Abstract
Thyroid surgery may cause severe postoperative pain and discomfort for patients. Superficial cervical plexus block (SCPB) is one of the regional anesthesia techniques that can provide postoperative analgesia for thyroid surgery. The purpose of this study was to evaluate analgesic effect of ultrasound (US) guided SCPB in patients undergoing thyroid surgery. Fifty ASA I–II patients, aged 20–60, were included in this single blinded study. In a randomized and prospective manner patients were allocated to either SCPB or control group. Bilateral SCPB was performed preoperatively under US guidance using 10 ml 0.25 % bupivacaine for each side. Postoperative analgesia was provided with patient-controlled analgesia method with morphine intravenous. Primary outcome measure was postoperative opioid consumption and analyzed using Mann–Whitney U test. Secondary outcome measures were comparison of opioid side effects like nausea and vomiting and analyzed using Chi square test. VAS scores for pain at postoperative 1st, 6th, 12th, and 24th h were similar in SCPB and control groups (Median VAS values were 2.5, 3, 2, 0 and 3.5, 3, 2, 0 respectively). Postoperative morphine consumption was lower in SCPB group compared to control group at postoperative 6th, 12th, and 24th h (Median doses of morphine consumption were 4, 8, 9 and 5, 9, 11 mg respectively) (P < 0.05). Eight patients in the control group and six patients in the SCBP group had vomiting. Seven patients in the SCPB and none in the control group had hoarseness. Our study has shown that US guided SCPB has a significant analgesic effect in patients undergoing thyroid surgery. Further studies are required to search for the optimal LA dose during US guided SCPB.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Surgery of the thyroid gland is one of the most commonly performed operations for either benign or malignant pathologies. Thyroid surgery is a quite painful procedure performed in a sensitive skin area of the human body. Unless pain is treated adequately thyroid surgery may cause severe postoperative pain and discomfort for the patients [1]. Opioids used to treat postoperative pain cause potential side effects like nausea and vomiting that contributes to patient discomfort and even delayed discharge from the hospital.
Regional techniques may help to alleviate postoperative pain and reduce systemic analgesic requirement. Cervical plexus block and wound infiltration techniques are the main regional techniques that can be performed to provide postoperative analgesia following thyroid surgery. The study of Suh et al. [1] has shown that superficial cervical plexus block (SCPB) alone is a more effective technique than combining superficial and deep cervical plexus blocks. Current literature regarding analgesic effect of SCPB on postoperative pain is controversial [2–5]. While some studies claim no analgesic effect of cervical plexus block; some others claim that thyroid surgery can be performed awake under cervical plexus block [2, 3, 6, 7].
Ultrasound (US) guidance during regional anesthesia practices has been a revolutionary advancement to improve success and safety of regional anesthesia [8, 9]. Most of the regional techniques have been re-evaluated following the introduction of US into regional anesthesia practice.
To the best of our knowledge the analgesic effect of US guided SCPB in patients undergoing thyroid surgery has not been reported yet. The aim of this study was to evaluate the analgesic effect of US guided SCPB in patients undergoing elective thyroid surgery. We aimed to compare primarily postoperative opioid requirements in patients undergoing thyroid surgery. Secondary end points were to compare opioid related side effects; postoperative nausea and vomiting.
2 Methods
After Kocaeli city clinical research ethical committee permission and informed written patients’ consent, 50 patients ASA physical status I–II, aged 20–60 years and scheduled for elective thyroid surgery under general anesthesia were included into this study.
Exclusion criteria were known allergy to any of the study drugs, previous thyroid surgery, thyroid surgery in combination with neck dissection or sternotomy, pregnancy, recent use of opioids, corticosteroids or any analgesic drug.
Randomization was provided using sequentially numbered opaque sealed envelope technique (SNOSE) [10]. Patients were randomized to receive either bilateral SCPB or no intervention (control group). All patients were premedicated using midazolam 0.03 mg kg−1 iv upon arrival to the preoperative holding area.
