Summary
Osteogenesis imperfecta is a rare hereditary disease mostly caused by mutations impairing collagen synthesis and modification. Recently recessive forms have been described influencing differentiation and activity of osteoblasts and osteoclasts. Most prominent signs are fractures due to low traumata and deformities of long bones and vertebrae. Additional patients can be affected by dwarfism, scoliosis Dentinogenesis imperfecta, deafness and a blueish discoloration of the sclera. During childhood state of the art medical treatment are i.v. bisphosphonates to increase bone mass and to reduce fracture rate. Surgical interventions are needed to treat fractures, to correct deformities and should always be accompanied by physiotherapeutic and rehabilitative interventions.
Zusammenfassung
Die Osteogenesis imperfecta ist eine seltene angeborene Erkrankung, welche in ~ 85% der Fälle auf Mutationen in den Kollagengenen COL1A1/A2 beruht. Folglich kommt es in den Osteoblasten zu einer veränderten Kollagensynthese und -modifikation. In den letzten Jahren ist es gelungen, die genetische Ursache für seltene rezessive Formen, welche nicht nur die Osteoblastenfunktion, sondern auch die Osteoklastenfunktion verändern, zu identifizieren. Das führende klinische Symptom ist die erhöhte Knochenfragilität im Rahmen niedrig-traumatischer Ereignisse und die Deformierung der langen Röhrenknochen. Zusätzlich können eine Dentinogenesis imperfecta, ein Kleinwuchs, eine Schwerhörigkeit und eine „Blau- bzw Grauverfärbung" der Skleren auftreten. Die Therapie basiert auf 3 Ansätzen: Während Kindheit und Jugend ist die intravenöse Gabe von Bisphosphonaten die medikamentöse Therapie der Wahl mit der best verfügbaren Evidenz. Chirurgische / orthopädische Interventionen sind notwendig zur Versorgung komplizierter Frakturen und der elektiven osteosynthetischen Begradigung im Falle schwerer Deformierungen der Extremitäten. Sowohl die medikamentöse Therapie als auch orthopädische Eingriffe sollten kontinuierlich von physiotherapeutischen Maßnahmen begleitet werden, um eine Kräftigung der Muskulatur als wichtigstem osteoanabolen Stimulus und eine langfristige Selbständigkeit der Betroffenen zu gewährleisten.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Recurrent fractures during childhood are rare and should always initiate further diagnostic procedures. It has to be differentiated between diseases affecting mineralization (rickets, X-linked hypophosphatemia and hypophosphatasia) and those affecting bone formation.
Osteogenesis imperfecta (OI) is the most common hereditary form of osteoporosis in childhood with an estimated incidence of 1:20,000 births. In Germany, approximately 5,000 patients with different severities of the disease exist and are in need of medical treatment.
Signs
A reduced amount of bone mass with recurrent fractures due to inadequate traumata is the most common symptom of OI [1]. Fractures and deformities of long bones can be diagnosed by prenatal ultrasound in severe cases during the first/second trimester of pregnancy [2]. In moderate cases, the deformities develop during the first 1–2 years of life and fractures occur as soon as patients start weight bearing on the lower limbs. In mildly affected cases, the patients suffer fractures only in periods of rapid growth, e.g. before puberty.
The phenotype of the patients differ substantially starting with patients who only suffer a few fractures until puberty and those who die during the first few days/weeks of life due to rib fractures and lung hypoplasia [3].
Besides the increased fracture risk, the patients are affected by a disproportioned dwarfism, and some develop a severe kyphoscoliosis during the second decade [4]. This deformation of the spine and thorax can cause pulmonary insufficiency and compression of organs [5].
In severely affected children, the X-rays after birth show fractures of different ages and deformities of long bones as displayed in Fig. 1.
In addition to the skeletal symptoms, patients can be affected by hyperlaxity of joints due to instability of ligaments causing luxations of shoulders and knees. A blueish/greyish discoloration of the sclera is pathognomonic but occurs only in 50 % of patients [6]. Dentinogenesis imperfecta (DI) with brittleness of teeth and an increased risk of caries is prevalent in some patients and some develop deafness later in their life [7]. During the last years, more and more reports about an involvement of the vessels have become available. Some patients suffer from hematoma after minimal traumata, and some are also affected by valve insufficiencies and aneurysmata. It has to be underlined that patients with OI have no mental deficits and that they have to be treated intellectually according to their age and not to their height.
