Abstract
Background and objective
Hypertension is not a typical feature of steroid sensitive nephrotic syndrome (SSNS) and the presence of persistent hypertension is suggestive of significant renal lesion. There is paucity of data regarding occurrence and severity of hypertension in SSNS in pediatric population during remission and was the main objective of this study. In addition, correlation with factors like family history, BMI, and lipid profile was studied.
Methods
Cross-sectional study conducted at tertiary care center in India including 81 children of infrequent relapsing SSNS between 1 and 10 years in remission and was off steroids. Grading and severity of hypertension were assessed. Statistical analysis was done using SPSS version 21.0.
Results
Median age of presentation was 5 years, with male:female ratio of 1.3:1. Out of 81 infrequent relapsing SSNS children, 23.45% (19) had hypertension. Among those children with hypertension (n = 19), 73.68% (14) had positive family history compared to 32.25% (20) in those without hypertension. Positive correlation was found between BP and serum cholesterol and LDL. Of the hypertensive patients, 1 (5.26%) had fundus changes, 2 (10.52%) had features of left ventricular hypertrophy, and 13 (68.42%) had non-nephrotic range proteinuria.
Conclusion
There is high incidence of hypertension in NS children during remission. Though significant positive correlation was found with positive family history of hypertension and deranged lipid profile highlighting possibility of essential hypertension in them, there is need for close active monitoring and management of hypertension in them as untreated cases may have significant target organ damage.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nephrotic syndrome (NS) is a common chronic renal disorder in children. In countries like US and Europe cumulative prevalence is reported to be 16 per 100,000 children below 16 years and is relatively higher in the Indian subcontinent [1, 2]. About 95% cases are idiopathic with majority of them having histological picture of Minimal Change Disease (MCD). Depending on response to steroids which is the mainstay of therapy, children with NS can be categorized into steroid sensitive nephrotic syndrome (SSNS) which constitutes about 80–85% cases and steroid resistant nephrotic syndrome (SRNS) [3]. Systemic hypertension is usually not a feature of MCD, but may be transiently present during relapse or during high doses of steroid therapy, as has been reported in most studies to vary from 14% to as high as 95% [4,5,6,7,8,9,10]. Persistent hypertension in NS is usually associated with significant renal lesion and may be an indication for renal biopsy [3, 11]. Irrespective of the cause, hypertension can have both short- and long-term adverse effects on various organ systems. However, data regarding hypertension in childhood SSNS specially in remission phase are much less. Most of the available studies are in adult population; moreover, most available data are during relapse phase with only few studies evaluating hypertension during remission. Therefore, this study was done to know the occurrence of hypertension in SSNS during remission phase along with assessment of its severity in terms of end organ damage and also to study its correlation with factors like family history, BMI, and lipid profile in childhood population.
Materials and methods
This was a cross-sectional study conducted in the department of pediatrics at a tertiary care center in India from September 2015 to March 2017 for duration of 18 months. Institutional Ethical Review Board approval was obtained.
Sample size
In a study by Gabban et al., the percentage of children of SSNS with blood pressure higher than the 95th percentile was 15.15% [9]. Taking this value as reference, the minimum required sample size with 9% margin of error and 5% level of significance was 73 patients. To reduce margin of error, total sample size taken was 81.
Formula used is
where Zα is value of Z at two-sided alpha error of 5%, ME is margin of error, and p is prevalence rate.
