Abstract
Purpose
Individuals with spinal cord injury (SCI) have an increased risk of cardiac arrhythmias, particularly during autonomic dysreflexia (acute hypertensive episodes). This may be partly due to impaired autonomic control of the heart after SCI. The interval between the peak and end of the T-wave of the electrocardiograph (ECG) provides an index of transmural dispersion of repolarisation, a factor underlying the development of ventricular arrhythmias. Another ECG-based risk factor for ventricular arrhythmias is variability in the QT segment, the QT variability index (QTVI). Similarly, P-wave variability may be correlated with risk for atrial arrhythmias. We aimed to: (1) determine whether there are abnormalities in these parameters at rest in those with SCI; (2) determine correlations between these ECG parameters and severity of autonomic impairment after SCI.
Methods
ECG intervals were determined using customised software from a 15 min ECG recording (lead II) in 28 SCI subjects and 27 controls. Autonomic severity of SCI was determined from sympathetic skin responses, low frequency systolic blood pressure variability, and plasma noradrenaline levels.
Results
Tpeak–Tend variability and QTVI were increased in those with autonomically complete SCI compared to controls. P-wave variability was increased in SCI individuals compared to controls, and was negatively correlated with plasma noradrenaline.
Conclusion
The higher Tpeak–Tend variability, QTVI and P-wave variability in individuals with SCI could be markers of severity of injury to cardiac autonomic (sympathetic) pathways after SCI, and may represent new risk assessment parameters for predisposition to cardiac arrhythmias in this population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiovascular disease is the leading cause of mortality and morbidity in individuals with spinal cord injury (SCI) [1, 2]. Furthermore, cardiovascular disease after SCI has an earlier onset and more rapid progression than in the able-bodied [1].
One possible cause of this increased risk for cardiovascular disease is altered autonomic function after SCI, with associated modulations in cardiac electrophysiology and increased risk of cardiac arrhythmias [3]. Certainly, rats with high thoracic lesions demonstrate changes in protein expression that increase sarcoplasmatic reticulum calcium load and lead to ectopic activity [3]. These changes are associated with a decreased electrical stimulation threshold to induce ectopics [3].
The extent of cardiovascular autonomic dysfunction is related to the level and severity of injury to spinal cardiovascular sympathetic pathways [4]. Injuries above the fifth thoracic level (T5) can impair sympathetic regulation of the heart and splanchnic vasculature (a key site for blood pressure regulation) with particularly pronounced effects on cardiovascular control [4]. Cardiovascular parasympathetic pathways do not pass through the spinal cord and are thus not affected by SCI. As such, the normal coordinated pattern of activity of the autonomic nervous system can become dyssynchronous, with devastating effects on cardiovascular function [5–7].
Case reports in humans [8–10] as well as studies in rodents [11] have documented ventricular and/or atrial arrhythmias after SCI, particularly during episodes of autonomic dysreflexia (AD, sudden onset of profound hypertension triggered by sensory stimuli below lesion). During AD, the precipitating stimulus triggers massive sympathetic discharge through a spinal reflex that is no longer subject to regulation by the injured descending spinal autonomic pathways. This leads to extreme hypertension, and increases the spatial dispersion of ventricular repolarization, increasing the likelihood of re-entry arrhythmias [7]. In addition, unique to SCI, this elevated cardiac sympathetic activity is coupled with elevated cardiac vagal activity during AD, through hypertension-induced stimulation of the arterial baroreflex and subsequent increases in efferent parasympathetic activity mediated via the cardiac vagus nerves [12], and this may be particularly proarrhythmogenic.
The electrocardiograph (ECG) can potentially be used to identify those individuals at risk of developing arrhythmias during episodes of AD. Prolonged transmural dispersion of ventricular repolarisation has been shown to be a substrate for ventricular arrhythmias, specifically Torsade des Pointes [13]. Transmural dispersion of repolarisation corresponds to the difference in timing and duration of repolarisation in the different layers of the ventricular wall [14], which is reflected by the Tpeak–Tend interval of the ECG [14]. Hence, Tpeak–Tend can be used as a risk assessment parameter for ventricular arrhythmias [14, 15]. Another ECG-derived parameter that is believed to identify increased risk for ventricular arrhythmias is the QT variability index (QTVI) [16].
