Abstract
Vasculopathy is a crucial feature of systemic sclerosis (SSc), and Raynaud’s phenomenon (RP) and digital ulcers (DU) have a deep impact on the quality of patients’ life. The management of vascular disease can be challenging for the clinician because of the suboptimal tolerability of the treatments and lack of consensus on the best therapeutic approach. Intravenous iloprost, a synthetic analogue of prostacyclin, is broadly used for the treatment of RP and ischemic ulcers secondary to SSc. However, no standardized protocol on iloprost use is currently available and, consequently, the management of this treatment is largely based on the experience of each single center. The PROSIT project is an observational, multicenter study aiming to investigate the current treatments for SSc vasculopathy, the use of prostanoids, with special regard to iloprost, and the perception of the treatment from a patient’s perspective. The study was conducted on a cohort of 346 patients from eight Italian centers and included a structured survey addressed to physicians, data collected from patient’s medical records and two patient-administered questionnaires assessing the level of satisfaction, tolerability and perception of the efficacy of Iloprost. PROSIT data confirmed that in the contest of SSc iloprost represents the first-line choice for the management of severe RP and DU. Moreover, it is a well-tolerated treatment as reported by patients’ experience. Although a standard protocol for the treatment of SSc-related vasculopathy is lacking, PROSIT study identified different therapeutic approaches largely supported by tertiary Italian centers. Further studies are needed in order to optimize the best treatment for SSc vascular diseases, in particular to improve the best iloprost schedule management.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Systemic sclerosis (SSc, scleroderma) is a chronic autoimmune systemic disease of unknown cause, characterized by immune dysregulation, microvasculopathy and diffuse tissue fibrosis [1, 2].
In SSc, the earliest and most typical manifestation of vascular involvement is Raynaud’s phenomenon (RP), which is the result of a disturbed control of the vascular tone. It involves small digital peripheral arteries, usually in response to cold exposure, resulting in impaired blood flow in the extremities (digits, ears, tongue). Clinically, RP is characterized by an initial phase of pallor caused by local ischemia, followed by cyanosis due to venous stasis and, finally erythema secondary to reactive hyperemia. RP secondary to SSc is characterized by structural changes in the vessels, and its early characterization is mandatory to early identify the patient affected by SSc [3] and to start specific treatments [4,5,6,7].
Digital ulcers (DU) represent an important cause of morbidity that affects 30 to 50% of SSc patients [8,9,10]. DU are defined as a “Loss of epidermal covering with a break in the basement membrane (which separates dermis from epidermis). It appears clinically as visible blood vessels, fibrin, granulation tissue and/or underlying deeper structures (e.g., muscle, ligament, fat) or as it would appear on debridement” [11]; they are typically found on the fingertips and are characterized by impaired function and local pain. DU are susceptible to complications, primarily infections, that potentially may progress to gangrene, osteomyelitis and amputation [8]. These complications, often requiring hospitalization, increase the burden of the disability and the cost of treatment in these patients [12,13,14]. Therefore, a local and systemic treatment for SSc-related vasculopathy represents a priority for the clinicians dealing with SSc [15,16,17].
Although pathophysiological mechanisms of SSc are still elusive, vascular damage is generally considered as an early event in the history of the disease [18]. In the context of the SSc-related endothelial dysfunction, the alteration of the normal balance between vasodilating agents, such as prostacyclin, and vasoconstricting factors, such as thromboxane A2, seems to play a pivotal role [19, 20]. Prostacyclin (also known as prostaglandin I2) is a member of the prostaglandin family, physiologically produced by endothelial cells through the cyclooxygenase–arachidonic pathway. Prostacyclin exerts vasodilators and antithrombotic and antiproliferative effects that are essential for endothelial function [21].
Vasodilating agents represent a cornerstone in the treatment of SSc-related vascular disease, allowing the reduction of vasospastic phenomenon as RP, occlusion of vessels and occurrence of DU. The most commonly used drugs for the treatment of SSc-related vasculopathy are summarized in Table 1. According to the latest European League Against Rheumatism (EULAR) recommendations [22], the pharmacological management of digital vasculopathy (i.e., RP and DU) secondary to SSc includes different therapeutic approaches. Dihydropyridine-type calcium channel blockers (CCBs) are indicated for first-line treatment for SSc-RP. Phosphodiesterase type 5 inhibitors (PDE5i) could be considered in SSc patients with severe RP and/or in those non-responders to CCBs. Intravenous iloprost is indicated for severe SSc-RP, when oral therapy (including CCBs and PDE5i) has failed. In addition, intravenous iloprost or PDE5i are also recommended for the treatment of DU secondary to SSc. It emerges clearly that prostanoids, and in particular iloprost, represent a significant option in the treatment of SSc vasculopathy. Iloprost, a synthetic analogue of prostacyclin PGI2, is a second-generation structural analogue of prostacyclin with an increased potency if compared with first-generation stable analogues (e.g., carbaprostacyclin). Iloprost binds to human prostacyclin and prostaglandin E2 receptors with equal affinity. It inhibits the ADP, thrombin and collagen-induced aggregation of human platelets resulting in antiplatelet, cytoprotective and immuno-modulating properties and in dilatation of systemic and pulmonary arterial vascular beds [23,24,25]. In SSc, iloprost has been used to fight RP and DU and in its version also pulmonary hypertension.
