Summary
Background
Our aim was to demonstrate the analgesic efficacy of the bilateral superficial cervical plexus block (BSCPB) combined with bilateral greater occipital nerve block (BGONB) on different sources of pain after thyroid surgery; in terms of pain scores and morphine-PCA consumption in the first 24 h.
Materials and method
Sixty patients were randomized into three groups; Group C (n = 20) to receive management without blocks; Group GS (n = 20), the combination of BSCPB and BGONB; and Group S (n = 20), BSCPB alone. Levobupivacaine of 0.25 % (15 ml (each side) for BSCPB; 5 ml (each side) BGONB) was used for nerve blocks. All patients received morphine-PCA for the first 24 h postoperatively. In all, 0 h, 1 h, 2 h, 4 h, 6 h, 12 h, and 24 h were the measurement times for incision pain at rest, pain on swallowing, headache, and posterior neck pain scores (VAS) and PONV. Requirement for rescue analgesics and 24 h morphine consumption were recorded.
Results
Incision pain scores at rest and on swallowing was lower in Groups GS and S (p < 0.001). Posterior neck pain scores were lower in Group GS (p < 0.001). Headache was similar in all groups, but the number of patients with pain scores VAS > 3 was lower in Group GS (p < 0.001). In Groups GS and S 24 h morphine consumption was lower, compared to Group C (p < 0.001). PONV and rescue analgesic use were similar.
Conclusion
The combination of three-injection technique BSCPB with BGONB performed before surgical incision by using 0.25 % levobupivacaine, significantly reduced incision pain at rest, incision pain on swallowing, headache and posterior neck pain after thyroid surgery, while reducing morphine consumption in 24 h postoperatively.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The thyroid surgery is known to result in moderate and short-stay pain in the postoperative period [1, 2]. However, post-thyroidectomy pain was reported to be significant in the first 24 h, resulting in visual analogue scale (VAS) scores over 6 [3, 4]. There are many published trials addressing post-thyroidectomy pain, in terms of the types and doses of analgesics used and their side effects [5–9]. Since the superficial component of the thyroid surgery is more pronounced, the most common technique of choice for analgesia seems to be the regional techniques. Suh et al. [7] and Steffen et al. [10] reported that bilateral superficial cervical plexus block (BSCPB) proved to be effective in patients undergoing thyroid surgery, however, the authors stated that the VAS scores were still over 4. Similarly, Dieudonne et al. [4] also reported that BSCPB effectively reduced pain scores when compared to their control group, but they also stated that this block was not sufficient for optimal pain relief after thyroid surgery, when used alone.
The sources of pain after thyroid surgery may vary. Incision pain at rest and on swallowing are the main sources of pain. In addition to these, the position of the head and neck during surgery may lead to headache and posterior neck pain [8, 9]. BSCPB has proven to be effective in reducing incision pain at rest and on swallowing, while bilateral greater occipital nerve block (BGONB) has been shown to be effective in reducing the intensity of headache and posterior neck pain [1, 7, 8, 10]. Suh et al. [7] investigated different sources of pain individually, and stated that BSCPB could be supported by a regular analgesic protocol, which they did not employed in their study. We aimed to investigate the impact of the combination of BSCPB and BGONB for patients undergoing thyroid surgery, by comparing this combination with an analgesic regimen without blocks and with the employment of BSCPB alone.
We tested the hypothesis that ‘BSCPB effectively reduces the impact of different sources of pain after thyroid surgery, with less morphine consumption in 24 h, when combined with BGONB’.
Materials and method
This randomized, double-blinded, prospective study was approved by Ethical Committee of Duzce University School of Medicine, Duzce, on 14 January 2013 with number 2013/353. Written informed consent was obtained from each patient enrolled for the study. The patients were informed about the use of VAS and the patient-controlled-analgesia (PCA) device the day before surgery.
The patients who had medical therapy including opioids, corticosteroids, and analgesics were not included. In addition, thyroidectomy with parathyroidectomy, coagulation disorders, hypersensitivity to paracetamol, NSAIDs, and local anesthetics, immune disorders, anatomical-developmental pathologies or previous operations in head and neck, morbid obesity, difficulty in cooperation (language problems, dementia, and mental state), and disapproval of being a participant to the study, were the noninclusion criteria. The patients who had predicted invasive carcinoma, cervical lymph node dissection, or postoperative hematoma were excluded from data analysis.
