Abstract
Background
Idiopathic nephrotic syndrome (INS) is the most common glomerular disease in children. We performed this study to report histopathological findings, the correlation between clinical and histopathological features, and the response to steroids and other immunosuppressive drugs and outcomes in Syrian children with INS.
Methods
A single-center retrospective observational cohort study was conducted at Children’s University Hospital in Damascus, and included all patients aged 1–14 years, admitted from January 2013 to December 2022, with INS and who underwent kidney biopsy.
Results
The study included 109 patients, with a male/female ratio of 1.13:1, and a median age of 5 years with interquartile range (2.8–10). The main indication of kidney biopsy was steroid-resistant nephrotic syndrome (SRNS) (57.8%). The main histopathological patterns were minimal change disease (MCD) (45%) and focal segmental glomerulosclerosis (FSGS) (37.6%). FSGS was the most common histopathological pattern in SRNS (44.3%). In SRNS, we used calcineurin inhibitors to induce remission. Tacrolimus was used in 49 patients with response rate (complete remission of proteinuria) of 69.4% and cyclosporine in 20 patients with response rate of 50%. In steroid-dependent nephrotic syndrome (SDNS), we used mycophenolate mofetil (MMF) and cyclophosphamide to prevent relapses; MMF was used in 9 patients with response rate (maintaining sustained remission) of 89% and cyclophosphamide in 3 patients with response rate of 66.7%. Rituximab was used in four patients with FSGS, two SRNS patients and two SDNS patients, with sustained remission rate of 100%. Fifteen patients (13.7%) progressed to chronic kidney disease stage 5. Of them, 7 patients had FSGS and 8 patients had focal and global glomerulosclerosis;14 of them were steroid-resistant and one patient was steroid-dependent with persistent relapses. The most common outcome was sustained remission (47%) in MCD and frequent relapses (31.7%) in FSGS.
Conclusions
FSGS was the most common histopathological pattern in idiopathic SRNS and had the worst prognosis. Calcineurin inhibitors could be an effective therapy to induce complete remission in SRNS. Rituximab may be an effective treatment to achieve sustained remission in SDNS and frequently relapsing NS and may have a potential role in SRNS with further studies required.
Graphical abstract

A higher resolution version of the Graphical abstract is available as Supplementary information
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Idiopathic nephrotic syndrome (INS) is the most common glomerular disease in children, with an estimated annual incidence of about 2–7 per 100,000 children less than 18 years of age, and prevalence of about 12–16 per 100,000 [1, 2]. Childhood nephrotic syndrome accounts for most patients with nephrotic syndrome (NS). The International Pediatric Nephrology Association (IPNA) defined NS as nephrotic-range proteinuria (urinary protein creatinine ratio (UPCR) ≥ 2 mg/mg in a spot urine, or proteinuria in a 24-h urine ≥ 1000 mg/m2 per day) and either hypoalbuminemia (serum albumin < 30 g/L) or edema when serum albumin is not available [3, 4]. The histopathological features are of prognostic significance. Minimal change disease (MCD) is the most common histopathologic finding in childhood NS and has a high response rate to steroids and good prognosis, although most patients have one or more relapses [1, 2, 5]. Other pathologic findings can include focal segmental glomerulosclerosis (FSGS), mesangial proliferative glomerulonephritis, and other rare glomerular diseases [1, 2, 5]. Response to corticosteroids is the best prognostic marker of childhood NS, which is classified by clinical response to corticosteroids as either steroid-sensitive NS (SSNS), steroid-dependent NS (SDNS), or steroid-resistant NS (SRNS). Children with SRNS fail to achieve remission even after undergoing 4 to 8 weeks of standard steroid therapy [5]. Approximately 10–20% of children with NS have idiopathic SRNS and almost 50% of these patients progress to chronic kidney disease stage 5 [6, 7].
The management of idiopathic SRNS and SDNS is one of the challenges faced in pediatric nephrology in our country. In such patients, kidney biopsy is required, and sometimes serial biopsies may be recommended. A variety of immunosuppressive drugs have been tried, such as methyl prednisolone, calcineurin inhibitors (CNI) (cyclosporine, tacrolimus), cyclophosphamide, mycophenolate mofetil (MMF), and rituximab, with wide variation in the response to these drugs [6,7,8].
There is very little published work on the histopathological spectrum, associated clinical features, treatment, and outcome in children with INS in Syria [9, 10]. We performed this descriptive study to report histopathological findings, correlation between the clinical and histopathological features, the response to steroids, and other immunosuppressive drugs and outcomes in Syrian children with INS at our center.
