Abstract
Deep-vein thrombosis and pulmonary embolism are important causes of morbidity and mortality among patients undergoing major surgery. Fondaparinux is a new antithrombotic agent for use in prophylaxis, and this study compared its cost and effect vs. enoxaparin as prophylactic treatment in patients undergoing total knee replacement, total hip replacement, or hip-fracture surgery in Sweden. The analyses were based on a simulation model. Swedish data on cost for deep-vein thrombosis and pulmonary embolism were obtained from a large sample of patients undergoing major orthopedic surgery. The relative risk reduction for treatment with fondaparinux was estimated from results of four recently published clinical trials. The base case analyses showed that fondaparinux was cost saving and more effective than enoxaparin after total knee replacement and hip-fracture surgery and had costs per prevented venous thromboembolism of about €239 after total hip replacement. Fondaparinux is thus more cost-effective than enoxaparin as prophylactic treatment in patients undergoing major surgery in Sweden.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Deep-vein thrombosis (DVT) and pulmonary embolism (PE) are important causes of morbidity, mortality, and costs. DVT can cause local symptoms such as acute pain and swelling and may lead to recurrences and postthrombotic syndrome. DVT is also the source of over 90% of cases of PE [1]. PE may cause symptoms such as acute dyspnea, chest pain, cough, and in some cases death.
There are several diagnostic methods for identifying DVT and PE. Ultrasound, phlebography, and spiral-computed tomography are the three most commonly used methods in Sweden today [2]. The total incidence of venous thromboembolism (VTE), i.e., DVT or PE, in Western countries has been estimated at about 1.5–2 cases per 1,000 persons and year, but the estimate is uncertain since many VTE probably are undetected [3]. The risk of these events increases with age and patients undergoing major surgery have a particularly high risk of developing VTE [2, 4, 5, 6].
Total hip replacement (THR), total knee replacement (TKR), and hip fracture surgery (HFS) entail a high risk of causing postoperative VTE. About 30,000 patients undergo these operations every year in Sweden [7, 8]. The number of orthopedic operations in Sweden is increasing, mainly due to the increasing age of the population but also because the upper age limit for surgery has increased. The average age of a hip fracture patient in Sweden today is about 80 years, and about 70% of the patients are women [7]. The hospitalization time for hip fracture patients in Sweden has decreased in recent decades. The average hospitalization time at the end of the 1980s was about 19 days and today is about 10 days. Patients having hip and knee replacements are on average 10–15 years younger than hip fracture patients [9].
The incidence of VTE after surgery varies substantially, depending on the patient population and the type of surgery performed. VTE can develop during the hospitalization (early VTE) or after discharge from hospital (late VTE). Detection of VTE can be based on a diagnostic method (venographic VTE) or on clinical symptoms (clinical VTE). Venographic VTE can stay asymptomatic without leading to any clinical symptoms. The relationship between venographic and clinical VTE is not yet clear. The incidence of venographic thrombosis without prophylaxis has been estimated at about 50–60% after TKR, about 45–50% after THR, and about 40–60% after HFS [2]. There are, however, effective prophylactic treatments available and the incidence of thrombosis after prophylaxis is considerable lower. Colwell et al. [10] found the incidence of clinical VTE after THR to be 3.6% and 3.7% after enoxaparin and warfarin prophylaxis. Le Clerc et al. [11] found the incidence of clinical VTE after enoxaparin to be 3.9% and 4.3% after TKR and THR, respectively. Data on incidence of VTE after surgery in Sweden is limited. One study of THR surgery found the 1-month postoperatively incidences of clinical DVT to be 6.9% and the incidences of clinical PE 1.7% in patients receiving enoxaparin as prophylaxis [12].
The acute cost of VTE is due mainly to treatment and hospitalization, but there is also risk of substantial long-term costs. A Swedish study estimated the average cost of treating long-term complications of thrombosis to about $4,700 in patients with a history of deep venous thrombosis compared to about $400 in patients without thrombosis [4].
The most common prophylactic drugs used in Sweden today are the low molecular weight heparins [2]. Enoxaparin is one of the most commonly used low molecular weight heparins, and several studies have analyzed the effect and cost-effectiveness of enoxaparin. Studies have found enoxaparin to be cost-effective compared to unfractionated heparin and warfarin in prophylaxis after orthopedic surgery [13, 14, 15, 16]. A Swedish study found prolonged prophylaxis with enoxaparin after THR to be less expensive than in-hospital prophylaxis only [12]. Pure thrombin inhibitors and pure Xa inhibitors belong to a new generation of antithrombotic drugs. These drugs have a more specific inactivation effect which is believed to result in an effective inhibition of thrombin generation. Fondaparinux is one such new drug for use as prophylaxis against venous thromboembolism. Clinical trials have found fondaparinux to yield a 54% risk reduction in venographic DVT by day 11 after elective major knee surgery and HFS compared to enoxaparin [2, 17, 18, 19], although no statistical difference in symptomatic VTEs was found [20]. Symptomatic VTE, however, was not the primary endpoint in the clinical trials.
