Abstract
Porcine-derived collagen matrix (PDCM) has been reported as a promising alternative to autogenous soft tissue grafts in periodontal plastic surgery. The aim of this study was to analyze the influence of a novel PDCM on endothelial progenitor cells (EPC) in vitro. EPC were isolated from human peripheral blood, cultured and transferred on the PDCM (mucoderm®). Tissue culture polystyrene surface (TCPS) served as control. Cell viability of EPC on PDCM was measured by a MTT and PrestoBlue® assay. Migration ability was tested using a Boyden migration assay. A ToxiLight® assay was performed to analyze the influence of PDCM on adenylate kinase (ADK) release and apoptosis rate of EPC. Using the MTT assay, EPC cultured on PDCM demonstrated a significantly increased cell viability compared to the control group at days 3, 6 and 12 (p each <0.001). According to the PrestoBlue® assay, EPC showed a significant increase of cell viability compared to the control group at 48, 72, and 96 h (p each <0.001). In the Boyden migration assay, a significantly increased EPC migration ability could be observed after 3–12 days (p each ≤0.001). No significantly increased apoptosis rate of EPC on PDCM could be observed with exception after 96 h (p each >0.05). Overall, our results suggest a good biocompatibility of PDCM without any cytotoxic effects on EPC, which might support a rapid revascularization and therefore a sufficient ingrowth of the PDCM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Several periodontal surgical procedures have been proposed for root coverage to reduce root sensitivity and to improve esthetics [1]. Within the wide range of therapeutic options, bilaminar techniques with the interposition of a connective tissue graft (CTG) are highly predictable root coverage procedures and can be considered the gold standard for treating periodontal recessions [2, 3]. Limitations of using CTGs are the painful procedure and patient morbidity in conjunction with the second surgical site as well as the limited availability of soft tissue from the hard palate in the oral cavity.
Therefore, the use of an acellular dermal matrix (ADM) allograft from human cadaveric skin as a CTG replacement is a promising approach to overcome all the mentioned problems. A recent meta-analysis on comparison of ADM to common mucogingival procedures demonstrated no statistically significant differences for any of the outcome measures (recession coverage, keratinized tissue formation, probing depths, and clinical attachment levels) when comparing ADM versus CTG for root coverage procedures [4]. However, ADM also exhibits certain disadvantages and limitations. Thus, the use of human-based tissue products may be associated with ethical concerns and potential risk of disease transmission. Indeed, most European countries have heavy restrictions on ADM allografts and its use has been limited. As a response, acellularized materials derived from xenogeneic sources have been introduced [5–7].
Porcine-derived collagen matrices (PDCM) have been approved as soft tissue grafts and represent a possible alternative to autogenous connective tissue and human acellular dermal matrices in periodontal plastic surgery. The decisive advantages of PDCM are the avoidance of using human donor tissues, their unlimited availability, and low costs [7]. A new PDCM (mucoderm®, Botiss dental, Berlin, Germany) has been developed and recently characterized in vitro and in vivo. This PDCM demonstrated a sufficient growth and proliferation of different cell lines, e.g., fibroblasts and keratinocytes, and the ability to promote a rapid ingrowth and repopulation of fibroblasts and epithelium from surrounding tissues without any immunological reactions [7]. In addition, other authors evaluated the histometrical outcomes of connective tissue grafts (CTG) vs. porcine dermal matrices (PDX) reporting that PDX can be safely used for grafting dehiscence-type defects in periodontal plastic surgery [8].
Next to the ingrowth of soft tissue cells and epithelium from surrounding tissues, microvessel ingrowth, called angiogenesis, is absolutely essential to ensure the perfusion of an implanted matrix. This results in a sufficient incorporation of the matrix, prevents for avascular wound infections and avouchs a high-quality wound healing [9].
