Abstract
Cilostazol is a selective inhibitor of phosphodiesterase-III with antiplatelet, antithrombotic and vasodilating properties. The aim of our study was to evaluate the effect of the drug on vasculopathy and Raynaud’s phenomenon (RP), in a series of patients with systemic sclerosis (SSc), before and after cilostazol treatment. Twenty-one consecutive SSc patients with moderate or severe RP were enrolled in an open-label study. Cilostazol was administered at the dose of 100 mg twice a day, for 12 months. Evaluations included: daily RP attack diary documenting the frequency and duration of RP episodes, Health Assessment Questionnaire-Disability Index, scleroderma visual analogue scales (VAS), flow-mediated dilation and immunological status, including endothelin 1 and interleukin 6 plasma levels. Thirteen patients completed the study. RP duration and daily number episodes recorded over a 3-week period significantly decreased after cilostazol treatment (p = 0.0049 and p = 0.0067, respectively). VAS score indicated a significant amelioration of the patients’ perception of RP (p = 0.0117), and both baseline and post-ischemic brachial artery diameters were significantly increased after cilostazol treatment, as compared with basal values (p = 0.0119 and p = 0.0076, respectively). None of the patients developed digital ulcers during the study. A significant clinical improvement of RP was recorded in SSc patients undergoing cilostazol treatment. Study results indicate a potential role of cilostazol as oral maintenance therapy in SSc patients with RP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Systemic sclerosis (SSc) is a connective tissue disease characterized by vasculopathy, immune dysregulation and fibrosis [1]. Raynaud’s phenomenon (RP) is the early onset symptom in most SSc patients. RP is determined by vasoconstriction and blood flow reduction in peripheral arterial vessels occurring when the subject moves from a warm to a cold environment. It is characterized by an ischemic phase, in which fingers are typically pale, followed by cyanosis and reactive hyperemia. RP may be isolated (primary RP) or associated with other pathological conditions (secondary RP), such as connective tissue and hematological diseases as well as with some drugs (i.e., beta-blockers) use [2, 3]. Raynaud’s phenomenon is almost always detectable in SSc patients and may precede the disease onset by many years [1].
Several therapies have been tested for the treatment of RP; however, they have low efficacy and/or significant side effects [2, 4, 5]. At present, guidelines for the treatment of RP recommend only dihydropyridine-type calcium channel blockers and intravenous iloprost [6]. The effectiveness of calcium channel blocker is controversial and limited to the symptoms of RP (frequency and severity of attacks); on the other hand, intravenous iloprost shows a greater efficacy on RP and more generally on scleroderma vasculopathy resulting effective in healing active digital ulcers (DUs) [3, 6, 7]. In view of costs and feasibility, the experts suggest that intravenous prostanoids should be used when calcium channel blocker has failed or for the treatment of active DUs [6]. In addition to the above-mentioned treatments, various other therapies are employed for the treatment of RP, but at the present oral treatment for RP is still disappointing.
Cilostazol is a selective inhibitor of phosphodiesterase-III with antiplatelet, antithrombotic and vasodilating properties. It also exhibits antiproliferative effects on smooth muscle cells and has beneficial effects on high-density lipoprotein-cholesterol and triglyceride levels [8–10]. Cilostazol is currently licensed for the treatment of patients suffering from “claudicatio intermittens” due to peripheral artery disease, but current literature reports evidence of efficacy of the drug in reducing the progression of carotid intima-media thickness [11], improving clinical outcome after endovascular interventions [12] and preventing stroke [8]. Moreover, a previous study indicated that cilostazol is able to increase brachial artery diameter in patients with primary and secondary RP, with a favorable impact on brachial artery responsiveness to cold in patients with primary RP [13].
Thus, the aim of our study was to evaluate the effect of cilostazol on RP, in a series of SSc patients with moderate to severe RP.
Materials and methods
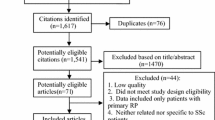
This single-center, open-label study has been approved by the local ethical committee, and all patients signed a written informed consent. The study was conducted in accordance with the principles of the Declaration of Helsinki and was registered in the European Clinical Trials Database (EudraCT No. 2010-019977-14). The study was conducted at the Clinical Immunology Unit of the San Martino Hospital, Genoa, Italy, from November 2010 to April 2012.
Patients
Outpatients affected by SSc, diagnosed according to the American College of Rheumatology criteria [14], were classified into the diffuse and limited forms of the disease according to LeRoy criteria [15].
Inclusion criteria
Moderate to severe RP and absence of contraindications to cilostazol use.
Exclusion criteria
Severe renal insufficiency (glomerular filtration rate <25 ml/min); severe liver disease; congestive heart failure; history of ventricular tachycardia; ventricular fibrillation and multifocal ventricular extrasystoles; QT prolongation; pregnancy and lactation; CYP3A4 or CYP2C19 inhibitors use; and known predisposition to bleeding.