This study compared the cost-effectiveness of fondaparinux and enoxaparin as prophylaxis after major orthopedic surgery in Sweden. Enoxaparin was chosen as comparator since it is one of the most commonly used prophylaxis in Sweden today, and since clinical trials have compared fondaparinux and enoxaparin prophylaxis [21]. We used a model to estimate the cost and consequences of thrombosis prophylaxis as modeling provides a convenient way to incorporate the different sources of information into an economic evaluation. Models can also be used to simulate consequences beyond the observation times in a clinical trial, which is necessary in this study since thrombosis prophylaxis can have long-term consequences that are not captured within the clinical trial of fondaparinux.
Knowledge about cost-effectiveness of new drugs is important for rational choices between different therapies. Fondaparinux is a new drug and it is important to have information about the cost-effectiveness as basis for decisions about pricing, reimbursement, and use of this drug.
Methods
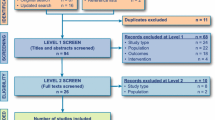
The analyses were performed using a decision model previously used to analyze the cost effectiveness of fondaparinux in the United Kingdom and the United States [22, 23, 24] (S. Sullivan, submitted). The model simulates a cohort of patients undergoing THR, TKR, or HFS over a period of 5 years. Cohorts of 10,000 patients receiving either enoxaparin or fondaparinux as prophylaxis were simulated. The model estimated costs, clinical DVTs and PEs, and VTE-related deaths. A discount rate of 3% was used as base case in the analyses.
Model structure
Patients in the model may develop a thrombosis during hospitalization that can be clinically apparent or silent. Detection of clinical DVT or PE is based on symptomatic presentation which is subsequently confirmed. The model also accounts for patients incorrectly suspected of having a DVT or PE. Patients with confirmed clinical VTE receive treatment and remain at risk of long-term complications (recurrent VTE or postthrombotic syndrome, PTS). Patients with undetected and untreated venographic DVT are also assumed to be at risk of PTS. PE can develop from either clinical and venographic DVT. Patients are also at risk of having bleeding complications. Patients with PE or bleeding complications have increased mortality.
The model is dived into two phases: an acute phase, from surgery to 3 months postsurgery, and a chronic phase, from 3 months to 5 years after the surgical procedure. Patients may develop early clinical or venographic thrombi during the period of hospitalization or late clinical or venographic thrombi between hospital discharge and day 30.
Event probabilities
The main probabilities were derived from four randomized trials comparing fondaparinux and enoxaparin following THR, TKR, and HFS, supplemented by data from the literature [2, 17, 18, 19]. Table 1 shows the probabilities used in the model.
The prevalence of venographic DVT in the fondaparinux clinical trial was used to estimate the risk of early venographic DVT in the model [17, 18, 19]. The risk of late venographic DVT (between discharge and day 30) was estimated from a study of THR patients with negative findings on a venogram at hospital discharge [25]. The risk of late venographic DVT following TKR was estimated at 65% of that following THR, based on a large cohort study [26].
The model assumes a direct relationship between venographic and clinical VTE, i.e., patients with venopgraphic VTE have a probability of developing clinical VTE. The probabilities of developing clinical DVT or PE following early and late venographic DVT were estimated from cohort studies and randomized trials of patients undergoing total hip or knee replacement [10, 27, 28]. No similar data existed for HFS, but the probability of clinical VTE is expected to be higher following HFS than following THR because of age, comorbidities, and traumatic injuries [2, 17, 18, 19, 20, 29]. Using evidence of venographic proximal DVT rates seen in both recent studies and the fondaparinux trials the probability of clinical VTE following HFS was estimated at 70% greater than that following hip replacement [2, 18, 19, 30, 31]. This estimate was consistent with the clinical VTE rates seen between HFS and THR in the Pulmonary Embolism Prevention study [32]. Fondaparinux was estimated at reduce the risk of early venographic DVT by 54% compared to enoxaparin [2, 17, 18, 19, 20, 21]. Since a direct relationship between venographic VTE and clinical VTE was assumed, this also meant that the risk of clinical VTE was reduced by 54% in the model.
The risk of recurrent VTE was estimated from a long-term follow-up study [33]. The risk of PTS following clinical DVT was estimated from a long-term prospective cohort study [34]. Risks of PTS following venographic DVT were derived from two retrospective studies [35, 36]. The same risks of suspected but unconfirmed DVT and PE were assumed for both prophylaxes [1]. The probabilities of prophylaxis-related major bleeding were estimated from pooled rates observed in the clinical trials of fondaparinux [2, 17, 18, 19, 20, 21]. The probability of bleeding related to treatment of clinical DVT or PE was calculated from pooled data observed in studies in which patients were treated with therapeutic heparin and warfarin for at least 3 months [37, 38, 39, 40, 41].