In addition to an increased risk of ventricular arrhythmias, atrial arrhythmias such as atrial fibrillation are common in individuals with SCI [6]. Prolongation of intra-atrial conduction time is associated with atrial fibrillation attributable to inhomogeneous propagation of sinus impulses in the atria [17]. It has been proposed that this could be identified by variation in P-wave duration in differently oriented surface ECG leads, or P-wave dispersion (PWD) [18]. Another approach would be to study P-wave variability in the time and frequency domain (by assessing the P-wave duration in the same ECG lead over time), and we propose that this parameter could also be a predictor for atrial arrhythmias.
A previous report in humans has investigated differences in ECG parameters [19] between individuals with high and low level SCI, but failed to account for injury to cardiovascular autonomic pathways, which would be expected to influence both the ECG characteristics, and susceptibility to arrhythmia. Accordingly, our goal was to explore the proposed ECG predictors for ventricular and atrial arrhythmias in individuals with chronic SCI with different levels and severities of injury to cardiovascular autonomic pathways. We hypothesised that those with severe autonomic injury would have increased Tpeak–Tend, QTVI, PWD and P-wave variability compared to those with incomplete autonomic injury and able-bodied controls.
Methods
The study received ethical approval from the Simon Fraser University and the University of British Columbia Research Ethics Committees, and was performed in association with the Declaration of Helsinki of the World Medical Association.
Subjects
Studies were performed on 28 individuals with chronic (>1 year) SCI, and 27 able-bodied controls. All volunteers gave written informed consent, and were apparently healthy and not taking any cardiovascular medications. Females were not tested during their menstrual period. Volunteers abstained from drinking alcoholic beverages starting the night before testing, and caffeine the morning of testing.
Measures of completeness of injury
Motor and sensory impairment
Neurological classification of level and severity of SCI was determined from the American Spinal Injury Association (ASIA) Impairment Scale (AIS). This scale assesses motor and sensory function after SCI [20], but does not incorporate a quantitative measure of autonomic function [21]. An AIS A score reflects complete loss of motor and sensory function; the B, C and D scores reflect gradually less severe impairments. Level of injury and impairment score together form the classification of the injury (e.g. T5A).
Autonomic impairment
At present, there is no gold standard for the quantitative assessment of autonomic completeness of SCI. Therefore, to assess severity of injury to spinal autonomic pathways in individuals with SCI we used three methods: sympathetic skin responses (SSR); plasma noradrenaline levels; and low frequency power of systolic arterial pressure (LF SAP).
Sympathetic skin responses
This test assesses sympathetic cholinergic pathways, which are dependent on central and peripheral sympathetic input [22]. Impaired supraspinal control of sympathetic pathways leads to an impaired SSR; therefore, this can be used to evaluate autonomic injury following SCI. Recordings were conducted simultaneously and bilaterally from both hands in response to a pulse applied ten times to the left median nerve [5]. The outcome measurement is a sum score of the normal elicited SSR with a maximum response of 10 for each stimulation site. The maximum score (20) is considered a normal SSR. For categorical analyses, autonomic completeness of injury was determined based on the SSR, whereby individuals with autonomically complete lesions had a SSR score of 0, and those with autonomically incomplete lesions had a score of 1 or higher [23].
Plasma noradrenaline levels
We used an orthostatic stress test [23] to assess severity of cardiovascular autonomic dysfunction from plasma noradrenaline responses to orthostasis. Low noradrenaline levels, due to sympathetic hypoactivity, are indicative of injury to descending sympathetic pathways [24]. A butterfly catheter was inserted into an antecubital vein and samples were withdrawn after 15 min of supine rest, and then 5 min after the passive assumption of a seated position. Samples were centrifuged at 3 °C and 3,000 rpm for 10 min and the plasma component withdrawn for subsequent analysis. The plasma samples were sent to the clinical laboratory of Vancouver General Hospital for determination of noradrenaline levels. For correlative analyses we used the absolute noradrenaline level, as described by our group previously [23].