2.1 SCPB Technique
SCPB was performed at the preoperative block area following standardized monitoring, which included noninvasive blood pressure, electrocardiogram, and pulse oximetry. All blocks were performed approximately 20 min before induction of general anesthesia. The block was performed as described by Hadzic [11] in the supine position and the head was turned slightly away from the side to be blocked to facilitate operator access. Blocks were performed bilaterally using the same approach. Skin preparation was performed using 10 % povidone iodide. Probe was covered with a sterile cover. All blocks were performed using high frequency broadband linear probe (Philips, Sparq, L 4-12, Bothell, USA) by the same anesthesiologist (YG) experienced in US guided nerve blocks. Block was performed at the midpoint of sternocleidomastoid muscle (SCM) (Fig. 1). Linear probe was placed on the lateral neck, over the SCM using a transverse approach. Once the SCM is identified the probe was moved posteriorly so that the edge of the SCM is on the screen. Following negative aspiration 0.5–1 ml of local anesthetic (LA) is administered to verify correct position of the needle tip and the rest of LA is administered in fractioned doses following intermittent aspiration to avoid any inadvertent intravascular injection. The plexus was visualized as small hypoechoic structures immediately deep to the SCM (Fig. 2). Using a 5 cm sonovisible nerve block needle (BBraun Sonoplex, Melsungen, Germany), block was performed using out-of-plane approach. Ten ml of bupivacaine 0.25 % was deposited in the plane immediately deep to the SCM and underneath the prevertebral fascia.
Ultrasound image of superficial cervical plexus in transverse view. Branches of superficial cervical plexus behind the prevertebral fascia. SCM sternocleidomastoid muscle, SCP superficial cervical plexus, CA carotid artery, IJV internal jugular vein. Thin white arrows Prevertebral fascia, thick white arrows superficial cervical plexus. a Before block performance, b after LA administration
2.2 General anesthesia
General anesthesia was induced using thiopental (5–7 mg kg−1) and fentanyl (2 μg kg−1) iv. Tracheal intubation was performed following rocuronium 0.6 mg kg−1 administration iv. General anesthesia was maintained with desflurane in combination with nitrous oxide in oxygen with a ratio of 2:1 in 3 L of fresh gas flow. Desflurane was adjusted to maintain a bispectral index index (BIS; Aspect Medical Systems, Newton, USA) between 40 and 60. The lungs were ventilated to maintain end-tidal carbon dioxide at 35 to 40 mmHg. During anesthesia maintenance, monitoring included pulse oximetry, an electrocardiogram, NIBP, BIS, end-tidal carbon dioxide, end-tidal desflurane, and fraction of inspired oxygen. Lornoxicam 8 mg and paracetamol 1 g was administered intravenously to provide postoperative analgesia approximately 10 min before the end of the surgery. Ondansetron 8 mg was also administered to prevent PONV.
Neuromuscular reversal was provided with administration of 0.05 mg/kg of neostigmine and 0.02 mg/kg of intravenous atropine at the end of surgery.
All patients were operated by the same surgical team. Postoperative pain was assessed using VAS scale ranging from 0 (no pain) to 10 (worst imaginable pain). In the recovery room, all patients were provided a patient-controlled analgesia device (PCA) containing morphine 0.5 mg ml−1.
Postoperative analgesia device was set to deliver 1 mg bolus dose morphine, 8 min lockout time and 6 mg 1 h limit. On the ward, VAS scores were recorded at 1, 6, 12 and 24 h postoperatively. The incidence of nausea and vomiting, total morphine consumption during the 24 h postoperative period was recorded. A blinded pain nurse performed postoperative follow-up of patients.
Statistical analysis was performed using the SPSS software (version 15 SPSS Inc, Chicago, Illinois, USA). Demographic data are presented as mean (±SD). Numerical data are presented as median (25.−75. percentiles). P < 0.05 was considered as statistically significant difference.
The Kolmogorov–Smirnov test used for normality. Mann–Whitney U test was used for comparison of VAS scores in movement and morphine consumption between two groups. For comparison of side effects like nausea and vomiting Chi square test was performed.
