Abstract
Introduction
Spinal cord injury (SCI) is commonly associated with devastating paralysis. This condition also results in cardiovascular autonomic dysfunction associated with increased mortality from cardiovascular disease. The purpose of this study was to explore the differences in cardiovascular autonomic modulation in individuals with and without SCI.
Methods
The study included 60 individuals: 30 individuals without SCI, who formed the control group—CG and 30 individuals with SCI, who formed the SCI group—SCIG. The latter group was divided into two, one group of subjects with SCI above the spinal segment T6—SCIG (above T6) and a group of individuals with SCI below T6—SCIG (below T6). The subjects were evaluated by linear and nonlinear analysis of heart rate variability (HRV).
Results
The SCIG showed significantly lower square root of the mean squares differences of successive NN intervals (rMSSD), number of pairs of adjacent NN intervals differing by more than 50 ms (pNN50), standard deviation of short-term HRV (SD1), and high frequency power (HF). Their low frequency power (LF) in absolute units (ms2) was significantly lower and their normalized units (n.u.) were significantly higher. Their LF/HF ratio was significantly higher, and sample entropy (SampEn), which indicates the complexity and irregularity of the NN intervals time series, was significantly lower compared to the CG. The differences between the SCIG and CG were derived mainly from the SCIG (above T6). The correlation test revealed very low values between each of the parameters evaluated for CG and SCIG.
Conclusions
The SCIG (above T6) showed greater cardiovascular autonomic impairment compared to SCIG (below T6) and CG. The SCIG (below T6) also presented some degree of autonomic dysfunction. All parameters, linear or nonlinear, are suitable to demonstrate the differences between the SCIG and CG.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
According to the World Health Organization [1] about 500 million new cases of spinal cord injury (SCI) occur every year. The disconnection of processing and bundles of nerve fibers responsible for descending communication on the spinal cord result in sensory and motor impairment as well as autonomic control impairment of internal organs such as the heart [2].
Heart rate variability (HRV) is considered a tool with great potential to quantify the residual cardiovascular sympathovagal regulation after SCI [3] and was highly reproducible in this population [4]. Studies have shown that cardiovascular sympathetic control in SCI above spinal segment T6 is impaired or even absent [3, 5–10]. Consequently, cardiovascular disorders may occur such as: reduced heart rate variability (HRV), low frequency power (LF), RR intervals, delay cardiac baroreflex [11], bradycardia, arterial hypotension, and autonomic dysreflexia [5].
Although sympathetic innervation is preserved in SCI below T6, there may be autonomic control disorders, such as decreased high frequency power (HF) [11] and lower square root of the mean of the sum of the squares of differences between adjacent NN intervals (rMSSD) [12].
Previous studies on cardiovascular autonomic modulation in individuals who have suffered SCI used smaller samples, n = 1 [5] and n = 26 [6], evaluated only quadriplegics [10] or only paraplegics [13, 14]. Moreover, for HRV analysis, some authors used only linear methods [3, 6, 9, 11] considered inadequate to analyze signs with nonlinear behavior such as HRV [15]. Therefore, additional information is required which can be used as the basis for future experimental studies that address, for example, preventive sports programs for cardiovascular disease in this population.
The autonomic control disorders associated with paralysis and hence to a sedentary lifestyle result in increased morbidity and mortality from cardiovascular disease in individuals with SCI [8, 12]. Early detection and characterization of autonomic dysfunction in individuals with SCI are extremely relevant for determining treatment. According to Myers et al. [16], the degree of autonomic dysfunction is an important indicator of physical functions and general health in a person with SCI.
Therefore, the objectives of this study were to explore the differences in cardiovascular autonomic modulation between individuals with and without SCI, analyze the autonomic behavior in people with SCI above and below T6, and identify which of the HRV parameters evaluated are more sensitive in detecting abnormalities in individuals with SCI.