The standard protocol provided for the use of iloprost in RP consists of intravenous administration via infusion pump progressively increasing the dose until reaching the maximum tolerated dose, starting at a rate of 0.5 ng/kg/min to a maximum of 2 ng/kg/min for 6–8 h/day. Many studies disclosed the efficacy of iloprost for treatment of secondary RP with benefit confirmed in the short and long terms [26,27,28,29,30,31,32]. More recently, the capacity of the Iloprost to stabilize the disease has been addressed [33, 34]. The optimal regimen for iloprost in SSc still remains undefined. In fact, the main unmet need is a standardized guideline or clinical recommendation to guide the choice of the treatment regimens [35]. The aim of the PROSIT [Utilizzo dei PROstanoidi endovenoSI nel Trattamento della vasculopatia sclerodermica (the use of intravenous prostanoids in the treatment of SSc-related vasculopathy)] multicenter study was to verify the iloprost therapeutic regimens employed in Italian tertiary referral centers in the treatment of SSc vasculopathy. The study investigated also the quality of life of SSc patients treated with Iloprost.
Methods
Centers
The PROSIT study was conducted between January 2016 and February 2017 in eight selected tertiary referral centers identified by the Italian Group against Scleroderma (GILS, Gruppo Italiano per la Lotta alla Sclerodermia) that supported the research: Department of Internal Medicine, University of Genoa, Policlinico San Martino (Genoa); Department of Experimental and Clinical Medicine, AOUC University of Florence (Florence); Internal Medicine, San Luigi Gonzaga Hospital Orbassano (Torino); Fondazione IRCCS Ca’ Granda, Ospedale Maggiore Policlinico di Milano, (Milan); Rheumatology Unit, Department of Clinical and Experimental Medicine, University of Pisa (Pisa); Rheumatology Unit University of Modena and Reggio Emilia, Azienda Ospedaliero Universitaria (Modena); Rheumatology Unit Fondazione Policlinico Universitario A. Gemelli IRCCS (Rome); and Rheumatology Unit ARNAS Garibaldi (Catania).
The study was approved by local ethics committees and conducted in accordance with the principles of the Declaration of Helsinki; all patients signed a written informed consent.
Inclusion/exclusion criteria
Inclusion criteria were: (a) age ≥ 18 years at the beginning of iloprost treatment; (b) classification of SSc, according to the 2013 ACR/EULAR classification criteria [36]; (c) presence of RP or DU related to SSc at the beginning of iloprost treatment; (d) long-term treatment with iloprost for at least 12 months at the time of enrollment without any limitation of dosage or strategy of administration. All the patients were consecutive. Patients with primary RP were excluded from the study. There were no limitations for combination treatments for SSc or other comorbidities.
Study procedures
PROSIT project was designed as an observational, retrospective, multicenter study conducted in eight Italian scleroderma units.
Data analyzed in PROSIT study were obtained as follows: (1) Experts’ opinion on management of SSc-related vasculopathy was investigated through a multi-choice question survey addressed to the experts of the eight Italian referral centers; (2) clinical and epidemiological data of iloprost treated patients were retrospectively obtained from patient’s medical records; (3) patients’ point of view on iloprost treatment and its impact on their quality of life were investigated through two patient-administered questionnaires: the “Treatment Satisfaction Questionnaire for Medication” and a second questionnaire specifically elaborated for the study with the aim of specifically investigating the perception of iloprost treatment by SSc patients. A total number of 346 SSc patients with RP and/or DU were enrolled according with inclusion criteria. Treatment Satisfaction Questionnaire for Medication (TSQM), vers.1.4, is validated as useful tool in several studies on different conditions [37,38,39]. Briefly, TSQM is structured in four scales that explore effectiveness, side effects, convenience and the global satisfaction of the patient toward the treatment. Item scores are summed to give four domain scores, which are in turn transformed to a scale of 0–100, with higher scores indicating greater satisfaction [37]. In order to analyze results, an algorithm scoring was applied [37]. Internal consistency reliability analysis was calculated with Cronbach α [40]; reliability coefficients greater than 0.70 were considered acceptable.