Endothelial progenitor cells (EPC) have been firstly described by Asahara et al. [10] and play an essential role in blood vessel development and revascularization. These EPC have the potential to leave the bone-marrow niches and to introduce the development of completely new blood vessels, called neovascularization. Furthermore, they can transform to mature endothelial cells between the wound healing processes and induce the development of new blood vessels from pre-existing blood vessels, called angiogenesis [11].
The aim of the present study was to analyze the influence of a novel PDCM on endothelial progenitor cells (EPC) in vitro, which may play an active and fundamental role in the cellular process of vessel development and revascularization of PDCM.
Materials and methods
Collagen matrix
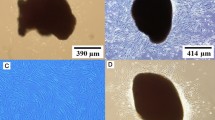
Mucoderm® is a three-dimensional (3D), pure porcine collagen matrix without further artificial cross-linking or additional chemical treatment. The processing technique removes all antigenic components from the dermis, while maintaining the structure of the graft. The decellularization and sterilization process leaves behind a 3D matrix consisting of collagen and elastin as previously reported [7]. Before the start of the in vitro assays, discs of the mucoderm® matrix were prepared according to the manufacturer’s instructions. The discs were created with a sterile, cylindrical and sharp surgical punch (6.4 ± 0.1 mm for the MTT, PrestoBlue® and ToxiLight® assays; 15.5 ± 0.1 mm for the Boyden migration assay) and the diameters of all samples were controlled with a sterile sliding caliper. Subsequently, samples were hydrated in sterile 0.9 % sodium chloride solution for 5 min. All procedures were performed under sterile conditions as previously described [7].
EPC culture
Mononuclear cells (MNCs) were isolated by density gradient centrifugation with Biocoll (Biochrom KG, Berlin, Germany) from human peripheral blood as previously described by Ziebart et al. [11]. Immediately following isolation, total MNCs (8 × 106 cells/ml medium) were plated on 25-cm2 culture flasks coated with human fibronectin (Sigma, Steinheim, Germany) and maintained in EBM (endothelium basal medium; Lonza, Basel, Switzerland) supplemented with EGM (endothelium growth medium; Lonza, Basel, Switzerland) SingleQuots, 100 ng/ml VEGF (vascular endothelium growth factor; Sigma, Steinheim, Germany), and 20 % FCS (fetal calf serum; Lonza, Basel, Switzerland). Endothelial progenitor cells (EPC) were cultured in a cell culture incubator at 37 °C and 5 % CO2 with sporadic agitation [11].
MTT assay
To examine the cell viability of EPC, a 3-(4,5- dimethylthiazol-2-yl)-2,5-diphenyl tetrazolium bromide colorimetric assay (MTT; Sigma, Steinheim, Germany) was performed as previously described [7]. Tetrazolium bromide is reduced to formazan by viable cells. Formazan can be measured photometrically at 550 nm.
For the MTT assay, blanked discs of the matrix (diameter 6.4 ± 0.1 mm) were transferred into 48 wells of 96-well plates. Remaining 48 wells were used as TCPS (tissue culture polystyrene surface) control group. Subsequently, EPC were transferred into the 96-well plates (each 12,500 cells/well). Cell viability was measured at four points of time after 3, 6, 9 and 12 days of cell growing with a Synergy HT Multi-Mode Microplate Reader (corresponding setting: absorbance; BioTek Instruments, Winooski, VT, USA).
PrestoBlue® assay
PrestoBlue® assay (Invitrogen, Life Technologies GmbH, Darmstadt, Germany) was used to assess the influence of the PDCM on cell viability and proliferation ability of EPC as previously described [7]. This assay contains a fluorometric growth indicator and is based on the detection of metabolic mitochondrial activity. PrestoBlue® Cell Viability Reagent (Invitrogen) is a soluble, nontoxic blue stain that is incorporated by cells and reduced to a red fluorescing stain (resorufin) in accordance with their proliferative activity. 96-well plates were prepared similar to the MTT assay (each 12,500 cells/well). At 24–120 h (h; 24, 48, 72, 96, 120 h) after applying 10 % PrestoBlue®, the color change induced by the reduction of resazurin to resorufin was measured at a wavelength of 560/20 and 620/40 nm with a Synergy HT Multi-Mode Microplate Reader (corresponding setting: fluorescence; BioTek Instruments, Winooski, VT, USA) and analyzed with Gen5 (BioTek Instruments, Bad Friedrichshall, Germany).