Low frequency power of systolic arterial pressure
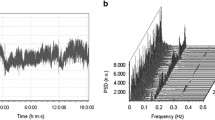
The power of LF SAP variability reflects sympathetic drive to the resistance vessels [24], and is markedly reduced in individuals with autonomically complete SCI [25]. Continuous beat-to-beat blood pressure was recorded using finger plethysmography (Finometer, Finapres Medical Systems BV, Arnhem, The Netherlands) during 15 min of supine rest. We fitted autoregressive monovariate models to the time series of the beat-to-beat systolic arterial pressure signal and identified the low frequency peak (at ~0.1 Hz) from the power spectrum. We calculated central frequency, attributed power, percentage power and power in normalised units (LF SAP nu = LF SAP power/[total variance−very low frequency SAP power (~0.03 Hz)] × 100). For correlative analyses, we used the absolute value of the LF SAP, as described by our group previously [23].
Continuous electrocardiogram
A resting lead II ECG (Finometer ECG module, Finapres Medical Systems BV, Arnhem, The Netherlands) was continuously recorded in the supine position for 15 min. Data acquisition was performed with a sampling frequency of 1 kHz using an analogue-to-digital converter (Powerlab 16/30, AD Instruments, Colorado Springs, CO).
ECG interval detection
ECG parameters (RR interval, QT, QTc, using the method of Bazett [25], Tpeak–Tend, QTVI and P-wave duration) were determined for every beat using customised software (LabView 2009, National Instruments) (Fig. 1).
Example graphical representation of the customised interval detection programme outcomes on a continuous ECG tracing, using different coloured markers for the different points of interest. The programme outputs time and amplitude coordinates for each point of interest as well as the corresponding intervals. The shaded areas represent P-wave duration (light grey), QT interval (grey) and Tpeak–Tend duration (dark grey)
The location and amplitude of the R-wave was determined from the point of zero slope at the maximum amplitude of the derivative of the signal. The stable T–P section was identified by linear regression of the signal between two consecutive R-waves. The Tpeak was determined from the maximum value of a 3rd order polynomial applied 100 ms after the preceding R up until the midpoint of the T–P section. The Q-wave was identified from the minimum value of a 3rd order polynomial applied to the 50 ms of data preceding the R-wave. The Ppeak was determined from the maximum point of a polynomial regression of the 20 ms of data preceding the Q-wave. The Tend was determined from the point at which two regression lines intersect, applied from the Tpeak forwards and from the middle of the T–P section backwards. Finally, the Pend was identified from the point at which regressions applied to the section between the Ppeak and Q-waves intersect.
Variability analyses
We determined variability for each of the ECG intervals (Tpeak–Tend and P-wave duration) using autoregressive spectral analysis. QTVI was determined using the following equation:
where QTv is the QT variability, QTm the mean QT interval, RRv the variability of RR interval, and RRm the mean RR interval [16]. QTVI is typically a negative value, with values closer to zero being considered abnormal [13].
12-Lead electrocardiogram
To determine PWD, we collected 12-lead ECG’s during seated rest from 17 volunteers with cervical SCI. In 15 age and gender matched able-bodied controls a 12-lead ECG (Burdick Atria 6100, Cardiac Science Corporation, Hannover, Germany) was recorded during supine (n = 14) and seated (n = 10) rest. Digital callipers were used to measure the P-wave duration in every lead from the signal averaged 12-lead ECG’s scanned in high resolution (600 dpi) from a paper print. According to convention [17], P-wave duration in a single lead was discarded when the beginning and end of the P-wave could not be accurately determined. PWD was calculated for every ECG with more than nine measurable leads [17].
Statistics
Statistical analyses were performed using SigmaPlot version 11 (Systat Software Inc, San Jose, CA). Data were tested for normality using the Shapiro–Wilk test. Comparisons between two groups were performed using unpaired Student’s t-tests or Wilcoxon tests for parametric and nonparametric data, respectively. One-way ANOVA or Kruskal–Wallis tests with Tukey post hoc tests were performed for comparisons between three groups. Correlations between variables were performed using Pearson Product Moment analyses or Spearman Rank Order tests. Possible differences in gender and the number of discarded leads in each group (PWD analysis) were determined using the Pearson Chi-squared test. All data are presented as mean ± SEM. Statistical significance was assumed at the level of p < 0.05.
Results
The SCI volunteers were subdivided into different groups for analyses: (1) by region of injury—cervical or thoracic; (2) by level of injury—below or above (and at) T5; (3) by autonomic impairment as determined from the SSR—complete (score of zero) or incomplete (score greater than zero); (4) by motor and sensory impairment according to the AIS score—complete (AIS A) or incomplete (AIS B, C or D).
