Abstract
Introduction
Patients with moderate to severe allergic asthma have persistent poorly controlled asthma despite inhaled or systemic corticosteroid therapy. New therapies are becoming more widely available to treat such patients, but their value needs to be formally assessed in an economic evaluation. Within a publicly funded health care system such an analysis should reflect societal preferences when measuring treatment benefits. The aim of this study was to elicit societal preferences for the symptom burden associated with moderate to severe allergic asthma.
Method
Existing daily symptom diary data from a clinical trial were used to develop health state descriptions for evaluation in a standard gamble interview. Five health states were produced that reflected five distinct levels of control ranging from ‘complete control of asthma’ to ‘worsening of asthma’, as defined by another outcome measure. The symptom diary data were also used as attributes in a discrete choice experiment (DCE) to estimate willingness to pay for improvements in symptoms. Members of the general public (n = 101) completed the interview.
Results
Thirteen participants failed the consistency checks and were excluded from the analysis. Societal utility ratings for the health states ranged from 0.71 (worsening of asthma) to 0.78 (complete control of asthma). The participants were also willing to pay £160 a month for the avoidance of all symptoms.
Conclusions
The range of utility values (0.71–0.78) demonstrates the severity of moderate to severe allergic asthma. However the spread of scores between complete control of asthma and worsening of asthma was lower than was expected. The community sample placed only a moderate value on the avoidance of all asthma symptoms in the DCE survey. The results suggest that the community sample may not have fully understood the benefits of control over asthma symptoms and the limitations such symptoms can impose on everyday life.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Asthma can be classified in terms of its severity and the treatment required to control symptoms and exacerbations [6, 17]. There is a substantial group of patients who have poorly controlled moderate to severe asthma despite modern treatments. Inhaled and even oral corticosteroid therapy is often not sufficient to control the symptoms of their disease. Such patients remain at increased risk for severe exacerbations. In reviewing this area Marshall and Sorkness [16] conclude that these patients are characterised by regular use of high-dose inhaled corticosteroids and systemic corticosteroids, excessive use of asthma rescue medications, and poor adherence to therapy. In addition these patients experience poor health-related quality of life (HRQL) and a history of frequent unscheduled visits to their doctor, or the emergency department at their hospital, and also frequent hospital admissions [16]. These patients also miss a substantial number of work and/or school days as a result of asthma [16].
Innovative new therapies have been developed to improve symptom control in patients with moderate to severe allergic asthma such as anti-IgE monoclonal antibodies [2, 4, 9, 22]. These trials assessed treatment effectiveness in terms of exacerbation rates, symptom burden, HRQL and a global measure of treatment effectiveness called the GETE (global evaluation of treatment effectiveness).
Treatments for asthma offer benefit for patients by reducing their risk of exacerbations and also reducing their day-to-day symptom burden. We have previously undertaken work which was designed to capture the HRQL burden of exacerbations in this patient sample [12]. This study used the EQ-5D to capture the utility of acute exacerbations in moderate to severe asthma. However no HRQL data exist which demonstrate the value of day-to-day symptom reduction in moderate to severe asthma which would be suitable for use in an economic evaluation. The present study therefore was designed to try to estimate the value in changes in day-to-day symptoms. The day-to-day change in patients’ symptoms was assessed through the use of asthma symptom diaries. These symptom diaries asked patients to classify their asthma symptoms in terms of night time, morning and daytime symptoms including activity limitations and use of rescue medication.
The present study was designed to capture preferences for changes in symptoms. This was captured in terms of both health utility and also in monetary terms as willingness to pay (WTP). Preferences of the general public were elicited in order to meet the requirements of economic evaluations in a publicly funded health care system [7]. Willingness to pay for changes in the severity of symptoms was also estimated using a discrete choice experiment (DCE). The different preference elicitation methodologies were used to gain a more thorough understanding of the preferences of participants in terms of WTP and cardinal health utilities. Specific health states were developed to describe the symptom burden corresponding to different levels of the GETE, and these were evaluated using the standard gamble (SG) and visual analogue scale (VAS) methods.
