Abstract
Neurogenic orthostatic hypotension results from failure to release norepinephrine, the neurotransmitter of sympathetic postganglionic neurons, appropriately upon standing. In double blind, cross over, placebo controlled trials, administration of droxidopa, a synthetic amino acid that is decarboxylated to norepinephrine by the enzyme l-aromatic amino acid decarboxylase increases standing blood pressure, ameliorates symptoms of orthostatic hypotension and improves standing ability in patients with neurogenic orthostatic hypotension due to degenerative autonomic disorders. The pressor effect results from conversion of droxidopa to norepinephrine outside the central nervous system both in neural and non-neural tissue. This mechanism of action makes droxidopa effective in patients with central and peripheral autonomic disorders.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Autonomic failure, like Parkinson’s disease, is a neurotransmitter disorder. While Parkinson’s disease is a disorder of dopamine neurotransmission, autonomic failure is a disorder of norepinephrine neurotransmission. The idea that deficient dopamine neurotransmission in Parkinson’s disease could be overcome by treatment with oral levodopa, the amino acid precursor of dopamine, led to the most successful therapeutic intervention in 20th century neurology.
Although levodopa is the amino acid precursor of both dopamine and norepinephrine, treatment with levodopa leads to an increase in dopamine but not to a significant increase in norepinephrine levels. Norepinephrine is synthesized from levodopa in two steps (Fig. 1). The first step is the decarboxylation of levodopa to dopamine by the enzyme l-aromatic amino acid decarboxylase. The second step, catalyzed by the enzyme dopamine beta hydroxylase, is the hydroxylation of dopamine to norepinephrine. Dopamine beta hydroxylase is the rate-limiting enzyme and it creates a “bottle neck” like effect, so that taking levodopa orally results in an increase in dopamine levels but not to a significant increase in norepinephrine levels.
Catecholamine pathway: Norepinephrine is synthesized from levodopa in two steps. The first step is the decarboxylation of levodopa to dopamine by l-aromatic amino acid decarboxylase. The second step is the hydroxylation of dopamine to norepinephrine by the rate-limiting enzyme dopamine beta hydroxylase. Droxipoda bypasses this rate-limiting enzyme and is converted to norepinephrine in a single step by l-aromatic amino acid decarboxylase
Fortunately, the possibility of overcoming this limitation and realizing another therapeutic breakthrough using a precursor amino acid to replace a deficient catecholamine neurotransmitter, in this case norepinephrine, was made possible by the discovery, in the 1950’, that an artificial amino acid, 3,4-threo-dihydroxyphenylserine, identical to levodopa but with an added beta hydroxyl group (Fig. 2) was converted to norepinephrine in a single step by the enzyme l-aromatic amino acid decarboxylase, thus bypassing the need for dopamine beta hydroxylase and its bottle neck effect [3, 15].
Droxidopa was first used successfully to treat one particular form of autonomic failure: congenital deficiency of the enzyme dopamine beta hydroxylase. Robertson and Biaggioni and Man in’t Veld et al. showed that after oral administration, droxidopa was taken up by post-ganglionic sympathetic neurons, decarboxylated to NE, stored and released appropriately when standing up [2, 12]. Droxidopa has now been used to treat orthostatic hypotension in several autonomic disorders, including familial amyloid polyneuropathy [16], autoimmune autonomic neuropathy [5], pure autonomic failure (PAF), Parkinson’s disease and multiple system atrophy [MSA; 4, 10, 11, 13].
3,4-Threo-dihydroxyphenylserine has four steroisomers [1]. Early studies used a racemic mixture that contained both the d and l isoforms of 3,4-threo-dihydroxyphenylserine but only the l-isoform is converted to biologically active l-norepinephrine. Furthermore, the d-stereoisomer of 3,4-threo-dihydroxyphenylserine might competitively inhibit the decarboxylation of the l stereoisomer to l-norepinephrine [8]. Thus, the pure l isoform of 3,4-threo-dihydroxyphenylserine (droxidopa) is the preferred formulation for treatment.
Here I will review the most recent studies conducted in the United States using droxidopa in the treatment of orthostatic hypotension in patients with degenerative autonomic disorders, including PAF and MSA.