Materials and methods
A single-center retrospective observational cohort study was conducted in the Department of Pediatric Nephrology at Children’s University Hospital in Damascus. Children’s Hospital is a public institution affiliated with the Faculty of Medicine at Damascus University, under the Syrian Ministry of Higher Education and Scientific Research. The study included all patients aged 1–14 years, admitted over a period of 10 years, from January 2013 to December 2022, with INS and who underwent kidney biopsy, which was studied by light microscopy and immunofluorescence staining. Electron microscopy is unavailable in our center. The presence of a minimum of eight glomeruli on light microscopy was required for the biopsy sample to be considered adequate or optimal.
We retrospectively analyzed the medical charts of all patients. Gender, age, clinical and laboratory parameters, indication of kidney biopsy, histopathological findings on light microscopy and immunofluorescence staining study, response to steroid and other immunosuppressive drugs, and outcomes were evaluated.
Histopathological findings were correlated with clinical response to steroids and immunosuppressants, other relevant clinical parameters, and outcomes.
All patients were followed until September 2023 (a period of at least 12 months post-kidney biopsy).
Definitions [3, 4]
Nephrotic-range proteinuria UPCR ≥ 2 mg/mg in a spot urine or proteinuria in a 24-h urine ≥ 1000 mg/m2 per day corresponding to 3 + or 4 + by urine dipstick.
Nephrotic syndrome Nephrotic-range proteinuria and either hypoalbuminemia (serum albumin < 30 g/L) or edema when serum albumin is not available.
Complete remission UPCR (based on first morning void or 24-h urine sample) ≤ 0.2 mg/mg or negative or trace dipstick on 3 or more consecutive days.
Steroid-sensitive nephrotic syndrome (SSNS) Complete remission within 4 weeks of prednisolone at standard dose (60 mg/m2/day or 2 mg/kg/day, maximum 60 mg/day).
Steroid-resistant nephrotic syndrome (SRNS) Lack of complete remission within 4 weeks of treatment with prednisolone at standard dose ± followed by three methylprednisolone pulses.
Relapse Urine dipstick ≥ 3 + on 3 consecutive days or UPCR ≥ 2 mg/mg on a first morning urine sample, with or without reappearance of edema in a child who had previously achieved complete remission.
Frequently relapsing nephrotic syndrome (FRNS) ≥ 2 relapses in the first 6 months following remission of the initial episode or ≥ 3 relapses in any 12 months.
Steroid-dependent nephrotic syndrome (SDNS) A patient with SSNS who experiences 2 consecutive relapses during recommended prednisolone therapy for first presentation or relapse or within 14 days of its discontinuation.
Steroid-sparing agent-resistant (SRNS) Absence of remission after 6 months of treatment with a steroid-sparing agent at adequate doses and/or levels.
Sustained remission No relapses over 12 months with or without therapy.
INS Patients were categorized as having INS when no distinctive clinical or laboratory features indicative of a secondary cause were identified (INS = NS in the absence of systemic or extrarenal disorders).
NS with nephritic component NS with hematuria, hypertension, or kidney failure.
Hypertension was characterized by systolic or diastolic blood pressure levels exceeding the 95th percentile for age, gender, and height [11].
Follow-up interruption was defined as the patient’s discontinuation of clinical visits for a period of 6 months or more.
Treatment protocol
All patients with INS were treated with a daily oral prednisolone dosage of 60 mg/m2 for a duration of 4 weeks. In cases where remission was not attained within this 4-week treatment period, they received three methylprednisolone pulses (20 mg/kg per dose for 3 consecutive days) for possible response. Subsequently, if they failed to achieve remission, they were considered steroid resistant. Children who had SRNS received calcineurin inhibitors (cyclosporine or tacrolimus) to induce remission, subsequent to undergoing a kidney biopsy. For individuals attaining remission following steroid therapy, an alternate day prednisolone regimen at 40 mg/m2 was administered for a duration of 4 weeks. Subsequently, a gradual tapering of prednisolone occurred over the next 2–3 months, leading to its eventual discontinuation.
MMF and cyclophosphamide were used in a few SDNS patients to prevent relapses and maintain sustained remission as steroid-sparing agents. Rituximab was used in four patients; two patients were steroid resistant and two were steroid dependent.
Statistical analysis
Data collection was conducted using Microsoft Excel (Version 2016). Categorical variables were presented as frequencies and percentages, while continuous variables were presented by their median values and range or interquartile range (IQR).
