Abstract
The purpose of this study was to compare the fracture resistance, mode of fracture, and stress distribution of endodontically treated teeth prepared with three different fiber post lengths and two different abutment heights, using both experimental and finite element (FE) approaches. Forty-eight human maxillary premolars with two roots were selected and endodontically treated. The teeth were randomly distributed into six equally sized groups (n = 8) with different combinations of post lengths (7.5, 11, and 15 mm) and abutment heights (3 and 5 mm). All the teeth restored with glass fiber post (Rely X Fiber Post, 3M ESPE, USA) and a full zirconia crown. All the specimens were thermocycled and then loaded to failure at an oblique angle of 135°. Statistical analysis was performed for the effects of post length and abutment height on failure loads using ANOVA and Tukey’s honestly significant difference test. In addition, corresponding FE models of a premolar restored with a glass fiber post were developed to examine mechanical responses. The factor of post length (P < 0.01) had a significant effect on failure load. The abutment height (P > 0.05) did not have a significant effect on failure load. The highest mean fracture resistance was recorded for the 15 mm post length and 5 mm abutment height test group, which was significantly more resistant to fracture than the 7.5 mm post and 5 mm abutment height group (P < 0.05). The FE analysis showed the peak compression and tension stress values of 7.5 mm post length were higher than that of 11 and 15 mm post length. The stress value of remaining tooth decreased as the post length was increased. Within the limitations of this experimental and FE analysis study, increasing the post length inside the root of endodontically treated premolar teeth restored with glass-fiber posts increase the fracture resistance to non-axial forces. Failure mode is more favorable with reduced abutment heights.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The decision of how to rehabilitate endodontically treated teeth (ETT) with extensive loss of coronal structure is a challenge in restorative dentistry [1]. Clinicians are increasingly opting for fiber post materials that have biomechanical characteristics similar to those of dentin, which creates homogenous stress distributions and reduces the incidence of unrestorable root fractures [2, 3].
A desirable post length has been considered to be equal to 2/3–3/4 of the root length from an era of cast metal posts and zinc phosphate cement. However, dental materials have evolved and with the use of fiber post [4], total-etch/self-etch adhesive and resin cement [5], stress distribution, and post retention have improved over conventional metal post and zinc phosphate/glass-ionomer cement retained restorations [6]. Therefore, it is theorized that with improved retention of these bonded posts, the post length within the root could be reduced while still offering retentive restorations.
Post design is a variable issue in restorative dentistry and experimental data from literature are not conclusive. Studies have investigated post length and the stiffness of the post. Franco et al. [7] found the intraradicular length of glass fiber posts was not a relevant factor in the fracture resistance of endodontically treated maxillary canines. Some studies have reported that increasing the post length resulted in a significant increase in retention and fracture resistance [8,9,10]. However, when a post is placed beyond two-thirds of the root depth, the level of stress in the apical region increases [11]. Posts are used to retain coronal restorations; they do not reinforce roots and may even weaken them through loss of radicular dentin necessitated by post space preparation [12, 13]. This is supported in a previous study whereby a 10-mm stainless steel post, inserted on maxillary central incisors, exhibited a statistically lower mean failure load than 5 mm group [14].
The presence of a ferrule is considered a key feature for the fracture resistance of ETT which has been supported by numerous studies [15, 16]. Nevertheless, various factors will affect the longevity of teeth restored using fiber posts, i.e. amount of remaining tooth structure, alveolar bone level [17], tooth post insertion, and possibly post insertion depth. To date, no clinical studies which evaluated the performance of ETT restored with GFPs have included abutment height as a variable either clinically or in vitro.
The purpose of this study was to compare the fracture resistance, mode of fracture, and stress distribution of endodontically treated teeth prepared with three different fiber post lengths and two different abutment heights, using both experimental and finite element (FE) approaches. The null hypothesis tested was that there was no effect of post length and abutment height on the fracture resistance of the ETT.