Drug regimen
Cilostazol (Pletal®, Italfarmaco S.p.A., under license from Otsuka Pharmaceutical Europe Ltd.) was administered at the dose of 100 mg twice a day, 30 min before or 2 h after the breakfast and the dinner. Treatment duration was 12 months.
Endpoints
Primary endpoint
Pre- and post-therapy frequency, duration and severity of RP attacks in patients affected by SSc.
Secondary endpoints
Pre- and post-therapy modifications of Health Assessment Questionnaire-Disability Index (HAQ-DI), scleroderma visual analogue scales (VAS), flow-mediated dilation (FMD) of the brachial artery, in vitro immunological status (lymphocytes subpopulations and ET-1 and IL-6 plasma levels).
Questionnaires
Patients were invited to fill in the following questionnaires before and after treatment.
RP attack diary
Each day patients recorded the number of RP attacks as well as the duration of each RP attack (in minutes) [16].
Health Assessment Questionnaire-Disability Index (HAQ-DI)
The HAQ-DI is a self-reported questionnaire that measures physical disability in 8 domains on a total of 20 items. There are 4 possible responses for each item, ranging from 0 (without any difficulty) to 3 (unable to do). The individual scores are aggregated to yield a single index of disability ranging from 0 (normal) to 3 (severe). The HAQ has been used extensively in studies of rheumatoid arthritis and has also been validated in patients with SSc [17, 18].
Visual analogue scales (VAS)
Patients completed three VAS scales to evaluate the impact of SSc on their perception of RP severity, DUs and global disease activity on a scale ranging from 0 mm (none) to 100 mm (very severe) [18].
Flow-mediated dilation (FMD)
FMD assessment was performed as previously described [19]. Ultrasound scans were performed using the C512 Acuson Sequoia, equipped with a 5.0–8.0 MHz linear wideband multihertz imaging probe (8L5). The brachial artery was scanned over a longitudinal section 2–3 cm above the antecubital fossa. After baseline measurements of brachial artery diameter, the pressure cuff was kept inflated for 5 min at 50 mm Hg over systolic blood pressure on the proximal portion of the forearm. Post-ischemic artery diameter recording was started 30 s before rapid deflation of the blood pressure cuff, and the longitudinal image of the artery was recorded continuously for up to 4 min. Ultrasound images were analyzed offline by averaging the arterial diameter along 10-mm segments. Diameters from 3 consecutive end-diastolic frames (identified by the electrocardiographic R wave) were averaged to yield the brachial artery diameter during the respective experimental stages. FMD was expressed as percentage of increase in arterial diameter from baseline to the post-occlusive period.
Immunological parameters
Blood samples were taken before and after the end of treatment. Peripheral blood lymphocyte phenotype was determined as previously described [20]. Briefly, peripheral blood mononuclear cells (PBMCs) were obtained by Ficoll-Hypaque gradient centrifugation, and expression of membrane antigens was analyzed by direct immunofluorescence incubating PBMCs (1 × 105 cells) with anti-CD3, CD4, CD8, CD19 and CD56 (Beckman Coulter, Europe) monoclonal antibodies at 4 °C for 30 min in the dark; fluorochrome-conjugated isotype-matched antibodies were used as controls. After staining, the analysis was performed by flow cytometry using a FC500 flow cytometer equipped with CXP software (Beckman Coulter, Europe).
The plasma levels of endothelin-1 (ET-1) and interleukin-6 (IL-6) by use of commercially available sandwich immunoenzymatic assays (ELISA) kits (R&D Systems) according to manufacturer’s instructions.
Statistical analysis
Statistical analyses were performed using GraphPad Prism version 6.03 for Windows (GraphPad Software, San Diego, California, USA). Comparisons between values obtained before and after treatment were made by nonparametric Wilcoxon matched pairs test. A p value <0.05 was considered as statistically significant. When indicated, values are reported as mean ± standard error of the mean (SEM).
Results
Twenty-one patients (aged 61.3 ± 14.8 years) agreed to participate in the study. Among them, 8 were affected by the limited form and 13 by the diffuse form of the disease. Six patients did not complete the study because of side effects of the treatment and two patients were lost to follow-up. None of the patients showed DUs at the enrollment or developed DUs during the study.
Effect of cilostazol treatment on duration and number of Raynaud’s phenomenon attacks
The total duration of RP episodes recorded over a 3-week period significantly decreased after cilostazol treatment (p = 0.0049) (Fig. 1, panel A). The mean percentage reduction in duration of RP attacks after treatment was 46 ± 12 %. Cilostazol significantly decreased the total number of RP attacks recorded over a 3-week period (p = 0.0067) (Fig. 1, panel B). The mean percentage decrease in number of RP attacks observed after cilostazol treatment was 36 ± 11 %.