Boyden migration assay
For the migration assay, a 24-well Boyden chamber assay system (Thin-Cert™; Greiner BioOne, Essen, Germany) was used as previously described [11]. Blanked squares of the membrane (diameter 15.5 ± 0.1 mm) were transferred into four 24-well plates. In addition, four 24-well plates were used as TCPS control group. Subsequently, EPC were transferred into the 24-well plates (each 100,000 cells/well). Migration ability was measured at four points of time after 3, 6, 9 and 12 days of cell growing. At each time point, the cells of a 24-well plate with PDCM discs and a 24-well plate of a TCPS control were trypsinized with 500 µl Trypsin–EDTA (Invitrogen, Life Technologies GmbH, Darmstadt, Germany) per well, counted and then transferred into the migration chambers (each 12,500 cells/chamber). After 24 h, cells were stained with Calcein-AM fluorescent dye (Invitrogen). Thereafter, the inserts were transferred to the wells of freshly prepared black 24-well plates containing 500 µl Trypsin–EDTA per well. These plates were incubated for 10 min in a cell culture incubator at 37 °C and 5 % CO2. The inserts were discarded, and 250 µl of each well of the Trypsin–EDTA solution, containing the detached migratory cells, was transferred to wells of flat-bottom black 24-well plates with transparent bottom. A Synergy HT Multi-Mode Microplate Reader (corresponding setting: fluorescence; BioTek Instruments, Winooski, VT, USA) was used for quantification.
ToxiLight® assay
The cytotoxic potential of the employed PDCM on EPC was investigated using the ToxiLight® BioAssay Kit (Lonza Rockland, Inc., Rockland, ME, USA) as previously described [7]. The ToxiLight® BioAssay is a nondestructive, bioluminescent cytotoxicity assay that quantitatively measures the release of adenylate kinase (AK) from damaged cells. 96-well plates were prepared similar to the MTT assay (each 25,000 cells/well). After different points of time ranging from 24 to 120 h (24, 48, 72, 96, 120 h), the supernatant was mixed with ToxiLight® agent. After a short incubation time, the emitted light intensity was measured using a Synergy HT Multi-Mode Microplate Reader (corresponding setting: luminescence; BioTek Instruments, Winooski, VT, USA).
Statistical analysis
Comparisons were analyzed by ANOVA (post hoc test: Tukey; SPSS version 17.0). p values <0.05 were considered to be statistically significant. All assays were performed in triplicate. Continuous variables were expressed as mean values with standard deviations in the vertical bar charts. Asterisks over horizontal beams demonstrate a statistically significant difference between the EPC control and the EPC mucoderm® group for the particular point of measurement (p < 0.05).
Results
MTT assay
Concerning the EPC viability, EPC on the mucoderm® matrix demonstrated a significantly increased cell viability after 3, 6 and 12 days compared to the EPC control group on TCPS (p each <0.001).
After 3 and 6 days, EPC on the mucoderm® matrix showed a significantly increased cell viability of +31.19 % (after 3 days) and +37.67 % (after 6 days) compared to the EPC control group on TCPS (p each <0.001).
After 9 days, a significantly decreased EPC viability on the mucoderm® matrix of −3.89 % compared to the EPC control group on TCPS (p = 0.046) could be detected and in the broader experimental course after 12 days, EPC on the mucoderm® matrix demonstrated a significantly increased cell viability of +16.19 % compared to the EPC control group on TCPS again (p < 0.001; Fig. 1).