Methods
This clinical trial, a controlled cross-sectional study, was approved by the Human Research Ethics Committees of Universidade do Vale do Paraíba (UNIVAP), number 18353613.0.0000.5503, and registered in the Clinical Trials, protocol number NCT02177929. The subjects read and signed the informed consent.
Subjects
The study included 60 subjects, divided equally into two groups: control group (CG) consisting of individuals without neurological affections, and spinal cord injury Group (SCIG), made up of individuals with traumatic SCI. The SCIG was subdivided into two groups: a group of individuals with SCI above spinal segment T6—SCIG (above T6) and a group of individuals with SCI below T6—SCIG (below T6). To determine the level of spinal cord injury, individuals previously undergone a physical examination based on the evaluation of dermatomes and myotomes established by the American Spinal Injury Association.
Inclusion criteria were: age between 18 and 50, this age group was chosen because previous epidemiological studies of patients who have suffered LM in the region used subjects from 20 to 40 years [17] and 18 to 74 years [18]; therefore, this strategy would facilitate the selection of the sample. Other inclusion criteria considered included no cardiovascular abnormalities, or risk factors, such as hypertension, diabetes, or obesity, or use of cardiac depressant or stimulatory medications. The group of people with SCI had complete or incomplete thoracic or cervical SCI, clinical stability and more than 8 months after injury. By this time, type I and type II muscle fiber atrophy was considered to have occur 7–8 months after LM [19], and spasticity is usually established 2–6 months after injury [20].
Exclusion criteria were athletes and pregnant women. The group with SCI also could not have urine infection or severe pressure ulcers.
Subjects were classified as sedentary if they practiced physical activity for 2 h or less per week and active if they practiced 3 or more hours per week [13].
The study sample was composed mostly of males, which reduced the interference of hormonal changes of the menstrual cycle on the cardiovascular autonomic control. According to Yildirir et al. [21] and Sato et al. [22], the LF power and LF/HF ratio are higher in the luteal phase, indicating increased sympathetic activity at this stage of the menstrual cycle, while in the follicular phase, the HF power is greater, indicating increased parasympathetic activity at this stage.
The study sample is characterized in Table 1.
ECG data acquisition
All subjects were evaluated by HRV. For this, the intervals between R waves of the electrocardiogram (RRi) so-called normal-to-normal (NN) intervals were obtained by a Polar® RS800CX with a sampling rate of 1000 Hz [23].
The strap heart monitor was positioned below the pectoral muscle of individuals who remained seated during collection. Data collection was performed for 7 min, preceded by at least 2 min of rest. The subjects were instructed to breathe spontaneously throughout the procedure. The sitting position was chosen because, due to the extensive functional loss after SCI, affected individuals use a wheelchair and remain in the seated position most of the time [13].
Data analysis
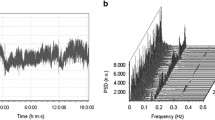
The acquired data were transferred to a microcomputer equipped with Polar ProTrainer software. First, to remove artifacts, signals were filtered using an automatic adaptive filter, developed by Santos et al. [23]. The filter is based on the adaptation of the average and standard deviation values, following the series without interfering variability in the characteristics of the data. Subsequently, the signals were analyzed by linear (time domain and frequency) and nonlinear (Poincaré plot, and sample entropy) methods, using Kubios HRV Analysis® software.
For temporal analysis, the following variables were obtained: RRi; standard deviation of the NN intervals (SDNN), which represent the sympathetic and parasympathetic modulation; square root of the mean squares differences of successive NN intervals (rMSSD); and number of pairs of adjacent NN intervals differing by more than 50 ms (pNN50). The latter two indices are related to the parasympathetic modulation [24].