Subject characteristics
We found no significant age or gender differences between groups. Levels of injury in the cervical SCI group ranged from C4 to C7 and motor/sensory impairment defined by AIS grades [20] was as follows: grade A, n = 7; grade B, n = 5; grade C, n = 2; and grade D, n = 1. Levels of injury in the thoracic group ranged from T3 to T11 and motor/sensory impairment was as follows: grade A, n = 11; grade B, n = 1; and grade D, n = 1. Not all volunteers opted to complete all test procedures. Subject details can be found in Table 1.
Continuous ECG
ECG interval analyses
Resting RR interval was significantly longer in the cervical SCI group (1,047 ± 29 ms) compared to controls (952 ± 21 ms, p = 0.04), consistent with modest bradycardia. RR interval was significantly shorter in the thoracic SCI group (925 ± 39 ms) compared to the cervical SCI group (1,047 ± 29 ms, p = 0.02). There were no differences between groups for all other parameters (QT, QTc, Tpeak–Tend and P-wave duration). Absolute values for all intervals are summarised in Table 2.
Variability analyses
Tpeak–Tend variability was significantly greater in the SCI group (91.0 ± 14.9 ms2) compared to controls (49.7 ± 12.7 ms2, p = 0.04) (Fig. 2a). Level of injury influenced Tpeak–Tend variability, with significantly greater Tpeak–Tend variability only in those with lesions above T5 (93.2 ± 16.9 ms2) compared to controls (p = 0.024) (Fig. 2b). Tpeak–Tend variability was also significantly greater in those with autonomically complete injuries (103.3 ± 24.6 ms2) compared to controls (p = 0.019) (Fig. 2c). We found no significant differences in Tpeak–Tend variability between SCI groups and controls when grouped according to AIS scores (Fig. 2d).
Tpeak–Tend and Tpeak–Tend variability in controls and SCI volunteers. a Tpeak–Tend variability was significantly greater in individuals with SCI. b Tpeak–Tend variability was significantly greater in those with SCI above T5 compared to controls. c Tpeak–Tend variability was significantly greater in the autonomically complete SCI group compared to controls. d Tpeak–Tend variability was not significantly different between groups when subdivided according to the AIS examination
QTVI was significantly greater (closer to zero) in the SCI group (−1.03 ± 0.100) compared to controls (−1.31 ± 0.078, p = 0.019). Again, this was related to the level of injury, with greater QTVI in those with lesions above T5 (−1.12 ± 0.166) compared to controls (p = 0.021) (Fig. 3a). We found no significant difference between those with lesions below T5 and controls. Similarly QTVI was significantly greater in those with autonomically complete injuries (−0.87 ± 0.172), compared to controls (p = 0.009). Responses in those with autonomically incomplete injuries were not significantly different from both other groups (Fig. 3b). We found no significant differences in QTVI between control and SCI groups when grouped according to AIS scores (Fig. 3c).
QTVI in controls and SCI volunteers. a QTVI was significantly greater in those with SCI above T5 compared to controls. b QTVI was significantly greater in the autonomically complete SCI group compared to controls. c QTVI was not significantly different between groups when subdivided according to the AIS examination. d A significant positive correlation can be seen between QTVI and Tpeak–Tend variability
In addition, QTVI and Tpeak–Tend variability were significantly correlated with each other (r = 0.734, p < 0.001, Fig. 3d).
P-wave duration variability was greater in SCI individuals (104.9 ± 15.8 ms2) compared to controls (28.6 ± 4.6 ms2, p = 0.004) (Fig. 4a). ANOVA testing with the different SCI subgroups was not conducted for this parameter due to a smaller sample size for this measure (control n = 17 and SCI n = 16). P-wave variability was correlated with both Tpeak–Tend variability (r = 0.608, p < 0.001, Fig. 4b) and QTVI (r = 0.421, p = 0.015). There was no correlation between P-wave variability and the average cycle length (RR interval) (r = 0.074, p = 0.068). All variability data is summarised in Table 3.