A total of 90 children of SSNS attending pediatric nephrology clinic who were infrequent relapsers in remission and off steroids in age group of 1–10 years were included after informed written consent from all individual parents/guardians. Those requiring prednisolone for remission, those having frequent relapses, having significant hematuria, possibility of secondary causes of nephrotic syndrome like systemic lupus erythematosus, hepatitis B, hepatitis C, etc., those with known congenital anomalies of kidney or urinary tract were excluded from the study. Remission was defined as urine dipstick for proteins either nil or trace for consecutive 3 days. Infrequent relapsing nephrotic syndrome was defined as < 3 relapses in 1 year and frequent relapsing nephrotic syndrome was defined as > 2 relapses within 6 months of the initial episode or > 3 relapses in any 1 year. Nine children were further excluded (three parents withdrew consent for study, and in six, both parents were not available for evaluation). Relevant detailed history and examination including anthropometry (WHO growth standards) and biochemical investigations including lipid profile was done in 81 children. Blood pressure (BP) was recorded using a clinical sphygmomanometer (aneroid, dial type, Hiene, Gamma G5) by auscultatory method with appropriate size cuff and charts from “The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents” was used to estimate 50th, 90th, 95th, and 99th percentile BP for that age, sex and height [12]. Normal BP was defined as systolic blood pressure and diastolic blood pressure that is < 90th percentile for that gender, age and height. BP between the 90th and 95th percentile was prehypertension. If BP > 90th percentile, BP was repeated twice in the same office and the average BP was used. Hypertension was defined as average SBP and/or DBP that is ≥ 95th percentile for gender, age, and height on ≥ 3 occasions. In this study, BP was taken thrice on the same day at gap of 5–10 min. Family history of hypertension was considered to be present on the basis of history of antihypertensive medication taken by any parents or grandparents.
Those with hypertension were further graded as stage I (95th percentile up to 99th percentile plus 5 mmHg) or stage II hypertension (> 99th percentile plus 5 mmHg). In all cases with hypertension, fundus examination for evidence of hypertensive retinopathy was done and classified [13]. Left ventricular mass indexed to body surface area was estimated by LV cavity dimension and wall thickness at end-diastole by 2-D echocardiography was done to assess LV hypertrophy (LVH defined as LVMI ≥ 95th percentile compared to age and sex). Standard charts by Khoury et al. were used to classify left ventricular hypertrophy as LVMI ≥ 95th percentile compared to age and sex [14]. Spot urine protein/creatinine ratio was done to quantify proteinuria in hypertensive children [15, 16]. Figure 1 depicts the flow of study.
Statistical analysis
Categorical variables were presented in number and percentage (%) and continuous variables were presented as mean ± SD and median. Normality of data was tested by Kolmogorov–Smirnov test. Quantitative variables were compared using unpaired t test/Mann–Whitney test (when the data sets were not normally distributed) between the two groups and ANOVA/Kruskal–Wallis test (for non-parametric data) was used for comparison between more than two groups. Qualitative variables were correlated using Chi-square test/Fisher’s exact test. Spearman rank correlation coefficient was used to assess the association of grading of BP with various parameters. A p value of < 0.05 was considered statistically significant. The data were entered in MS EXCEL spreadsheet and analysis was done using Statistical Package for Social Sciences (SPSS) version 21.0.
Results
In this study, the median age of SSNS was 5 years, with slightly male predominance (male:female ratio of 1.3:1).
The mean age of patients at the time of study was 5.57 + 2.11 years, the median being 5 years. The mean age of onset of nephrotic syndrome was 4.61 + 1.62 years, with median being 4.5 years. The mean duration of nephrotic syndrome in this study was 11.91 + 8.56 months with a median of 10 months (Table 1).
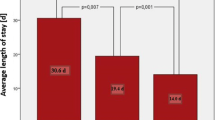
Out of 81 nephrotic children, 23.45% (19) showed hypertension. Of the 19 hypertensive children, 22.22% (18) had stage I hypertension and rest 1.23% (1) had stage II hypertension. Of the 62 normotensive children, 59.26% (48) had blood pressure < 90th percentile and rest 17.28% (14) had prehypertension (Table 2).
There was no significant difference in blood pressure between males and females. Among children with hypertension (n = 19), 73.68% (14) had family history of hypertension, whereas in those without hypertension, about 32.26% (20) had family history of hypertension and the difference was statistically significant. In addition, significant positive correlation was found between blood pressure and serum cholesterol as well as LDL. However, no significant difference in occurrence of hypertension was observed with BMI of the children (Table 3).
While evaluating for end organ damage, of 19 patients, 5.26% (1) showed fundus changes of hypertensive retinopathy having grade 2 retinopathy, 10.52% (2) patients had features of left ventricular hypertrophy (LVMI ≥ 95th percentile); however, it did not correlate with the severity of hypertension. About 68.42% (13) patients were observed to have non-nephrotic proteinuria, but did not correlate with severity of hypertension (Table 4).