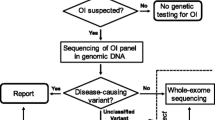
Pathophysiology and genetic background
Patients with OI have a very heterogeneous phenotype which is not completely explained by the genetic background. Formerly, OI was known to be a disease impairing production of collagen 1. Most patients carry heterozygous mutations in COL1A1 and COL1A2 and thus by an autosomal dominant inherited type of OI. But mutations in these genes can only be detected in 85 % of patients with the clinical diagnosis of OI. There are mainly two different types of mutations in COL1A1/2 causing distinct phenotypes. Nonsense mutations typically lead to reduced amounts of normal collagen, whereas glycine substitutions result in the production of structurally impaired collagen and are accompanied by a more severe skeletal phenotype. Among others, formation of collagen triple-helices is delayed in the latter case, leading to posttranslational overmodification.
During the past decade, mutations in more than 10 additional genes have been identified in patients with an OI phenotype. Some recessive OI forms are caused by mutations affecting the posttranslational modification of collagen [8]. Two OI genes will be presented here in more detail because they provided unexpected insights into the pathophysiology of OI.
A recurrent and highly unusual mutation in the 5ʹ-untranslated region of IFITM5, several nucleotides upstream of the start codon of the gene, causes autosomal-dominant OI V [9, 10]. This mutation creates a novel in-frame start codon and therefore adds five amino acids to the N-terminus of the protein. The function of the transmembrane receptor IFITM5, both in the wild-type and in the mutated state, has been only partially elucidated so far, but the protein clearly plays a crucial role for osteoblasts. This is congruent with the clinical hallmarks of OI V like hyperplastic callus formation after fractures and surgeries as well as ossification of the membrana interossea of the forearms [11]. Very recent data on protein expression in patient cell-lines suggest that IFITM5 is functionally connected with SERPINF1, the gene underlying recessive OI type VI [12]. PEDF, the protein encoded by SERPINF1, interacts with the Osteoprotegerin/RANKL-pathway [13]. There is evidence that patients with loss-of-function mutations in SERPINF1 have an increased activation and differentiation of osteoclasts and an increased bone resorption due to decreased production of PEDF (“pigment epithelium derived factor”) [14]. This increased bone resorption could explain that patient with OI VI present with reduced bone mass and brittleness of the skeleton without any other typical signs of OI like blue sclera and DI. Therefore, the phenotype of OI VI may not be caused by an impaired bone formation, but by an increased bone resorption.
Most of the other causative genes are responsible for rare subtypes of the disease. These genes are presented in Table 1.
Therapy
Aim of all interdisciplinary treatment approaches has to be the maximal independency for the individual patient regardless of underlying genotype or socio-economic situation of patient and families. Besides medical treatment, this includes support for the families, especially during the first 2 decades, to include the children into a “normal” life. Education is one of the most important therapies for the patients to give them the possibility to become independent even with their handicap.
The medical treatment is based on three parts: an antiresorptive drug treatment to increase bone mass and to reduce fracture rate and bone pain; orthopedic/surgical procedures to treat fractures and deformities to give the patient the possibility to verticalize; and physiotherapy to teach the patients how they can use their strengthened and straitened bones.
Drug therapy
It is common sense to treat children and adolescents with moderate or severe forms of OI with an antiresorptive therapy. This should be done in patients who suffer two or more low impact fractures per year of the long bones or in patients with multiple vertebral fractures. Currently bisphosphonates are the most frequently used antiresorptive therapy. Bisphosphonates bind to the hydroxyapatite crystals of the bone and inactivate osteoclasts, when this part of the bone is being resorbed due to physiological remodeling processes. With this treatment bone mass of patients increase and consequently the skeleton becomes more stable and the fracture rate decreases. Additionally, most patients report a decrease of chronical bone pain and become physically more active [15]. During childhood, this treatment is much more efficient than after the end of growth. As long as the skeleton develops there is the most potential to influence the bones. In children with compressed or deformed vertebrae, a reshaping of the vertebrae can be reached [16] as demonstrated in Fig. 2a and b. After puberty, the bone turnover decreases and the treatment can be stopped in most of the patients. Some patients report to have chronic back pain later in life and in those adults a restart of a bisphosphonate treatment has to be discussed.