For spectral analysis, Fast Fourier Transform (FFT) was used to obtain the variables: low frequency power (LF: 0.04–0.15 Hz) which for some authors is related only to sympathetic modulation [25] and for others is both sympathetic and parasympathetic activity [26]; high frequency (HF: 0.15–0.4 Hz) representing the parasympathetic activity; and LF/HF ratio which is related to the sympathovagal balance. The LF and HF power were expressed in both absolute (ms2) and normalized units (n.u.). Normalized units are obtained by dividing the power of a given component (LF or HF) by the total power minus the VLF power.
Using Poincaré plot, the standard deviation of short-term HRV (SD1), and the standard deviation of long-term HRV (SD2) were obtained. Furthermore, the Poincare map allows visual analysis which summarizes the short and long-term levels of the series of RR intervals in a figure. This map consists of plotting each RR interval in relation to the next interval to produce a set of coordinate points (RRi, RRi + 1) [27].
Analysis by sample entropy (SampEn) indicates the complexity and irregularity of the RRi time series. The length (m) of the subseries and the tolerance (r) were fixed at m = 2 and r = 0.2 [28]. This type of entropy was chosen because of its better performances on short-term time series data [29]. The complexity of heart rate (HR) by entropy can be a general marker of sympathovagal interaction; therefore, its increase reflects an improvement in the sympathovagal balance [30].
The first 2 min was excluded from the time series. The analysis was performed with the last 5 min, which for the Task Force [30] is suitable for short recording time.
Statistical analysis
Data normality was verified using the D’Agostino test and extreme value. To compare the averages of the parameters between the CG and SCIG, Student’s t test or the Mann–Whitney was used. To compare the averages of the parameters between the CG, SCIG (above T6), and SCIG (below T6), the ANOVA test or Kruskal–Wallis test was used. Statistical significance was set at p < 0.05. In addition, the degree of correlation of the parameters evaluated between the CG and SCIG was assessed by the Pearson’s correlation coefficient.
Results
There were no statistically significant differences between groups for the evaluated physical characteristics (age, weight, height, and BMI).
Comparisons of the means of HRV parameters evaluated between the CG and SCIG showed a statistically significant difference for most parameters, except for SDNN and SD2. The SCIG had significantly lower rMSSD, pNN50, SD1, and HF in ms2 or in n.u., which reflect the parasympathetic activity. The LF power was significantly lower in ms2 and n.u. It was significantly higher in the SCIG compared to CG. The LF/HF ratio was significantly higher, and sample entropy (SampEn) was significantly lower in the SCIG compared to the GG (Table 2).
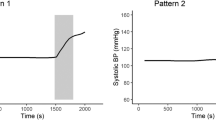
Comparisons of the means of HRV parameters evaluated between CG, SCIG (above T6), and SCIG (below T6) revealed that the differences between the CG and SCIG were attributed mainly to the SCIG (above T6) groups, as shown in Figs. 1, 2, and 3.
The visual analysis of Poincaré plot shows a growing dispersion of SCIG (above T6) to CG (Fig. 4).
Pearson’s test showed very low correlation values between the evaluated parameters for CG and SCIG, demonstrating that there is no correlation between evaluated parameters (Table 3).
Discussion
The results showed an LF power in ms2 lower in the SCIG compared to control. Comparisons of the averages of the parameters evaluated between CG, SCIG (above T6), and SCIG (below T6) revealed that this difference was attributed, especially in the SCIG (above T6), who showed lower LF power (ms2), which reflects in lower sympathetic activity. This finding corroborates that of Malmqvist et al. [3]; Oh and Eun [5]; Jan et al. [6]; Caldeira et al. [7]; Krassioukov [8]; Inoue et al. [9], who found that a reduction of LF, especially in the SCI above T6, and assign this to interruption of neuronal pathways that connect the supraspinatus command to the cardiovascular peripheral sympathetic control.
However, the LF power in n.u. was higher in the SCIG compared to control, and similarly, the means of comparison of the parameters measured between the CG, SCIG (above T6), and SCIG (below T6) revealed that difference was attributed mainly to the SCIG (above T6). Similar results were not found in the literature. However, when performing normalization of spectral powers removed the influence of the very low frequency (VLF) power, which for Delaney et al. [31] is associated with the renin-angiotensin-aldosterone system and thermoregulatory mechanisms, sometimes altered in people with SCI [32, 33].