The mortality risk for patients undergoing THR or TKR who develop PE was estimated from four different studies [10, 28, 42, 43]. Results from the fondaparinux clinical trial were used to estimate mortality after HFS [18]. The mortality from bleeding events was derived from the fondaparinux studies. Probabilities of deaths unrelated to VTE were estimated from Swedish life tables [44].
Model validation
The model used in the analyses was based on various international studies of thrombotic diseases. The incidence of clinical VTE in the model for patients treated with enoxaparin was about 3.9% after TKR and THR and about 6.4% after HFS. It is important to validate these assumptions to determine whether they are applicable to Swedish settings. The incidence of clinical VTE in our sample from the inpatient care statistics was about 1.4%, which is lower than the model assumptions. Missing diagnosis reporting and outpatient treatment are believed to be the major sources of this discrepancy. The inpatients sample can thus not be used as a reliable estimate of the incidence in Sweden. Other studies of incidence of VTE in Sweden must be used. There are, however, very few studies available estimating the incidence of VTE after prophylaxis with low molecular weight heparins in Sweden. One study of THR surgery compared in-hospital enoxaparin prophylaxis with prolonged enoxaparin prophylaxis. The study found the 1-month postoperatively incidences of clinical DVT to be 6.9% and the incidences of clinical PE to 1.7%, in the normal prophylaxis group [12]. The study found the incidence of venographic DVT to be 39% in the normal prophylaxis group [45]. Another study of hip replacement surgery performed at 11 centers in Scandinavia found incidences of venographic DVT of 7% and 23% in patients receiving prophylaxis with either desirudin or unfractionated heparin [46]. Eriksson et al. [47] compared hirudin and enoxaparin in patients undergoing hip replacements in 10 European countries and found overall incidences of venographic DVT to be 18% and 26%. It is difficult to find reliable Swedish estimates to be able to assess the validity of the model assumptions in Sweden. The few studies found, however, agreed fairly well with the assumptions in the model.
Inpatient care statistics
All costs in the model were estimated in a Swedish context. The cost estimations were mainly based on information from the national inpatient care statistics in Sweden and from the literature. The inpatient care statistics is a national register of all hospitalization episodes [8]. Patient characteristics and information of the cause of the hospitalization (e.g., diagnoses, surgical procedures) can be found in the statistics. There is a slight lag time for hospitalization episodes to be included in the statistics, and information after year 2000 could therefore not be used.
The information from the national inpatient care statistics was collected for the years 1998–2000. A sample of patients undergoing TKR, THR, or HFS was identified in the statistics by operation codes NGBxx (TKR), NFBxx (THR), and NFJxx (HFS of the femoral neck, pentrochanteric or subtrochanteric). Patients from the sample also having a secondary diagnosis for PE, DVT or major bleedings were identified by International Disease Classification (ICD-10) codes (I80, I26, T81.0, I60, I61, I62, R04, R58, K62.5 and K92.2). All patients in the sample who were readmitted to a hospital within 3 months with a diagnosis of PE or DVT were identified. Between 1998 and 2000 there were totally 96,110 admissions due to TKR, THR, or HFS. Of these were 17,208 due to TKR, 36,492 to THR, and 42,410 to HFS. The average ages of the patients identified in the sample were 70 years for TKR, 72 years for THR, and 83 years for HFS. There were 224 cases of PE, 315 cases of DVT, and 586 cases of bleeding among the 96,110 admissions in the sample.
A regression model was constructed to predict the length of stay in hospital. The distribution of length of stays was found to be heavily skewed. A log-linear model was found to be the most suitable, although some heteroscedasticity was present. The presence of PE, DVT, or bleeding was analyzed as explanatory dummy variables in the model. The model also included age and sex of the patients as explanatory variables.
Costs
The regression analyses presented above were the basis of the cost calculations. All unit costs are summarized in Table 2. All costs were converted to 2002 price level, using the Swedish consumer price index. All cost are presented in euros, using a rate of 9.1 Swedish crowns to €1.
Cost of prophylaxis
The cost of 7 days enoxaparin (40 mg per day) was estimated at €25.2 [48] and the cost of 7 days fondaparinux (2.5 mg per day) estimated at €76.9.
Cost of clinical VTE treatment in hospital
The cost of treating DVT and PE in hospital was calculated from the additional hospital days in the regression analysis. The cost of one additional day in hospital was estimated at €507, based on the cost of a hospital day at a surgical ward at middle-sized hospitals in Sweden [49]. Costs of standard treatments and diagnostic tests of DVT and PE were added.
Cost of clinical VTE treatment after discharge
The total incidence of DVT after discharge in our sample was about 0.5%, while the estimated incidence of DVT after discharge in the model was about 2.5%. Some of this difference was believed to be due to missing diagnoses in the inpatient care statistics and some to the fact that many patients having a DVT after discharge are treated as outpatients. No information of the distribution of outpatients and in-hospital patients was available, but we estimated in a base case that 33% were treated in-hospital and 66% were treated as outpatients. The assumptions were based on the incidence in our sample compared to the estimated incidence in the model after adjustment for some lost cases due to missing diagnoses. We also test two additional cases in which 66% and 20% were treated in-hospital.