X-rays of the lateral spine of a boy with severe OI. Figure 2A shows the vertebrae with severe compression fractures and deformities at start of i.v. bisphosphonate treatment . Figure 2B presents the x-ray of the lateral spine after 2 years of therapy with a reshaping (increase of height, reduced compression and sclerotic dense lines marking the areas of new bone formation) of the vertebrae
During childhood, the best results have been reached using a cyclic intravenous therapy. Currently no bisphosphonates are approved for children with OI. A therapy is therefore an off-lable use and needs informed consent from the patients and legal representatives. First experiences have been gathered with “pamidronate” which was the first medical treatment for children with OI. Pamidronate has to be given on three consecutive days every 2–4 months depending on the age of the patients and has to be given during an inpatient stay [17].
Since a few years neridronate became available. In placebo controlled trials it has been shown to be effective and can be administered as a single i.v. treatment every 3 months [18]. As it can be given in an outpatient setting in children older than 1 year of age it is the most used bisphosphonate in Germany currently. The dosing is shown in Table 2.
After the first administration of bisphosphonates, ca. 50 % of patients suffer from “flu-like symptoms” with increased body temperature and muscle and skeletal pain for 2–3 days. This reaction is only reported after the first administration and will not recur after further treatment cycles.
No long-term side effects have been reported up till now, but only a relative small number of patients have been treated in the past decade and it is not known if the skeleton will be influenced negatively later in life. There have been great concerns regarding the effect of bisphosphonates on dental health in children. In 2 studies, no negative effects, especially no appearance of osteonecrosis of the jaws, have been reported in children treated with neridronate or pamidronate [19].
In the past, different studies using more convenient oral bisphosphonates have been performed. Those studies demonstrated only a small effect on bone mineral density and failed to have a significant effect on bone pain and fracture rate. In addition they can cause gastrointestinal side effects and the weight adapted dosing is difficult [20].
Recently, new antiresorptive drugs like denosumab became available. This antibody reduces the differentiation and activity of osteoclasts directly and will be resorbed after a few months. Therefore, the unknown long term risks might be lower than those of bisphosphonates which bind to the bone for many years. In addition, denosumab could be injected subcutaneously. First experiences about the use of denosumab in children with OI VI are promising but at the moment such a treatment should only be performed in a clinical trial especially because there is a severe risk of hypocalcemia after the application of denosumab in children with OI [21].
Besides the antiresorptive approach, an osteoanabolic treatment with teriparatide has been investigated in adults with OI. These studies demonstrated an increase of bone mineral density in adults with mostly mild types of OI [22, 23]. This might be an interesting therapeutic approach for adults with moderate or severe forms of OI but it has to be investigated if such an anabolic therapy can increase bone formation or if the osteoblasts produce already as much collagen as possible in these patients with brittle bones. Teriparatide has not been investigated in children yet due to reports of an increased risk of neoplasmas in growing rats treated with teriparatide [24].
A therapy with bisphosphonates is the state of the art therapy for severely affected children with OI but it is an “off-lable” treatment which has to be monitored closely. Bone mineral density scans and X-rays of the lateral spine can be used to document the effect of drug-treatment. The radiographs of the spine should be evaluated using quantitative or semiquantitative scores and should not only describe vertebral deformities [25]. To assess the suppressive effect on osteoclasts different markers of bone resorption (like deoxypyridinoline) can be monitored in the urine. Additionally, the effect of the treatment on the mobility of the patients should be monitored using physiotherapeutic tests, like the “Gross motor function measurement”.
Surgical/Orthopedic treatment
There are two different situations where orthopedic procedures are needed.
-
1.
In the case of fractures without dislocation or when intramedullary rods are in place in most patients a conservative treatment with a cast is sufficient. The aim is to limit pain and to ensure a healing of the fracture without increasing pre-existing deformities. Fracture healing in patients with OI is normal and the immobilization has to be as short as necessary to reduce secondary loss of muscle function and to prevent a secondary osteoporosis [26].