Methods
Development of health states
Secondary analysis of clinical trial data was undertaken to summarise differences in the symptom burden-associated different levels of treatment response as defined by the patient GETE. The GETE is a single item global measure of perceived treatment effectiveness whereby patients are asked to separately rate treatment effectiveness at the end of the study period. The scale has five levels ranging from ‘complete control of asthma’ to ‘marked improvement in asthma’, ‘discernible but limited improvement in asthma’, ‘no appreciable change in asthma’ to ‘worsening of asthma’. The GETE therefore presents a convenient method for stratifying patients in order to produce health states. Data from the INNOVATE trial [9] were analysed in order to characterise the five GETE levels in terms of symptom burden. The INNOVATE study is a randomised, placebo-controlled trial of a novel therapy for patients with severe persistent asthma (meeting the GINA [6] definition of severe persistent asthma). GETE was collected at the end of the study (week 28) and so the symptom diary data from week 28 were summarised for patients at each level of the GETE. We wanted to describe health at a specific point in time and so only data from this week were used.
The symptom diary included information regarding nocturnal, morning and daytime symptoms including the need for reliever medication and limitations on activities. Nocturnal symptoms were scored on a five-point scale from 0 (no symptoms at all) to 4 (difficulty sleeping because of breathing problems despite use of rescue medication). The diary recorded the presence or absence of any morning symptoms. Daytime symptoms were also recorded on a five-point scale ranging from 0 (no symptoms at all) to 4 (symptoms occurred at rest, caused marked discomfort, and usually limited routine activity). The evaluation of daytime symptoms includes an overall assessment of shortness of breath (breathlessness), chest discomfort (tightness), wheezing, and cough. The health state descriptions that were developed were designed to reflect the median and range of symptom burden for each state from patients in the trial. Previous work has demonstrated how the different levels of the GETE reflect tangible and important differences in clinical and quality of life outcomes [13]. The wording from the symptom diary was used in the health states (see “Appendix”).
The health states were designed to be evaluated by the general public so some minor wording changes were required to improve comprehensibility. The health state descriptions are included in the Appendix.
Development of discrete choice experiment
A DCE was developed to determine preferences and WTP for the avoidance of asthma symptoms. DCE methods were used because this approach can be used to estimate the marginal value, in terms of WTP of different aspects of asthma symptoms [20].
The DCE survey presents pairs of hypothetical treatments which vary in terms of different attributes. Four attributes were included which included the three aspects of the symptom diary (nocturnal, morning and daytime asthma symptoms) and an attribute describing out of pocket cost. The cost attribute is included in order to estimate WTP for improvements in attribute levels. Pilot work was designed to assess the acceptability of asking people their maximum WTP for changes in asthma outcomes.
Each attribute was associated with specific levels, and these were derived from the symptom diary. The five levels of the daytime and nocturnal symptoms were reduced to four levels (in order to simplify the underlying design).
Questionnaire design
The attributes and levels are combined into choice sets using a fractional factorial orthogonal design (http://www.research.att.com/~njas/oadir/#3_2) and folded over to ensure zero overlap and orthogonality in differences. This was a main effects-only design and did not include interaction terms. The choice sets were then randomly placed within the questionnaire so as to avoid possible ordering effects and were presented as pairwise choices. Participants were asked to state whether they preferred treatment A or treatment B in line with the conditional demand model. A third alternative (treatment C) was a ‘status quo’ option which described the worst level on each symptom attribute but zero cost. An example question is included below (Fig. 1). The questionnaire contained 16 choices per respondent including a consistency check where one alternative was better or as good as the other choice on all attributes. Choosing the worst choice may indicate that people fail to understand the task or are irrational. Socio-demographic data were also collected.