The total incidence of PE after discharge in our sample was about 0.3% while the estimated incidence of PE after discharge was about 0.9%. As for DVT, some of this difference was believed to be due to missing diagnoses. However, since PE is a more severe diagnosis than DVT, we estimated that all patients having a PE were treated as in-hospital patients.
Cost of in-hospital treatment of DVT and PE after discharge was calculated from average length of stay for patients readmitted with a diagnosis of DVT or PE within 90 days after discharge, with addition of costs of standard treatments and diagnostic tests. The cost of one additional day in hospital was estimated at €340, based on the cost of a hospital day at a medicine ward at middle-sized hospitals in Sweden [49]. Outpatient treatment of DVT and PE was expected to be the same as for DVT in hospital, except for additional costs for administration of enoxaparin during outpatient care and for two outpatient visits to a physician. These estimates were based partly on a previous Swedish study [12, 50].
Suspected VTE
A suspected but unconfirmed DVT was assumed to lead to one physician visit and one ultrasound/duplex Doppler or phlebography investigation [2, 30]. A suspected but unconfirmed PE was estimated at lead to one physician visit and one diagnostic spiral computed tomography [2, 30].
Bleeding adverse events
The additional length of stay for patients undergoing TKR, THR, and HFS and also having a secondary diagnosis of bleeding was calculated from the regression analysis. The average additional length of stay was estimated at 1.1 days. The cost of one additional day in hospital was estimated at the cost of a hospital day at a surgical ward at middle-sized hospitals in Sweden. Cost of bleeding caused by treatment of DVT or PE was based on diagnosis-related group number 175, with a mean cost of €1,464.
Postthrombotic syndrome
The cost of post thrombotic syndrome is based on a Swedish study of cost of long-term complication of DVT [4]. The cost of acute post thrombotic syndrome (first quarter) was estimated at €1,047 and the cost of chronic PTS at €156 per quarter.
Results
Table 3 shows the result from the regression analyses of the length of stay in hospital. Since the model is a log-linear model, the coefficients show the relative effect on additional hospital days. The coefficients in the table were therefore converted to show the absolute effect of the explanatory variables on additional days in hospital. This means that the calculated additional days in hospital only corresponds to the additional hospital days of a specified patient, which in this case were average patients at the same ages as the average ages in the simulated cohorts, i.e., 65 years for TKR and THR and 80 years for HFS.
The regression analyses were also carried out separately for the three different types of surgery. All variables except bleeding were found highly significant in the separate regressions. The bleeding variable, however, was significant when all types of surgery were run together. The effect of bleeding on length of stay for the three types of surgery was therefore analyzed as a group. Table 4 shows the results from the regression models.
The length of stays for patients readmitted with a diagnosis of PE or DVT were analyzed separately; 317 patients were readmitted due to PE and 488 patients were readmitted due to DVT. The average length of stay in hospital for these patients was calculated for the three types of surgery. The average length of stay was 3.8, 4.4, and 5.6 days after a DVT for TKR, THR, and HFS, and 7.6, 7.3 and 10.9 days after a PE for TKR, THR, and HFS.
The results from the base case simulations, presented in Table 5, show that the cost difference between fondaparinux and enoxaparin varies with the type of surgery. Fondaparinux had higher cost than enoxaparin after THR at 5 years follow-up but lower cost after TKR and HFS. Fondaparinux was found to avoid between 87 and 135 clinical DVTs and between 51 and 86 clinical PEs per cohort of 10,000 patients. The cost per clinical VTE event (i.e., DVT or PE) prevented was €239 after THR. During the inpatient care period, fondaparinux had additional costs of €28.0 and €43.4 per patient after TKR and THR, but lower costs after HFS.
Fondaparinux reduced the risk of VTE, and since these events are associated with increased mortality, fondaparinux also had a lower predicted mortality rate. Fondaparinux prevented between 8 and 61 deaths per 10,000 treated patients.
Sensitivity analyses
The additional length of stay in hospital for a DVT after HFS was estimated at 15 days, using the regression model presented above. This additional hospitalization time for DVT after HFS was much longer than after the other types of surgery and also longer than for a PE after HFS. We therefore used another estimate of this additional hospitalization days to test the effect on the results. We used the average hospitalization time for the DRG group related to DVT, which was 5.4 days. The new total costs of confirm/treat DVT in hospital after HFS was estimated at €3,202. Fondaparinux was still found to be cost saving after HFS.
Sensitivity analyses were made with new discount rates of 0% and 5%, with new estimates of the proportion of DVT patients treated in-hospital of 66% and 20% and with new relative risks of prophylaxis-related bleeding of 0% and 15%. These analyses affected only the cost outcomes, and the results were found stable. The discount rate had only minor effects, which was not surprising since the maximum follow-up time was only 5 years.