-
2.
The surgical more demanding situation is the correction of deformities in early childhood. Especially in severely affected patients the long bones can be deformed in a way that verticalization of the children is not possible without fractures. In these children a surgery is essential to offer them the chance of weight bearing. During childhood, while the skeleton is still developing and the patient is growing it is state of the art to use telescopic rods [27]. Those rods consist of two parts which can distend during growth. Therefore, re-operations due to a “too short rod” after a few years (as shown in Fig. 3) can be avoided. Telescopic rods can not be used only in the femur and tibiae but also in the humeri (Fig. 4) [28]. As these surgeries are rare and difficult, they should be performed in specialized centers, where surgeons, nurses, and anaesthesists are used to handle children with OI.
Fig. 3
Mobility training
Probably the most important part in an interdisciplinary treatment approach is continuous physiotherapy and muscle training. The patients have to learn how to move during childhood, what healthy children learn as toddlers. To increase their independence, the children need to build up muscle force and have to adapt to their handicap. They have to try new patterns of movement in a “secured environment” with the help of specialized physiotherapists. Every new movement has a risk of new fractures but if the children donʼt try new patterns of locomotion they will never increase their mobility. Therefore, physical training and sometimes psychological support are necessary because the children fear new pain and fractures and need to be motivated to learn new movements.
Besides the muscle training, the use of adequate equipment needs to be trained. The children have to learn how to use a walker or a wheelchair and specially the transfer from the wheelchair in a walker or on a normal chair. They have to learn how to handle stairs, how they are using crutches, and how to take care for their own physical belongings (how to transfer to the toilet etc.).
During childhood recurrent fractures cause a lot of setbacks and it is difficult to motivate patients and families to continue training and not to resign. One new therapeutic approach is the use of a side alternating vibration platform to increase muscle force and muscle function. This approach can be very effective but the exercises performed during vibration have to be performed very precisely and have to be selected individually according to the next motoric steps of the patient [29].
Interdisciplinary approach
OI is a rare disease and it is unrealistic that every medical professional knows about the current therapeutic possibilities. Therefore, it is useful to treat those patients in specialized centers. The perspective of an independent life of the patients depends on the treatment in childhood and on the coordination of different medical, surgical, and therapeutic procedures. An additional problem is that most skeletal problems occur during the period in which the intellectual education takes place. Therefore, not only medical belongings have to be coordinated but also aspects of school and social integration have to be considered.
Another benefit of a centralized therapy is the possibility to improve therapies in the future. Only if many patients are treated in one center, it is possible to recognize differences in the patients and the response to treatment, and to evaluate the incidence of side effects of the treatment. An interdisciplinary team should at least include a pediatrician, physiotherapist, surgeon, social worker, the parents and siblings and further family members, and teachers.
Conflict of interest
None of the authors declare a conflict of interest.
References
Rauch F, Glorieux FH. Osteogenesis imperfecta. Lancet. 2004;363(9418):1377–85.
Schramm T, et al. Prenatal sonographic diagnosis of skeletal dysplasias. Ultrasound Obstet Gynecol. 2009;34(2):160–70.
Pontz BF, Stoss H, Spranger J. Heterogeneity in osteogenesis imperfecta: clinical and morphological findings. Ann N Y Acad Sci. 1988;543:30–9.
Anissipour AK, et al. Behavior of scoliosis during growth in children with osteogenesis imperfecta. J Bone Joint Surg Am. 2014;96(3):237–43.
Karbowski A, Schwitalle M, Eckardt A. [Scoliosis in patients with osteogenesis imperfecta: a federal nation-wide cross-sectional study]. Z Orthop Ihre Grenzgeb. 1999;137(3):219–22.
Kaiser-Kupfer MI, et al. Correlation of ocular rigidity and blue sclerae in osteogenesis imperfecta. Trans Ophthalmol Soc U K. 1985;104(Pt. 2):191–5.
Devaraju D, et al. Dentinogenesis imperfecta type I: a case report with literature review on nomenclature system. J Oral Maxillofac Pathol. 2014;18(Suppl. 1):131–4.