In people with SCI, especially above T6, control of blood pressure is extremely dependent on high levels of plasma renin. In these people, the renin levels increase much more and faster in response to a postural change from the supine to the standing position compared to control. In this case, renin release ceases to be mediated by the sympathetic nervous system and becomes dependent on renal baroreceptors [34–36]. Due to the elevation in plasma rennin activity, there is a late rise in plasma aldosterone [36].
Corroborating this finding, a study by Kawasaki et al. [37] showed in SCI patients na attenuated increase in plasma adrenaline and an increase in plasma aldosterone during exercise compared with controls. These findings suggested that this could be because of adaptation to a disordered sympathetic nervous system.
Moreover, in SCI above T6, more than half the body loses the hypothalamic-friendly descendant control responsible for thermoregulatory mechanisms such as poikilothermia (inability to maintain a constant core temperature), piloerection, tremor, peripheral vasoconstriction and cutaneous heat or sweating, cutaneous vasodilation to reduce the temperature, which can cause severe thermal dysfunction. This is largely due to reduced sensory input to thermo-regulating centers and the loss of sympathetic control of temperature and sweat regulation below the level of injury [33, 38]. Although thermoregulation is recognized as an autonomic function, the precise mechanisms of dysregulation have not been fully elucidated [39].
Therefore, the increase in LF power in n.u. SCIG can reflect the great influence of the renin-angiotensin-aldosterone system and the thermoregulatory mechanisms, showing that this power not only reflects the sympathetic activity in people with SCI. The physiological effects of SCI on renin-angiotensin-aldosterone system and thermoregulatory mechanisms and its influence on the components of HRV require additional investigation.
In addition, greater LF/HF ratio and lower sample entropy (SampEn) were found in SCIG, especially in SCIG (above T6), which represent an impaired sympathovagal balance [15, 40]. These results corroborate Inoue et al. [9], who found a LF/HF ratio higher in quadriplegic patients compared to the control. The higher the value of this ratio, the greater the sympathetic predominance [26], but as SCI above T6 is sympathetic interruption, one should be cautious about interpreting this parameter for this population.
The results also showed reduced parasympathetic activity in SCIG (rMSSD, pNN50, SD1, and HF in ms2 or n.u.) compared to CG. According to Inoue et al. [9], the reduction of HF power may offset the lack of sympathetic activity. A study by Aysin and Aysin [41] showed a predominance of parasympathetic activity during deep breathing. Because quadriplegics with SCI below C5 have shallow breathing due to respiratory muscle weakness, as the intercostal, this can influence the spectral power of the HF power [9].
The data from this study corroborate Claydon and Krassioukov [11] and Bunten et al. [42], who found in individuals with SCI sympathetic and parasympathetic neurocardiac impairment, which is more in cervical SCI and minimum in thoracic and lumbar SCI. Similarly, our data show similarities with the studies of Caldeira et al. [7] in tetraplegics and Serra-Año et al. [13] in paraplegics.
Serra-Año et al. [13] believe that parasympathetic cardiac autonomic dysfunction in people with SCI below T6 can occur due to immobility, associated with impairment of the venous pump of the paralyzed muscles, which is associated with confinement in a wheelchair and a sedentary lifestyle.
For Claydom and Krassioukov [11], the abnormal cardiovascular regulation post-SCI is related to the level of the injury and severity of the autonomic pathways. According to Jan et al., in cervical or high-thoracic (above T6) SCI, the cardiovascular system loses sympathetic innervation. However, the results of this study show that the components that reflect the sympathetic modulation (LF, SD2) have not disappeared in SCIG (above T6), even in complete injuries. These findings corroborate those from Claydom and Krassioukov [11], who highlighted some hypotheses: the sympathetic oscillations can occur even in the absence of downward sympathetic control from spinal sympathetic neurons; the LF component may be mediated by parasympathetic mechanisms; and the destruction of sympathetic descending pathways may have been incomplete. This shows that the level of sensory and motor damage may not correspond to the level of autonomic injury.