Sixty ASA I-II patients, at age of 18–75 years, scheduled for elective thyroid surgery were enrolled in the study and randomized into three groups (1:1:1) by using computer generated random number list. The interventions were performed by the anesthesiologists who did not participate to the follow-up period and collection of data.
On arrival to the operating room, after routine monitoring by electrocardiography (ECG), noninvasive blood pressure (NIBP), and pulse oximetry; anesthesia was induced by using 1–2 mg/kg propofol and 1 mcg/kg fentanyl. Rocuronium of 0.6 mg/kg was used for neuromuscular blockade due to its short duration of action. Anesthesia was maintained by using 2 % sevoflurane in air: O2 (1:1) and 0.05 mcg/kg/min intravenous remifentanil infusion. Neuromuscular blockade was not maintained throughout the procedure, none of our patients received additional dose of rocuronium, for the surgeons to monitor the integrity of recurrent laryngeal nerve. Anesthetics were titrated according to hemodynamic parameters. Fentanyl of 1 mcg/kg was administered when mean arterial blood pressure increased more than 20 % of the baseline. Neostigmin of 0.05 mg/kg with 0.01 mg/kg atropin were used for the reversal of neuromuscular blockade to prevent any residual effect. All patients received 10 mg intravenous (i.v.) metoclopramide and 1 mg/kg methylprednisolone as our routine practice in head and neck surgeries.
The control group received an established analgesic protocol. We administered 1 g i.v. paracetamol every 6 h, starting with the first dose intraoperatively (30 min before the end of the surgery); and 75 mg intramuscular (im) diclophenac sodium every 12 h postoperatively. In addition, we used mophine-PCA for the first 24 h after surgery.
Under general anesthesia, after endotracheal intubation the blocks were performed. For BSCPB; the head turned towards opposite side. With aseptic precautions, sternocleidomastoid (SCM) muscle was identified. A 23-gauge short beveled needle inserted to the midpoint of the posterior border of SCM, to the depth of 0.5 cm to inject 0.25 % levobupivacaine 5 ml to each three-injection site (three-injection technique) (15 ml for each side of the neck) by redirecting the needle to cephalad-transverse-caudal along posterior border of SCM with negative aspiration. Three-injections provided the blockade of greater auricular nerve, transverse cervical, and supraclavicular nerves. We used 5 ml local anesthetic for each site to a depth of 0.5 cm under the cervical fascia, as it is recommended for the performance of the technique [11]. The needle was inserted to a depth not more than 0.5 cm to avoid subarachnoid or vertebral artery injection [1, 12].
The patients allocated to Group GS received bilateral GON block in combination with BSCPB. The occipital artery was palpable at 2 cm lateral and 1 cm inferior to the greater occipital protuberance. The 23-gauge needle was inserted medial to the artery to a depth to meet periost. To each side, 5 ml 0.25 % levobupivacaine was injected. Pressure was applied for a few minutes to ensure hemostasis.
All the blocks were performed by the same anesthesiologists and all the operations were performed by the same surgical team. After the blocks were performed, the patient was placed in a supine position with the extension of the neck. A collar incision was made and carried down through the subcutaneous tissue and platysma muscle. Superior and inferior flaps were developed between hyoid bone and sternum. The strap muscles were divided vertically in the midline and retracted laterally. The thyroid lobe was bluntly dissected free from its investing fascia and rotated medially. The middle thyroid vein and the superior pole vessels were ligated adjacent to the thyroid lobe. Recurrent laryngeal nerve was dissected in the tracheoesophageal groove. The nerve was gently unroofed from surrounding tissue. Once the nerve and parathyroid glands were identified and preserved, the thyroid lobe was removed from its tracheal attachments by dividing the ligament of Berry. Throughout the operations in all of our patients, Nerve Integrity Monitoring (NIM-Response® 2.0, Medtronic Xomed, Jacksonville, FL, USA) system was used in order to monitor the recurrent laryngeal nerve. We used Medtronic Xomed Nerve Integrity Monitor Standard Reinforced Electromyography Endotracheal Tube (Jacksonville, FL, USA) for endotracheal intubations. The tube was positioned in such a way that the middle parts of the exposed electrodes made direct contact with the true vocal cords. The stimulation level was set at 0.8 mA. The recurrent laryngeal nerve was stimulated pre- and postdissection of thyroid gland to confirm integrity. The superior laryngeal nerve was not stimulated.