Materials and methods
Human teeth preparation
This study was approved by the ethics committee of Fujian Medical University. Forty-eight freshly extracted double-rooted maxillary premolars free of cracks, caries, fractures, and restorations were selected for the study. These teeth were extracted for orthodontic reasons. The inclusion criteria were that extracted teeth had to have complete and straight roots. A hand scaling instrument was used for surface debridement of the teeth, followed by cleaning with pumice slurry. After cleaning, the teeth were examined stereoscopically at ×10 magnification to verify the absence of cracks. No formal Cohen’s Kappa statistic was performed to measure agreement of the sample. Each premolar was measured with a digital caliper accurate to 0.01 mm (Digimatic Calipers Model 580821; HARDEN, Shanghai, China) to ensure that the samples were of similar crown and root sizes. Only teeth with a total length of 20.5 ± 0.5 mm, buccal-lingual crown dimension of 9.5 ± 0.5 mm, mesial-distal crown dimension of 7.2 ± 0.5 mm, root length of 12.1 ± 0.5 mm, the widest buccal-lingual root dimension of 8.4 ± 0.2 mm, and the widest mesial-distal root dimension of 4.9 ± 0.2 mm were selected [18]. The root lengths were measured from the cementoenamel junctions (CEJ) on the buccal surfaces. Teeth were stored in 0.1% thymol solution for a maximum of 4 weeks until use.
Root canal therapy
A standard access opening was prepared to simulate root canal treatment in each tooth. The pulp chamber of each tooth was opened using a diamond ball bur in a high-speed airturbine handpiece with water cooling. All files were new and 25 mm in length. Canals were located and patency achieved using #15 K-files (Mani, Tochigi, Japan). The canal length was visually determined by placing the #15 K-file in the root canal until its tip was visible from the apical foramen. The working length was established to be 1 mm short of the apex visually. Coronal flare was created using IntroFile (FlexMaster, VDW, Munich, Germany). All root canals were prepared to size #25/0.06 using rotary Ni–Ti instruments (Mtwo, VDW). Instrumentation was performed strictly according to manufacturers’ instructions. During the instrumentation, the root canal was irrigated with 5.25% sodium hypochlorite and 10% ethylene diamine tetra-acetic acid solution (EDTA), alternately. A final rinse with H2O was performed, and canals were dried using paper points. Warm vertical obturation of the canals was then performed using gutta-percha and a root canal sealer (AH plus, Dentsply, DeTrey GmbH, Konstanz, Germany) to the orifice level and condensed.
Post space preparation and cementation
After completion of the endodontic treatments, the teeth were randomly distributed into six equally sized groups (n = 8) with different combinations of post lengths and abutment heights:
-
Group 7.5/5, 7.5 mm post length from palatal cusp tip and 5 mm abutment height from CEJ;
-
Group 11/5, 11 mm post insertion length from palatal cusp tip and 5 mm abutment height from CEJ;
-
Group 15/5, 15 mm post insertion length from palatal cusp tip and 5 mm abutment height from CEJ;
-
Group 7.5/3, 7.5 mm post insertion length from palatal cusp tip and 3 mm abutment height from CEJ;
-
Group 11/3, 11 mm post insertion length from palatal cusp tip and 3 mm abutment height from CEJ;
-
Group 15/3, 15 mm post insertion length from palatal cusp tip and 3 mm abutment height from CEJ.
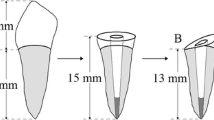
Using a dental slow handpiece at 800–1200 rpm, gutta-percha of the palatal root canal was removed with a drills in sequence until drill No. 2 (3M ESPE, USA), in strict accordance with manufacturer’s instructions. According to the morphology of root canals, one translucent glass fiber post (Rely X Fiber Post No. 2, 3M ESPE) was inserted per tooth. In the groups with 7.5 and 11 mm post lengths, the drill sequence and fiber post were cut 7.5 and 4 mm from the tip with a diamond bur, respectively, in order to ensure the consistency of the post diameter in the same position. Each post was tried into the root canal before cementation. The root canals were cleaned with a 5.25% solution of sodium hypochlorite as the final step before cementation; the post spaces were rinsed with water in a syringe and dried with air and paper points.