We made a statistical analysis using the SPSS program (Version 26). We used the Chi-square test for categorical variables, and the Mann–Whitney U test for continuous variables when comparing two independent samples with non-normal distributions, to study the presence of NS with nephritic component rates, steroid resistance rates, sustained remission rates, and median age across the two different histopathological patterns (FSGS and MCD). Statistical significance was determined by a p-value less than 0.05.
Results
This study included 109 patients admitted to Children’s University Hospital in Damascus with INS and who underwent kidney biopsy over a period of 10 years, from January 2013 to December 2022. The number of INS patients who underwent kidney biopsy was the fewest in 2020 (6 cases/year), which was due to the COVID-19 epidemic (Fig. 1).
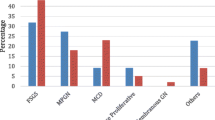
Our patients included 58 (53.2%) males and 51 (46.8%) females. The median age at presentation was 5 years, ranging from 1 to 14 years (IQR 2.8–10 years). The parents of 54 patients (49.5%) had blood relation (positive consanguinity), and 20 patients (18.3%) had a positive family history of NS. The associated clinical features were microscopic (and occasionally macroscopic) hematuria (30.2%), hypertension (18.3%), and kidney failure (10%). The indications of kidney biopsy were SRNS (57.8%), NS with nephritic component (26.6%), SDNS (9.1%), and FRNS (6.4%). The histopathological patterns were predominantly MCD (45%) and FSGS (37.6%) followed by the other patterns. FSGS was the most common histopathological pattern in SRNS patients (44.3%) then MCD (38.6%) (Table 1).
By reviewing the histopathology based on the indications for kidney biopsy we found that FSGS was the most common histopathological pattern when the indication of biopsy was SRNS or NS with nephritic component, and MCD was the histopathological pattern in 80 and 100% when the indication of biopsy was SDNS and FRNS, respectively (Table 2).
Histopathological findings were correlated with age groups. MCD was most common between 4 and 8 years of age (38.8%), while FSGS was most common between 1 and 4 years (39%). Focal and global glomerulosclerosis, mesangial glomerulonephritis, and membranous glomerulonephritis were most common between 8 and 14 years (Fig. 2).
Histopathological findings were correlated with clinical features. We found that MCD is the least associated with NS with nephritic component (NS with hematuria, hypertension, or kidney failure) (Table 3).
Table 4 shows the treatment protocol adopted in our patients with the response rate to steroids and other immunosuppressive drugs, and Table 5 shows the steroid response rate across the age groups.
We evaluated the outcomes of our patients according to the histopathological pattern (Table 6). There were five deaths due to infection, which was COVID-19 in three cases and pneumonia without identifying the germ, treated with meropenem, in two cases.
We compared FSGS and MCD patients. We found that the presence of NS with nephritic component was higher in FSGS patients with statistical significance (p-value = 0.008), and the sustained remission was higher in MCD patients with statistical significance (p-value = 0.04) (Table 7).
Discussion
Nephrotic syndrome remains the main concern of the pediatric nephrologist because of its high prevalence, and many complications associated with persistent NS including poor quality of life, hypertension, serious infections, and possibility of leading to chronic kidney disease stage 5. By reviewing the medical literature of the incidence of SRNS and SDNS, we observed an increasing trend in such cases, particularly over the past decade [6]. Alarmingly, about 50% of these cases will lead to chronic kidney disease stage 5 [6]. The management of such cases, mostly due to FSGS, remains a difficult mission.
Limited research has been published on the histopathological spectrum, treatment, and outcome in children with INS in Syria; therefore, our study is important to address this gap and emphasizes the potential impact and contributions that it could make to the field.
A retrospective study about genetic screening in 58 Syrian patients aged 0 to 12 years at presentation with challenging NS revealed that the most common histopathologic diagnoses were FSGS (41%), MCD (34%), and mesangioproliferative glomerulonephritis (14%). A genetic disease cause was identified in 20.7% of the screened patients. The study concluded that genetic testing is indicated in pediatric patients with SRNS [9].
In 2015, Syrian participation was registered by Dr. Saeed from Kidney Hospital, Damascus in The PodoNet Registry Cohort. The PodoNet Consortium has created an international registry for congenital NS and childhood-onset SRNS. From August 2009 to August 2014, 1655 patients were registered aged 0–20 years at disease onset. Among these, 153 (9.2%) patients were living in the Middle East (Syria, Lebanon, Iran, and the United Arab Emirates). The most common histopathologic diagnoses were FSGS (56%), minimal change nephropathy (21%), and mesangioproliferative GN (12%). Mutation screening was performed in 1174 patients, and a genetic disease cause was identified in 23.6% of the screened patients. The study concluded that confirmation of a genetic diagnosis but not the histopathologic disease type in children with SRNS was strongly predictive of intensified immunosuppressive therapy responsiveness [10].