The Poincaré figures allow a better view of the differences between individuals in CG, SCIG (above T6), and SCIG (below T6). They revealed an autonomic dysfunction present in an individual in the SCIG (above T6), as expected due to sympathetic denervation, but also showed an autonomic impairment in an individual in the SCIG (below T6). In addition, despite having no significant differences for most of the parameters evaluated between the CG and SCIG (below T6), RRi were lower in this group. In addition, there was a greater dispersion of the Poincaré plot in the CG, then the SCIG (below T6), and finally the SCIG (above T6). According to Serra-Año et al. [13], a greater dispersion of the points is related to a good autonomic balance, whereas a narrow dispersion indicates autonomic imbalance, usually associated with the predominance of sympathetic activity.
Studies have pointed out that some indexes of HRV can detect autonomic changes from SCI with better sensitivity and specificity. Significant results were found by Merati et al. [15], Millar et al. [28], and Agiovlasitis et al. [40] using nonlinear methods such as entropy, but without changes in linear measurements (LF, HF, and LF/HF). Therefore, the present study analyzed the HRV using linear and nonlinear methods. Unlike previous studies, significant differences were found between CG and SCIG for most of the evaluated parameters. In addition, the Pearson’s test correlation revealed very low levels of each of the parameters for CG and SCIG, suggesting that all linear (time and frequency domain) or nonlinear (Poincare plot and sample entropy) parameters can be used to demonstrate the differences in cardiovascular autonomic behavior in people with and without SCI.
Differences between the SCIG (above T6) and SCIG (below T6) show that during the clinical strategies in the cardiovascular rehabilitation programs, the decrease in sympathetic activity, especially in the SCIG (above T6), can lead to a difficulty in accelerating the HR during physical exertion, so this parameter is not the most appropriate in the prescription of exercises.
In addition, the literature shows that SCI was associated with significantly increased odds of heart attack, stroke [43], and type 2 diabetes, irrespective of known risk factors for type 2 diabetes [44]. The deregulation of the autonomic nerve system could be involved in the pathophysiology of these diseases. On the other hand, studies show the benefits of exercise training in people with SCI. Nash et al. [45] demonstrated that electrically stimulated physical training (1 month of electrical stimulation of the quadriceps and 6 months electrostimulation of quadriceps, hamstrings, and glutes associated with the cycle ergometer) can reverse left ventricular atrophy in tetraplegic individuals, and that the changes in cardiac architecture are likely to be the result of both pressure and volume challenge to the heart imposed by exercise.
Further studies should be carried out to define the physiological mechanisms of autonomic impairment after SCI, to identify the effects of different therapeutic interventions, such as sport, to enable greater security to conduct the rehabilitation process of affected individuals and establishment guidelines for prescription of exercise.
Conclusions
The SCIG showed less sympathetic (LF in ms2) and parasympathetic activity (rMSSD, pNN50, HF in ms2 or n.u., SD1) and consequently compromised sympathovagal balance (LF/HF, SampEn) compared to CG. These differences were attributed, particularly, in the SCIG (above T6). Moreover, the larger LF power in n.u. of the SCIG may reflect the influence of changes of the renin-angiotensin-aldosterone system and the thermoregulatory mechanisms.
The reduction of sympathetic activity may be related to the interruption of sympathetic pathways originating from spinal segments T1 to T5. The reduction in parasympathetic activity may be related to sedentary lifestyle acquired after SCI. Therefore, the SCIG (above T6) may present greater risk of morbidity and mortality by cardiovascular diseases. However, the SCIG (below T6) also presented some degree of autonomic dysfunction, such as shorter RRi and less dispersion in the Poincaré plot, which also deserves clinical attention.