Posts were cleaned with ethanol and dried with air free of water and oil. A self-adhesive resin cement (RelyX Unicem, 3M ESPE) was applied into the post space using the provided elongation tip. The resin cement capsule was mixed in a RotoMix device (220 V/60 Hz centrifugal capsule mixer) for 12 s. Posts were seated into the post spaces, and excess cement was removed using a microbrush. Resin cement was light-cured through the coronal portion of the cemented post for 40 s using an LED curing light (Elipar S10, 3M ESPE) at 1200 mW/cm2 light intensity.
Tooth Embedding
Figure 1 shows the schematic drawing of specimen mounted in acrylic resin block. The root of each tooth was embedded in a self-curing acrylic resin block (self-cure tooth acrylic resin, Shangchi, China) in a custom-made stainless steel cylinder system (D = 10 mm, H = 20 mm), up to 2 mm below CEJ, and with its long axis perpendicular to the base of the block. The tooth was mounted in an acrylic resin block for testing.
Tooth preparation
A standardized extracoronal crown preparation was performed on all teeth using a water-cooled diamond bur in an air turbine at 300,000 rpm. The tooth was prepared with 0.5 to 1.5 mm of long axis reduction and minimal taper with a chamfer finish line to receive a complete full zirconia crown. Two different abutment heights were 5 and 3 mm from CEJ, respectively. The abutments were 4.0–4.5 mm in the mesiodistal dimension and 7.0–7.5 mm in the buccolingual dimension.
Design, manufacturing, and placement of Restorations
The premolar crowns were fabricated using the Zenotec CAD/CAM system (Wieland Dental, Pforzheim, Germany). Each tooth was digitally scanned with a 3Shape D750 optical scanner (3Shape, Copenhagen, Denmark). The specimens were fitted with a crown of standardized occlusal anatomy (first maxillary premolar, ZENO Kit database, ZENO CAD software). The zirconia blocks (Zenostar, Wieland Dental) were milled in a 4030M1 milling machine (Wieland Dental). Each zirconia crown was luted to the tooth abutment using the dual-cure self-adhesive resin cement (RelyX Unicem, 3M ESPE) according to manufacturer’s instructions. Before cementation, each crown was fitted on its respective tooth to check its marginal adaptation and steam cleaned. The inner surface of crowns were sandblasted with 50 um aluminum oxide at a pressure of 0.28 MPa from a distance of approximately 10 mm for 20 s in circling movements, rinsed, and cleaned in an ultrasonic bath in distilled water for 1 min. The prepared teeth were rinsed and dried. The cement was applied to the inner surface of the crowns, which were then seated on the tooth. Cement excesses were removed after a brief light exposure (ca. 2 s) with the LED curing light (Elipar S10, 3M ESPE) and followed by light polymerization for 20 s on each surface.
Thermocycling
To simulate the oral environment, specimens were stored in an incubator, ranging from 24 to 72 h, at 37 °C in 90% humidity until thermocycling commenced. The restored teeth were subjected to 10,000 thermal cycles in water baths of 5 and 55 °C alternately with a 20-s dwell time for each bath.
Fracture resistance
After thermocycling, fracture resistance was measured using a universal testing machine (AGS-X, shimadzu, Japan). Each specimen was inserted into a custom-made holding device with the long axis of the tooth inclined at a 135°angle to the load direction (Fig. 2). Linear compressive load was applied with a crosshead speed of 1 mm/min at the occlusal surface of the palatal cusp until failure. The maximum breaking load before failure was recorded in Newtons (N), and mean values were calculated per group.
Fracture modes
After mechanical failure, mode of failure was classified as “restorable” (fracture line above the CEJ) or “unrestorable” (fracture line under the CEJ), and failure mode at macroscopic view was determined by visual inspection. Specimens which presented the appearance of a root fracture were classified to have “unrestorable” fracture mode. All “unrestorable” fractures were classified as horizontal, oblique, or wave-like according to the fracture mode.