Results
Management of SSc-related vasculopathy
In the PROSIT cohort, RP represented the main indication for iloprost treatment (n = 187, 54%), while the remaining patients (n = 159, 46%) received the drug for treatment and/or prevention of DU.
Management of moderate Raynaud’s phenomenon (< 10 attacks/week)
All centers consider CCBs as first-line treatment for the management of moderate RP. CCBs were used in association with antiplatelet drugs for the majority of the experts (5 out of 8). In the case of failure of the first-line treatment, experts agreed to add a new drug to the ongoing treatment (7 out of 8) instead of switching to a new one (1 out of 8). Iloprost was the most commonly employed second-line drug for patients with moderate RP: Alternative options were pentoxifylline, ERA, cilostazol or PDE5i.
Management of severe Raynaud’s phenomenon (≥ 10 attacks/week)
The use of CCBs was supported by 7/8 experts as the first-line treatment for the severe RP. In these cases, CCBs was employed in combination with iloprost (4/8) and/or antiplatelet therapy (5/8). In case of treatment failure, all experts suggested to combine a new treatment, but the choice of the second-line treatments was very heterogeneous across centers.
Prevention of DU
First-line strategy for the prevention of new DU in patients with a history of DU was represented by a combination therapy. The most common combination was CCBs and antiplatelet (6/8) with iloprost (4/6). Three centers of the four employing CCBs–antiplatelet–iloprost reported also the use of endothelial receptor antagonists (ERAs). All investigators agreed to add a further drug in patients not responding to treatment. The most frequently drug employed as second-line treatment was PDE5i.
Digital Ulcers
All experts agreed to the use of iloprost, associated with CCBs and/or ERAs, as first option for the treatment of DU. All investigators suggested to add new drugs in non-responder patients (100%). According to the majority of the interviewed experts (5/8), DU and severe vasculopathy manifestations (e.g., critical ischemia) were managed with daily infusion of iloprost until resolution. Recommended strategies for the management of SSc-related vasculopathy derived from PROSIT study are summarized in Table 2.
Iloprost infusion length and dosage
Concerning iloprost infusion length, four experts suggested a 6–8 h infusion, while three centers favored a 4–6-h regimen. Only one center employs a longer infusion schedule (8–12 h). Volumetric infusion pump was the device most commonly used for the continuous intravenous administration, and the suggested infusion rate ranges from 0.5 to 2.0 ng/kg/min. In 5/8 centers, the rate of iloprost infusion was titrated to the maximum tolerated dose without exceeding the limit of 2 ng/kg/min, whereas in the remaining centers, drug dose was adjusted only according to individual tolerability.
Iloprost infusion regimens
Iloprost schedule consisted in periodic infusions, ranging from one to more consecutive days. The intervals between administrations was generally 30 days (7/8), and for maintenance regimen (i.e., infusions following the induction), the majority of the experts adopted the once a month infusion (6/8). During the summer, the treatment was withdrawn in 3/8 centers, while the remaining centers continued the treatment.
Management of concomitant therapies during iloprost administration
To treat RP and/or for the prevention of DU, the majority of Italian centers (respectively, 5/8 and 6/8) used antiplatelet agents in combination with CCBs. None of the centers reported bleeding, and for 7/8 centers the potential antiplatelet interaction was of no concern. None of the centers advised interruption of antiplatelet agent during or in prevision of iloprost infusion. Four centers stopped vasodilators during iloprost infusion, three reduced the dosage reduction, and only one center maintained the vasodilators schedule unchanged during the days of iloprost infusion.
The most commonly adopted regimens for iloprost administration resulted from PROSIT study are summarized in Table 3.
Characteristics of SSc patients treated with iloprost
A total of 346 patients were included in the study, with no patient lost to follow-up. The characteristics of the patients enrolled in the PROSIT protocol are summarized in Table 4. As expected, the majority of patients (n: 298, 86.2%) were females, and the cohort was characterized by a prevalence of limited cutaneous subset (68.8%).