All reviews, linear or nonlinear parameters were adequate to demonstrate the differences between the CG and SCIG, except for SDNN and SD2, which showed no significant differences between groups. Therefore, it was not possible to clearly identify which of the HRV parameters are more sensitive in detecting abnormalities in patients with SCI.
References
World Health Organization, The International Spinal Cord Society. International Perspectives on Spinal Cord Injury. World Health Organization; 2013 http://apps.who.int/iris/bitstream/10665/94190/1/9789241564663_eng.pdf. Accessed 26 May 2015
Thuret S, Moon LDF, Gage FH (2006) Therapeutic interventions after spinal cord injury. Nat Rev Neurosci 7:628–643. doi:10.1038/nrn1955
Malmqvist L, Biering-Sørensen T, Bartholdy K, Krassioukov A, Welling K-L, Svendsen JH et al (2015) Assessment of autonomic function after acute spinal cord injury using heart rate variability analyses. Spinal Cord 53:54–58. doi:10.1038/sc.2014.195
Ditor DS, Kamath MV, Macdonald MJ, Bugaresti J, McCartney N, Hicks AL (2005) Reproducibility of heart rate variability and blood pressure variability in individuals with spinal cord injury. Clin Auton Res 15(6):387–93
Oh YM, Eun JP (2015) Cardiovascular dysfunction due to sympathetic hypoactivity after complete cervical spinal cord injury: a case report and literature review. Medicine 94(12):e686. doi:10.1097/MD.0000000000000686
Jan Y-K, Anderson M, Soltani J, Burns S, Foreman RD (2013) Comparison of changes in heart rate variability and sacral skin perfusion in response to postural changes in people with spinal cord injury. J Rehabil Res Dev (JRRD) 50(2):203–14. http://dx.doi.org/10.1682/JRRD.2011.08.0138
Caldeira JB, Sancho AG, Manoel F, Almeida Júnior N, Faria D, Rosa JLS, Nemer SN (2012) Avaliação da função autonômica cardiovascular em portadores de lesão medular através dos índices de Valsalva e da arritmia sinusal respiratória. Rev Bras Cardiol 25(2):118–125
Krassioukov A (2009) Autonomic function following cervical spinal cord injury. Respir Physiol Neurobiol 169(2):157–64. doi:10.1016/j.resp.2009.08.003
Inoue K, Ogata H, Hayano J, Miyake S, Kamada T, Kuno M, Kumashiro M (1995) Assessment of autonomic function in traumatic quadriplegic and paraplegic patients by spectral analysis of heart rate variability. J Auton Nerv Syst 54(3):225–234
Inoue K, Miyake S, Kumashiro M, Ogata H, Yoshimura O (1990) Power spectral analysis of heart rate variability in traumatic quadriplegic humans. Am J Physiol 258(6Pt2):H1722–6
Claydon VE, Krassioukov AV (2008) Clinical correlates of frequency analyses of cardiovascular control after spinal cord injury. Am J Physiol Heart Circ Physiol 294:H668–H678. doi:10.1152/ajpheart.00869.2007
Rosado-Rivera D, Radulovic M, Handrakis JP, Cirnigliaro CM, Jensen AM, Kirshblum S et al (2011) Comparison of 24-hour cardiovascular and autonomic function in paraplegia, tetraplegia, and control groups: implications for cardiovascular risk. J Spinal Cord Med 34(4):395–403. doi:10.1179/2045772311Y.0000000019
Serra-Año P, Montesinos LL, Morales J, López-Bueno L, Gomis M, García-Massó X et al (2015) Heart rate variability in individuals with thoracic spinal cord injury. Spinal Cord 53(1):59–63. doi:10.1038/sc.2014.207
Uhlíř P, Opavský J, Zaatar A, Betlachová M (2010) Spectral analysis of heart rate variability in patients with spinal cord injury. Acta Univ Palacki Olomuc Gymn 40(2):55–62