The patients received morphine-PCA to be used for the first 24 h postoperatively. The PCA was programmed to deliver 1 mg bolus on demand, no basal infusion with a lock-out interval of 6 min. Rescue medication was provided by 1 g intravenous paracetamol ensuring that maximum daily dose was not exceeded.
The intensity of pain after surgery was measured by visual analogue scale (VAS) within 0–10; where no pain: 0 and worst pain imaginable: 10. Incision pain score at rest and on swallowing, headache, and posterior neck pain scores were asked individually at 0, 1, 2, 4, 6, 12, and 24 h in the first 24 h after surgery. At these same measurement times postoperative nausea and vomiting (PONV) was also asked and recorded.
Statistical analysis
Data analysis was performed by using Statistical Package for Social Sciences (SPSS) for Windows, version 11.5 (SPSS Inc., Chicago, IL, United States). Kolmogorov–Smirnov test was used to determine the normal distribution of the continuous and discrete numerical variables. Levene test was used for the evaluation of homogeneity of variances. The significance of the differences between groups, in terms of variables that distributed normally and where the variances were homogeneous, were assessed by using one-way ANOVA. The significance of the differences between groups, in terms of variables that distributed not normally and where the variances were not homogeneous, were evaluated by Mann–Whitney U test when the number of independent groups were two, otherwise, Kruskal–Wallis test was applied when the number of independent groups was more than two. When the p value of Kruskal–Wallis test were statistically significant, Conover’s non-parametric multiple comparison test was used to show which group was different. Nominal variables were analyzed by Pearson’s chi-square test. The change in pain scores with time within each group was shown by Friedman test. Where the result of Friedman test was significant, the time at which the change revealed this significance was assessed by using Wilcoxon signed-rank test. A p value less than 0.05 was considered statistically significant. But, all possible multiple comparisons, the Bonferroni correction was applied for controlling Type I error.
Sample size was estimated according to the primary outcome parameter, which was morphine-PCA consumption in 24 h. From a pilot study, the sample size was estimated to be at least 13 patients for each group to define significance with 95 % power with α-error of 0.05.
Results
Ninety-six patients scheduled for thyroid surgery were assessed for eligibility. Sixty patients were recruited and randomized into three groups. Fifty-nine patient’s data were analyzed, one patient developed hematoma after surgery and dropped out from follow-up (Fig. 1). Demographic data and ASA classifications of patients; and durations of surgery were similar in all groups (Table 1).
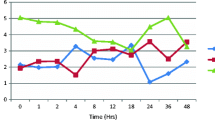
Incision pain scores at rest and on swallowing, immediately after surgery (0 h) were significantly lower in Groups GS and S, compared to Group C (Table 2). The gradual decline in 24 h period is shown in Fig. 2a, 2b. The number of patients, who described incision pain scores at rest and on swallowing as VAS ≥ 6 at any time in the first 24 h postoperatively, was significantly less in Groups GS and S, compared to Group C (Table 3).
Incision pain scores at rest (a), incision pain on swallowing (b), headache (c), and posterior neck pain (d) VAS scores in 24 h postoperatively. * Difference between groups is significant at 0 h (p < 0.001). a # The gradual decline in VAS score of incision pain at rest became significant at 6, 12, and 24 h in Groups C, S and GS, respectively; compared to 0 h. b # The gradual decline in VAS score of incision pain on swallowing became significant at 12 h in Groups C and S; compared to 0 h. c # The gradual decline in VAS score of headache became significant at 12 h in Group C; compared to 0 h. d # The gradual decline in VAS score of posterior neck pain became significant at 12 h and 24 h in Groups C and S, respectively; compared to 0 h
VAS scores of headache immediately after surgery (0 h) were similar in all three groups (Table 2). The gradual decline in 24 h period is shown in Fig. 2c. The number of patients, whose headache was VAS > 3 at any time in the first 24 h postoperatively, was significantly less in Group GS (Table 3). None of the patient’s headache was VAS ≥ 6 in 24 h in Group GS (Table 3).