A preliminary study on the same surgical population in our clinic showed that the mean (±SD) morphine consumption in the postoperative 24 h was 18 mg (±9). For 90 % power and an error of 0.05, the sample size necessary to detect a 30 % difference in postoperative morphine requirement using bilateral SCPB compared to control group was 22 subjects per group. We included 25 patients in each group to increase the power of the study and also to secure patients dropouts for any reason.
3 Results
Fifty patients were included into the study starting from the first of September till the end of December 2013. Demographic data, type and duration of surgery were similar between the groups (Table 1). Only one patient in the control group was excluded from the study because of persistent nausea and vomiting due to morphine PCA consumption at postoperative 12 h.
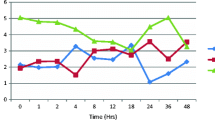
VAS score for pain is presented in Table 2. In both groups adequate analgesia was achieved with the use of morphine PCA. VAS scores for pain were similar between groups. Morphine consumption at 6, 12 and 24 h postoperatively were significantly higher in the control group compared to the SCPB group (P < 0.05).
Seven patients in the SCPB group had hoarseness following block performance. None of the patients had hoarseness in the control group.
Six patients in SCPB group had nausea and 4 of them also had vomiting. In control group eight patients had nausea and four of them also had vomiting. One patient in SCPB group complained of ear lobe numbness, which resolved in 12 h postoperatively.
4 Discussion
Controversial study findings about the effectiveness of SCPB for thyroid surgery has led us to evaluate the analgesic effect of the block this time under US guidance (2–7). In general success/effectiveness of a regional techniques relies on both localizing the target nerves or correct tissue plane and also providing optimum LA distribution within that anatomical field. Especially during interfacial or compartment blocks where LA is administered in between two fascia the incidence of correct tissue plane injection rate can be as low as 14 % [12]. US guidance has led to a refinement in regional anesthesia techniques improving their efficacy and safety [13–17]. Because most of the earlier studies were mainly blinded approaches for SCPB, we thought that the same questioning was necessary to evaluate the effect of SCPB used for thyroid surgery. To the best of our knowledge this is the first study that evaluated the effectiveness of SCPB under US guidance. Yet the lack of a blind technique group can be considered as a limitation of the study.
Current literature indicates that unless performed by the surgical team during surgery, other landmark based “blind” approaches to BSCPB may lead to unreliable success rates [4, 18, 19]. Contrary to blocks performed by the surgical team under direct vision results of “blind” approaches are more controversial and disfavoring BSCPB on postoperative pain [2, 3, 20]. On the other hand in the experienced hands SCPB has been utilized to provide surgical anesthesia [6, 7]. Therefore we think that the failure is probably not due to inability of the block to provide analgesia but using blind approaches its clinicians’ limited ability to know the exact needle tip localization and LA distribution. In our study using visual guidance postoperative analgesic requirement was significantly lower in the SCPB group favoring the effectiveness of SCPB.
Currently there is a large spectrum of both LA concentration (bupivacaine 0.25–0.5 %) and volume (5–20 ml) administered for SCPB. Although higher LA dose/concentration may be required to provide surgical anesthesia, optimal LA dose for postoperative analgesia needs to be studies (6–7). Therefore not all SCPB studies are standardized and easily comparable to others. Because the superficial cervical plexus is made up of purely sensory nerves we have administered a relatively low concentration of LA (bupivacaine 0.25 %). In our study we administered only 10 ml of LA and considering the US images it is our clinical impression that even lower doses could also be sufficient. A cadaver study has shown that as low as 2 ml of LA can cover the superficial cervical plexus [21]. Yet clinical dose finding studies are required to evaluate the optimal dose of LA when SCPB is performed under US guidance.
To the best of our knowledge hoarseness was not reported following SCPB for thyroid surgery. Twenty-eight per cent of our patients had hoarseness without respiratory distress. We performed our blocks around 20 min before general anesthesia induction, which allowed us to detect hoarseness, which was solely due to the block performance. In most of the earlier studies SCPB was performed just before or after GA induction that is why hoarseness due to block was not recorded. In all patients hoarseness was relieved within 6 h after surgery. Compared to blind techniques US guidance might allow us to inject LA to a closer location to the nerve. The incidence of hoarseness also should be studied during future studies. The incidence of hoarseness in patients undergoing carotid endarterectomy was reported to range between 22–32 %, which is similar to our rates [22].