PrestoBlue® assay
Concerning the EPC viability within the first 5 days, EPC on the mucoderm® matrix demonstrated a significantly increased cell viability after 48, 72 and 96 h compared to the EPC control group on TCPS (p each < 0.001).
After 24 h, EPC on the mucoderm® matrix showed a significantly decreased cell viability of −9.6 % compared to the EPC control group on TCPS (p = 0.127). After 48, 72 and 96 h, a significantly increased EPC viability on the mucoderm® matrix of +43.95 % (after 48 h), +56.14 % (after 72 h) and +20.43 % (after 96 h) could be detected compared to the EPC control group on TCPS (p < 0.001). Finally after 120 h, EPC on the mucoderm® matrix demonstrated a significantly decreased cell viability of −3.06 % compared to the EPC control group on TCPS (p = 0.07; Fig. 2).
Boyden migration assay
Concerning the EPC migration ability, EPC on the mucoderm® matrix demonstrated a significantly increased migration ability after 3, 6, 9 and 12 days compared to the EPC control group on TCPS (p each ≤0.001).
After 3 days, EPC on the mucoderm® matrix showed a significantly increased migration ability of +45.25 % compared to the EPC control group on TCPS (p < 0.001). After 6 days, a significantly increased EPC migration ability on the mucoderm® matrix of +67.55 % could be detected compared to the EPC control group on TCPS (p < 0.001). After 9 days, EPC on the mucoderm® matrix demonstrated a significantly increased migration ability of +34.3 % compared to the EPC control group on TCPS (p < 0.001). After 12 days, EPC on the mucoderm® matrix showed a significantly increased migration ability of +18.09 % compared to the EPC control group on TCPS (p = 0.001; Fig. 3).
ToxiLight® assay
Concerning the EPC ADK release and apoptosis rate, EPC on the mucoderm® matrix demonstrated no significantly increased ADK release and apoptosis rate at all points of measurement after 24, 48, 72 and 120 h compared to the EPC control group on TCPS (p each >0.05).
After 24 h, EPC on the mucoderm® matrix showed no significantly increased ADK release and apoptosis rate of +2.68 % compared to the EPC control group on TCPS (p = 0.182). After 48 h, EPC on the mucoderm® matrix demonstrated no significantly decreased ADK release and apoptosis rate of −8.09 % compared to the EPC control group on TCPS (p = 0.08). After 72 and 96 h, an increased EPC ADK release and apoptosis rate on the mucoderm® matrix of +6.09 % (after 72 h) and +7.46 % (after 96 h) could be detected compared to the EPC control group on TCPS, which became significant after 96 h (p = 0.001). After 120 h, EPC on the mucoderm® matrix demonstrated a significantly decreased ADK release and apoptosis rate of −13.41 % compared to the EPC control group on TCPS (p < 0.001; Fig. 4).
Discussion
The results of the present study demonstrated a good in vitro biocompatibility for PDCM with regard to EPC. This is reflecting a high EPC viability and migration ability without any cytotoxic or apoptotic effects on the investigated progenitor cell lineage. It might support a rapid and sufficient PDCM revascularization and therefore a high-quality ingrowth of the PDCM.
The proven success of PDCM for soft tissue grafting strongly depends on the ingrowth of new endothelial cells, resulting in new blood vessel development and revascularization. Unfortunately, one major limitation of PDCM is the fact that these scaffolds are completely acellular and avascular in their natural and unmodified condition. Therefore, in contrast to regular wound healing in cellular and vascularized tissues, PDCM cannot stimulate blood vessel ingrowth and revascularization by exsolution of stimulating, proangiogenic cytokines and growth factors, e.g., VEGF (vascular endothelial growth factor), bFGF (beta fibroblast growth factor) or PDGF (platelet-derived growth factor) [12–14]. Consequently, the revascularization of PDCM cannot be stimulated directly by the scaffold. Thus, it is absolutely essential that PDCM offers ideal conditions from the very first for migrating cells to be revascularized. Since the influence of PDCM on mature endothelial cells (HUVEC) has been analyzed previously, this study focused on endothelial progenitor cells (EPC) as the progenitor lineage of the endothelial cell line [7].