P-wave variability over time in the control and SCI group. a P-wave variability was significantly greater in the SCI group compared to controls. b A significant positive correlation can be seen between P-wave variability and Tpeak–Tend variability. c A significant negative correlation can be seen between P-wave variability and upright noradrenaline (NA). d A significant negative correlation between P-wave variability and LF SAPnu can be seen
Correlations with autonomic impairment
We found a significant negative correlation between upright noradrenaline and P-wave variability (r = −0.496, p = 0.035, Fig. 4c). In addition, Tpeak–Tend variability (r = −0.341, p = 0.011) and P-wave variability (r = −0.497, p = 0.004) were significantly correlated with the severity of autonomic impairment, as determined from the LF SAPnu (Fig. 4d).
12-Lead electrocardiogram
We found no significant differences in PWD between the SCI group (36.7 ± 3.2 ms) and controls (31.5 ± 3.3 ms, p = 0.346). In more individuals with SCI (n = 15; 88 %) one or more leads were rejected for analysis than in controls (n = 2; 14 %) (χ2 = 2.261 and p < 0.001).
Since the 12-lead ECG was recorded while seated in SCI volunteers, but while supine in controls according to convention, we evaluated whether alterations in autonomic tone associated with postural changes could have influenced our results, in a subset (n = 10) of controls. We found no significant differences in supine and seated PWD in controls (31.5 ± 3.3 ms and 29.1 ± 1.6 ms, respectively, p = 0.613). Also, when compared to the SCI group, the seated PWD in controls remained similar (p > 0.05).
Discussion
We evaluated different ECG-based parameters that might be used as risk assessment tools for the propensity to develop cardiac arrhythmias after SCI. Not only did we observe differences in these parameters between individuals with SCI and able-bodied controls, but we also found correlations between these measures and the severity of autonomic impairment after injury. Our main finding was that Tpeak–Tend variability and QTVI were greater in the SCI group, particularly in those with high-level and autonomically complete lesions. The relationship between the severity of autonomic impairment and increased variability in the Tpeak–Tend and QT intervals suggests that autonomic impairment could underlie the increased risk for ventricular arrhythmias after SCI. The abnormal variability of Tpeak–Tend and QTVI was independent of the AIS score, confirming that completeness of injury to motor or sensory pathways does not necessarily correlate with completeness of injury to autonomic pathways. This is consistent with our earlier findings [5] and highlights the need for quantitative autonomic function testing after SCI.
Our data are supported by a recent study that reported increased QTVI in individuals with SCI [26]. However, their data did not show differences in QTVI between different SCI groups, which were subdivided by level of injury. This likely reflects the failure to account for completeness of injury to cardiovascular autonomic pathways.
Both proposed risk assessment parameters for ventricular arrhythmias tested were correlated with each other, and with the severity of injury to cardiovascular autonomic pathways, indicating their possible utility as screening tools to assess risk for ventricular arrhythmia after SCI.
P-wave duration variability in a continuous ECG recording was increased in the SCI group compared to controls. The increase in P-wave variability was significantly correlated with measures of severity of injury to autonomic pathways. Unfortunately, due to a smaller amplitude of the P-wave in general, occasional background noise, and axis shifts, faithful detection of P-wave duration was difficult, reducing the sample size for this measure (SCI n = 16; control n = 17), rendering subanalyses invalid. Nevertheless, we can exclude the possibility that the increased P-wave variability in the SCI group was artefactual due to increased background noise in this group because we quantified the noise levels at the isoelectric T–P sections of the ECG and they were not significantly different between groups (control 0.0002 ± 0.0001 ms2 and SCI 0.0007 ± 0.0001 ms2, p = 0.29). We propose that the increased P-wave variability observed is compatible with abnormal repolarisation properties within the atria in those with loss of the normal sympathetic modulation of the heart, and may be associated with an increased risk of experiencing atrial arrhythmia.
PWD is thought to be correlated with risk for atrial arrhythmia. In this study, we found no difference in PWD between the SCI group and controls. This can be explained in two ways: either the SCI group is not at greater risk for atrial arrhythmias, or PWD is not a good risk assessment parameter for atrial arrhythmias after SCI. In a subgroup (n = 9) of individuals with autonomically complete SCI (and thus a high likelihood of experiencing atrial arrhythmia) the PWD remained similar to controls, making the first explanation unlikely. The second explanation is supported by some technical difficulties in measuring this parameter; more leads were discarded in the ECG of SCI individuals than in controls. This could have led to an artificial decrease in PWD in the SCI group, and may have masked any true differences between groups in this parameter. Since the determination of P-wave variability over time on a continuous ECG requires measureable P-waves in only one ECG lead, we suggest it may provide a better parameter for risk of atrial arrhythmias after SCI.