Studies of droxidopa in the United States
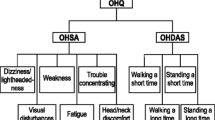
We conducted a comprehensive study of droxidopa in patients with severe symptomatic orthostatic hypotension due to MSA or PAF [11]. We examined the effect of droxidopa on standing blood pressure and orthostatic tolerance, as well as its pharmacokinetics and its mechanism of action.
Dose titration study
Because patients with autonomic failure have different degrees of adrenergic denervation supersensitivity, we individualized the dose of droxidopa for each patient in a single blind dose-ranging study.
Patients received progressively higher dosages of droxidopa, beginning with 200 mg followed by 400, 1,000, 1,600, and 2,000 mg on successive days. The dose ranging study was terminated when the orthostatic fall in systolic blood pressure after 3 min of standing was consistently < 20 mm Hg, or the patient had a sustained supine systolic blood pressure of > 200 mm Hg or diastolic blood pressure of > 110 mm Hg; or when a maximum dose of 2,000 mg of droxidopa was reached. The optimal dose of droxidopa varied between 200 mg and 2,000 mg (mean dose ± SE was 1,137 ± 131 mg).
Double blind, crossover, placebo controlled study
Once the individual dose of droxidopa was determined, patients were enrolled in a double blind crossover study lasting 3 days. On days 1 and 3 either droxidopa (at the dose previously determined in the dose ranging study) or placebo was given at 7:00 am. Day 2 was a washout day. As shown in Fig. 3 administration of droxidopa significantly increased blood pressure in all patients (P < 0.001 versus placebo), both while supine and after standing for 1 min and for 3 min.
Standing blood pressure after droxipoda and placebo administration. The effect of droxipoda and placebo on mean arterial pressure (MAP) after 3 min standing. Time 0 (arrow) represents the time of drug administration (7 am). Meals were served at -1 (6 am) and 6 h (1 pm). *P < 0.05 (l-DOPS vs. placebo). All data are mean ± SEM, (n = 19). Data from Kaufmann et al. [11]
The pressor effect began 1 h after droxidopa administration and lasted for 6 h while standing and for 8 h while supine. The highest standing blood pressure occurred 3.5 h after droxidopa administration (P < 0.00001 versus placebo, see Fig. 3). There were no significant changes in heart rate following administration of droxidopa or placebo.
There was a clear symptomatic improvement in all patients after taking droxidopa. Patients were less lightheaded and reported feeling better. This was noticeable in the patient’s ability to stay standing. Patients were able to stand for the 1-min blood pressure determination 96% of the time after receiving either droxidopa or placebo. However, for the 3-min blood pressure measurement, patients were able to stand 94% of the time after receiving droxidopa but only 84% of the time after receiving placebo (P < 0.001).
Adverse events
Droxidopa was well tolerated by all patients and there were no significant side effects. The frequency of supine hypertension (systolic pressure > 180, diastolic > 110 mmHg or both) was higher on droxidopa than on placebo (45% vs. 23% of blood pressure measurements, P < 0.00001). After receiving droxidopa, the frequency of supine systolic and diastolic hypertension was similar in MSA and PAF patients. However, on placebo, diastolic, but not systolic, supine hypertension was more common in MSA patients than in PAF (25% vs. 3%, P < 0.05). One patient had hyponatremia, which reversed after saline infusion. Another patient had transitory chest pain with electrocardiographic ST segment depression, but cardiac enzymes were normal.
Mechanism and site of action of droxidopa
Droxidopa could exert its pressor effect in three different ways [9] (Fig. 4):
-
1.
As a central stimulator of sympathetic activity. Because droxidopa crosses the blood brain barrier, it could, at least theoretically, act as a central stimulator of sympathetic outflow. It could be converted to epinephrine and activate sympathetic preganglionic neurons in the spinal cord.
-
2.
As a peripheral sympathetic neurotransmitter. As it had been shown in patients with dopamine beta hydroxylase (DBH) deficiency [2, 12] droxidopa could be taken up by post ganglionic peripheral sympathetic neurons, transformed to norepinephrine intraneuronally, and released when sympathetic neurons are activated, i.e., act as a physiologic sympathetic neurotransmitter in peripheral sympathetic neurons.