Effect of cilostazol treatment on global disease activity perception, Raynaud’s phenomenon severity perception and functional status (disability)
Pre- and post-treatment VAS scales scores indicated that cilostazol significantly improved the patients’ perception of RP severity (p = 0.0117, Fig. 2). On average, the improvement on RP severity perception after treatment was 19 ± 6 mm. The global disease activity VAS scores were not significantly modified by the treatment (p = 0.3125, data not shown). VAS scale rating DUs was not analyzed since none of the patients presented DUs at the enrollment or developed DUs during the study. HAQ-DI questionnaire scores are not significantly improved by cilostazol therapy (p = 0.7500, data not shown).
Effect of cilostazol treatment on FMD and brachial artery diameter
The evaluation of FMD, expressed as percentage of increase in arterial diameter from baseline to the post-occlusive period, did not show significant variations after cilostazol treatment (p = 0.345, data not shown). However, both baseline and post-ischemic diameter of brachial artery were significantly increased (p = 0.0119 and p = 0.0076, respectively) after cilostazol treatment, as compared with pre-treatment values (Fig. 3). After treatment, pre- and post-ischemic increases in brachial artery diameter were 0.035 ± 0.011 and 0.034 ± 0.009 cm, respectively.
Effect of cilostazol treatment on immunological parameters
Cilostazol treatment did not significantly modify lymphocyte absolute count and lymphocytes subpopulations, as well as ET-1 and IL-6 plasma levels (data not shown).
Side effects
Side effects attributable to cilostazol were generally mild and transient, as expected. The most common side effect was headache that resolved in a few days either adopting an up-titration schedule at beginning of cilostazol administration or with the administration of paracetamol. Less common and transitory side effects were diarrhea and palpitations. Six patients withdrew from the study due to the onset of more severe side effects, namely headache (1 case), palpitations (1 case), hypotension (1 case), nausea (1 case) and dizziness (2 cases). Two patients were lost to follow-up.
Discussion
To the best of our knowledge, this is the first study that specifically evaluated the effect of cilostazol in patients affected by SSc. The results of this study show that cilostazol: (a) reduces duration and daily number of RP attacks, (b) ameliorates patients’ perception of RP and (c) increases brachial artery diameter in treated patients.
The main finding of the present study is a significant amelioration of RP after cilostazol treatment. This positive effect is related to the decrease in both number and duration of RP episodes, and to a significant decrease in RP severity, according to subjective perception.
Although no patient was affected by DUs at enrollment, it is noteworthy that patients did not develop any new DUs during cilostazol treatment for a period of 1 year. In the present study, the incidence of DUs was not compared with a control group; however, the result can be considered positive, as DUs generally affect more than half of the patients during the course of the disease and occur in about 30 % of the patients each year [7]. Our results are consistent with a recent study by De Franciscis et al. [21] in which cilostazol treatment demonstrated to reduce significantly the incidence of new ulcers in diabetic patients with peripheral arterial disease and decrease MMP-9 plasma levels—a metalloproteinase that has been implicated in various pathologic conditions characterized by excessive fibrosis including SSc [22]. It is possible that a similar effect on MMP-9 also occurs in SSc patients and deserves to be investigated in future studies.
FMD evaluation did not show an increase in vascular reactivity; however, both baseline and post-ischemic diameter of brachial artery were significantly increased after cilostazol treatment due to the well-known vasodilator effect of the drug. The increases in vessel diameter are coherent with the well-known vasodilator effect of cilostazol and could explain the clinical improvement observed in treated patients.
Cilostazol did not induce variations of peripheral blood lymphocyte subpopulations as well as of ET-1 and IL-6 plasma levels. This finding is not surprising as cilostazol mainly exerts antiplatelet, vasodilating, but not immunomodulatory effects; however, we cannot exclude that it might modify other soluble factors that were not evaluated in the present study.
The side effects observed were generally not severe and led to the interruption of treatment only in a limited number of cases, confirming a satisfactory safety profile of the drug.
The present study shows some limitations, especially related to the study design (open-label, non-placebo-controlled) and the relatively small sample size. However, the good clinical profile of the drug, in terms of both tolerability and effectiveness, and the encouraging results of our study allow us to express a positive opinion on the risk/benefit ratio of cilostazol use for the treatment of RP in SSc patients; thus, indicating a potential role of cilostazol as oral maintenance therapy in patients for whom the use of other oral medications is contraindicated or unsuitable.
However, further studies are needed to confirm present data, to identify any subgroup of SSc patients who may particularly benefit from treatment with cilostazol and to define specific mechanisms of action of this drug in SSc.
References
Gabrielli A, Avvedimento EV, Krieg T. Scleroderma. N Engl J Med. 2009;360:1989–2003.