In this context, e.g., after surgical procedures, endothelial progenitor cells (EPC) can migrate from the bone-marrow niches into the vascular system, where they circulate and partly differentiate into mature endothelial cells [15]. Through the vascular system, EPC can reach wound areas or primary avascular, ischemic areas, e.g. freshly placed PDCM, with a strong need for revascularization. This tissue ischemia is presumed to be the strongest stimulus for EPC mobilization from the bone-marrow niches to the circulation [16, 17]. After arriving in the wounded or ischemic area, EPC leave the vascular system and migrate into the wound area, where they can stimulate the growing of new blood vessels in different ways: First, they stimulate the sprouting angiogenesis as well as the intussusceptive angiogenesis from pre-existing vessels by strong autocrine and paracrine effects by production of several proangiogenic cytokines and growth factors such as VEGF [10]. Second, they migrate into the wound area as well as into, e.g., PDCM, where they can differentiate into mature endothelial cells and be incorporated into newly formed vessels from pre-existing vessels, called angiogenesis, or promoting a de novo creation of primordial vessels, called neovasculogenesis [10, 18–20].
Wound healing can be divided into three phases: with a special view on the revascularization process, in the inflammation phase, 1 h after wounding (a.w.) as far as 14 days a.w., PDGF as proangiogenic cytokine is released into the wound. The following proliferation phase, 1 day a.w. as far as 14 days a.w., is among others characterized by endothelial cell migration as well as angiogenesis and revascularization, starting about 3 days a.w. and continuing up to 3 weeks a.w. In the remodeling phase, dispensable cells are removed by apoptosis and the collagen structures are remodeled [21–23].
Our results demonstrated an increased cell viability of EPC on PDCM using the PrestoBlue® assay after 2–4 days and using the MTT assay after 3 days and especially after 6 days. In addition, a significant increase in EPC migration ability could be detected after 3 days and exceptionally after 6 days. This increased cell viability and migration ability of EPC, especially during the time period of the inflammation phase and the early proliferation phase, might support a rapid and early revascularization of the scaffold. It might be possible that the stimulating influence of PDCM on EPC viability during the inflammatory phase may stimulate the described and VEGF attributed autocrine and paracrine effects of EPC. Based on this strong autocrine VEGF stimulation, the EPC migration ability may be increased, which is absolutely essential during the proliferation phase to migrate into the wound area. Mucoderm® matrix is completely acellular and sensitive during the early healing phase. Therefore, a bilaminar vascular environment should be created to nourish the mucoderm® matrix in root coverage surgical procedures. This might optimize the revascularization and wound healing process of the scaffold.
To the best of our knowledge, there is no other in vitro or in vivo study dealing with results concerning the influence of PDCM on EPC. Beside the influence of PDCM on mature endothelial cells (HUVEC) in vitro, several previous studies analyzed the in vivo characteristics of different matrices. In addition to a sufficient blood vessel ingrowth into PDCM (mucoderm®) after 21 days in situ as assessed by CD31 immunochemistry, other studies showed that the central parts of a bilayered porcine matrix became revascularized after 30 and 60 days [7, 24]. Other authors reported rapid revascularization of a single-layer acellular human dermis as well as a human acellular dermal matrix within 2 weeks after surgery [7, 25, 26]. Guiha et al. [27] evaluated the healing and revascularization of autogenous, subepithelial connective tissue graft in dogs. The authors found that the graft was completely revascularized after 14 days. At 28 and 60 days, normal vascularization could be demonstrated histologically. Hoyama et al. [28] reported that human and porcine acellular dermal tissues are both well tolerated when implanted subcutaneously in rats [7]. Moreover, an increased microvessel density within the scaffolds and the surrounding tissues of the porcine graft could be demonstrated after 6 months in situ. Another in vivo-designed study reported an increased soft tissue ingrowth and microvessel density in human-based dermis compared to porcine-based dermis [7, 29]. Most of these studies had their focus on the later wound healing phases and revascularization. Consequently, further studies may also investigate the first days of wound healing concerning the revascularization in vivo (day 1–6).