Serologically, the majority of patients presented anticentromere (136–39.3%) or anti-Scl70 (124–35.8%) antibodies. We observed a significant time delay from the first manifestation of SSc, generally RP, and the referral to a specialized center (6.3 years on average). Usually, SSc diagnosis occurred during the fifth decade of age. In our cohort, 63% of patients experienced DU, involving, as expected, more frequently the hands (86%) as compared to lower limbs (14%). Iloprost was usually prescribed for patients with a diagnosis of SSc satisfying the currently available classification criteria. It is worth of note that six centers considered its use also in the very early scleroderma patients. The mean iloprost dosage was 1.5 (± 0.5) ng/kg/min. In 52% of patients, the velocity of infusion did not change throughout the years: 34% of the patients reported an improved tolerability (allowing an increase of the dose over the years), while 14% of the patients only showed a decreased tolerability leading to a reduced infusion velocity. With reference to patients that increased the infusion rate over time, the improvement of tolerability was spontaneous in 60% of the cases and related to concomitant administration of premedication in the remaining percentage of patients.
Side effects, including hypotension, headache, flushing, nausea, vomiting and diarrhea, were reported by 61% of the interviewed patients. Side effects were described as mild by 57% of the patients, moderately to very annoying in 40% of the cases, while only 3% of the patients reported extremely annoying side effects. The majority of patients (86%) reported that side effects disappeared immediately or within few hours after infusion, whereas only 14% of patients experienced more prolonged symptoms. In order to limit the potential side effects related to iloprost infusion, experts agreed with the adoption of a premedication, routinely (5/8) or electively (3/8). Usually, paracetamol was the first adopted drug to reduce migraine, whereas dopamine receptor antagonists, both central (e.g., metoclopramide) and peripheral (e.g., domperidone), were the preferred medications to limit nausea and vomiting.
Patient’s point of view
TSQM was administered to patients to investigate their satisfaction with iloprost treatment. Mean satisfaction scores observed across all TSQM domain ranged from 55.5 to 66.2%. The highest satisfaction scores were observed for the side effect item, whereas convenience and overall satisfaction items demonstrated a lower mean satisfaction value (data summarized in Table 4). In order to assess the internal consistency reliability, the Cronbach α for the four TSQM scales was calculated finding good values for the Effectiveness (0.83) and Overall Satisfaction (0.86) and acceptable results for Side Effects (0.72) and Convenience (0.78) summary scales (Table 5). These values are in agreement with those reported in the original TSQM validation studies [37,38,39].
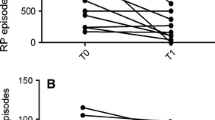
The perceived impact of the treatment on the number and severity of RP attacks was investigated among the PROSIT cohort. Concerning the number of RP attacks, 52% of the patients reported a decrease, 37% observed stability, and only 11% perceived an increase in the RP attacks’ frequency. Moreover, 55% of the patients reported a reduction of RP attacks, 33% reported stability, and only a minority (12%) reported an increase of RP severity.
After the introduction of iloprost, the majority of patients (74%) with DU declared a reduction of the severity and frequency of the lesions. In the 36% of the patients that experienced calcinosis, 54% reported positive effect of iloprost as reduction of severity and frequency of calcinosis, whereas 46% did not observe any improvement.
The impact of iloprost treatment on patients’ working and social activity was investigated through two different 10-point Likert scales ranging from 0 (no impact) to 10 (maximum impact): The results are summarized in Fig. 1. Although the limitation of the infusion regimen, patients reported that iloprost treatment does not affect, or minimally influence, their working activity (impact on working activity: median 1, IQR 0–4). Regarding the consequences of iloprost treatment on patients’ social life, the majority of the cohort reported no (or very low) influence (impact social activity: median 2, IQR 1–5).
Discussion
Currently, the treatment of SSc-related RP and DU includes non-pharmacologic, pharmacologic and surgical intervention. A survey to evaluate experts’ attitude toward the management of SSc-related vasculopathy has been conducted by the Canadian Scleroderma research group [41] and by the UK Scleroderma Study group [42]. Both studies despite the difficulty to obtain a complete agreement among interviewed experts represent a helpful guidance for the clinician and provide references and treatment algorithms to facilitate the management of SSc-related complications including RP, DU and critical ischemia. Overall, our data do not differ from the currently available guidelines or recommendations for the management of SSc-related vasculopathy [22, 41,42,43]. In the contest of RP management, UK experts suggested the use of iloprost for refractory cases, similarly to what was reported by the experts from Italian Scleroderma Units. Conversely, the majority of the experts from the Canadian survey indicated iloprost as fourth-line treatment or second-/third-line treatment option for moderate or severe RP management, respectively. In addition, the same experts reported an early use of PDE5i, typically after CCBs. According to PROSIT experts, iloprost is used earlier, namely in combination or immediately after CCBs. Interestingly, a regression analysis conducted on a single series of patients identified the delay in beginning iloprost therapy as a variable significantly associated with the development of ischemic DU [44]. These data support the use of prostanoids, both alone and in combination with CCBs, in an early phase of the disease in order to prevent the development of more severe manifestations of vasculopathy such as DU or critical ischemia. The PROSIT study clearly shows that PDE5i is more rarely prescribed and are generally employed as late treatment for RP. This dissimilarity probably reflects the different accesses to treatment and country-specific drug indications. Similarly to what observed for RP, data form Italian Scleroderma Units indicate a predominant use of prostanoids, as compared to PDE5i, for both the prevention and treatment of DU. However, PDE5i were used for the treatment of refractory DU also in our cohort, accordingly to the results reported in other studies [45,46,47].