Our study included 109 INS patients, with a slight predominance of males (a male-to-female ratio of 1.13:1). Medical literature indicates a male gender predominance, with a male-to-female ratio reported in the range of 1.2:1 to 2:1 [1, 6, 12, 13].
Our patients’ ages at presentation ranged from 1 to 14 years, with a median age of 5 years (IQR 2.8–10 years), which was a little younger than what is mentioned in the medical literature [6, 12, 13]. The majority of our patients (65%) were between 1 and 8 years of age. Chaudhari et al. reported that 50% of Indian children with NS presented in the age group 0–8 years [1].
Consanguineous marriages are common in our region. We found that the parents of 54 patients (49.5%) had blood relation, and 20 patients (18.3%) had a positive family history of NS. The patients with parental consanguinity had a higher rate of steroid resistance (81.5%), and the majority (90%) of the patients with a family history of NS, which was SRNS, had also SRNS. Unfortunately, genetic analysis was unavailable. They were treated according to the adopted treatment protocols. The patients with a family history of NS had poor outcomes, and of them only two patients had sustained remission with tacrolimus, while the others developed chronic kidney disease stage 5, death, or discontinued follow-up.
Kidney biopsy in NS is generally indicated in SRNS before starting immunosuppressive drugs, age of onset below 1 year or above 15 years, persistent microscopic hematuria, low C3 levels, sustained hypertension, acute kidney injury not related to hypovolemia, or raised suspicion of secondary causes of NS [3, 12, 14]. The most common indication of kidney biopsy in our patients was SRNS (57.8%) followed by NS with nephritic component (26.6%).
Chaudhari et al. found that MCD was the most common histopathological pattern in pediatric NS (47.14%), followed by FSGS (22.85%); therefore, they concluded that MCD is still the most common histopathological pattern in pediatric NS but a rise in FSGS cases is now being encountered [1], which is consistent with our results, where the two main histopathological patterns of our INS patients were MCD (45%) and FSGS (37.6%). The majority of our MCD patients (75.5%) were under 8 years of age, in line with the medical literature [1, 12]. FSGS was the most common histopathological pattern in our SRNS patients (44.3%) in line with reports by others [1, 7, 12, 15].
Hypertension will develop in 10–35% of children with INS depending on the histologic pattern, and about 20% of children with MCD will experience hematuria [16]. A recent study reported a significant number of children with NS have hypertension [17].
Hematuria was found in 30.2% of our patients, and it was most common in MPGN patients (75%). Hypertension was found in 18.3% of our patients, and was most common in MPGN patients (75%). In a study of childhood NS in Nigeria, Ibeneme et al. reported hypertension in 56% of the patients and hematuria in 53.8% [13]. Taner et al. found in a study of pediatric NS from Turkey that the prevalence of hypertension and hematuria in patients with MPGN was 67% [12]. In contrast, Alchi et al. mentioned that hematuria has been reported in 20–30% of MPGN patients [18]. We found kidney failure in 10%, and it was most common in focal and global glomerulosclerosis patients (62.5%). Most of our patients (79.8%) were treated with steroid-sparing agents, where they had SRNS, SDNS, or FRNS. We use calcineurin inhibitors to induce remission in SRNS patients as the first-line choice in line with Kidney Disease: Improving Global Outcomes (KDIGO) guidelines [19]. In our study, we used tacrolimus (49 patients) more than cyclosporine (20 patients) due to the frequent side effects of the latter, especially hirsutism and gingival hyperplasia. The complete remission rate with tacrolimus was (69.4%), exceeding the complete remission rate achieved with cyclosporine (50%) in line with the medical literature [20, 21]. This issue is still debated among nephrologists, and the difference in complete remission rates in our study may be related to the difference in sample sizes.
In SDNS and FRNS, we use MMF and cyclophosphamide after inducing remission with prednisone to prevent relapses. MMF was used in 9 patients with a response rate (maintaining sustained remission) of 89%, while we used cyclophosphamide in 3 patients with a response rate of 66.7%. Given the limited number of patients in our study and its retrospective analysis, it is pointless to compare the two drugs. However, MMF was a good choice to treat SDNS patients without recording significant side effects in line with KDIGO guidelines [19].