In conclusion, our findings indicate that PDCM is a promising substitute in periodontal plastic surgery with high biocompatibility concerning endothelial progenitor cells (EPC) and therefore allowing a sufficient revascularization of its collagen structure in the early and the advanced wound healing phases. Further studies should focus on the biofunctionalization of PDCM, e.g. using different proangiogenic cytokine- (e.g. VEGF) or platelet-rich fibrin (PRF) coatings.
References
Zucchelli G, Amore C, Sforza NM, Montebugnoli L, de Sanctis M. Bilaminar techniques for the treatment of recession-type defects. A comparative clinical study. J Clin Periodontol. 2003;30:862–70.
Cairo F, Pagliaro U, Nieri M. Treatment of gingival recession with coronally advanced flap procedures: a systematic review. J Clin Periodontol. 2008;35:136–62.
Chambrone L, Sukekava F, Araujo MG, Pustiglioni FE, Chambrone LA, Lima LA. J Periodontol. 2010;81:452–78.
Gapski R, Parks CA, Wang HL. Acellular dermal matrix for mucogingival surgery: a meta-analysis. J Periodontol. 2005;76:1814–22.
Jepsen K, Jepsen S, Zucchelli G, Stefanini M, de Sanctis M, Baldini N, Greven B, Heinz B, Wennström J, Cassel B, Vignoletti F, Sanz M. Treatment of gingival recession defects with a coronally advanced flap and a xenogeneic collagen matrix: a multicenter randomized clinical trial. J Clin Periodontol. 2012;40:82–9.
Schlee M, Ghanaati S, Willershausen I, Stimmlmayr M, Sculean A, Sader RA. Bovine pericardium based non-cross linked collagen matrix for successful root coverage, a clinical study in human. Head Face Med. 2012;8:6.
Pabst AM, Happe A, Callaway A, Ziebart T, Stratul SI, Ackermann M, Konerding MA, Willershausen B, Kasaj A. In vitro and in vivo characterization of porcine acellular dermal matrix for gingival augmentation procedures. J Periodontal Res. 2014;49:371–81.
Fickl S, Nannmark U, Schlagenhauf U, Hürzeler MB, Kebschull M. Porcine dermal matrix in the treatment of dehiscence-type defects: an experimental split-mouth animal trial. Clin Oral Impl Res. 2014 [Epub ahead of print].
Tonnesen MG, Feng X, Clark RA. Angiogenesis in wound healing. J Investig Dermatol Symp Proc. 2000;5:40–6.
Asahara T, Murohara T, Sullivan A, Silver M, van der Zee R, Li T, Witzenbichler B, Schatteman G, Isner JM. Isolation of putative progenitor endothelial cells for angiogenesis. Science. 1997;275:964–7.
Ziebart T, Pabst A, Klein MO, Kaemmerer P, Gauss L, Bruellmann D, et al. Bisphosphonates: restrictions for vasculogenesis and angiogenesis: inhibition of cell function of endothelial progenitor cells and mature endothelial cells in vitro. Clin Oral Investig. 2011;15:105–11.
Bao P, Kodra A, Tomic-Canic M, Golinko MS, Ehrlich P, Brem H. The role of vascular endothelial growth factor in wound healing. J Surg Res. 2009;153:347–58.
Werner S, Grose R. Regulation of wound healing by growth factors and cytokines. Physiol Rev. 2003;83:835–70.
Pierce GF, Mustoe TA, Altrock BW, Deuel TF, Thomason A. Role of platelet-derived growth factor in wound healing. J Cell Biochem. 1991;45:319–26.