Merati G, Di Rienzo M, Parati G, Veicsteinas A, Castiglioni P (2006) Assessment of the autonomic control of heart rate variability in healthy and spinal-cord injured subjects: contribution of different complexity-based estimators. IEEE Trans Biomed Eng 53(1):43–52. doi:10.1109/TBME.2005.859786
Myers JN, Hsu L, Hadley D, Kiratli BJ (2010) Post-exercise heart rate recovery in individuals with spinal cord injury. Spinal Cord 48(8):639–44. doi:10.1038/sc.2009.196
Botelho RV, Abgussen CMB, Furtado GC, Machado P, Elias AJR, Benedito-Silva AA et al (2001) Epidemiologia do trauma raquimedular cervical na zona norte da cidade de São Paulo. Arq Bras Neurocir 20(3–4):64–76. doi:10.1590/S0100-69912008000200005
Salomão AF, Soares PN, Lucareli PRG, Freitas STT, Lima FPS, Lima MO. Estudo epidemiológico dos pacientes com traumatismo raquimedular atendidos na Clínica de Fisioterapia da UNIVAP. Anais do VI Encontro Latino Americano de Iniciação Científica da UNIVAP. 2006. http://www.inicepg.UNIVAP.br/cd/INIC_2006/inic/inic/03/INIC0001290.pdf
Scelsi R (2001) Skeletal muscle pathology after spinal cord injury: our 20 year experience and results on skeletal muscle changes in paraplegics, related to functional rehabilitation. Basic Appl Myol 11(2):75–85
Hiersemenzel LP, Curt A, Dietz V (2000) From spinal shock to spasticity: neuronal adaptations to a spinal cord injury. Neurology 54(8):1574–82. doi:http://dx.doi.org/10.1212/WNL.54.8.1574
Yildirir A, Kabakci G, Akgul E, Tokgozoglu L, Oto A (2002) Effects of menstrual cycle on cardiac autonomic innervation as assessed by heart rate variability. Ann Noninvasive Electrocardiol 7(1):60–63
Sato N, Miyake S, Akatsu J, Kumashiro M (1995) Power spectral analysis of heart rate variability in healthy young women during the normal menstrual cycle. Psychosom Med 57(4):331–335
Santos L, Barroso JJ, Macau EE, Godoy MF (2013) Application of an automatic adaptive filter for Heart Rate Variability analysis. Med Eng Phys 35(12):1778–85. doi:10.1016/j.medengphy.2013.07.009. (Epub 2013 Aug 18)
Pumprla J, Howorka K, Groves D, Chester M, Nolan J (2002) Functional assessment of heart rate variability: physiological basis and practical applications. Int J Cardiol 84(1):1–14
Malliani A (1999) The Pattern of sympathovagal balance explored in the frequency domain. News Physiol Sci 14:111–117
Zaza A, Lombardi F (2001) Autonomic indexes based on the analysis of heart rate variability: a view from the sinus node. Cardiovasc Res 50(3):434–442
Piskorski J, Guzik P (2007) Geometry of the poincar plot of RR intervals and its asym-metry in healthy adults. Physiol Meas 28:287–300
Millar PJ, Rakobowchuk M, Adams MM, Hicks AL, McCartney N, MacDonald MJ (2009) Effects of short-term training on heart rate dynamics in individuals with spinal cord injury. Auton Neurosci 150(1–2):116–21
Lake DE, Richman JS, Griffin MP, Moorman JR (2002) Sample entropy analysis of neonatal heart rate variability. Am J Physiol Integr Comp Physiol 283(3):R789–97
Task Force of the European Society of Cardiology and the North America Society of Pacing and Electrophysiology (1996) Heart rate variability—standarts of measurement, physiological interpretation, and clinical use. Eur Heart J 17(3):354–381