Statistical analysis
Data were statistically analyzed using the SPSS software (SPSS 10.0, SPSS, USA). Fracture resistance data were first analyzed by the Kolmogrov–Smirnov test to confirm normal distribution; then a 2-way ANOVA was used to examine the effect of the post length and abutment height, as well as the interaction between each variable. The statistical differences in various post groups were analyzed with a 1-way ANOVA test followed by a post hoc Tukey’s honestly significant difference test. Fracture modes were compared using Pearson’s Chi square test. Level of significance was set at α = 0.05.
Finite element method
A longitudinal bucco-palatal section of a double-rooted maxillary premolar was digitized and used to create 2-dimensional (2-D) models using a FE analysis software (ANSYS 10.0; ANSYS, USA) (Fig. 1). The geometry of the tooth model consisted of a zirconia crown, composite resin core, resin cement, fiber post, dentin, gutta-percha, and alveolar bone. Six models were fabricated by changing the post lengths (7.5, 11 or 10 mm) and abutment height (3 or 5 mm). The geometric designs of 2-D numeric models were similar as the experiment. Jacket crown preparations were created with 3 or 5 mm occlusal clearance, 1–1.5 mm cervical clearance and shoulder margin, 2°–5° tapering angle for premolars, 7.5, 11 or 15 mm post lengths. The chamfer finish line and anatomic occlusal reduction were included in the model. Perfect bonding was assumed at all the interfaces.
All materials in the FE analysis were considered as linearly elastic and isotropic, except for the glass fiber posts, which were modeled as transversally isotropic materials (Table 1). All of the models were meshed with 2-D 4-node structural solid elements (PLANE42) using a higher degree of interpolation function. The meshing process generated at least 16,066 elements and 16,267 nodes for each model.
As a boundary condition, fixed zero-displacement in both the horizontal and vertical directions was defined at the horizontal and vertical cut-planes of the supporting bone. 2-D models were generated with the similar treatment variations used in laboratory tests. Teeth were subjected to a 100-N force on the palatal cusp surface of the crown, 2 mm below the cusp tip, and at 135° angulations to the long axis of the tooth.
The stress distribution was solved with the FE analysis software (ANSYS 10.0; ANSYS). Since root fracture is the primary cause of failure in these restored teeth, the stress distribution in the root dentin was analyzed to identify the locations of peak stresses under the loading condition. The maximum compression and tension stress values were recorded. The areas of compression and tension were evaluated in the form of principal stress maps.
Results
Table 2 shows the mean fracture loads for each group and the results of the statistical analysis. 2-way ANOVA revealed that the factor of post length (P = 0.002 < 0.01) had a significant effect on failure load. The factor of abutment height (P = 0.66 > 0.05) and the interaction (P = 0.32 > 0.05) did not have a significant effect on failure load. The one-way ANOVA revealed that there was a statistical difference among the six groups for the mean fracture loads (P = 0.012 < 0.05). The highest mean fracture resistance was recorded for Group 15/5 at 2080.82 N ± 705.22 and it was significantly more resistant to fracture than Group 7.5/5 (1268.02 N ± 282.68) (P = 0.011 < 0.05).
As for the mode of failure, the abutments with 3 mm height showed a higher percentage of restorable fractures (Table 3). The restorable fractures were 25% for Group 7.5/5 and Group 15/5, 37.5% for Group 11/5, 67.5% for Group 11/3 and Group 15/3, and 75% for Group 7.5/3. The Chi square test showed that there was no statistical difference in the fracture mode within the groups (χ 2 = 7.43, P = 0.19 > 0.05). Figure 3 presents the representative views of restorable and unrestorable fracture modes.
Compression and tensile stress concentrations were located at the palatal and buccal areas around cervical margins, respectively, by FE analysis (Fig. 4). The maximum compression and tensile stress values in the remaining tooth are presented in Table 4. Group 7.5/5 showed the highest compression stress (−18.55 MPa) and tension stress (13.48 MPa). The peak compression and tension stress values of 7.5 mm post length were higher than that of 11 and 15 mm post length. The stress value of remaining tooth decreased as the post length was increased. In the premolar with a 3-mm abutment height, the maximum tensile stress values decreased by 1% versus 5-mm abutment height (Table 4, Group 7.5/5 versus Group 7.5/3, Group 11/5 versus Group 11/3, Group 15/5 versus Group 15/3). For the 3-mm abutment height group, a significant tensile peak was found at the cement layer (Fig. 4 black arrows).