Posterior neck pain scores, immediately after surgery (0 h) were significantly lower in Group GS, whereas these pain scores were similar in Groups C and S (Table 2). The gradual decline in 24 h period is shown in Fig. 2d. The number of patients whose posterior neck pain was VAS > 3 at any time in the first 24 h postoperatively, was significantly less in Group GS (Table 3). None of the patient’s posterior neck pain was VAS ≥ 6 in 24 h in Group GS (Table 3).
The total morphine-PCA consumption in the first 24 h after surgery was significantly higher in Group C, whereas similar in Groups GS and S (Fig. 3). The requirement for rescue analgesics and postoperative nausea and vomiting were similar in all three groups (Table 4).
Discussion
In our study, we demonstrated that the bilateral superficial cervical plexus block combined with bilateral greater occipital nerve block provided effective analgesia for different sources of pain in patients undergoing thyroid surgery, while reducing the morphine consumption in 24 h after surgery. This result was obtained by the employment of the 3-injection technique for the BSCPB, with the use of 15 ml 0.25 % levobupivacaine, 5 ml for each of the three injection sites; and with the use of 5 ml 0.25 % levobupivacaine for each side of the BGONB.
The use of superficial cervical plexus block in thyroid surgery is a well known technique, which have contradictory results in terms of effectiveness in analgesia. The contradictory results mainly depend on the technique of choice, the correctness of the performance of the technique, assessment of the success of the block, the concentration of the local anesthetics used, adjuvant agents used in combination with local anesthetics, and depth of injections [1].Two-injection and three-injection SCPB has been recommended as the techniques of choice, however, the data has generally been in favor of 3-injection technique [4, 7]. This technique includes a horizontal injection to block the transverse cervical nerves, which were reported to be the major nerve fibers to be blocked for a successful SCPB [7, 11, 14]. This difference between two techniques may have led the difference between trials. The depth at which the local anesthetics administered has also been a concern, because subcutaneous injections were previously reported to have a possible negative impact on the efficacy of the blocks, due to insufficient spread beyond the subcutaneous layer [13]. Thus, this way of local anesthetic administration may have led to difference between trials [4, 14]. In several studies, the volume of local anesthetics injected to each site of the block were in different amounts, sparing the larger volume for transverse cervical nerves and smaller for greater auricular nerve and supraclavicular nerves; which may also have affected the impact of this block [1, 6, 7]. However, with all the approaches for BSCPB, there are several trials reporting both positive and negative results, in terms of its analgesic efficacy [4, 7, 9, 14]. We preferred 3-injection technique to provide the blockade of transverse cervical nerves and used levobupivacaine because of the less toxic effect compared to bupivacaine. We used the concentration of 0.25 % as it is recommended for the superficial cervical plexus block, which is composed of sensory nerves [11]. We administered local anesthetic 5 ml for each injection site under the cervical fascia, to a depth of 0.5 cm as recommended for this procedure [11]. Larger equal amounts of local anesthetic injections, which were applied under the cervical fascia, to each of the three-injection sites may have improved the impact of our blocks performed with low concentration of local anesthetic.
In previous studies, pain after thyroid surgery was mostly examined from a general aspect and the different sources were mostly not questioned individually. However, Suh et al. [7], recorded VAS scores of postoperative pain, in terms of its different sources, which were suggested to occur after thyroid surgery [9]. The authors addressed incision pain at rest, incision pain on swallowing, headache, and posterior neck pain postoperatively; and compared the single use of BSCPB with its combination with bilateral deep cervical plexus block. They also had a control group, in which patients did not receive any blocks. All of their patients including the control group, received analgesic medication when VAS scores were over 6 [7]. Our control group revealed comparable pain scores with the control group of this study, in terms of incision pain at rest, headache, and posterior neck pain. However, incision pain on swallowing was lower in our study. This difference may be due to the beneficial effect of our scheduled regular analgesic medication we used in our study. In report by Suh et al., they stated that patients in all of their groups had higher pain scores compared to previous studies. They also explained this, with the lack of regular analgesic use in the postoperative period [7]. Despite the lower pain scores in our control group compared to this previous study, the patients who constituted our control still had higher VAS scores and morphine consumption in 24 h postoperatively, when compared to our other two groups, in which patients received blocks. In addition, incision pain scores at rest and on swallowing were over 6 in significantly more patients in our control group, and this data supports the employment of blocks in postoperative pain management of thyroid surgery.