It is obvious that LA administered around the SCPB could also distributed to interscalene area, which may cause brachial plexus block. Earlier studies reported cases with motor block of upper extremity and even diaphragmatic paresis [3, 5]. We think that lowering the dose and concentration of LA administered for SCPB will reduce the risk brachial plexus block and diaphragmatic paresis as it was shown during interscalene block [16]. In our study using only 10 ml of LA, none of our patients had brachial plexus block.
One patient in the SCPB group complained for ear lobe numbness, which is a physiological result of the block. Steffen [20] reported that in about half of the patients in their study ear lobe numbness was reported. Ear lobe numbness was not specifically questioned during our study therefore we cannot provide an exact incidence.
Thyroid surgery can be associated with a high incidence of PONV ranging from 21.7 to 63.3 % [23]. We think that US guided SBCP is a relatively simple technique. SCBP by providing effective analgesia has reduced the requirement for opioids. Yet this decrease in opioid consumption was not enough to provide a significant decrease in the incidence of postoperative nausea and vomiting. The use of inhalational anesthesia with nitrous oxide during our study could eliminate the anti-nausea-effect of regional anesthesia.
This study was not double blinded therefore the possibility of a placebo effect could be considered as a limitation of the study.
In conclusion our study has shown that US guided SCPB has a significant analgesic effect in patients undergoing thyroid surgery. Although reduced postoperative analgesic requirement resulted in reduced opioid consumption this decrease was not enough to provide a significant decrease on the morphine related side effects. Further studies are required to search for the optimal LA dose during US guided SCPB.
References
Suh YJ, Kim YS, In JH, Joo JD, Jeon YS, Kim HK. Comparison of analgesic efficacy between bilateral superficial and combined (superficial and deep) cervical plexus block administered before thyroid surgery. Eur J Anaesthesiol. 2009;26:1043–7.
Eti Z, Irmak P, Gulluoglu BM, Manukyan MN, Gogus FY. Does bilateral superficial cervical plexus block decrease analgesic requirement after thyroid surgery? Anesth Analg. 2006;102:1174–6.
Herbland A, Cantini O, Reynier P, Valat P, Jougon J, Arimone Y, Janvier G. The bilateral superficial cervical plexus block with 0.75% ropivacaine administered before or after surgery does not prevent postoperative pain after total thyroidectomy. Reg Anesth Pain Med. 2006;31:34–9.
Kesisoglou I, Papavramidis TS, Michalopoulos N, Ioannidis K, Trikoupi A, Sapalidis K, Papavramidis ST. Superficial selective cervical plexus block following total thyroidectomy: a randomized trial. Head Neck. 2010;32:984–8.
Shih ML, Duh QY, Hsieh CB, Liu YC, Lu CH, Wong CS, Yu JC, Yeh CC. Bilateral superficial cervical plexus block combined with general anesthesia administered in thyroid operations. World J Surg. 2010;34:2338–43.
Karthikeyan VS, Sistla SC, Badhe AS, Mahalakshmy T, Rajkumar N, Ali SM, Gopalakrishnan S. Randomized controlled trial on the efficacy of bilateral superficial cervical plexus block in thyroidectomy. Pain Pract. 2012;13:539–46.
Mukhopadhyay S, Niyogi M, Dutta M, Ray R, Gayen GC, Mukherjee M, Mukhopadhyay BS. Bilateral superficial cervical plexus block with or without low-dose intravenous ketamine analgesia: effective, simple, safe, and cheap alternative to conventional general anesthesia for selected neck surgeries. Local Reg Anesth. 2012;5:1–7.
Antonakakis JG, Ting PH, Sites B. Ultrasound-guided regional anesthesia for peripheral nerve blocks: an evidence-based outcome review. Anesthesiol Clin. 2011;29:179–91.