Additional sensitivity analyses were made where the risks of early and late DVT was changed. In the first analyses the 95% confidence interval of the risk reduction in early DVT for fondaparinux from the clinical trials was analyzed, and in the second analysis the risk difference in late DVT between enoxaparin and fondaparinux was set to +50% and −50%. The effects of using the new calculated cost of confirm/treat DVT in hospital after HFS was tested in two-way sensitivity analyses. Selected results from sensitivity analyses are presented in Table 6. The results were fairly insensitive to the different assumptions.
If the reduction in venographic VTE cannot be directly translated into the same relative reduction in clinical VTE, the efficacy of fondaparinux in reducing clinical VTE may be lower than assumed. We made a sensitivity analysis where only 50% of the base case fondaparinux efficacy was assumed to determine how a large reduction in efficacy would affect the results. Fondaparinux was still cost-saving after HFS, while the cost per VTE prevented after THR was about €4,000.
Discussion
The clinical trials of fondaparinux estimated the risk reduction in venographic DVT, which in the model was translated into risk reduction in clinical DVT and PE. One of the clinical studies comparing fondaparinux and enoxaparin did not find a statistically significant difference in efficacy. However, a pooled analysis of the clinical trials for patients treated with the recommended dose regimen of fondaparinux vs. enoxaparin showed a significant difference in incidence of venographic VTE [20]. The relationship between venographic DVT and clinical DVT and PE has been questioned, although studies have demonstrated a link between venographic DVT and clinical events [1, 51, 52, 53, 54, 55]. The exact nature of the relationship between venographic and clinical VTE is not clear, however. A meta-analysis of the clinical trials of fondaparinux, for example, showed no significant difference in symptomatic VTE.
The sample taken from the national inpatient care statistics included 96,110 admissions but contained only few cases of PE, DVT, and bleeding. The calculation of additional hospitalization time is surrounded with some uncertainty particularly since there were fewer events in the sample than expected. The reasons for the few cases of PE, DVT, and bleeding are unclear, but one might be missing diagnosis reporting. Many patients are also treated as outpatients, which might explain the low incidence of postdischarge DVT in our sample. The number of additional hospital days for patients with DVT after HFS was much larger than after the other types of operation, which did not seem logical. The reason is unclear but could partly be a result of the low incidence of DVT in our sample. Another explanation could be that hip fracture patients are elderly, and some elderly patients with complications are transferred from hospital to medical care at other institution, for example, nursing home. It is sometimes difficult, however, to find places for patients at these institutions, and some patients may therefore stay hospitalized while waiting to be transferred to another institution. Normally it is expected that PE is a more complicated diagnosis than DVT and therefore has longer treatment time. This was the case for the first two types of surgery and can also be seen in the average DRG hospitalization times, but was not seen after the HFS in our sample.
The base case analyses showed that fondaparinux was cost saving and more effective than enoxaparin in two surgery cases and had costs per prevented clinical VTE event of about €239 in the third. The sensitivity analyses showed that the results were stable. The result for the HFS case was a bit more uncertain than the other two cases due to the somewhat uncertain hospitalization time for patients with DVT after hip fracture. However, the analyses of HFS showed that fondaparinux was both cost saving and more effective than enoxaparin and the result was stable also when the additional hospital days after DVT were reduced to about one-third of the estimate based on the data from the inpatient care statistics sample. The sensitivity analyses included efficacy estimates corresponding to the 95% confidence interval from the clinical trial of fondaparinux. However, this, represents only the uncertainty around the efficacy of fondaparinux in reducing venographic VTE and does not reflect the uncertainty around the relationship between venographic and clinical VTE. As noted above, the model is based on the assumption that a reduction in venographic VTE leads to the same relative reduction in clinical VTE. Since this relationship still is uncertain, the findings in this study may be seen as potential cost-effectiveness of fondaparinux, provided that the relationship between venographic and clinical VTE can be established.
Fondaparinux was found to be associated with a higher risk of bleeding complications than enoxaparin. Bleeding may cause severe consequences, and subanalyses of patients with different risk of bleeding may therefore affect results, although the variations in risk of bleeding made in the sensitivity analyze did not affect the cost-effectiveness considerably. The risk of bleeding is also assumed to be related to the timing of prophylaxis, and different starting time for prophylaxis may therefore affect the cost-effectiveness [53].
The price of fondaparinux was €11 per day, based on an estimate of the expected retail price of fondaparinux in Sweden. The sensitivity analyses showed that a 20% higher fondaparinux price increased the cost per VTE prevented to about €1,354 after THR while fondaparinux was still more cost-effective than enoxaparin after the other two types of surgery.