Discussion
The current study evaluated the combined influence of post length and abutment height on the fracture resistance of ETT restored with GFP and covered with a full zirconia crown. Since 2-way ANOVA revealed that the post length had a significant difference and the abutment height had no significant effect on failure load, the null hypothesis was partly verified.
In the present study, two variables were considered: three different post lengths of GFP (7.5, 11 or 15 mm) and two different abutment heights. Post length levers were too close to each other to be distinguishable in some previous studies. When the influence of the size and morphology of natural teeth was greater than those of the post length, the experimental data were discordant. In the present study, we increased the range of post length from 7.5 to 15 mm, and the highest mean fracture resistance for Group 15/5 was significantly more resistant to fracture than Group 7.5/5. Two abutment heights were chosen, namely 5 or 3 mm to simulate normal and increased occlusal tooth tissue loss, respectively.
A number of studies [25] recommended a minimal height of 2 mm of intact tooth structure above the crown margin for 360 degrees around the circumference of the tooth preparation as a rational guideline for the ferrule effect. In this study, the ferrule lengths were greater than 2 mm. From a clinical point of view, we can design a post in such a situation. Only one post was used in the current study as more posts will increase the risk of the root canal perforation and the vertical root fracture. Multiple posts will have more variables, making the results more complex and difficult to understand. Therefore, it is not the focus of this study.
In this study, the inner surface of crowns were sandblasted with 50 um aluminum oxide at a pressure of 0.2 MPa from a distance of approximately 10 mm for 20 s in circling movements. Although sandblasting of zirconia will induce phase transformation [26], it cannot reduce the material strength and increase the fracture of the restoration. Inokoshi et al. [27] reported the influence of sandblasting and thermal annealing on the bending strength of zirconia. The results showed that sandblasting with 50 μm aluminum oxide particles for 15 s/cm2 at a distance of 10 mm hardly changed the bending strength of zirconia. Aurélio et al. [28] reported that the flexural strength of zirconia is enhanced by airborne-particle abrasion, independent of particle size, blasting time, air pressure, and the presence of aging.
On the effect of GF post length, results of the present study showed a significant difference in fracture resistance according to different post lengths. Short GFPs seemed to adversely affect the fracture resistance of ETT. It has been proven that metal posts have greater fracture resistance than GFPs [29]. This is because the elastic modulus of glass fiber post is closer to the modulus of dentin structure than that of metal posts. This leads to the difference in fracture resistance of the glass fiber post were more difficult to be found (e.g. 7.5 mm and 11, 11 and 15 mm). Furthermore, the FEA enabled a more accurate representation and analysis of the dependencies between the post length and the fracture resistance. The stress distribution in each post length group showed regular pattern. The arrangement order of the maximum tensile stress values in different post length groups was 7.5 mm > 11 mm > 15 mm (Table 4). Post length should, therefore, be optimized to the biomechanical conditions of the clinical scenario, not taken to be the longer the better. In particular the post length should retain 3–5 mm apical seal. It is sensible to keep a balance of the root fracture resistance and the post retention.
Abutment height was mostly used to study the retention and stability of implant superstructure in recent years [30]. In a study by Cano-Batalla et al. [31], which investigated the effects of abutment height (4, 5, and 6 mm) on the tensile resistance of cement-retained implant restorations, there was a significant difference detected between 4- and 6-mm abutments, with the 6-mm abutments being more retentive. In the present study, the specimens received the 135° oblique loading force, which simulated the occlusal contact of the antagonist tooth. Results of the present study suggest no significant differences in fracture resistance between the two levels of abutment height. On the other hand, the FEA results seemed to suggest that the low abutments (3 mm) were more retentive. The tensile peak at the cement layer shared a part of the tensile stress; it caused a lower tensile stress concentration in cervical dentin for Group 7.5/3, Group 11/3, and Group 15/3 (Table 4; Fig. 4) and crown debonding. The failure modes also slightly varied, with less favorable outcomes when using a high abutment (5 mm). Failure modes tended to be more favorable with the 3-mm abutment. Most of the 3-mm abutment groups failed with crown debonding, core fracture, and small margin dentin chipping, which was still considered restorable. In the clinical setting, it would be feasible to re-buildup core and smooth this margin or use periodontal surgery technique [32]. Therefore, the low abutment is similar to a “fuse”, which protects the root of ETT from oversized occlusal force.