One limitation of this study is that not all parameters were collected in every volunteer; some volunteers declined to participate in all tests. A second limitation is that we could not measure a direct correlation between Tpeak–Tend variability, QTVI and P-wave variability and the occurrence of cardiac arrhythmias. There is good evidence, however, that AD, and thus autonomic impairment after SCI, is associated with cardiac arrhythmias [5, 6]. The relationship shown between autonomic impairment and these ECG parameters implies that a correlation between these measures and susceptibility to cardiac arrhythmias may exist, but does not confirm it. Therefore, at present we acknowledge that we have not demonstrated a link between these measures and propensity to experience arrhythmia, but rather that we have identified ECG-based characteristics in individuals with SCI that are associated with an increased risk of arrhythmia in other populations [14, 16, 26]. However, preliminary data during AD from four individuals with autonomically complete cervical SCI (in whom resting QTVI and Tpeak–Tend variability were already increased, similar to the present findings) reveal further marked increases in both QTVI (+0.43 ± 0.1; p < 0.05) and Tpeak–Tend variability (+300 ± 97 ms2; p < 0.05) compared to baseline, associated with marked ventricular ectopy. These data need verification in a larger population, but do support our hypothesis that these measures are related to arrhythmia risk. Future directions would, therefore, be to determine the relationships between these ECG-based parameters at rest and the occurrence of cardiac arrhythmias during episodes of AD, when risks for arrhythmia are highest.
Conclusions
We have observed abnormal ECG characteristics in individuals with autonomically complete SCI that, at least in able-bodied populations, are associated with increased susceptibility to cardiac arrhythmia. The increases in Tpeak–Tend variability, P-wave variability and QTVI observed occurred only in those individuals with complete lesions to descending cardiac sympathetic pathways, who also experience episodes of AD during which risk for arrhythmia is high. Furthermore, the magnitude of impairment to cardiac autonomic pathways was directly correlated with the severity of these ECG abnormalities. We propose that these ECG characteristics provide useful measures of severity of injury to cardiovascular autonomic pathways, and may prove to be indicative of susceptibilty to cardiac arrhythmia after SCI.
References
Myers J, Lee M, Kiratli J (2007) Cardiovascular disease in spinal cord injury: an overview of prevalence, risk, evaluation, and management. Am J Phys Med Rehabil 86(2):142–152
Garshick E, Kelley A, Cohen SA, Garrison A, Tun CG, Gagnon D, Brown R (2005) A prospective assessment of mortality in chronic spinal cord injury. Spinal Cord 43(7):408–416
Rodenbaugh DW, Collins HL, DiCarlo SE (2003) Increased susceptibility to ventricular arrhythmias in hypertensive paraplegic rats. Clin Exp Hypertens 25(6):349–358
Krassioukov A, Claydon VE (2006) The clinical problems in cardiovascular control following spinal cord injury: an overview. Prog Brain Res 152:223–229
Claydon VE, Elliott SL, Sheel AW, Krassioukov A (2006) Cardiovascular responses to vibrostimulation for sperm retrieval in men with spinal cord injury. J spinal cord Med 29(3):207–216
Forrest GP (1991) Atrial fibrillation associated with autonomic dysreflexia in patients with tetraplegia. Arch Phys Med Rehabil 72(8):592–594
Verrier RL, Antzelevitch C (2004) Autonomic aspects of arrhythmogenesis: the enduring and the new. Curr Opin Cardiol 19(1):2–11
Guttmann L, Whitteridge D (1947) Effects of bladder distension on autonomic mechanisms after spinal cord injuries. Brain 70(Pt 4):361–404
Colachis SC 3rd, Clinchot DM (1997) Autonomic hyperreflexia associated with recurrent cardiac arrest: case report. Spinal Cord 35(4):256–257