Pilot study
The health states and DCE survey were piloted with five members of the general public in a cognitive debrief interview. Following these interviews, changes were made which included describing symptom frequency in terms of ‘every few days’, and replacing the word ‘some’ with ‘moderate’. Participants (four out of five) described how they were familiar with asthma. They also indicated that they were happy to consider hypothetical choices which involved paying for improvements in symptoms. Participants reported that they could understand the content of the health states. Following suggestions from participants the health states were reformatted into a larger font size and double line spacing between the bullet points in order to more clearly identify the differences between the health states.
Main study
It was considered important that study participants understood something about the nature of moderate to severe allergic asthma before starting the valuation task. Therefore they were asked to imagine that they had this form of asthma and were given a quite detailed description of the nature of the disease at the start of the study. Participants were asked to consider this information when judging the health states.
Members of the general public were recruited to take part in the utility interviews. Participants were recruited from the Greater London area through newspaper advertisements and through an existing internal database of participants who have completed previous utility studies. Interviews were conducted by trained interviewers at UBC’s London office. All participants first provided written informed consent and then completed a socio-demographic questionnaire, the EQ-5D, and the DCE questionnaire.
The SG interview included two tasks. Health states were first assessed against a VAS anchored by dead and full health. This exercise was primarily used to just familiarise participants with the health states and the concept of valuing states of health. The health states were then assessed again using the SG utility interview [1, 23]. The SG task followed the methodology described by Furlong et al. [5]. All health states were first valued against the prospect of ‘worst health’ (which was logically worse than any of the health states in the study). For each health state (including the patient's own health state), participants were asked to choose one of three options: (1) to live in the hypothetical health state with certainty for 10 years; (2) to choose between various probabilities of having either full health or worst health for the rest of their lives; or (3) to indicate that the two options were equal. High and low probabilities of full health and the worst health state were alternated to avoid anchoring bias [1]. Finally, the worst health state card was assessed based on a gamble between dead and full health. The utility value for the worst state was used to recalibrate the utilities for the other health states on the dead to full health scale.
Statistical analyses
Demographic and other background data were summarised using frequencies and descriptive statistics as appropriate. Standard gamble and VAS data were summarised. Initially the choice data were analyzed with a generalized estimating equations (GEEs) model in SAS, using a binomial distribution and the logit link. It was assumed that there was independence of the data—no allowance was made for any intra-patient correlation between the 16 choices per participant. This was decided on after review of the estimated correlation matrix between the 16 measurements. However, a model allowing for intra-patient correlation using an independence and an exchangeable (or compound symmetry) correlation structure was also estimated in sensitivity analysis. The parameter estimates were very similar to the model obtained with logistic regression. The estimated correlation in the exchangeable correlations structure was very low (0.0274), justifying the assumption on the independence of the data. For the independence structure this correlation is forced to be zero; however this model is not entirely equivalent to the simple logistic regression because the GEE method still accounts for some correlation by operating at the cluster level. In terms of WTP for attribute levels, using the parameter estimates from a GEE model with an independence or an exchangeable correlation structure does not have an impact on the amount participants are willing to pay to avoid certain side effects (the difference was at most 1 pence per month). The WTP values were calculated by taking the marginal rates of substitution between the symptom attributes and the cost attribute. The resulting WTP values for changes in attribute levels were then used to weight the symptom diary data from the INNOVATE trial to estimate welfare shifts between GETE defined health states.
Results
Participant characteristics
The participant demographic data are presented in Table 1. Thirteen participants failed the consistency check in the DCE survey and were not included in any analyses, including health state utility data. The remaining participants (n = 88) represented a relatively close match to the residents of the UK when compared to census and other published data. The sample has a slightly higher proportion of women and ethnic minorities than the UK population. Thirty-nine percent of our sample was employed in full time jobs and 13% were part-time employed, compared to 44% in total according to ONS data.