In our study, the patients who received BSCPB alone, had incision pain scores at rest and on swallowing lower than the patients in Suh et al.'s study. This result may have been due to our analgesic protocol including morphine-PCA for the first 24 h postoperatively. Headache and posterior neck pain scores in these patients who received this block alone, seemed to be comparable with our study and had a tendency to be low. Suh et al. explained this tendency with the favorable effect of the blocks on these components of pain, which they suggested to be a kind of referred pain. However, this tendency was also observed in their control group. So, this result may not be actually related to the effect of their blocks. As previously been reported by Han et al. [8] and Eti et al. [9], the position of the head and neck during surgery for exposure, may be the source of pain, due to the compression and entrapment of the greater occipital nerve. Han et al. used BGONB to eliminate headache and posterior neck pain after thyroidectomy; and demonstrated that BGONB had a significant effect on these sources of pain [8]. However, they did not address incision pain at rest or on swallowing, which are the main components of pain after thyroid surgery. In our study, we combined these two blocks in order to reduce the impact of these different sources of pain after thyroid surgery.
We demonstrated that BSCPB had a significant effect on the incision pain at rest and on swallowing, while BGONB had a significant effect on posterior neck pain. Although the scores of headache were not significantly different in patients receiving the combination, the number of patients describing VAS > 3 were significantly lower in this group. This result reveals that the combination of these two blocks was more effective than BSCPB alone in analgesic management of thyroid surgery.
The 24 h morphine-PCA consumptions were similar in our patients who received BSCPB alone or in combination with BGONB; and significantly lower when compared to the control group.
The number of patients who had PONV in our control group, although not statistically significant, were clinically relevant. The less number of patients with PONV in groups receiving blocks can be suggested as a clinical improvement led by reduced morphine consumption provided with blocks.
Limitations
In our study, all the blocks were performed after induction of general anesthesia and endotracheal intubation, prior to surgical incision. This performance was advantageous in terms of patient and anesthetist’s comfort and ease of application. Thus, it was not possible to evaluate the success of these blocks. However, the patients in our control group had significantly higher pain scores and higher morphine requirement, compared to patients receiving either BSCPB alone or in combination with BGONB. Thus, we thought that the blocks were successful in our patients.
These peripheral blocks did not last long to result any significant delay in the operating room. However, it should be kept in mind that any peripheral nerve block may become a burden for surgeons, if the anesthesia team is inexperienced. Since this was not planned as a primary or secondary outcome parameter in our study, we did not record the duration of our block performance.
On the other hand, we cannot make any suggestion about the durations of blocks, because we did not have a record of the exact time of first activation of morphine-PCA. We could not obtain data about the exact time of demands for bolus doses from our PCA device, so we cannot provide a timing diagram, which may have provided data on block durations.
In previous studies, the intraoperative anesthetic agent and opioid requirements were evaluated as well. We did not include this data as an outcome parameter, so we cannot make any suggestion on that kind of effect.
Metoclopramid and methylprednisolone were administered to all patients as hospital policy. As we used these medications in all patients, we thought that this protocol did not affect the reliability of our evaluation. On the other hand, sample size was also not sufficient to describe a significant effect on PONV, as the sample size was not estimated according to this parameter. The incidence of PONV after thyroid surgery and its prevention via decreasing opioid requirement by the application of peripheral nerve blocks, should be investigated with larger patient groups.
Our control group received a detailed multimodal analgesic plan and did not receive placebo instead. In the light of previously reported data, it may have been considered unethical to use placebo in any kind of surgery or intervention, which may result in pain.
Conclusion
In conclusion, we demonstrated that the combination of BSCPB and BGONB, which was applied before surgical incision, reduced incision pain at rest, incision pain on swallowing, headache, and posterior neck pain effectively after thyroid surgery, while reducing morphine-PCA consumption in the first 24 h. This effect was obtained by using 15 ml 0.25 % levobupivacaine to each side of the neck; 5 ml injection under the cervical fascia to each three injection site of SCPB; and 5 ml 0.25 % levobupivacaine for each side of GONB. This approach can be used both for reducing pain scores and decreasing the analgesic consumption after thyroid surgery.
References
Andrieu G, Amrouni H, Robin E, Carnaille B, Wattier JM, Pattou F, et.al. Analgesic efficacy of bilateral superficial cervical plexus block administered before thyroid surgery under general anaesthesia. Br J Anaesth. 2007;99(4):561–6.