Discussion
Nephrotic syndrome is a common renal disease in children and is mostly idiopathic due to MCD. It often shows good response to steroids with many children completely off steroids. Hypertension is not a common association with SSNS particularly in remission. This was a cross-sectional observational study conducted at a tertiary care center of north India to find occurrence of hypertension in nephrotic children in remission who are off steroids. 90 consecutive children in age group 1–10 years attending pediatric nephrology clinic and meeting inclusion criteria were reviewed, out of which 81 children were finally included (9 excluded due to reasons mentioned above). Median age of children was 5 years (minimum age of 2 years and maximum age of 10 years) with 60% of patients being less than or equal to 5 years. SSNS in children is mostly idiopathic and most commonly involves age group of 1–8 years [3]. There was slightly male predominance (1.31:1). Most studies have documented a higher male:female ratio as in our study ranging from 1.3:1 to 2.05:1 [4,5,6,7,8,9,10] (Table 1).
In study population (n = 81), 23.45% (19) of the children with SSNS had hypertension in remission period, out of which 22.22% (18) had stage I hypertension, and 1.23% (1) had stage II hypertension (Table 2). Of 76.54% (62) children without hypertension, 59.26% (48) had blood pressure less than 90th percentile and rest 17.28% (14) had prehypertension. It shows that about a quarter of children of SSNS continue to be hypertensive even in remission state and, therefore, does not appear to be transient. There are similar studies in patients of SSNS showing prevalence of hypertension ranging from 15 to 34%. Whereas other studies reported a much higher prevalence of hypertension ranging up to 95% [4,5,6,7,8,9,10]. However, most of these studies observed high prevalence during relapse which significantly decreased during remission. Xu et al. measured ABP (ambulatory blood pressure) in 114 children of primary nephrotic syndrome and reported a very high percentage (88.6%) to be hypertensive. Majority of them showed increased BP during sleep and large number of children (39.5%) and masked hypertension [4]. ABP is the ideal instrument to diagnose nocturnal hypertension, non-dipper hypertension, and masked hypertension which are often missed by office BP measurement, but is not routinely used for measuring BP in clinic setting.Kontchou et al. observed BP > 90th percentile (prehypertension and hypertension) in 65% out of 49 children of SSNS during relapse which decreased to 34% at the end of 4 weeks of steroid therapy. They reported high BP in SSNS is related to relapse state with edema which decreased during remission, but effect of high dose of steroids in these children was not assessed and it may have accounted for higher prevalence of hypertension as compared to this study [6]. Similarly, Kuster et al. studied 57 children and reported hypertension in as high as 95% children which significantly reduced to 19% after steroid therapy and Zsuzsanna et al. reported hypertension in 75% children in relapse state which decreased to 25% in remission out of 69 nephrotic patients, although theirs was a mixed cohort having SSNS, SDNS, and SRNS [7, 10].
In this study, 56.79% (46) were males and about 23.91% (11) of males and 22.85% (8) females had hypertension and gender difference in occurrence of hypertension was statistically not significant (p = 0.912) which is similar to studies done by Kuster et al. and Gabban et al. [7, 9].
A significantly higher percentage of children had positive family history of hypertension among those who were hypertensive 73.68% (14), whereas those children without hypertension had positive family history in about 32% (20) (p = 0.001). Similar observation was made by Kontchou et al. [6]. Correlation between BMI and hypertension was not statistically significant. There is paucity of the literature done in SSNS to correlate hypertension and BMI. However, in studies done in general population, a positive correlation has been found between BMI and essential hypertension [17,18,19,20,21].