The self-reported HRQL profile of the study sample was also explored using the EQ-5D five dimension categorisation system (Table 2). The frequency of people reporting moderate or extreme problems was compared to a UK national survey reported by Kind et al. [10]. The distribution of moderate and extreme problems, as recorded by the EQ-5D, is similar to the Kind et al. [10] study.
Health state utility values
Table 3 shows the mean VAS and SG derived utility scores for the asthma health states. A decrement in utility was observed in moving from ‘complete control of asthma’ through to ‘worsening of asthma’. The mean scores for the VAS ranged from 65.2 for ‘complete control of asthma’ to 35.2 for ‘worsening of asthma’. The values for health states were significantly different to each other (F = 47.50, P < 0.0001) and every state was rated significantly different to every other state, apart from the worst two states.
Mean SG utility scores ranged from 0.784 for ‘complete control of asthma’ to 0.711 for ‘worsening of asthma’. In comparison to the 30 point spread on the VAS scores between the best and worst states there is just a 0.07 point spread on SG derived utilities. The health states were not rated significantly differently to each other.
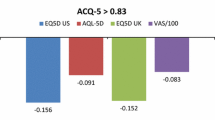
Willingness to pay values
The base case in this analysis—represented by the intercept—is a therapy with no morning symptoms, no nighttime awakenings, and no daytime symptoms. For a treatment which was associated with the absence of symptoms in the morning, during the day and at night participants were willing to pay £160.66 a month. Each parameter estimate represents the “penalty” in the likelihood for choosing a product with that specific level of the attribute. This negative propensity to choose a product with a higher-than-baseline level of morning, night and day symptoms is translated into a negative value on the WTP for that attribute.
The coefficients in the model for the higher levels of each attribute are negative—so they are negative predictors of choice. As a result, patients are willing to pay less for a therapy with a higher level than baseline level of each attribute. Each attribute is also a significant predictor of choice, as indicated by the P-values <0.05.
There is a linear relationship between a participants’ WTP for a therapy and the presence of daytime symptoms: participants are willing to pay more for a therapy with fewer daytime symptoms. There is however a non-linear relationship between participants’ WTP for a therapy and the presence of nighttime symptoms. Participants’ disliked a therapy where they would wake up once but did not need their inhaler more than a therapy where they woke up once but did need their inhaler. The difference in WTP is around £12.
The WTP data from the choice experiment was then used to illustrate the value of achieving different levels of treatment effectiveness as described by the GETE measure. The symptom diary data from week 28 of the INNOVATE trial were weighted by the DCE results to estimate WTP for different GETE endpoints. For example the symptom profile of people who classified themselves as having ‘complete control of asthma’ was determined from the trial data and the WTP data were used to value the level of symptom control. These values or welfare shifts represent a WTP to move from the description of moderate to severe allergic asthma that participants were shown at the start of the survey. Avoidance of all asthma symptoms was valued at £160.66 per month. Tables 4 and 5 show that to achieve ‘complete control of asthma’ participant were willing to pay £105.21 per month. Alternatively ‘worsening of asthma’ was associated with a negative WTP value of −£75.61.
Discussion
This study was designed to capture societal preferences for the avoidance of the symptoms associated with moderate to severe allergic asthma. This severe form of asthma has not been studied extensively in the quality of life or health economic literature. Niebauer et al. (2006) report a meta-analysis of quality of life outcomes from trials of omalizumab. This analysis demonstrated the benefits of omalizumab in terms of a high proportion of patients who reported moderate or large gains on the AQLQ. The improvements were across all domains of the AQLQ. Clinicians have argued that there is a substantial unmet need amongst these patients [16]. However this is one of the first attempts to determine general public preferences on asthma severity and health states. This report has documented three methods of eliciting the value of this disease for society, one using SG and the other using a DCE.