Conclusion
Within the limitations of this experimental and FE analysis study, it can be concluded that increasing the post length inside the root of endodontically treated premolar teeth restored with glass-fiber posts increase the fracture resistance to non-axial forces. Failure mode is more favorable with reduced abutment heights. The use of a low abutment preparation may be useful to provide enhanced geometry and decrease unrestorable catastrophic fractures. Further experimental studies and clinical trials are needed to validate the results of this in vitro study.
References
Nicola S, Alberto F, Riccardo MT, Allegra C, Massimo SC, Damiano P, Mario A, Elio B. Effects of fiber-glass-reinforced composite restorations on fracture resistance and failure mode of endodontically treated molars. J Dent. 2016;53:82–7.
Kim SH, Oh TO, Kim JY, Park CW, Baek SH, Park ES. Effects of metal- and fiber-reinforced composite root canal posts on flexural properties. Dent Mater J. 2016;35:138–46.
Hatta M, Shinya A, Vallittu PK, Shinya A, Lassila LV. High volume individual fibre post versus low volume fibre post: the fracture load of the restored tooth. J Dent. 2011;39:65–71.
Baena E, Flores A, Ceballos L. Influence of root dentin treatment on the push-out bond strength of fiber posts. Odontology. 2017;105:170–7.
Lin J, Shinya A, Gomi H, Shinya A. Bonding of self-adhesive resin cements to enamel using different surface treatments: bond strength and etching pattern evaluations. Dent Mater J. 2010;29:425–32.
Elnaghy AM, Elsaka SE. Effect of surface treatments on the flexural properties and adhesion of glass fiber-reinforced composite post to self-adhesive luting agent and radicular dentin. Odontology. 2016;104:60–7.
Franco EB, et al. Fracture resistance of endodontically treated teeth restored with glass fiber posts of different lengths. J Prosthet Dent. 2014;111:30–4.
Jindal S, Jindal R, Mahajan S, Dua R, Jain N, Sharma S. In vitro evaluation of the effect of post system and length on the fracture resistance of endodontically treated human anterior teeth. Clin Oral Investig. 2012;16:1627–33.
Amarnath GS, Swetha MU, Muddugangadhar BC, Sonika R, Garg A, Rao TR. Effect of post material and length on fracture resistance of endodontically treated premolars: an in-vitro study. J Int Oral Health. 2015;7:22–8.
Adanir N, Belli S. Evaluation of different post lengths’ effect on fracture resistance of a glass fiber post system. Eur J Dent. 2008;2:23–8.
Cecchin D, Farina AP, Guerreiro CA, Carlini-Júnior B. Fracture resistance of roots prosthetically restored with intra-radicular posts of different lengths. J Oral Rehabil. 2010;37:116–22.
Krejci I, Mueller E, Lutz F. Effects of thermocycling and occlusal force on adhesive composite crowns. J Dent Res. 1994;73:1228–32.
Dietschi D, Duc O, Krejci I, Sadan A. Biomechanical considerations for the restoration of endodontically treated teeth: a systematic review of the literature—Part 1. Composition and micro- and macrostructure alterations. Quintessence Int. 2007;38:733–43.
Chuang SF, Yaman P, Herrero A, Dennison JB, Chang CH. Influence of post material and length on endodontically treated incisors: an in vitro and finite element study. J Prosthet Dent. 2010;104:379–88.