Mean serum total cholesterol levels were high in hypertensive children (182.4 vs 153.34 mg/dl). In this study, serum total cholesterol were mostly in normal range. Despite remission, all four children who had serum cholesterol level > 200 mg/dl had hypertension. Similarly, mean values of LDL cholesterol and serum triglycerides were lower in our cohort in contrast to study by other authors as they had included patient in relapse as well; however, above variables showed higher mean values in hypertensive children and significant positive correlation was observed between grade of hypertension with LDL [8] (Table 3). Above observations suggest strong influence of factors like positive family history, high serum total cholesterol, and LDL cholesterol highlighting role of essential or primary hypertension leading to overall increased prevalence of hypertension in these children. On further evaluation of those who had hypertension for evidence of end organ damage, 5.26% (1) had features of hypertensive retinopathy (grade 2). There is a paucity of literature about end organ damage in eye due to hypertension in nephrotic patients. However, studies done in hypertensive children show prevalence of hypertensive retinopathy in 8.6–18% [22, 23]. 10.52% (2) patients had evidence of left ventricular hypertrophy but did not correlate with severity or grade of hypertension (p = 0.105). In the study done by Torres et al. in patients with NS, 98.1% showed carotid IMT > 97 percentile and 25.4% (14) patients had left ventricular mass > 110 g [8]. Studies in non-nephrotic children with hypertension have documented LVH ranging between 8 and 41.1% [24,25,26,27]. The presence of such high percentage of LVH further questions the transient nature of hypertension as considered in SSNS. 68.42% (13) patients in this study showed non-nephrotic proteinuria (spot urine protein:creatinine ratio > 0.2 but less than 1), but it did not correlate to the severity of hypertension. There is a lack of similar study in nephrotic patients. However, in children with hypertension (because of primary/any secondary cause), non-nephrotic proteinuria done by Up/Uc ratio was observed in 20–25% of the patients [15, 16].
To conclude, hypertension although not considered as typical finding in SSNS, appears to be commonly observed in remission state as well with evidence of significant end organ damage, particularly cardiovascular. Therefore, all nephrotic patients who are being followed up in remission should be routinely monitored for their blood pressure and pharmacological agents should be started early to prevent end organ damage.
Limitations
-
1.
By definition, hypertension is defined as blood pressure on three different occasions. Being a cross-sectional study, blood pressure was repeated three times on the same day may have included white-coat hypertension.
-
2.
Family history of hypertension was taken on the basis of verbal confirmation from parents as parents or grandparents taking antihypertensive medication.
-
3.
The children with stage II hypertension were small which could have been the reason of inability to find correlation of end organ damage in terms of hypertensive retinopathy, LVH, and proteinuria to the severity of hypertension.
-
4.
Baseline data about hypertension not included being a cross-sectional study. Hypertensive nephropathy was assessed using spot urine protein:creatinine ratio as in previous studies, but in this study it could be confounding.
References
Niaudet P, Boyer O. Idiopathic nephrotic syndrome in children: clinical aspects. In: Avner ED, harmon WE, Niaudet P, Yoshikawa N, Emma F, Goldstein SL, editors. Pediatric nephrology. Berlin: Springer; 2016. pp. 840.
Bagga A, Srivastava RN. Nephrotic syndrome. In: Srivastava RN, Bagga A, editors. Pediatric nephrology. New Delhi: Jaypee Brothers medical Publishers (P) LTD; 2011. p. 195.
Kliegman RM, Stanton BF, Geme JWS, Schor NF. Nelson textbook of pediatrics. 20th ed. In: Behrman RE, editors. Toronto: Elsevier; 2016. pp 2521–2527
Xu ZQ, Yi ZW, Dang XQ, Wu XC, He XJ. Relationship of 24-hour ambulatory blood pressure and rennin–angiotensin–aldosterone system in children with primary nephrotic syndrome. Zhongguo Dang Dai Er Ke Za Zhi. 2010;12(10):788–92.
Xu ZQ, Yi ZW, Dang XQ, et al. Sympathetic nervous system level and ambulatory blood pressure in children with primary nephrotic syndrome. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2010;35(7):693–8.
Kontchou LM, Liccioli G, Pela I. Blood pressure in children with minimal change nephrotic syndrome during oedema and after steroid therapy: the influence of familial essential hypertension. Kidney Blood Press Res. 2009;32(4):258–62.
Küster S, Mehls O, Seidel C, Ritz E. Blood pressure in minimal change and other types of nephrotic syndrome. Am J Nephrol. 1990;10(Suppl 1):76–80.
Torres GAA, Kitsu MAA, Loza MJE, Keever MÁV. Cardiovascular risk factors in children with primary nephrotic syndrome. Rev Med Inst Mex Seguro Soc. 2015;53(Suppl 3):S284–93. (PubMed PMID: 26509304).
Gabban NI, Abdullah EA, Abdullah HN. Nephrotic syndrome and hypertension. Iraqi J Commun Med. 2010 (4);271–76.
Zsuzsanna A, Carmen D, Eva K, Zsigmond E, et al. Clinical features and histopathological spectrum in adolescent onset nephrotic syndrome in a Romanian Children Population. Acta Med Marisiensis. 2014;60(4):146–50.