-
3.
As a circulating hormone. Norepinephrine synthesized from droxidopa could also act as a circulating hormone. The enzyme aromatic aminoacid decarboxylase is widely expressed throughout the body, in the stomach, kidney and liver. Thus, droxidopa could be converted to norepinephrine outside neurons, and then released into the blood stream were it would exert a pressor effect as a circulating hormone.
Possible mechanisms of action of droxidopa—Droxidopa could exert its pressor effect in three ways: 1. Because droxidopa crosses the blood brain barrier, it could be converted to epinephrine and activate sympathetic preganglionic neurons in the spinal cord. 2. Droxidopa could be taken up by post ganglionic sympathetic neurons, converted to norepinephrine intraneuronally, and released when sympathetic neurons are activated. 3. Droxidopa could be converted to norepinephrine outside neurons (in the stomach, kidney and liver), released into the blood stream and exert a pressor effect as a circulating hormone
Decarboxylase inhibitior study
To determine whether the pressor action of droxidopa was due to its metabolism to norepinephrine inside or outside the central nervous system we used carbidopa as a pharmacological probe [11]. Carbidopa is an inhibitor of l-aromatic-amino-acid decarboxylase that does not cross the blood-brain barrier. Therefore, carbidopa’s inhibition of l-aromatic-amino-acid decarboxylase and its blockade of norepinephrine synthesis from droxidopa is confined to tissues outside the brain and it does not affect the decarboxylation of droxidopa to norepinephrine within the central nervous system.
If the mechanism of action of droxidopa is in the central nervous system, a large dose of carbidopa taken before droxidopa should not prevent its pressor effect. Indeed, it may even increase its pressor effect, similarly to the enhanced anti parkinsonian effect of levodopa when it is administered with carbidopa. Conversely, if the mechanism of action of droxidopa is through its conversion to norepinephrine outside the central nervous system, either in neural or non-neural tissue, then concomitant administration of carbidopa will block the pressor effect of droxidopa.
In a double-blind placebo controlled study, six patients [11] sequentially received droxidopa alone on day 1, 200 mg of carbidopa alone on day 2, and 200 mg of carbidopa combined with droxidopa on day 3.
As expected, droxidopa taken alone increased standing blood pressure in all patients. Carbidopa taken alone had no effect on blood pressure. However, when carbidopa was administered together with droxidopa the increase in blood pressure previously seen with droxidopa alone was completely abolished (Fig. 5). From this study we concluded that the pressor effect of droxidopa was due to it conversion into norepinephrine outside the brain, either in neuronal or non-neuronal tissues.
Droxidopa plus decarboxylase inhibitior study. The effect of droxipoda, decarboxylase inhibitior (DCI), droxidopa and DCI, and placebo on mean arterial pressure (MAP) after 3 min standing. Time 0 (arrow) represents the time of drug administration (7 am). Meals were served at −1 (6 am) and 6 h (1 pm). *P < 0.05 (versus placebo). All data are mean ± SEM, (n = 6). Data from Kaufmann et al. [11]
After carbidopa administration plasma levels of droxidopa were higher than when droxidopa was administered without carbidopa (4,556 ± 1,011 ng/ml, P < 0.01, versus droxidopa alone). In addition, carbidopa markedly attenuated the increase in plasma norepinephrine levels. Six hours after concomitant carbidopa and droxidopa administration, the venous plasma norepinephrine level had only increased from 216 ± 125 to 407 ± 271 pg/ml (P < 0.05, versus droxidopa alone).
Droxidopa in patients with PD taking levodopa and a decarboxylase inhibitor
Levodopa/carbidopa therapy is a mainstay in the treatment of Parkinson disease. Because carbidopa inhibits the conversion of droxidopa to norepinephrine, droxidopa may be ineffective in the treatment of orthostatic hypotension in patients with Parkinson disease treated with levodopa/carbidopa. However, to block the pressor effect of droxidopa it is necessary to completely inhibit the enzyme aromatic aminoacid decarboxylase. To achieve complete inhibition of aromatic aminoacid decarboxylase a high dose of carbidopa (200 mg) is required. Lower dosages of carbidopa, such as those commonly used to treat Parkinson disease, should not abolish the pressor effect of droxidopa. Indeed, studies of droxidopa in Europe included patients with PD who were also taking benzeraside, an aromatic aminoacid decarboxylase inhibitor, at a low dose, together with levodopa (i.e., Madopar, see Mathias, this supplement). Because benzerazide at a low dose does not completely inhibit the enzyme aromatic aminoacid decarboxylase, patients with PD still experienced the desired pressor effect of droxidopa.