Motamed C, Merle JC, Yakhou L, Combes X, Dumerat M, Vodinh J, et.al. Intraoperative i.v. morphine reduces pain scores and length of stay in the post anaesthetic care unit after thyroidectomy. Br J Anaesth. 2004;93(2):306–7.
Gozal Y, Shapira SC, Gozal D, Magora F. Bupivacaine wound infiltration in thyroid surgery reduces postoperative pain and opioid demand. Acta Anaesth Scand. 1994;38:813–5.
Dieudonne N, Gomola A, Bonnichon P, Ozier YM. Prevention of postoperative pain after thyroid surgery: a double blind randomized study of bilateral superficial cervical plexus blocks. Anesth Analg. 2001;92:1538–42.
Aunac S, Carlier M, Singelyn F, De Kock M. The analgesic efficacy of bilateral combined superficial and deep cervical plexus block administered before thyroid surgery under general anesthesia. Anesth Analg. 2002;95(3):746–50.
Shih ML, Duh QY, Hsieh CB, Liu YC, Lu CH, Wong CS, Yu JC, Yeh CC. Bilateral superficial cervical plexus block combined with general anesthesia administered in thyroid operations. World J Surg. 2010;34:2338–43.
Suh YJ, Kim YS, In JH, Joo JD, Jeon YS, Kim HK. Comparison of analgesic efficacy between bilateral Superficial and combined (superficial and deep) cervical plexus block administered before thyroid surgery. Eur J Anaesthesiol. 2009;26:1043–47.
Han DW, Koo BN, Chung WY. Park CS, Kim SY, Palmer P, et.al. Preoperative greater occipital nerve block in total thyroidectomy patients can reduce postoperative occipital headache and posterior neck pain. Thyroid. 2006; 16(6):599–603.
Eti Z, Irmak P, Gulluoglu BM, Manukyan MN, Gogüs FY. Does bilateral superficial cervical plexus block decrease analgesic requirement after thyroid surgery? Anesth Analg. 2006;102:1174–6.
Steffen T, Warschkow R, Brändle M, Tarantino I, Clerici T. Randomized controlled trial of bilateral superficial cervical plexus block versus placebo in thyroid surgery. Br J Surg. 2010;97:1000–6.
Hadzic A. Section 2. Nerve stimulator and surface-based nerve block techniques. Chapter 11. Cervical plexus block. In: Hadzic A, editor. Hadzic’s peripheral nerve blocks and anatomy for ultrasound-guided regional anesthesia. 2 ed. China: McGraw-Hill; 2011. pp. 139–48.
Kesisoglou I, Papavramidis TS, Michalopoulos N, Ioannidis K, Trikoupi A, Sapalidis K, et al. Superfıcıal selectıve cervıcal plexus block followıng total thyroıdectomy: a randomızed trıal. Head Neck. 2010;32(8):984–8.
1Herbland A, Cantini O, Reynier P, Valat P, Jougon J, Arimone Y, et al. The bilateral superficial cervical plexus block with 0.75 % ropivacaine administered before or after surgery does not prevent postoperative pain after total thyroidectomy. Reg Anesth Pain Med. 2006; 31(1):34–9.
Pandit JJ, Dutta D, Morris JF. Spread of injectate with superficial cervicalplexus block in humans: an anatomical study. Br J Anaesth. 2003;91:733–5.
Acknowledgements
No funding and no conflicts of interest. We appreciate the work for statistical analysis of Salih Ergocen, MSc.
Funding
None.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
The study was held in ‘Turkish Ministry of Health Ankara Dişkapi Yildirim Beyazit Research and Teaching Hospital, Anesthesiology and Reanimation Clinic, Ankara, Turkey’, while Dr. Filiz Uzumcugil was working there. Dr. Uzumcugil presently works in Hacettepe University School of Medicine, Department of Anesthesiology and Reanimation as an Instructor.
Rights and permissions
About this article
Cite this article
Kılınçkan, F., Uzumcugil, F., Sayın, M. et al. Bilateral superficial cervical plexus block combined with bilateral greater occipital nerve block reduces the impact of different sources of pain after thyroid surgery with less consumption of morphine-PCA: a randomized trial. Eur Surg 47, 181–187 (2015). https://doi.org/10.1007/s10353-015-0322-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10353-015-0322-z