Paul VK, Bagga A. Ghai essential pediatrics. 8th ed. Chennai: CBS Publishers & Distributors Pvt Ltd; 2013.
The Fourth Report on the Diagnosis, Evaluation, and Treatment of High Blood Pressure in Children and Adolescents. https://www.nhlbi.nih.gov/files/docs/resources/heart/hbp_ped.pdf.
Grosso A, Veglio F, Porta M, Grignolo FM, Wong TY. Hypertensive retinopathy revisited: some answers, more questions. Br J Ophthalmol. 2005;89:1646–54.
Khoury PR, Mitsnefes M, Daniels SR, Kimball TR. Age specific reference intervals for indexed left ventricular mass in children. J Am Soc Echocardiogr. 2009;22:709–14.
Assadi F. Effect of microalbuminuria lowering on regression of left ventricular hypertrophy in children and adolescents with essential hypertension. Pediatr Cardiol. 2007;28:27–33.
Seeman T, Pohl M, Palyzova D, John U. Microalbuminuria in children with primary and white-coat hypertension. Pediatr Nephrol. 2012;27:461–7.
Bloetzer C, Bovet P, Paccaud F, et al. Performance of targeted screening for the identification of hypertension in children. Blood Press. 2017;26(2):87–93.
Naha NK, John M, CherianVJ. Prevalence of hypertension and risk factors among school children in Kerala, India. J Contemp Pediatr. https://doi.org/10.18203/2349-3291.ijcp20162368.
Haas GM, Bertsch T, Schwandr P. Prehypertension and cardiovascular risk factors in children and adolescents participating in the community-based prevention education program family heart study. Int J Prev Med. 2014;5(Suppl 1):S50–6.
Hong YM, Kang YJ. Suh S. Correlation between high blood pressure and lipid profile in children. Korean J Pediatr. 1995;38(12):1645–52.
Dalili S, Mohammadi H, Rezvany SM, Dadashi A, Novin MH. The relationship between blood pressure, anthropometric indices and metabolic profile in adolescents: a cross sectional study. Indian J Pediatr. 2015;82(5):445–9.
Willaims KM, Shah AN, Morrison D, Sinha M. Demographic, clinical, and ophthalmoscopic findings from a 30 year british cohort. J Paediatr Ophthalmol Strabismus. 2013;50(4):222–8.
Foster BJ, Ali H, Mamber S, Polomeno RC, Mackie AS. Prevalence and severity of hypertensive retinopathy in children. Clin Pediatr (Phila). 2009;48(9):926–30. https://doi.org/10.1177/0009922809339385. (Epub 2009 Jul 1).
Hanevold C, Waller J, Daniels S, Portman R, Sorof J. The effects of obesity, gender, and ethnic group on left ventricular hypertrophy and geometry in hypertensive children: a collaborative study of the International Pediatric Hypertension Association. Pediatrics. 2004;113(2):328–33.
Richey PA1, Disessa TG, Somes GW, Alpert BS, Jones DP. Left ventricular geometry in children and adolescents with primary hypertension. Am J Hypertens. 2010;23(1):24–9. https://doi.org/10.1038/ajh.2009.164. (Epub 2009 Oct).
Stabouli S, Kotsis V, Rizos Z, Toumanidis S, Karagianni C. Left ventricular mass in normotensive, prehypertensive and hypertensive children and adolescents. Pediatr Nephrol. 2009;24(8):1545–51. https://doi.org/10.1007/s00467-009-1165-2. (Epub 2009 May 15).
Sorof JM1, Alexandrov AV, Cardwell G, Portman RJ. Carotid artery intimal–medial thickness and left ventricular hypertrophy in children with elevated blood pressure. Pediatrics. 2003;111(1):61–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors have declared that no conflict of interest exists.
Ethical approval
IRB committee approval has been obtained.
Informed consent
Informed written consent was obtained from individual parents/guardians.
About this article
Cite this article
Keshri, S., Sharma, S., Agrawal, N. et al. Hypertension and its severity in children with steroid sensitive nephrotic syndrome during remission. Clin Exp Nephrol 22, 1157–1162 (2018). https://doi.org/10.1007/s10157-018-1565-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-018-1565-3