Therapeutic implications
A peripheral mechanism of action makes droxidopa an exciting new treatment option in both central and peripheral autonomic disorders. In patients with destruction of peripheral autonomic neurons (i.e., in the Lewy body disorders), droxidopa can be converted to norepinephrine in non-neuronal tissues, released to the blood stream and act as a circulating vasoconstrictor hormone. In patients with central autonomic disorders and preserved peripheral autonomic neurons (i.e., MSA), droxidopa is converted to norepinephrine outside the central nervous system, both in neuronal and non-neuronal tissue. In these patients, droxidopa-derived norepinephrine acts as a neurotransmitter and a circulating hormone.
Pharmacokinetic study
We investigated the pharmacokinetics of droxidopa and the generated norepinephrine and determined the relationship between the pressor response and venous plasma norepinephrine levels [6, 11]. The peak droxidopa level of 1,942 ± 224 ng/ml was attained 3 h after its ingestion (P < 0.001). Plasma norepinephrine increased from the baseline level of 294 ± 80 pg/ml to 806 ± 235 pg/ml (P < 0.05) 2 h after droxidopa admi nistration. Norepinephrine peaked at 1,250 ± 208 pg/ml 6 h after droxidopa ingestion (P < 0.005, see Fig. 6). Plasma levels of norepinephrine remained significantly elevated for at least 46 h. The levels of norepinephrine associated with an increase in blood pressure were above 700 pg/ml (see Fig. 7), similar to the norepinephrine levels necessary to increase blood pressure when norepinephrine is infused.
Plasma levels of droxipoda and norepinephrine. Venous plasma levels of droxipoda and norepinephrine after droxidopa administration (Time 0, 7 am). Meals were served at −1 (6 am) and 6 h (1 pm). All data are mean ± SEM, (n = 8). Data from Kaufmann et al. [11]
Relationship between blood pressure and norepinephrine levels after droxidopa administration. Changes in systolic blood pressure (SBP) versus plasma concentration of norepinephrine after droxidopa administration. Solid curve represents the line of best fit. All data are mean ± SEM, (n = 8). Data from Kaufmann et al. [11]
Responses in patients with MSA and patients with PAF
Prior to droxidopa ingestion, MSA and PAF patients had similar blood pressures and similar heart rates, both while supine and while standing. The mean dose of droxidopa in the MSA group was 1,327 ± 441 mg (mean ± SD) for a mean weight of 78 ± 12 kg (mean ± SD) and in the PAF group 875 ± 650 mg (P = 0.09) for a mean weight of 77 ± 21 kg. Following droxidopa administration, systolic blood pressure in the supine position increased more in patients with PAF than in patients with MSA (P < 0.05). There was a trend towards higher systolic blood pressure in patients with PAF after 1 min in the standing position but this did not reach statistical significance. The finding that the pressor response to droxidopa in supine patients with PAF was more pronounced than in patients with MSA indicate a peripheral mechanism of action. Indeed, because of their widespread loss of sympathetic terminals, patients with PAF have markedly exaggerated pressor responses to circulating norepinephrine [7, 14].
In summary, Droxidopa effectively raises standing blood pressure and ameliorates symptoms of orthostatic hypotension in patients with central and peripheral autonomic disorders. The pressor effect of droxidopa is due to its conversion to norepinephrine outside the brain, both in neuronal and non neuronal tissues. In patients with peripheral autonomic disorders and degeneration of sympathetic neurons (e.g. PAF), droxidopa is converted to norepinephrine in non neuronal tissue. In patients with central autonomic degeneration and preserved peripheral sympathetic neurons (e.g. MSA), droxidopa is converted to norepinephrine in neuronal and non neuronal tissue.