Health states were developed based upon daily symptom diary data from a clinical trial. The patients were stratified according to their response to a global evaluation question—from ‘complete control of asthma’ to ‘worsening of asthma’. The data indicated that even ‘complete control of asthma’ was associated with some symptom burden, which is not surprising in this patient group. The results of the SG interviews indicated that the societal valuations ranged from 0.78 to 0.71. This equates to utility ratings for treatment in breast cancer [3], or Hodgkin’s lymphoma patients receiving chemotherapy [18]. The degree of difference between the five states is relatively small, which perhaps reflects the fact that even patients classified as in the state ‘complete control of asthma’ report some daily symptom burden. The utility values are lower than utility data from the EQ-5D reported from a prospective observational study of HRQL in people with moderate to severe asthma [12]. In this study patients with no exacerbations had a mean health utility of 0.89, whereas those requiring oral steroids for the treatment of an exacerbation had a health utility of 0.57. Previous observational work that we have reported revealed that patients with moderate to severe asthma who were stable on treatment reported a mean health utility of 0.89, whereas patients who experienced an exacerbation had a mean utility of 0.57 [12]. The ratings from the present study fall within this range. The SG and VAS ratings for the health states are quite different, most notably the VAS ratings show a much larger difference between the best and worst health state. This is a pattern we (and others) have found previously, whereby people are more willing to concede space on a VAS than they are willing to trade against risk. In the present study we consider VAS data as a useful check on people’s interpretation of the health states and also a good warm-up task, but we do not believe these data are a good basis for informing cost-effectiveness analyses. The SG data should be considered the primary source of utility data.
It is also worth noting how the SG values were not significantly different from each other (whereas the VAS values were). In this type of study the chance of reaching statistical significance is largely dictated by the sample size and the sample size here is quiet low. However the preference values themselves indicate the level of difference between the states which supersedes the importance of statistical testing. The utilities indicate not only if one state is better than another, but also by how much. The associated confidence intervals indicate the uncertainty around these values.
The WTP data also demonstrate the value that society place on the avoidance of asthma of this severity. For a complete avoidance of all asthma symptoms people were willing to pay £161 per month. The public placed the most value on the avoidance of daytime symptoms, particularly those that restricted activity. Daytime symptoms which lead to activity limitations probably have the greatest effect on a patients’ health-related quality of life and also their ability to work. Participants recognised the burden of waking up more than once in the night with symptoms and needing to use an asthma inhaler. However participants reported a higher WTP to avoid waking up in the night and not requiring an inhaler compared to waking up with symptoms and requiring an inhaler. This doesn’t make intuitive sense. It could be logically assumed that symptoms that require inhaler use are more severe and so more bothersome. This result may be a reflection of the general public sample not fully understanding the nature of inhaler use and its link with the severity of symptoms. This is a potential limitation in these results.
These data however should be considered in the broader context of moderate to severe asthma. The study captures preferences for the symptom burden in moderate to severe asthma which can be considered in addition to the impact of asthma exacerbations. The study allows us to separate out the effects of daily symptoms from exacerbations which could be important for better understanding the burden of asthma. This is particularly relevant when we consider that exacerbation rate is commonly used as a trial endpoint. Therefore the potential value of a treatment can be considered not just in terms of its ability to reduce exacerbations (and possibly mortality) but also in terms of better day-to-day symptom burden. This study helps to fill in the gap in terms of valuing this day-to-day variation. If the avoidance of asthma exacerbations and hospitalisations were included alongside the symptom burden then the societal valuations may increase significantly. In addition to the impact of exacerbations we find that there is a meaningful societal value placed on the impact of daily symptoms and symptom control.
Recent work has examined the value of avoidance of self-managed asthma exacerbations and exacerbations that required emergency care amongst people with asthma [13]. This study elicited preferences and WTP from 479 asthma patients in the UK, the Netherlands and Spain. On average participants were willing to pay €15.74 per month to avoid a self-managed exacerbation and €109.48 (~£75) to avoid an exacerbation that required an emergency visit to their doctor or to the emergency room or hospital. Therefore we could roughly estimate a societal valuation for the avoidance of exacerbations and the burden of daily symptoms to be about £236 per month. This figure is quite high considering that the present data are from a societal sample that is not used to paying market prices for their medication.