Unit costs for a stay in a middle-sizes hospital were based on average costs for 28 county and community hospitals in Sweden. The costs for diagnostic procedures were taken from the University Hospital in Lund. Only this hospital was used since estimates were not available from all hospitals in Sweden. The costs, however, are believed to be valid since the variation in these costs between hospitals in Sweden is small [44].
The model simulated a patient cohort over a period of 5 years. Modeling the consequences of prophylaxis beyond the initial hospitalization was considered necessary to capture the effects of long-term complications of VTE. The 5-year follow-up time was considered long enough to capture the relevant VTE-related consequences. The clinical trials of fondaparinux followed patients up only to 49 days, and extrapolation of results from the clinical trials were therefore necessary. Extrapolation of intermediate surrogate outcomes to final endpoints, however, introduces uncertainties into the model. Data on utility or long-term mortality was not available, and the number of life-years and quality-adjusted life-years gained was therefore not estimated. The cost per VTE prevented is a cost effectiveness ratio directly related to thrombotic diseases and cannot be used to compare the cost effectiveness of fondaparinux with treatments in other therapeutic areas. Other outcome measures, for example, life-years saved and quality-adjusted life-years, must be used to be able to make such comparisons. The results showed that fondaparinux could prevent between 8 and 61 more deaths per 10,000 treated patients than enoxaparin.
This study was based on a simulation model using clinical data taken from international studies carried out in different countries, in combination with Swedish cost data. It is therefore important to validate whether the clinical data and the assumptions in the model are relevant to Swedish practice. This is one important potential source of bias that may occur in studies such as this one, where different data sources are used. It was difficult, however, to validate the clinical assumptions in this model since only very few studies have been performed on Swedish patients. The few Swedish studies found agreed fairly well with the assumption used in the model.
Transferability of economic evaluations between different countries is an important and complicated issue. Country specific information is in most cases not available for new drugs, at least not in small countries such as Sweden, since clinical trials of new drugs often are multinational. Data must therefore be imported from studies performed in other countries. The validity of this imported data and the applicability of the results are therefore important issues to assess, but decisions must be made even with less than perfect data. However, real-world data from epidemiological and long-term follow-up studies are necessary to validate results from models such as the one used in this study.
References
Oster G, Tuden RL, Colditz GA (1987) A cost-effectiveness analysis of prophylaxis against deep-vein thrombosis in major orthopedic surgery. JAMA 257:203–208
Turpie AG, Bauer KA, Eriksson BI, Lassen MR (2002) Postoperative fondaparinux versus postoperative enoxaparin for prevention of venous thromboembolism after elective hip-replacement surgery: a randomised double-blind trial. Lancet 359:1721–1726
Norgren L, Rosfors S, Ivancev K, Plate G, Johnsson H (2000) [Deep venous thrombosis-news on diagnostics and treatment]. Lakartidningen 97:1411–1412
Bergqvist D, Jendteg S, Johansen L, Persson U, Odegaard K (1997) Cost of long-term complications of deep venous thrombosis of the lower extremities: an analysis of a defined patient population in Sweden. Ann Intern Med 126:454–457
Clagett GP, Anderson FA Jr, Heit J, Levine MN, Wheeler HB (1995) Prevention of venous thromboembolism. Chest 108:312S–34S
Haake DA, Berkman SA (1989) Venous thromboembolic disease after hip surgery. Risk factors, prophylaxis, and diagnosis. Clin Orthop 242:212–231
National Board of Health and Welfare (2002) Medicinsk faktadatabas (in Swedish) Socialstyrelsen: Stockholm
National Board of Health and Welfare (2002) National inpatient care statistics. Socialstyrelsen: Stockholm
Anonymous (2001) Årsrapport Svenska knäplastikregistret (in Swedish)
Colwell CW Jr, Collis DK, Paulson R, McCutchen JW, Bigler GT, Lutz S, et al (1999) Comparison of enoxaparin and warfarin for the prevention of venous thromboembolic disease after total hip arthroplasty. Evaluation during hospitalization and three months after discharge. J Bone Joint Surg Am 81:932–940