Liu SS, Ngeow J, John RS. Evidence basis for ultrasound-guided block characteristics: onset, quality, and duration. Reg Anesth Pain Med. 2010;35(2 Suppl):S26–35.
Doig GS, Simpson F. Randomization and allocation concealment: a practical guide for researchers. J Crit Care. 2005;20:187–93.
Hadzic A, editor. Ultrasound-guided cervical plexus block. In: Hadzic’s peripheral nerve blocks and anatomy for ultrasound-guided regional anesthesia. 2nd ed. New York: Mc-Graw Hill; 2012. p. 345–351.
Weintraud M, Marhofer P, Bösenberg A, Kapral S, Willschke H, Felfernig M, Kettner S. Ilioinguinal/iliohypogastric blocks in children: where do we administer the local anesthetic without direct visualization? Anesth Analg. 2008;106:89–93.
Willschke H, Bosenberg A, Marhofer P, Johnston S, Kettner S, Eichenberger U, Wanzel O, Kapral S. Ultrasonographic guided ilioinguinal/iliohypogastric nerve block in pediatric anesthesia: what is the optimal volume? Anesth Analg. 2006;102:1680–4.
Willschke H, Marhofer P, Bosenberg A, Johnston S, Wanzel O, Cox SG, Sitzwohl C, Kapral S. Ultrasonography for ilioinguinal/iliohypogastric nerve blocks in children. Br J Anaesth. 2005;95:226–30.
Koscielniak-Nielsen ZJ. Ultrasound-guided peripheral nerve blocks: what are the benefits? Acta Anaesthesiol Scand. 2008;52:727–37.
Riazi S, Carmichael N, Awad I, Holtby RM, McCartney CJ. Effect of local anaesthetic volume (20 vs 5 ml) on the efficacy and respiratory consequences of ultrasound-guided interscalene brachial plexus block. Br J Anaesth. 2008;101(4):549–56.
Marhofer P, Harrop-Griffiths W, Willschke H, Kirchmair L. Fifteen years of ultrasound guidance in regional anaesthesia: part 2-recent developments in block techniques. Br J Anaesth. 2010;104:673–83.
Egan RJ, Hopkins JC, Beamish AJ, Shah R, Edwards AG, Morgan JD. Randomized clinical trial of intraoperative superficial cervical plexus block versus incisional local anaesthesia in thyroid and parathyroid surgery. Br J Surg. 2013;100:1732–8.
Dieudonne N, Gomola A, Bonnichon P, Ozier YM. Prevention of postoperative pain after thyroid surgery: a double-blind randomized study of bilateral superficial cervical plexus blocks. Anesth Analg. 2001;92:1538–42.
Steffen T, Warschkow R, Brändle M, Tarantino I, Clerici T. Randomized controlled trial of bilateral superficial cervical plexus block versus placebo in thyroid surgery. Br J Surg. 2010;97:1000–6.
Guay J, Grabs D. A cadaver study to determine the minimum volume of methylene blue or black naphthol required to completely color the nerves relevant for anesthesia during breast surgery. Clin Anat. 2011;24:202–8.
Umbrain VJ, van Gorp VL, Schmedding E, Debing EE, von Kemp K, Van den Brande PM, Camu F. Ropivacaine 3.75 mg/ml, 5 mg/ml, or 7.5 mg/ml for cervical plexus block during carotid endarterectomy. Reg Anesth Pain Med. 2004;29:312–6.
Warschkow R, Tarantino I, Jensen K, Beutner U, Clerici T, Schmied BM, Steffen T. Bilateral superficial cervical plexus block in combination with general anesthesia has a low efficacy in thyroid surgery: a meta-analysis of randomized controlled trials. Thyroid. 2012;22:44–52.
Acknowledgments
The authors have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gürkan, Y., Taş, Z., Toker, K. et al. Ultrasound guided bilateral cervical plexus block reduces postoperative opioid consumption following thyroid surgery. J Clin Monit Comput 29, 579–584 (2015). https://doi.org/10.1007/s10877-014-9635-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-014-9635-x