence of antiglaucoma drops (timolol maleate, latanoprost, and brinzolamide) on posture-induced IOP changes in patients with normal-tension glaucoma and reported no significant posture-induced IOP change between baseline level and after drop use [10]. They postulated that the mechanism of action underlying posture-induced IOP change differs from the pharmacologic action of antiglaucoma drops. In a more recent study, Steigerwalt et al. [11] reported that latanoprost decreased the posture-induced IOP increase in patients with glaucoma and ocular hypertension. In our study, we did not observe a significant correlation between the number of antiglaucoma drops being used and the posture-induced IOP change. It is very difficult to compare these studies because of the differences in methodology.
The influence of postural changes, mainly shifts from the sitting to the supine position, on IOP was investigated, and a rise in IOP upon lying down was reported in previous studies [12–14]. The level of IOP change is reported to vary according to the presence of glaucoma. The present results confirmed a significant increase in IOP with a shift from the sitting to the supine position in patients with glaucoma. Furthermore, the IOP increase in the PXG patients in our study group was higher than that in the POAG patients. The mean MD and PSD indices did not differ significantly between the POAG and PXG groups. But the VFI was lower in the PXG group than in the POAG group. Therefore, the severity of glaucoma in patients with PXG may be more advanced than in POAG patients. That difference may be an explanation for the higher IOP increase in the PXG patients of our study group. In a study investigating the relationship between the severity of visual field loss and magnitude of IOP elevation with sitting to supine postural change, Hirooka et al. [4] reported higher IOP elevation in eyes with more advanced visual field damage. Similarly, Mizokami et al. [15] reported that the magnitude of IOP elevation was correlated with the severity of both functional and structural glaucomatous damage. The magnitude of IOP elevation was reported in many other studies to be higher in eyes with more advanced glaucomatous damage than in eyes with a lesser degree of glaucomatous damage [13, 16].
Another explanation for the higher posture-induced IOP difference in the PXG group could be the exfoliation component of PXG. Patients with PXG have higher pigmentation and exfoliating materials, which plug the trabecular meshwork. We hypothesize that in the sitting position, those materials go to the inferior trabecular quadrant and other trabecular quadrants may be able to drain the aqueous humor. But in the supine position, those materials may plug all the trabecular quadrants; therefore, the resistance to aqueous humor drainage could be greatly increased. Of course, this hypothesis needs to be proven with future studies. Regarding the facility of aqueous humor outflow, Kozobolis et al. [17] compared the tonographic profile differences between POAG and PXG in the sitting position. They reported temporary disruption of the aqueous humor outflow in patients with POAG and a generalized increase in outflow resistance in patients with PXG. Jakobi et al. [18] reported a significant and partially sustainable IOP decrease in patients with PXG with bimanual trabecular aspiration of the trabecular debris and pigment. We think that these studies favor our hypothesis because they suggest the role of exfoliating materials plugging the trabecular meshwork in the pathogenesis of PXG.
The proposed mechanisms for IOP increase with postural change include increased episcleral venous pressure and consequent choroidal vascular congestion. Friberg et al. [19] measured intraocular and episcleral venous pressures in both the horizontal and the head-down vertical positions and reported a correlation between episcleral venous pressure and posture-induced IOP increase. They concluded that posture-induced IOP increase is closely related to increased episcleral venous pressure in the orbit.
The primary goal in the management of glaucoma is to decrease the IOP level to target the pressure before further damage. Even a small increase in IOP is known to increase the risk of progression in glaucoma patients [20]. Humans usually spend almost one-third of the day in the horizontal position. Therefore, the IOP increase in the supine position may have a role in the progression of glaucoma. In the present study, we observed higher IOP increases in PXG patients in the supine position, which may be one of the reasons for the poorer prognosis in this glaucoma group.
This study has a number of limitations. First, the Icare Pro tonometer cannot measure IOP in oblique positions. Therefore, we measured horizontal IOP in the supine position rather than in the lateral decubitus position, which is the usual sleeping position for most people. Second, we measured the IOP in the awakened state. Therefore, the results may not reflect directly what really happens during sleep. Third, we did not check systemic parameters such as blood pressure and heart rate.
In conclusion, we found higher IOP increase in PXG patients during sitting to supine postural change than in POAG patients. The result implies a potential relationship between the higher IOP increase in the horizontal position and poorer prognosis among patients with PXG than among patients with POAG. Further studies are required to clarify this relationship.