Delaney JP, Leong KS, Watkins A, Brodie D (2002) The short-term effects of myofascial trigger point massage therapy on cardiac autonomic tone in healthy subjects. J Adv Nurs 37(4):364–371
Claydon VE, Steeves JD, Krassioukov AV (2006) Orthostatic hypotension following spinal cord injury: understanding clinical pathophysiology. Spinal Cord. 44(6):341–51
Schmidt K, Chan C (1992) Thermoregulation and fever in normal persons and in those with spinal cord injuries. Mayo Clin Proc 67(5):469–75
Claydon VE, Steeves JD, Krassioukov AV (2006) Orthostatic hypotension following spinal cord injury: understanding clinical pathophysiology. Spinal Cord 44:341–351. doi:10.1038/sj.sc.3101855
Mathias CJ, Christensen NJ. (1980) Rennin release during head–up tilt occurs independently of sympathetic nervous activity in tetraplegic man. Clin Sci 59(4):251–56. doi: 10.1042/cs0590251
Mathias CJ, Christensen NJ (1975) Orthostatic hypotension and autonomic pathways after spinal cord injury. Clin Sci Mol Med 49(4):291–99
Kawasaki T, Nakamura T, Sasaki Y, Sakamoto K, Ito T, Goto M et al. (2012) Renal function and endocrine responses to arm exercise in euhydrated individuals with spinal cord injury. Eur J Appl Physiol 112(4):1537–47. doi 10.1007/s00421-011-2105-y
Karlsson AK, Krassioukov A, Alexander MS, Donovan W, Biering-Sørensen F (2012) International spinal cord injury skin and thermoregulation function basic data set. Spinal Cord 50(7):512–6. doi:10.1038/sc.2011.167
Krassioukov AV, Karlsson AK, Wecht JM, Wuermser LA, Mathias CJ, Marino RJ (2007) Joint Committee of American Spinal Injury Association and International Spinal Cord Society. Assessment of autonomic dysfunction following spinal cord injury: rationale for additions to International Standards for Neurological Assessment. J Rehabil Res Dev 44(1):103–12. doi:10.1682/JRRD.2005.10.0159
Agiovlasitis S, Heffernan KS, Jae SY, Ranadive SM, Lee M, Mojtahedi MC et al (2010) Effects of paraplegia on cardiac autonomic regulation during static exercise. Am J Phys Med Rehabil 89:817–823
Aysin B, Aysin E (2006) Effect of respiration in heart rate variability (HRV) Analysis. Conf Proc IEEE Eng Med Biol Soc 1:1776–1779
Bunten DC, Warner AL, Brunnemann SR, Segal JL (1998) Heart rate variability is altered following spinal cord injury. Clin Auton Res 8(6):329–34
Cragg JJ, Noonan VK, Krassioukov A, Borisoff JF. (2013) Cardiovascular disease and spinal cord injury: results from a national population health survey. Neurology 81(8):723–8
Cragg JJ, Noonan VK, Dvorak M, Mancini GBJ, Borisoff J. (2013) Spinal cord injury and Type 2 Diabetes: results from a population health survey. Neurology 81(21):1864–8
Nash MS, Bilsker S, Marcillo AE, Isaac SM, Botelho LA, John Klose K. (1991) Reversal atrophy exercise of adaptive left ventricular following electrically-stimulated training in human tetraplegics. Paraplegia 29:590–99
Acknowledgments
Abreu EMC thanks CAPES/PROSUP (Ministry of Education, Brazil) for the doctorial fellowship. We would also like to thank to Prof. Dr. Laurita dos Santos (UNIVAP) for providing the adaptive filter.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
de Carvalho Abreu, E.M., Dias, L.P.S., Lima, F.P.S. et al. Cardiovascular autonomic control in paraplegic and quadriplegic. Clin Auton Res 26, 117–126 (2016). https://doi.org/10.1007/s10286-015-0339-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10286-015-0339-1