As reported in the literature, digital vascular complications occur more frequently in patients with SSc who are current smokers [48]. In our cohort, more than 10% of the patients were smokers, despite the well-known negative effects of smoke on cardiovascular and pulmonary systems. The literature reports the benefit of smoking cessation on RP [49, 50], and therefore, SSc patients should be encouraged to quit smoking. Similarly to what is described in other autoimmune disorders and SSc [51], a delay for the referral to a specialized center (6.6 years on average) was observed. This delay represents a hurdle for the optimal management of the patient in order to prevent the burden of complications. Consequently, efforts should be made to improve early diagnosis and referral to specialized centers.
The PROSIT study investigated also the regimen of administration of iloprost, and in particular, the dosage, the frequency, the rate and the length of infusion. We observed that adopted regimen in our patients does not differ from what was reported in iloprost seminal studies [27, 28, 32, 52] and the most recent expert consensus paper [35]. It is worth to underline that the occurrence of side effects was dose dependent and that some patients seem to be intolerant to iloprost [31]. A randomized single-center study demonstrated a comparable efficacy of the low-dose versus the high-dose treatment [53], suggesting the possibility to modulate the dosage accordingly to the tolerability of the patients, in order to improve patient adherence to treatment and limit its withdrawal. Our experts agreed on attempting to reach the maximum tolerated dose for each single patient. However, hypersensitive patients may still benefit from iloprost treatment even at lower/tolerated dosage. In addition, tolerability may be improved by the use of premedication as paracetamol or central dopamine antagonist and/or the suspension or dosage reduction of concomitant vasoactive medications. Interestingly, antiplatelet agents were not withdrawn in the majority of patients, since there is no clear evidence of increased risk of bleeding combining the two drugs.
Concerning the interval between iloprost infusions, almost all of the PROSIT experts agreed for a monthly administration, in agreement with the well-known evidence that iloprost beneficial effects may last for some weeks [28, 32]. The majority of centers adopted a single-day infusion as maintenance. Recently, imaging tools (for example, power Doppler US) have been proposed to investigate the acute and chronic effect of different iloprost infusion regimen without observing, however, any benefit [54]. Consequently, the issue of the timing of infusions remains open and specific trials comparing different schedules of maintenance infusion are warranted.
Patients’ opinion on iloprost therapy was investigated with a validated Treatment Satisfaction Questionnaire (TSQM) and an iloprost-specific questionnaire elaborated ad hoc for this study. To the best of our knowledge, the PROSIT study is the first investigation to address patient perception of intravenous iloprost treatment through TSQM. TSQM showed a moderate level of satisfaction among interviewed SSc patients; this observation may be explained as follows: (1) the efficacy of the treatment is difficult to be perceived by the patients since the drug is used to prevent complications such as DU or reduce, rather than eliminate, the intensity and number of RP attacks; (2) TSQM efficacy-oriented questions are probably more appropriate to evaluate drugs capable to rapidly modify a given sign (e.g., blood pressure levels) or symptom (e.g., pain). However, when specific questions were administered, only a minority of patients reported a perception inefficacy of the treatment on RP or DU (11% and 12%, respectively). Sixty-one percent of patients reported side effects that are mild, and consequently, the level of satisfaction with their impact was acceptable. Iloprost administration needs prolonged infusions in a hospital setting that may negatively influence the perceived satisfaction of patients. Likely, this explains the low TSQM score registered in the convenience item and could compromise, in some cases, the treatment adherence. To this purpose, portable infusion devices have been proposed in order to allow iloprost infusions in a home-based setting [55, 56]. As expected, all the above-mentioned criticisms influenced the global perception of the treatment as reflected by the overall satisfaction score.
Conclusion
Iloprost is widely used across tertiary Italian centers in the management of SSc-related vasculopathy. The schedule of iloprost administration, emerged from our survey, is homogeneous among the scleroderma units, and this same protocol could be extended in those centers with a limited experience with SSc management and iloprost administration. Interesting information about patients’ perspective concerning iloprost has also been obtained. Nevertheless, other questions remain to be addressed; in particular, if a given treatment’s schedule is superior to alternative regimens, our observations would need to be completed by a prospective comparison study analyzing different iloprost administration schedules in order to standardize the optimal treatment option.