There are certain limitations to this study which should be noted. First there was a relatively high proportion of participants who failed the consistency check in the DCE. This is a simple consistency check and a relatively low benchmark. Removing these participants from the dataset deflated the utility and WTP values in general. This suggests that these participants were either not willing to trade or perhaps had dominant preferences. This supports our decision to drop them from all analyses.
The DCE analyses are also limited by the finding that the presence of morning symptoms only approached significance. For the purposes of estimating WTP the attribute was still included because the attribute coefficient was so close to significance. However in a strict interpretation this attribute is not predicting choice and participants were not trading against morning symptoms.
The study sample size was small and further reduced by participants failing the consistency checks. A larger and more representative sample would give us greater confidence that these values can be considered truly societal preferences. A general public sample was chosen so that the data would be more appropriate to use in economic analyses which are intended to guide decision making regarding the allocation of public resources.
The three symptom attributes that were included based on the symptom diary. The methodology and utility function includes the assumption that the attributes are independent. However because of their similarity the three symptom-related attributes may not be independent. We do have trial data to suggest they can vary independently from each other and also different factors such as smoking, exposure to antigens at home or work or different activities undertaken at home or work) can mean that different patterns of asthma emerge. The study was partly designed to understand the relative value in reducing symptoms at different times of the day. On reflection it may be have been better to include interaction terms in the design to better understand the nature of people’s preferences.
It is relatively uncommon in health-related studies to provide detailed background information regarding the disease that the study is designed to elicit preferences on. However this was done here because of the nature of the present study. In many contingent valuation studies in environmental or transport economics it is quite common to provide the participants with some background information as to the nature of the issue you propose to collect WTP values for. Some studies even encourage focus group-type discussion first to allow people to explore their preferences before producing values. In the present context we were eliciting values for a relatively uncommon form of a common disease. We were concerned that people would interpret the information in terms of the much more common milder forms of asthma and so therefore we felt it was important to provide some information regarding how severe allergic asthma can affect people. This study includes the general public rather than patients and so we were concerned that they understood the severity of some of the health states we described.
The use of the health utility data is also limited by the decision to tie the development of health states to the GETE which to date has only been used in selected trials. This was done to stratify patients into overall levels of perceived treatment effectiveness. The five health states reflect a typical range of clinical outcomes in this patient group and could be used as a simple means of patients rating their current health state. The study results may also reveal another potential limitation in the approach. The utility shift between the five levels of the GETE is a relatively modest difference in utility. The overall level of the utility scores in the range of 0.70–0.80 seems consistent with the clinical impression of the severity of this disease. However there is only a small gain from ‘worsening of asthma’ to ‘complete control of asthma’, which may be because health utility includes symptom burden as well as the impact of exacerbations. The present health states really capture the day-to-day symptom burden. Therefore these data may be most suitable for use in a Markov-type model which models patients’ changing utility over time between exacerbations.
It is also possible that the general public does not recognise the full burden of this severe type of asthma. The observational data from the study reported above [12] identified much larger utility shifts related to the presence of an exacerbation (0.89 vs. 0.57). This suggests that the present sample may have under-weighted the differences between the health states. The general public has a much more common experience of more mild forms of asthma and so may have been interpreting the health states in the context of more mild asthma.
In conclusion, this study reports societal utility and preference values for health states describing the symptom burden in moderate to severe allergic asthma. The overall rating for the health states (as indicated by the range of scores) suggests that the general public recognises the overall severity of this form of asthma. However the limited range in utility values between ‘complete control of asthma’ and ‘worsening of asthma’ indicated that the general public did not appreciate the value of control over these symptoms. This is also supported to an extent by the WTP data. Participants were only willing to pay £160 per month for a total absence of asthma symptoms, this despite being given a quite detailed description of how severely affected these patients can be. Societal valuation studies are an important part of resource allocation decisions within publicly funded health care systems. However they are subject to potential bias because many participants have no direct experience of the disease and so may simply interpret health states in terms they are familiar with. Health states which are characterised by severe forms of everyday symptoms such as cough or fatigue may be undervalued because participants fail to appreciate the severity of the symptom.