Santos-Filho PC, Veríssimo C, Soares PV, Saltarelo RC, Soares CJ, Marcondes Martins LR. Influence of ferrule, post system, and length on biomechanical behavior of endodontically treated anterior teeth. J Endod. 2014;40:119–23.
Akkayan B. An in vitro study evaluating the effect of ferrule length on fracture resistance of endodontically treated teeth restored with fiber-reinforced and zirconia dowel systems. J Prosthet Dent. 2004;92:155–62.
Mobilio N, Borelli B, Sorrentino R, Catapano S. Effect of fiber post length and bone level on the fracture resistance of endodontically treated teeth. Dent Mater J. 2013;32:816–21.
Pi X, editor. Oral anatomy and physiology. 5th ed. Beijing: People’s Medical Publishing House; 2003. p. 38–40.
Craig R, Peyton F. Elastic and mechanical properties of human dentin. J Dent Res. 1958;37:710–8.
Friedman CM, Sandrik JL, Heuer MA, Rapp GW. Composition and mechanical properties of gutta-percha endodontic points. J Dent Res. 1975;54:921–5.
Borchers L, Reichart P. Three-dimensional stress distribution around a dental implant at different stages of interface development. J Dent Res. 1983;62:155–9.
Lin J, Shinya A, Gomi H, Shinya A. Finite element analysis to compare stress distribution of connector of lithia-disilicate reinforced glass ceramic and zirconia based fixed partial denture. Odontology. 2012;100:96–9.
Jie L, Shinya A, Lassila LV, Vallittu PK. Composite resin reinforced with pre-tensioned fibers: a three-dimensional finite element study on stress distribution. Odontology. 2013;101:29–33.
Yokoyama D, Shinya A, Gomi H, Vallittu PK, Shinya A. Effects of mechanical properties of adhesive resin cements on stress distribution in fiber-reinforced composite adhesive fixed partial dentures. Dent Mater J. 2012;31:189–96.
Saker S, Özcan M. Retentive strength of fiber-reinforced composite posts with composite resin cores: effect of remaining coronal structure and root canal dentin conditioning protocols. J Prosthet Dent. 2015;114:856–61.
Chintapalli RK, Marro FG, Jimenez-Pique E, Anglada M. Phase transformation and subsurface damage in 3Y-TZP after sandblasting. Dent Mater. 2013;29:566–72.
Inokoshi M, Zhang F, Vanmeensel K, De Munck J, Minakuchi S, Naert I, Vleugels J, Van Meerbeek B. Residual compressive surface stress increases the bending strength of dental zirconia. Dent Mater. 2017;33:e147–54.
Aurélio IL, Marchionatti AM, Montagner AF, May LG, Soares FZ. Does air particle abrasion affect the flexural strength and phase transformation of Y-TZP? A systematic review and meta-analysis. Dent Mater. 2016;32:827–45.
McLaren JD, McLaren CI, Yaman P, Bin-Shuwaish MS, Dennison JD, McDonald NJ. The effect of post type and length on the fracture resistance of endodontically treated teeth. J Prosthet Dent. 2009;101:174–82.
Sia PK, Masri R, Driscoll CF, Romberg E. Effect of locator abutment height on the retentive values of pink locator attachments: an in vitro study. J Prosthet Dent. 2017;117:283–8.
Cano-Batalla J, Soliva-Garriga J, Campillo-Funollet M, Munoz-Viveros CA, Giner-Tarrida L. Influence of abutment height and surface roughness on in vitro retention of three luting agents. Int J Oral Maxillofac Implant. 2012;27:36–41.
Magne P, Spreafico RC. Deep margin elevation: a paradigm shift. Am J Esthet Dent. 2012;2:86–96.
Acknowledgements
This work was supported by the National Natural Science Foundation of China (Grant no. 81300907).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Lin, J., Matinlinna, J.P., Shinya, A. et al. Effect of fiber post length and abutment height on fracture resistance of endodontically treated premolars prepared for zirconia crowns. Odontology 106, 215–222 (2018). https://doi.org/10.1007/s10266-017-0320-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10266-017-0320-7