Abbreviations
- SSc:
-
Systemic sclerosis
- RP:
-
Raynaud phenomenon
- DU:
-
Digital ulcers
- EULAR:
-
European League Against Rheumatism
- CCBs:
-
Dihydropiridine-type calcium channel blockers
- PDE5i:
-
Phosphodiesterase type 5 inhibitors
- PROSIT:
-
Utilizzo dei PROstanoidi endovenoSI nel Trattamento della vasculopatia sclerodermica
- GILS:
-
Gruppo Italiano Lotta alla Sclerodermia
- ACR:
-
American College of Rheumatology
- TSQM:
-
Treatment Satisfaction Questionnaire for medication
- ERAs:
-
Endothelial receptor antagonists
References
Varga J, Trojanowska M, Kuwana M. Pathogenesis of systemic sclerosis: recent insights of molecular and cellular mechanisms and therapeutic opportunities. J Scleroderma Relat Disord. 2017;2:137–52.
Negrini S, Fenoglio D, Parodi A, et al. Phenotypic alterations involved in CD8+ Treg impairment in systemic sclerosis. Front Immunol. 2017;8:18.
LeRoy EC, Medsger TA. Criteria for the classification of early systemic sclerosis. J Rheumatol. 2001;28:1573–6.
Herrick AL. Pathogenesis of Raynaud’s phenomenon. Rheumatology. 2005;44:587–96.
Maverakis E, Patel F, Kronenberg DG, et al. International consensus criteria for the diagnosis of Raynaud’s phenomenon. J Autoimmun. 2014;48–49:60–5.
Prete M, Fatone MC, Favoino E, Perosa F. Raynaud’s phenomenon: from molecular pathogenesis to therapy. Autoimmun Rev. 2014;13:655–67.
Negrini S, Spanò F, Penza E, et al. Efficacy of cilostazol for the treatment of Raynaud's phenomenon in systemic sclerosis patients. Clin Exp Med. 2016;16(3):407–12.
Allanore Y, Denton CP, Krieg T, et al. Clinical characteristics and predictors of gangrene in patients with systemic sclerosis and digital ulcers in the Digital Ulcer Outcome Registry: a prospective, observational cohort. Ann Rheum Dis. 2016;75(9):1736–40.
Guillevin L, Hunsche E, Denton CP, et al. Functional impairment of systemic scleroderma patients with digital ulcerations: results from the DUO Registry. Clin Exp Rheumatol. 2013;31:71–80.
Matucci-Cerinic M, Krieg T, Guillevin L, et al. Elucidating the burden of recurrent and chronic digital ulcers in systemic sclerosis: long-term results from the DUO Registry. Ann Rheum Dis. 2016;75:1770–6.
Suliman YA, Bruni C, Johnson SR, et al. Defining skin ulcers in systemic sclerosis: systematic literature review and proposed world scleroderma foundation (WSF) definition. J Scleroderma Relat Disord. 2017;2:115–20.
Mouthon L, Mestre-Stanislas C, Bérezné A, et al. Impact of digital ulcers on disability and health-related quality of life in systemic sclerosis. Ann Rheum Dis. 2010;69:214–7.
Mouthon L, Carpentier PH, Lok C, et al. Ischemic digital ulcers affect hand disability and pain in systemic sclerosis. J Rheumatol. 2014;41:1317–23.
Nihtyanova SI, Brough GM, Black CM, Denton CP. Clinical burden of digital vasculopathy in limited and diffuse cutaneous systemic sclerosis. Ann Rheum Dis. 2008;67:120–3.
Abraham S, Steen V. Optimal management of digital ulcers in systemic sclerosis. Ther Clin Risk Manag. 2015;11:939–47.
Galluccio F, Matucci-Cerinic M. Two faces of the same coin: Raynaud phenomenon and digital ulcers in systemic sclerosis. Autoimmun Rev. 2011;10(5):241–3.
Hughes M, Herrick AL. Digital ulcers in systemic sclerosis. Rheumatology (Oxford). 2017;56(1):14–25.
Matucci-Cerinic M, Kahaleh B, Wigley FM. Review: evidence that systemic sclerosis is a vascular disease. Arthritis Rheum. 2013;65:1953–62.
Sunderkotter C, Riemekasten G. Pathophysiology and clinical consequences of Raynaud’s phenomenon related to systemic sclerosis. Rheumatology. 2006;45:iii33–5.