References
Bennett, K., Torrance, G.: Measuring health state preferences and utilities: rating scale, time trade-off and standard gamble techniques. In: Spilker, B. (eds.) HRQL and Pharmacoeconomics in Clinical Trials, 2nd edn. Lippincott-Raven, Philadelphia, pp. 253–266 (1996)
Busse, W., Corren, J., Quentin Lanier, B., McAlary, M., Fowler-Taylor, A., Della Cioppa, van As A., Gupta, N.: Omalizumab, anti-IgE recombinant humanized monoclonal antibody, for the treatment of severe allergic asthma. J. Allergy Clin. Immunol. 108, 184–190 (2001)
Conner-Spady, B.L., et al.: A longitudinal prospective study of health-related quality of life in breast cancer patients following high-dose chemotherapy with autologous blood stem cell transplantation. Bone Marrow Transplant. 36(3), 251–259 (2005)
Finn, A., Gross, G., van Bavel, J., Lee, T., Windom, H., Everhard, F., Fowler-Taylor, A., Liu, J., Gupta, N.: Omalizumab improves asthma-related quality of life in patients with severe allergic asthma. J. Allergy Clin. Immunol. 111, 278–284 (2003)
Furlong, W., Feeny, D., Torrance, G.W., Barr, R.D., Horsman, J.: Guide to design and development of health-state utility instrumentation. McMaster University CHEPA working paper series (1990)
Global Initiative for Asthma (GINA): Global strategy for asthma management and prevention. NIH Publication 02-3659 issued January 1995 (updated 2002, 2003; accessed 26 Oct 2004). Available at: http://www.ginasthma.com
Gold, M.R., Siegel, J.E., Russell, L.B., Weinstein, MC.: Cost-Effectiveness in Health and Medicine. Oxford University Press (1996)
Greene, W.H., Greene, L.K., Seaks, T.G.: Estimating the functional form of the independent variables in probit models. Appl. Econ. 27, 193–196 (1995)
Humbert, M., Beasley, R., Ayres, J., Slavin, R., Hebert, J., Bousquet, J., Beech, K-M., Ramos, S., Canonica, G.W., Hedgecock, S., Fox, H., Blogg, M., Surrey, K.: Benefits of omalizumab as add-on therapy in patients with severe persistent asthma who are inadequately controlled despite best available therapy (GINA 2002 step 4 treatment): INNOVATE. Asthma 10, 1398 (2004)
Kind, P., Dolan, P., Gudex, C., Williams, A.: Variations in population health status: results from a United Kingdom national questionnaire survey. Br. Med. J. 316, 736–741 (1998)
Lloyd, A.J., McIntosh, E., Rabe, K., Williams, A.E.: Patient preferences for asthma therapy: a discrete choice experiment. Prim. Care Respir. J. (in press)
Lloyd, A.J., Price, D., Brown, R.: The impact of asthma exacerbations on health-related quality of life in moderate to severe asthma patients in the UK. Prim. Care Respir. J. 16, 22–27 (2007)
Lloyd, A., Turk, F., Leighton, T., Canonica, G.W.: Psychometric evaluation of global evaluation of treatment effectiveness: a tool to assess patients with moderate-to-severe allergic asthma. J. Med. Econ. 10(3), 285–296 (2007)
Louviere, J., Hensher, D., Swait, J.: Conjoint preference elicitation methods in the broader context of Random Utility Theory preference eliciation methods. In: Gustafson, A., Hermann, A., Huber, F. (eds.) Conjoint Measurement: Methods and Applications. Springer, Berlin, pp. 305–344 (2001)
Manski, C.F.: The structure of random utility models. Theory Decis. 8(229), 254 (1977)
Marshall. G.D. Jr, Sorkness, C.A.: IgE-blocking therapy for difficult-to-treat asthma: a brief review. Manag. Care 13(3), 45–50 (2004)
McFadden, E.R. Jr: Acute severe asthma. Am. J. Respir. Crit. Care Med. 168(7), 740–759 (2003)
Norum, J., et al.: Treatment costs in Hodgkin’s disease: a cost-utility analysis. Eur. J. Cancer 32A(9), 1510–1517 (1996)