References
Bartholini J, Constantinidis J, Puig M, Tissot R, Pletscher A (1975) The stereoisomers of 3,4-dihydroxyphenylserine as precursors of norepinephrine. J Pharmacol Exp Ther 193:523–532
Biaggioni I, Robertson D (1987) Endogenous restoration of noradrenaline by precursor therapy in dopamine-beta-hydroxylase deficiency. Lancet 2:1170–1172
Blaschko H, Burn JH, Langemann H (1950) The formation of noradrenaline from dihydroxyphenylserine. Br J Pharmacol 5:431–437
Freeman R, Landsberg L, Young J (1999) The treatment of neurogenic orthostatic hypotension with 3,4-dl-threo-dihydroxyphenylserine: a randomized, placebo-controlled, crossover trial. Neurology 53:2151–2157
Gibbons CH, Vernino SA, Kaufmann H, Freeman R (2005) l-DOPS therapy for refractory orthostatic hypotension in autoimmune autonomic neuropathy. Neurology 65:1104–1106
Goldstein DS, Holmes C, Kaufmann H, Freeman R (2004) Clinical pharmacokinetics of the norepinephrine precursor l-threo-DOPS in primary chronic autonomic failure. Clin Auton Res 14:363–368
Hague K, Lento P, Morgello S, Caro S, Kaufmann H (1997) The distribution of Lewy bodies in pure autonomic failure: autopsy findings and review of the literature. Acta Neuropathol (Berl) 94:192–196
Inagaki C, Fujiwara H, Tanaka C (1976) Inhibitory effect of (+)threo-3,4-dihydroxy-phenylserine (DOPS) on decarboxylation of (−)threo-dops. Jpn J Pharmacol 26:380–382 Issn: 0021-5198
Kaufmann H (1996) Could treatment with DOPS do for autonomic failure what DOPA did for Parkinson’s disease? Neurology 47:1370–1371
Kaufmann H, Oribe E, Yahr MD (1991) Differential effect of l-threo-3,4-dihydroxyphenylserine in pure autonomic failure and multiple system atrophy with autonomic failure. J Neural Transm Park Dis Dement Sect 3:143–148
Kaufmann H, Saadia D, Voustianiouk A, Goldstein DS, Holmes C, Yahr MD, Nardin R, Freeman R (2003) Norepinephrine precursor therapy in neurogenic orthostatic hypotension. Circulation 108:724–728
Man in’t Veld AJ, Boomsma F, van den Meiracker AH, Schalekamp MA (1987) Effect of unnatural noradrenaline precurser on sympathetic control and orthostatic hypotension in dopamine-beta-hydroxylase defficiency. Lancet 2:1172–1175
Mathias CJ, Senard JM, Braune S, Watson L, Aragishi A, Keeling JE, Taylor MD (2001) l-threo-dihydroxyphenylserine (l-threo-DOPS; droxidopa) in the management of neurogenic orthostatic hypotension: a multi-national, multi-center, dose-ranging study in multiple system atrophy and pure autonomic failure. Clin Auton Res 11:235–242
Polinsky RJ, Kopin IJ, Ebert MH, Weise V (1981) Pharmacologic distinction of different orthostatic hypotension syndromes. Neurology 31:1–7
Schmiterlow CG (1951) The formation in vivo of noradrenaline from 3:4-dihydroxyphenylserine (noradrenaline carboxylic acid). Br J Pharmacol 6:127–134
Suzuki T, Higa S, Tsuge I, Sakoda S, Hayashi A, Yamamura Y, Takaba Y, Nakajima A (1980) Effect of infused l-threo-3,4-dihydroxyphenylserine on adrenergic activity in patients with familial amyloid polyneuropathy. Eur J Clin Pharmacol 17:429–435
Acknowledgment
I am grateful to Dr. Lucy Norcliffe-Kaufmann for her help designing the figures. Disclosure Dr. Kaufmann has served as a consultant for Chelsea Therapeutics.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kaufmann, H. L-dihydroxyphenylserine (Droxidopa): a new therapy for neurogenic orthostatic hypotension. Clin Auton Res 18 (Suppl 1), 19–24 (2008). https://doi.org/10.1007/s10286-007-1002-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10286-007-1002-2