Kahaleh M. Vascular involvement in systemic sclerosis (SSc). Clin Exp Rheumatol. 2004;22:S19–23.
Mitchell JA, Ahmetaj-Shala B, Kirkby NS, et al. Role of prostacyclin in pulmonary hypertension. Glob Cardiol Sci Pract. 2014;2014:53.
Kowal-Bielecka O, Fransen J, Avouac J, et al. Update of EULAR recommendations for the treatment of systemic sclerosis. Ann Rheum Dis. 2017;76:1327–39.
Della Bella S, Molteni M, Mascagni B, Zulian C, Compasso S, Scorza R. Cytokine production in scleroderma patients: effects of therapy with either iloprost or nifedipine. Clin Exp Rheumatol. 1997;15:135–41.
Dowd PM, Martin MFR, Cooke ED, et al. Treatment of Raynaud’s phenomenon by intravenous infusion of prostacyclin (PGI2). Br J Dermatol. 1982;106:81–9.
Krause W, Krais T. Pharmacokinetics and pharmacodynamics of the prostacyclin analogue iloprost in man. Eur J Clin Pharmacol. 1986;30:61–8.
Wigley FM, Seibold JR, Wise RA, McCloskey DA, Dole WP. Intravenous iloprost treatment of Raynaud’s phenomenon and ischemic ulcers secondary to systemic sclerosis. J Rheumatol. 1992;19:1407–14.
McHugh NJ, Csuka M, Watson H, et al. Infusion of Iloprost, a prostacyclin analogue, for treatment of Raynaud’s phenomenon in systemic sclerosis. Ann Rheum Dis. 1988;47:43–7.
Scorza R, Caronni M, Mascagni B, et al. Effects of long-term cyclic iloprost therapy in systemic sclerosis with Raynaud’s phenomenon. A randomized, controlled study. Clin Exp Rheumatol. 2001;19(5):503–8.
Torley HI, Madhok R, Capell HA, et al. A double blind, randomised, multicentre comparison of two doses of intravenous iloprost in the treatment of Raynaud’s phenomenon secondary to connective tissue diseases. Ann Rheum Dis. 1991;50:800–4.
Ceru S, Pancera P, Sansone S, et al. Effects of five-day versus one-day infusion of iloprost on the peripheral microcirculation in patients with systemic sclerosis. Clin Exp Rheumatol. 1997;15:381–5.
Rademaker M, Cooke ED, Almond NE, et al. Comparison of intravenous infusions of iloprost and oral nifedipine in treatment of Raynaud’s phenomenon in patients with systemic sclerosis: a double blind randomised study. BMJ. 1989;298:561–4.
Wigley FM, Wise RA, Seibold JR, et al. Intravenous iloprost infusion in patients with Raynaud phenomenon secondary to systemic sclerosis: a multicenter, placebo-controlled, double- blind study. Ann Intern Med. 1994;120:199–206.
Foti R, Visalli E, Amato G, et al. Long-term clinical stabilization of scleroderma patients treated with a chronic and intensive IV iloprost regimen. Rheumatol Int. 2017;37:245–9.
Airò P, Rossi M, Scarsi M, Danieli E, Grottolo A, Zambruni A. Disease-modifying effects of long-term cyclic iloprost therapy in systemic sclerosis, A retrospective analysis and comparison with a control group. Clin Exp Rheumatol. 2007;25:722–7.
Ingegnoli F, Schioppo T, Allanore Y, et al. Practical suggestions on intravenous iloprost in Raynaud’s phenomenon and digital ulcer secondary to systemic sclerosis: systematic literature review and expert consensus. Semin Arthritis Rheum. 2019;48(4):686–693.
Van Den Hoogen F, Khanna D, Fransen J, et al. 2013 classification criteria for systemic sclerosis: an american college of rheumatology/European league against rheumatism collaborative initiative. Arthritis Rheum. 2013;65:2737–47.
Atkinson MJ, Kumar R, Cappelleri JC, Mass SL. Hierarchical construct validity of the Treatment Satisfaction Questionnaire for Medication (TSQM Version II) among outpatient pharmacy consumers. Value Health. 2005;8:S9–24.
Atkinson MJ, Sinha A, Hass SL, et al. Validation of a general measure of treatment satisfaction, the Treatment Satisfaction Questionnaire for Medication (TSQM), using a national panel study of chronic disease. Health Qual Life Outcomes. 2004;2:12.
Bharmal M, Payne K, Atkinson MJ, Desrosiers MP, Morisky DE, Gemmen E. Validation of an abbreviated Treatment Satisfaction Questionnaire for Medication (TSQM-9) among patients on antihypertensive medications. Health Qual Life Outcomes. 2009;27:7–36.
Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16:297–334.
Walker KM, Pope J, participating members of the Scleroderma Clinical Trials Consortium (SCTC), Canadian Scleroderma Research Group (CSRG). Treatment of systemic sclerosis complications: what to use when first-line treatment fails—a consensus of systemic sclerosis experts. Semin Arthritis Rheum. 2012;42:42–55.
Hughes M, Ong VH, Anderson ME, et al. Consensus best practice pathway of the UK Scleroderma Study Group: digital vasculopathy in systemic sclerosis. Rheumatology. 2015;54:2015–24.
Denton CP, Hughes M, Gak N, et al. BSR and BHPR guideline for the treatment of systemic sclerosis. Rheumatology (Oxford). 2016;55:1906–10.
Caramaschi P, Martinelli N, Volpe A, et al. A score of risk factors associated with ischemic digital ulcers in patients affected by systemic sclerosis treated with iloprost. Clin Rheumatol. 2009;28:807–13.
Fries R, Shariat K, von Wilmowsky H, Böhm M. Sildenafil in the treatment of Raynaud’s phenomenon resistant to vasodilatory therapy. Circulation. 2005;112:2980–5.
Hachulla E, Hatron P-Y, Carpentier P, et al. Efficacy of sildenafil on ischaemic digital ulcer healing in systemic sclerosis: the placebo-controlled SEDUCE study. Ann Rheum Dis. 2016;75:1009–15.
Brueckner CS, Becker MO, Kroencke T, et al. Effect of sildenafil on digital ulcers in systemic sclerosis: analysis from a single centre pilot study. Ann Rheum Dis. 2010;69:1475–8.
Harrison BJ, Silman AJ, Hider SL, Herrick AL. Cigarette smoking as a significant risk factor for digital vascular disease in patients with systemic sclerosis. Arthritis Rheum. 2002;46:3312–6.
Leask A. When there’s smoke there’s…scleroderma: evidence that patients with scleroderma should stop smoking. J Cell Commun Signal. 2011;5(1):67–8.
Hudson M, Lo E, Lu Y, Hercz D, Baron M, Steele R. Cigarette smoking in patients with systemic sclerosis. Arthritis Rheum. 2011;63:230–8.
Distler O, Allanore Y, Denton CP, et al. Factors influencing early referral, early diagnosis and management in patients with diffuse cutaneous systemic sclerosis. Rheumatology (Oxford). 2018;57:813–7.
Watson HR, Belcher G. Retrospective comparison of iloprost with other treatments for secondary Raynaud’s phenomenon. Ann Rheum Dis. 1991;50:359–61.
Kawald A, Burmester GR, Huscher D, Sunderkötter C, Riemekasten G. Low versus high-dose iloprost therapy over 21 days in patients with secondary Raynaud’s phenomenon and systemic sclerosis: a randomized, open, single-center study. J Rheumatol. 2008;35(9):1830–7.
Schioppo T, Orenti A, Boracchi P, De Lucia O, Murgo A, Ingegnoli F. Acute and chronic effects of two different intravenous iloprost regimens in systemic sclerosis: a pragmatic non-randomized trial. Rheumatology (Oxford). 2018;57:1408–16.
Fraticelli P, Martino GP, Murri M, Mattioli M, Gabrielli A. A novel iloprost administration method with portable syringe pump for the treatment of acral ulcers and Raynaud’s phenomenon in systemic sclerosis patients. A pilot study (ILOPORTA). Clin Exp Rheumatol. 2017;35:S173–8.
Laria A, Lurati AM, Re KA, et al. User preference for a portable syringe pump for iloprost infusion. Patient Relat Outcome Meas. 2015;6:139–44.
Acknowledgements
This work was supported by Grants from Gruppo Italiano Lotta alla Sclerodermia (GILS). The sponsors had no role in study design, in the collection, analysis and interpretation of data, in the writing of the report, and in the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
SN, LB, MCC, FI and OM were responsible for study conception and design, statistical analysis and interpretation of data, and writing and revising the article. All authors contributed to patients’ recruitment and data collection. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Authors declared that they have not competing interests.
Availability of data and material
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
The study was approved by local ethics committees and conducted in accordance with the principles of the Declaration of Helsinki; all patients signed a written informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Negrini, S., Magnani, O., Matucci-Cerinic, M. et al. Iloprost use and medical management of systemic sclerosis-related vasculopathy in Italian tertiary referral centers: results from the PROSIT study. Clin Exp Med 19, 357–366 (2019). https://doi.org/10.1007/s10238-019-00553-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10238-019-00553-y