Frankel HL, Mathias CJ, Spalding JM (1975) Mechanisms of reflex cardiac arrest in tetraplegic patients. Lancet 2(7946):1183–1185 (Pii S0140-6736(75)92662-8)
Collins HL, DiCarlo SE (2002) TENS attenuates response to colon distension in paraplegic and quadriplegic rats. Am J Physiol Heart Circ Physiol 283(4):H1734–H1739
Weaver LC, Marsh DR, Gris D, Brown A, Dekaban GA (2006) Autonomic dysreflexia after spinal cord injury: central mechanisms and strategies for prevention. Prog Brain Res 152:245–263
Antzelevitch C, Shimizu W, Yan GX, Sicouri S, Weissenburger J, Nesterenko VV, Burashnikov A, Di Diego J, Saffitz J, Thomas GP (1999) The M cell: its contribution to the ECG and to normal and abnormal electrical function of the heart. J Cardiovasc Electrophysiol 10(8):1124–1152
Antzelevitch C (2001) Tpeak-Tend interval as an index of transmural dispersion of repolarization. Eur J Clin Invest 31(7):555–557
Panikkath R, Reinier K, Uy-Evanado A, Teodorescu C, Hattenhauer J, Mariani R, Gunson K, Jui J, Chugh SS (2011) Prolonged Tpeak to Tend interval on the resting electrocardiogram is associated with increased risk of sudden cardiac death. Circ Arrhythm Electrophysiol 4:441–447
Piccirillo G, Cacciafesta M, Lionetti M, Nocco M, Di Giuseppe V, Moise A, Naso C, Marigliano V (2001) Influence of age, the autonomic nervous system and anxiety on QT-interval variability. Clin Sci (Lond) 101(4):429–438
Dilaveris PE, Gialafos JE (2001) P-wave dispersion: a novel predictor of paroxysmal atrial fibrillation. Ann Noninvasive Electrocardiol 6(2):159–165
Dilaveris PE, Gialafos JE (2001) P-wave duration and dispersion analysis: methodological considerations. Circulation 103(21):e111
Chung FP, Hu YF, Chao TF, Higa S, Cheng H, Lin YJ, Chang SL, Lo LW, Tuan TC, Tai CT, Li CH, Lin YK, Chen SA (2011) The correlation between ventricular repolarization and clinical severity of spinal cord injuries. Heart Rhythm 8(6):879–884
Marino RJ, Barros T, Biering-Sorensen F, Burns SP, Donovan WH, Graves DE, Haak M, Hudson LM, Priebe MM (2002) ANSC (2005) International standards for neurological classification of spinal cord injury. J Spinal Cord Med 26(Suppl 1):S50–S56
Alexander MS, Biering-Sorensen F, Bodner D, Brackett NL, Cardenas D, Charlifue S, Creasey G, Dietz V, Ditunno J, Donovan W, Elliott SL, Estores I, Graves DE, Green B, Gousse A, Jackson AB, Kennelly M, Karlsson A-K, Krassioukov A, Krogh K, Linsenmeyer T, Marino R, Mathias CJ, Perkash I, Sheel AW, Shilero G, Schurch B, Sonksen J, Stiens S, Wecht J, Wuermser LA, Wyndaele J–J (2009) International standards to document remaining autonomic function after spinal cord injury. Spinal Cord 47(1):36–43
Cariga P, Catley M, Mathias CJ, Savic G, Frankel HL, Ellaway PH (2002) Organisation of the sympathetic skin response in spinal cord injury. J Neurol Neurosurg Psychiatr 72(3):356–360
Claydon VE, Krassioukov AV (2006) Orthostatic hypotension and autonomic pathways after spinal cord injury. J Neurotrauma 23(12):1713–1725
Claydon VE, Steeves JD, Krassioukov A (2006) Orthostatic hypotension following spinal cord injury: understanding clinical pathophysiology. Spinal Cord 44(6):341–351
Bazett H (1920) An analysis of the time-relations of electrocardiograms. Heart 7:353–370
La Fountaine MF, Wecht JM, Rosado-Rivera D, Cirnigliaro CM, Spungen AM, Bauman WA (2011) The QT variability index and cardiac autonomic modulation: perspectives from apparently healthy men with spinal cord injury. Cardiology 117(4):253–259
Acknowledgments
We are grateful to Mr Inderjeet Sahota and Mr Brett Shaw for their assistance with this project. This work was supported by funding from the Heart and Stroke Foundation of Canada, the Christopher and Dana Reeve Foundation, and Simon Fraser University.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ravensbergen, H.J.C., Walsh, M.L., Krassioukov, A.V. et al. Electrocardiogram-based predictors for arrhythmia after spinal cord injury. Clin Auton Res 22, 265–273 (2012). https://doi.org/10.1007/s10286-012-0166-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10286-012-0166-6