Marini JC, Blissett AR. New genes in bone development: whatʼs new in osteogenesis imperfecta. J Clin Endocrinol Metab. 2013;98:3095–103.
Semler O, et al. A mutation in the 5ʹ-UTR of IFITM5 creates an in-frame start codon and causes autosomal-dominant osteogenesis imperfecta type V with hyperplastic callus. Am J Hum Genet. 2012;91(2):349–57.
Cho TJ, et al. A single recurrent mutation in the 5ʹ-UTR of IFITM5 causes osteogenesis imperfecta type V. Am J Hum Genet. 2012;91(2):343–8.
Glorieux FH, et al. Type V osteogenesis imperfecta: a new form of brittle bone disease. J Bone Miner Res. 2000;15(9):1650–8.
Farber CR, et al. A novel IFITM5 mutation in severe atypical osteogenesis imperfecta type VI impairs osteoblast production of pigment epithelium-derived factor. J Bone Miner Res. 2014;29:1402–11.
Becker J, et al. Exome sequencing identifies truncating mutations in human SERPINF1 in autosomal-recessive osteogenesis imperfecta. Am J Hum Genet. 2011;88(3):362–71.
Rauch F, et al. Lack of circulating pigment epithelium-derived factor is a marker of osteogenesis imperfecta type VI. J Clin Endocrinol Metab. 2012;97(8):E1550–6.
Land C, et al. Effect of intravenous pamidronate therapy on functional abilities and level of ambulation in children with osteogenesis imperfecta. J Pediatr. 2006;148(4):456–60.
Sumnik Z, et al. Effect of pamidronate treatment on vertebral deformity in children with primary osteoporosis. A pilot study using radiographic morphometry. Horm Res. 2004;61(3):137–42.
Glorieux FH, et al. Cyclic administration of pamidronate in children with severe osteogenesis imperfecta. N Engl J Med. 1998;339(14):947–52.
Gatti D, et al. Intravenous neridronate in children with osteogenesis imperfecta: a randomized controlled study. J Bone Miner Res. 2005;20(5):758–63.
Maines E, et al. Children and adolescents treated with neridronate for osteogenesis imperfecta show no evidence of any osteonecrosis of the jaw. J Bone Miner Metab. 2011;30:434–8.
Bishop N, et al. Risedronate in children with osteogenesis imperfecta: a randomised, double-blind, placebo-controlled trial. Lancet. 2013;382(9902):1424–32.
Hoyer-Kuhn H, et al. Two years experience with denosumab for children with Osteogenesis imperfecta type VI. Orphanet J Rare Dis. 2014;9(1):145.
Orwoll ES, et al. Evaluation of teriparatide treatment in adults with osteogenesis imperfecta. J Clin Invest. 2014;124(2):491–8.
Gatti D, et al. Teriparatide treatment in adult patients with osteogenesis imperfecta type I. Calcif Tissue Int. 2013;93(5):448–52.
Vahle JL, et al. Bone neoplasms in F344 rats given teriparatide [rhPTH(1–34)] are dependent on duration of treatment and dose. Toxicol Pathol. 2004;32(4):426–38.
Koerber F, et al. Introduction of a new standardized assessment score of spine morphology in osteogenesis imperfecta. Rofo. 2012;184(8):719–25.
Wirth T, [Osteogenesis imperfecta]. Orthopade. 2012;41(9):773–82; quiz 83–4.
Karbowski A, et al. Experience with Bailey-Dubow rodding in children with osteogenesis imperfecta. Eur J Pediatr Surg. 2000;10(2):119–24.
Ruck J, et al. Fassier-Duval femoral rodding in children with osteogenesis imperfecta receiving bisphosphonates: functional outcomes at one year. J Child Orthop. 2011;5(3):217–24.
Hoyer-Kuhn H, et al. A specialized rehabilitation approach improves mobility in children with osteogenesis imperfecta. J Musculoskelet Neuronal Interact. 2014;14(4):445–53.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hoyer-Kuhn, H., Netzer, C. & Semler, O. Osteogenesis imperfecta: pathophysiology and treatment. Wien Med Wochenschr 165, 278–284 (2015). https://doi.org/10.1007/s10354-015-0361-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10354-015-0361-x