Urbich C, Heeschen C, Aicher A, Sasaki K, Bruhl T, Farhadi MR, Vajkoczy P, Hofmann WK, Peters C, Pennacchio LA, Abolmaali ND, Chavakis E, Reinheckel T, Zeiher AM, Dimmeler S. Cathepsin L is required for endothelial progenitor cell-induced neovascularization. Nat Med. 2005;11:206–13.
Rafii S, Lyden D. Therapeutic stem and progenitor cell transplantation for organ vascularization and regeneration. Nat Med. 2003;9:702–12.
Yoon CH, Hur J, Oh IY, Park KW, Kim TY, Shin JH, Kim JH, Lee CS, Chung JK, Park YB, Kim HS. Intercellular adhesion molecule-1 is upregulated in ischemic muscle, which mediates trafficking of endothelial progenitor cells. Arterioscler Thromb Vasc Biol. 2006;26:1066–72.
Galiano RD, Tepper OM, Pelo CR, Bhatt KA, Callaghan M, Bastidas N, Bunting S, Steinmetz HG, Gurtner GC. Topical vascular endothelial growth factor accelerates diabetic wound healing through increased angiogenesis and by mobilizing and recruiting bone marrow-derived cells. Am J Pathol. 2004;164:1935–47.
Sivan-Loukianova E, Awad OA, Stepanovic V, Bickenbach J, Schatteman GC. CD34+ blood cells accelerate vascularization and healing of diabetic mouse skin wounds. J Vasc Res. 2003;40:368–77.
Asahara T, Masuda H, Takahashi T, Kalka C, Pastore C, Silver M, Kearne M, Magner M, Isner JM. Bone marrow origin of endothelial progenitor cells responsible for postnatal vasculogenesis in physiological and pathological neovascularization. Circ Res. 1999;85:221–8.
Kirsner RS, Eaglstein WH. The wound healing process. Dermatol Clin. 1993;11:629–40.
Hess CT, Kirsner RS. Orchestrating wound healing: assessing and preparing the wound bed. Adv Skin Wound Care. 2003;16:246–57.
Li J, Zhang YP, Kirsner RS. Angiogenesis in wound repair: angiogenic growth factors and the extracellular matrix. Microsc Res Tech. 2003;60:107–14.
Ghanaati S, Schlee M, Webber MJ, Willershausen I, Barbeck M, Balic E, Görlach C, Stupp SI, Sader RA, Kirkpatrick CJ. Evaluation of the tissue reaction to a new bilayered collagen matrix in vivo and its translation to the clinic. Biomed Mater. 2011;6:015010.
Wong AK, Schonmeyr B, Singh P, Carlson DL, Li S, Mehrara BJ. Histologic analysis of angiogenesis and lymphangiogenesis in acellular human dermis. Plast Reconstr Surg. 2008;121:1144–52.
Eppley B. Experimental assessment of the revascularization of acellular human dermis for soft-tissue augmentation. Plast Reconstr Surg. 2001;107:757–62.
Guiha R, el Khodeiry S, Mota L, Caffesse R. Histological evaluation of healing and revascularization of the subepithelial connective tissue graft. J Periodontol. 2001;72:470–8.
Hoyama E, Schellini SA, Marques ME, Rossa R, Padovani CR. A comparison of human and porcine acellular dermal tissues in the subcutaneous space of a rat model. Orbit. 2005;24:249–55.
Richter GT, Smith JE, Spencer HJ, Fan CY, Vural E. Histological comparison of implanted cadaveric and porcine dermal matrix grafts. Otolaryngol Head Neck Surg. 2007;137:239–42.
Conflict of interest
The authors declare that there is no conflict of interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pabst, A.M., Lehmann, KM., Walter, C. et al. Influence of porcine-derived collagen matrix on endothelial progenitor cells: an in vitro study. Odontology 104, 19–26 (2016). https://doi.org/10.1007/s10266-014-0186-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10266-014-0186-x