Office of National Statistics, National Statistics website “Population of the United Kingdom: by ethnic group, April 2001”. http://www.statistics.gov.uk/cci/nugget_print.asp?ID=764
Osman, L.M., McKenzie, L., Cairns, J., Friend, J.A.R., Godden, D.J., Legge, J.S., Douglas, J.G.: Patient weighting of importance of asthma symptoms. Thorax 56, 138–142 (2001)
Roe, B., Boyle, K.J., Teisl, M.F.: Using conjoint analysis to derive estimates of compensating variation. J. Environ. Econ. Manage. 31, 145–159 (1996)
Solèr, M., Matz, J., Townley, R., Buhl, R., O’Brien J., Fox, H., Thirlwell, J., Gupta, N.,Della Cioppa, G.: The anti-IgE antibody omalizumab reduces exacerbations and steroid requirement in allergic asthmatics. Eur. Respir. J. 18, 254–261 (2001)
Torrance, G.W.: Measurement of health state utilities for economic appraisal. J. Health Econ. 5(1), 1–30 (1986)
Torrance, G.W.: Preferences for health states: a review of measurement methods. Clin. Econ. Eval. Perinat. Dev. Med. 20, 37–45 (1982)
Torrance, G.W.: Utility approach to measuring health-related quality of life. J. Chronic Dis. 40(6), 593–600 (1987)
Acknowledgments
The authors would like to acknowledge the assistance of Bernadette Khoshaba who helped to develop the health states and interviewed some study participants. The study was funded by Novartis AG.
Author information
Authors and Affiliations
Corresponding author
Appendices
Appendix 1
Complete control of asthma
Marked improvement of asthma
Discernible, but limited improvement in asthma
No appreciable change in asthma
Worsening of asthma
Appendix 2: attributes and levels from DCE
Morning asthma symptoms
-
Each morning when you wake up you did not have any asthma symptoms (such as chest tightness, wheezing or cough).
-
Each morning when you wake up you have asthma symptoms (such as chest tightness, wheezing or cough).
Nighttime breathing problems
You may experience breathing problems at night. These normally include chest discomfort (tightness), wheezing, and cough, and possibly shortness of breath.
-
You did not wake up because of any breathing problems.
-
You wake up once a night because of breathing problems but did not need to use your inhaler.
-
You wake up once because of breathing problems, but you used your inhaler to control the symptoms.
-
You awoke more than once because of breathing problems, but you used your inhaler to control the symptoms.
Daytime asthma symptoms
You may experience asthma symptoms during the day. These include—shortness of breath (breathlessness), chest discomfort (tightness), wheezing, and cough.
-
You have no symptoms at all; unrestricted activity.
-
You have some symptoms which caused little or no discomfort; unrestricted activity.
-
You have symptoms which cause some discomfort, at times limiting strenuous activity.
-
You have symptoms which cause moderate discomfort and sometimes limited routine activity.
Cost
You would have to pay for your new asthma medication out of you pocket. Think about whether you could afford the price and whether you would be willing to pay.
-
Cost is £20 per month
-
Cost is £40 per month
-
Cost is £60 per month
-
Cost is £80 per month
Rights and permissions
About this article
Cite this article
Lloyd, A., Doyle, S., Dewilde, S. et al. Preferences and utilities for the symptoms of moderate to severe allergic asthma. Eur J Health Econ 9, 275–284 (2008). https://doi.org/10.1007/s10198-007-0075-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-007-0075-0