Leclerc JR, Gent M, Hirsh J, Geerts WH, Ginsberg JS (1998) The incidence of symptomatic venous thromboembolism after enoxaparin prophylaxis in lower extremity arthroplasty: a cohort study of 1:984 patients. Canadian Collaborative Group. Chest 114:115S–118S
Bergqvist D, Jonsson B (2000) Cost-effectiveness of prolonged out-of-hospital prophylaxis with low-molecular-weight heparin following total hip replacement. Haemostasis 30:130–135
Balen RM, Marra CA, Zed PJ, Cohen M, Frighetto L (1999) Cost-effectiveness analysis of enoxaparin versus unfractionated heparin for acute coronary syndromes. A Canadian hospital perspective. Pharmacoeconomics 16:533–542
Bergqvist D (2002) Enoxaparin: a pharmacoeconomic review of its use in the prevention and treatment of venous thromboembolism and in acute coronary syndromes. Pharmacoeconomics 20:225–243
Menzin J, Colditz GA, Regan MM, Richner RE, Oster G (1995) Cost-effectiveness of enoxaparin vs low-dose warfarin in the prevention of deep-vein thrombosis after total hip replacement surgery. Arch Intern Med 155:757–764
Saunders ME, Grant RE (1998) Cost effectiveness of low-molecular weight heparin versus warfarin following hip replacement surgery. J Natl Med Assoc 90:677–680
Bauer KA, Eriksson BI, Lassen MR, Turpie AG (2001) Fondaparinux compared with enoxaparin for the prevention of venous thromboembolism after elective major knee surgery. N Engl J Med 345:1305–1310
Eriksson BI, Bauer KA, Lassen MR, Turpie AG (2001) Fondaparinux compared with enoxaparin for the prevention of venous thromboembolism after hip-fracture surgery. N Engl J Med 345:1298–1304
Lassen MR, Bauer KA, Eriksson BI, Turpie AG (2002) Postoperative fondaparinux versus preoperative enoxaparin for prevention of venous thromboembolism in elective hip-replacement surgery: a randomised double-blind comparison. Lancet 359:1715–1720
Turpie AG, Bauer KA, Eriksson BI, Lassen MR (2002) Fondaparinux vs enoxaparin for the prevention of venous thromboembolism in major orthopedic surgery: a meta-analysis of 4 randomized double-blind studies. Arch Intern Med 162:1833–1840
National Corporation of Swedish Pharmacies (1999) Sale statistics. Apoteket AB: Stockholm
Outcomes and costs of prophylaxis against venous thromboembolism in patients undergoing major orthopedic surgery. Final technical report (2001) Policy Analysis Inc (PAI): Massachusetts
Gordois A, Posnett J, Borris L, Bossuyt P, Jönssson B, Levy E, et al (2002) The cost-effectiveness of fondaparinux compared to enoxaparin as prophylaxis against venous thromboembolism following major orthopaedic surgery (abstract). Value Health 5:444
Sullivan S, Kahn S, Davidson B, L. B, Bossuyt P, Raskob G (2002) Measuring the outcomes and economic consequences of venous thromboembolism prophylaxis in major orthopedic surgery. Pharmacoeconomics (in press)
Planes A, Vochelle N, Darmon JY, Fagola M, Bellaud M, Huet Y (1996) Risk of deep-venous thrombosis after hospital discharge in patients having undergone total hip replacement: double-blind randomised comparison of enoxaparin versus placebo. Lancet 348:224–228
White RH, Romano PS, Zhou H, Rodrigo J, Bargar W (1998) Incidence and time course of thromboembolic outcomes following total hip or knee arthroplasty. Arch Intern Med 158:1525–1531
Hull R, Raskob G, Pineo G (1993) A comparison of subcutaneous low-molecular-weight heparin with warfarin sodium for prophylaxis against deep-vein thrombosis after hip or knee implantation. N Engl J Med 329:1370–1376
Leclerc JR, Gent M, Hirsh J, Geerts WH, Ginsberg JS (1998) The incidence of symptomatic venous thromboembolism during and after prophylaxis with enoxaparin: a multi-institutional cohort study of patients who underwent hip or knee arthroplasty. Canadian Collaborative Group. Arch Intern Med 158:873–878
Lubinus P, Klauser W (2001) Mortality after total hip replacement due to fatal pulmonary embolism. Abstract 114. 1st SICOT/SIROT Annual International Conference, Paris
Geerts WH, Heit JA, Clagett GP, Pineo GF, Colwell CW, Anderson FA Jr, et al (2001) Prevention of venous thromboembolism. Chest 119:132S–175S
McNally MA, McAlinden MG, O'Connell BM, Mollan RA (1994) Postphlebitic syndrome after hip arthroplasty. 43 patients followed at least 5 years. Acta Orthop Scand 65:595–598
Pulmonary Embolism Prevention Trial Collaboration Group (2002) Prevention of pulmonary embolism and deep vein thrombosis with low dose aspirin: Pulmonary Embolism Prevention (PEP) trial. Lancet 355:1295–1302
Hansson PO, Sorbo J, Eriksson H (2000) Recurrent venous thromboembolism after deep vein thrombosis: incidence and risk factors. Arch Intern Med 160:769–774
Prandoni P, Lensing AW, Cogo A, Cuppini S, Villalta S, Carta M, et al (1996) The long-term clinical course of acute deep venous thrombosis. Ann Intern Med 125:1–7