References
Mitchell P, Wang JJ, Hourihan F. The relationship between glaucoma and pseudoexfoliation: the Blue Mountains Eye Study. Arch Ophthalmol. 1999;117:1319–24.
Gillies WE, Brooks AM. The presentation of acute glaucoma in pseudoexfoliation of the lens capsule. Aust N Z J Ophthalmol. 1988;16:101–6.
Mitchell P, Wang JJ, Smith W. Association of pseudoexfoliation syndrome with increased vascular risk. Am J Ophthalmol. 1997;124:685–7.
Hirooka K, Shiraga F. Relationship between postural change of the intraocular pressure and visual field loss in primary open-angle glaucoma. J Glaucoma. 2003;12:379–82.
Sawada A, Yamamoto T. Posture-induced intraocular pressure changes in eyes with open-angle glaucoma, primary angle closure with or without glaucoma medications, and control eyes. Invest Ophthalmol Vis Sci. 2012;53:7631–5.
Williams BI, Peart WS, Letley E. Abnormal intraocular pressure control in systemic hypertension and diabetic mellitus. Br J Ophthalmol. 1980;64:845–51.
Kontiola A. A new electromechanical method for measuring intraocular pressure. Doc Ophthalmol. 1996;93:265–76.
Jablonski KS, Rosentreter A, Gaki S, Lappas A, Dietlein TS. Clinical use of a new position-independent rebound tonometer. J Glaucoma. 2013;22:763–7.
Kim KN, Jeoung JW, Park KH, Lee DS, Kim DM. Effect of lateral decubitus position on intraocular pressure in glaucoma patients with asymmetric visual field loss. Ophthalmology. 2013;120:731–5.
Kiuchi T, Motoyama Y, Oshika T. Influence of ocular hypotensive eyedrops on intraocular pressure fluctuation with postural change in eyes with normal-tension glaucoma. Am J Ophthalmol. 2007;143:693–5.
Steigerwalt RD Jr, Vingolo EM, Plateroti P, Nebbioso M. The effect of latanoprost and influence of changes in body position on patients with glaucoma and ocular hypertension. Eur Rev Med Pharmacol Sci. 2012;16:1723–8.
Tsukahara S, Sasaki T. Postural change of IOP in normal persons and in patients with primary wide open-angle glaucoma and low-tension glaucoma. Br J Ophthalmol. 1984;68:389–92.
Kiuchi T, Motoyama Y, Oshika T. Relationship of progression of visual field damage to postural changes in intraocular pressure in patients with normal-tension glaucoma. Ophthalmology. 2006;113:2150–5.
Prata TS, De Moraes CG, Kanadani FN, Ritch R, Paranhos A Jr. Posture-induced intraocular pressure changes: considerations regarding body position in glaucoma patients. Surv Ophthalmol. 2010;55:445–53.
Mizokami J, Yamada Y, Negi A, Nakamura M. Postural changes in intraocular pressure are associated with asymmetrical retinal nerve fiber thinning in treated patients with primary open-angle glaucoma. Graefes Arch Clin Exp Ophthalmol. 2011;249:879–85.
Aref AA. What happens to glaucoma patients during sleep? Curr Opin Ophthalmol. 2013;24:162–6.
Kozobolis VP, Paschalis EI, Labiris G, Foudoulakis NC, Konstantinidis A, Koukoula SC. Tonography assessment using quantitative and qualitative analysis of the aqueous humor outflow mechanism. Eur J Ophthalmol. 2012;22:726–33.
Jacobi PC, Dietlein TS, Krieglstein GK. Bimanual trabecular aspiration in pseudoexfoliation glaucoma: an alternative in nonfiltering glaucoma surgery. Ophthalmology. 1998;105:886–94.
Friberg TR, Sanborn G, Weinreb RN. Intraocular and episcleral venous pressure increase during inverted posture. Am J Ophthalmol. 1987;103:523–6.
Mayama C, Araie M. Effects of antiglaucoma drugs on blood flow of optic nerve heads and related structures. Jpn J Ophthalmol. 2013;57:133–49.
Conflicts of interest
A. Ozkok, None; N. Tamcelik, None; O. Capar, None; E. Atalay, None.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Ozkok, A., Tamcelik, N., Capar, O. et al. Posture-induced changes in intraocular pressure: comparison of pseudoexfoliation glaucoma and primary open-angle glaucoma. Jpn J Ophthalmol 58, 261–266 (2014). https://doi.org/10.1007/s10384-014-0314-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-014-0314-8