Goundry B, Bell L, Langtree M, Moorthy A. Diagnosis and management of Raynaud’s phenomenon. BMJ. 2012;344:e289.
Prete M, Fatone MC, Favoino E, Perosa F. Raynaud’s phenomenon: from molecular pathogenesis to therapy. Autoimmun Rev. 2014;13:655–67.
Baumhakel M, Bohm M. Recent achievements in the management of Raynaud’s phenomenon. Vasc Health Risk Manag. 2010;6:207–14.
Levien TL. Advances in the treatment of Raynaud’s phenomenon. Vasc Health Risk Manag. 2010;6:167–77.
Kowal-Bielecka O, Landewe R, Avouac J, et al. EULAR recommendations for the treatment of systemic sclerosis: a report from the EULAR Scleroderma Trials and Research Group (EUSTAR). Ann Rheum Dis. 2009;68:620–8.
Caramaschi P, Dalla Gassa A, Prati D, et al. Severe vascular complications in patients affected by systemic sclerosis cyclically treated with iloprost. Rheumatol Int. 2012;32:1933–8.
Kamal AK, Naqvi I, Husain MR, Khealani BA. Cilostazol versus aspirin for secondary prevention of vascular events after stroke of arterial origin. Cochrane Database Syst Rev. 2011;(1):CD008076.
Kanlop N, Chattipakorn S, Chattipakorn N. Effects of cilostazol in the heart. J Cardiovasc Med (Hagerstown). 2011;12:88–95.
Pearce L, Ghosh J, Counsell A, Serracino-Inglott F. Cilostazol and peripheral arterial disease. Expert Opin Pharmacother. 2008;9:2683–90.
Geng DF, Deng J, Jin DM, Wu W, Wang JF. Effect of cilostazol on the progression of carotid intima-media thickness: a meta-analysis of randomized controlled trials. Atherosclerosis. 2012;220:177–83.
Warner CJ, Greaves SW, Larson RJ, et al. Cilostazol is associated with improved outcomes after peripheral endovascular interventions. J Vasc Surg. 2014;59:1607–14.
Rajagopalan S, Pfenninger D, Somers E, et al. Effects of cilostazol in patients with Raynaud’s syndrome. Am J Cardiol. 2003;92:1310–5.
Preliminary criteria for the classification of systemic sclerosis (scleroderma). Subcommittee for scleroderma criteria of the american rheumatism association diagnostic and therapeutic criteria committee. Arthritis Rheum. 1980;23:581–90.
LeRoy EC, Black C, Fleischmajer R, et al. Scleroderma (systemic sclerosis): classification, subsets and pathogenesis. J Rheumatol. 1988;15:202–5.
Merkel PA, Herlyn K, Martin RW, et al. Measuring disease activity and functional status in patients with scleroderma and Raynaud’s phenomenon. Arthritis Rheum. 2002;46:2410–20.
La Montagna G, Cuomo G, Chiarolanza I, Ruocco L. Valentini G [HAQ-DI italian version in systemic sclerosis]. Reumatismo. 2006;58:112–5.
Steen VD, Medsger TA Jr. The value of the health assessment questionnaire and special patient-generated scales to demonstrate change in systemic sclerosis patients over time. Arthritis Rheum. 1997;40:1984–91.
Rollando D, Bezante GP, Sulli A, et al. Brachial artery endothelial-dependent flow-mediated dilation identifies early-stage endothelial dysfunction in systemic sclerosis and correlates with nailfold microvascular impairment. J Rheumatol. 2010;37:1168–73.
Fenoglio D, Battaglia F, Parodi A, et al. Alteration of Th17 and Treg cell subpopulations co-exist in patients affected with systemic sclerosis. Clin Immunol. 2011;139(3):249–57.
De Franciscis S, Gallelli L, Battaglia L, et al. Cilostazol prevents foot ulcers in diabetic patients with peripheral vascular disease. Int Wound J. 2015;12(3):250–3.
Kim WU, Min SY, Cho ML, et al. Elevated matrix metalloproteinase-9 in patients with systemic sclerosis. Arthritis Res Ther. 2005;7:R71–9.
Acknowledgments
This work was supported by Grants from: “Gruppo Italiano Lotta alla Sclerodermia (GILS).” The sponsors had no role in study design, in the collection, analysis and interpretation of data, in the writing of the report, and in the decision to submit the article for publication.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Gilberto Filaci and Francesco Puppo have contributed equally to this paper.
Rights and permissions
About this article
Cite this article
Negrini, S., Spanò, F., Penza, E. et al. Efficacy of cilostazol for the treatment of Raynaud’s phenomenon in systemic sclerosis patients. Clin Exp Med 16, 407–412 (2016). https://doi.org/10.1007/s10238-015-0370-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10238-015-0370-5