Ginsberg JS, Turkstra F, Buller HR, MacKinnon B, Magier D, Hirsh J (2000) Postthrombotic syndrome after hip or knee arthroplasty: a cross-sectional study. Arch Intern Med 160:669–672
Siragusa S, Beltrametti C, Barone M, Piovella F (1997) [Clinical course and incidence of post-thrombophlebitic syndrome after profound asymptomatic deep vein thrombosis. Results of a transverse epidemiologic study]. Minerva Cardioangiol 45:57–66
Das SK, Cohen AT, Edmondson RA, Melissari E, Kakkar VV (1996) Low-molecular-weight heparin versus warfarin for prevention of recurrent venous thromboembolism: a randomized trial. World J Surg 20:521–526–
Hull R, Delmore T, Carter C, Hirsh J, Genton E, Gent M, et al (1982) Adjusted subcutaneous heparin versus warfarin sodium in the long-term treatment of venous thrombosis. N Engl J Med 306:189–194
Hull R, Hirsh J, Jay R, Carter C, England C, Gent M, et al (1982) Different intensities of oral anticoagulant therapy in the treatment of proximal-vein thrombosis. N Engl J Med 307:1676–1681
Lagerstedt CI, Olsson CG, Fagher BO, Oqvist BW, Albrechtsson U (1985) Need for long-term anticoagulant treatment in symptomatic calf-vein thrombosis. Lancet II:515–518
Pini M, Aiello S, Manotti C, Pattacini C, Quintavalla R, Poli T, et al (1994) Low molecular weight heparin versus warfarin in the prevention of recurrences after deep vein thrombosis. Thromb Haemost 72:191–197
Heit JA, Elliott CG, Trowbridge AA, Morrey BF, Gent M, Hirsh J (2000) Ardeparin sodium for extended out-of-hospital prophylaxis against venous thromboembolism after total hip or knee replacement. A randomized, double-blind, placebo-controlled trial. Ann Intern Med 132:853–861
Pellegrini VD Jr, Clement D, Lush-Ehmann C (1996) Natural history of thromboembolic disease after total hip arthroplasty. Clin Orthop 333:27–40
Anonymous (2002) Regional hospital price lists. County Councils in Sweden
Bergqvist D, Benoni G, Bjorgell O, Fredin H, Hedlundh U, Nicolas S, et al (1996) Low-molecular-weight heparin (enoxaparin) as prophylaxis against venous thromboembolism after total hip replacement. N Engl J Med 335:696–700
Eriksson BI, Ekman S, Lindbratt S, Baur M, Bach D, Torholm C, et al (1997) Prevention of thromboembolism with use of recombinant hirudin. Results of a double-blind, multicenter trial comparing the efficacy of desirudin (Revasc) with that of unfractionated heparin in patients having a total hip replacement. J Bone Joint Surg Am 79:326–333
Eriksson BI, Wille-Jorgensen P, Kalebo P, Mouret P, Rosencher N, Bosch P, et al (1997) A comparison of recombinant hirudin with a low-molecular-weight heparin to prevent thromboembolic complications after total hip replacement. N Engl J Med 337:1329–1335
LINFO (2001) FASS Läkemedel i Sverige. Läkemedelsinformation AB: Oslo
Anonymous (1996) Kostnad per intagen patient (in Swedish). Federation of County Councils: Stockholm
Bergqvist D, Jönsson B (1999) Cost-effectiveness of prolonged administration of a low molecular weight heparin for the prevention of deep venous thrombosis following total hip replacement. Value Health 2:288–294
Bounameaux H, Perneger T (2002) Fondaparinux: a new synthetic pentasaccharide for thrombosis prevention. Lancet 359:1710–1711
Eikelboom JW, Quinlan DJ, Douketis JD (2001) Extended-duration prophylaxis against venous thromboembolism after total hip or knee replacement: a meta-analysis of the randomised trials. Lancet 358:9–15
Heit JA (2002) The potential role of fondaparinux as venous thromboembolism prophylaxis after total hip or knee replacement or hip fracture surgery. Arch Intern Med 162:1806–1808
Hughes SJ (2003) Fondaparinux requires further study before firm recommendation. Arch Intern Med 163:498
Vormfelde SV (2002) Enoxaparin or fondaparinux for thrombosis prevention after orthopaedic surgery. Lancet 360:1701
Schulman S, Rhedin AS, Lindmarker P, Carlsson A, Larfars G, Nicol P, et al (1995) A comparison of six weeks with six months of oral anticoagulant therapy after a first episode of venous thromboembolism. Duration of Anticoagulation Trial Study Group. N Engl J Med 332:1661–1665
Anonymous (2002) Life tables. Statistic Sweden: Stockholm
Todd CJ, Freeman CJ, Camilleri-Ferrante C, Palmer CR, Hyder A, Laxton CE, et al (1995) Differences in mortality after fracture of hip: the East Anglian audit. BMJ 310:904–908
Acknowledgements
The study was supported by a grant from Sanofi Synthelabo AB, Sweden.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lundkvist, J., Bergqvist, D. & Jönsson, B. Cost-effectiveness of fondaparinux vs. enoxaparin as venous thromboembolism prophylaxis in Sweden. HEPAC 4, 254–262 (2003). https://doi.org/10.1007/s10198-003-0175-4
Issue Date:
DOI: https://doi.org/10.1007/s10198-003-0175-4