We tried tacrolimus with MMF and steroid in two patients, who were resistant to steroid and tacrolimus, without response.
Despite the effectiveness of rituximab mentioned in the medical literature, we administered it to just four patients due to its high cost and the current poor economic conditions in our country. Two patients were steroid-dependent, and two were steroid-resistant but tacrolimus-sensitive. All four patients developed persistent relapses with tacrolimus and had FSGS lesions on biopsy. The response rate of rituximab was 100% with continuous remission until present (more than 2 years).
Rituximab is a chimeric monoclonal antibody that effectively depletes CD20 B cells by targeting the CD20 receptor. Recent studies have reported the success of rituximab in achieving remission of pediatric NS, mainly in SDNS and FRNS, and to a lesser extent in SRNS cases [22, 23].
In a recent study, Basu et al. concluded that using rituximab in SDNS as the initial treatment seems to result in a more extended period of remission compared to its use as a secondary therapy, and that employing maintenance MMF after rituximab administration leads to sustained, long-term remission [24].
Regarding response to steroids, a significant proportion of our patients (64.2%) were steroid resistant, as our study inclusion criteria specifically included those children who underwent kidney biopsy. The lowest rate of steroid resistance was in the age group between 4 and 8 years (51.5%) where most of them (57.5%) had MCD, while the highest rate of steroid resistance was in the age group between 1 and 4 years (78.9%) with MCD pattern in 47.3% of them.
Sustained remission was reported in 35.8% of our patients, 47% in MCD patients, and 26.8% in FSGS patients.
Fifteen patients progressed to chronic kidney disease stage 5 (13.7%), and of them 7 patients had FSGS and 8 patients had focal and global glomerulosclerosis as an advanced stage of FSGS. Of these patients,14 of them were steroid resistant and one patient initially showed dependence on steroids with persistent relapses. However, over time, this patient developed secondary steroid resistance following prolonged relapses. Despite attempts with steroid-sparing agents, none of these 15 patients achieved sustained remission. Many studies have concluded that the underlying kidney histopathology modulate response to treatment is progression to chronic kidney disease stage 5, and that FSGS is a predictive factor of progression to chronic kidney disease stage 5, particularly in those who were resistant to steroids and other immunosuppressants [12, 25,26,27].
Regarding the five cases of death, the infection was the direct cause of death (3 cases of COVID-19 and 2 cases of pneumonia without identifying the germ); four patients had FSGS and one patient had mesangial glomerulonephritis, and all of them were steroid and immunosuppressant resistant.
By studying the outcomes according to the histopathological pattern, we found that the most common outcome was sustained remission (47%) in MCD patients and frequent relapses (31.7%) in FSGS patients, taking into consideration that all our patients were patients with NS who required a kidney biopsy for indications mentioned above. All patients with focal and global glomerulosclerosis (8 patients) progressed to chronic kidney disease stage 5. Most mesangial glomerulonephritis patients (60%) developed sustained remission. In the four patients with MPGN, we reported two cases (50%) with frequent relapses, one case with persistent proteinuria and one case with sustained remission. For the two patients with membranous glomerulonephritis, frequent relapses were reported in one case and sustained remission in the other.
We compared FSGS and MCD patients, where we found that the median age at presentation was without statistical significance (p-value > 0.05) in line with what was reported by Taner et al. [12], and the steroid resistance was higher in FSGS patients without statistical significance, while the presence of NS with nephritic component was higher in FSGS patients with statistical significance (p-value = 0.008), and the sustained remission was higher in MCD patients with statistical significance (p-value = 0.04).
Our study has several limitations, one of them being that it is a single-center study. Moreover, the presence of confounding factors included the absence of genetic studies, the exclusion of patients lacking kidney biopsy, which impacted response and outcome rates, and difficulty accessing immunosuppressants, like rituximab, due to high costs.
Conclusion
The best predictor of long-term kidney function and prognosis in childhood INS is response to corticosteroids and other immunosuppressants. MCD and FSGS were the most common associated histological lesions of INS. FSGS was the most common histopathological pattern in idiopathic SRNS and has the worst prognosis. Calcineurin inhibitors could be an effective therapy to induce complete remission in SRNS. Rituximab may be an effective treatment to achieve sustained remission in SDNS and FRNS and may have a potential role in SRNS with further studies required. Our country is still facing economic issues that affect clinical care, such as access to medications due to cost and availability, drug-level monitoring, kidney biopsy, and genetic study.
Data availability
The author can provide the datasets used and/or analyzed during the current study upon reasonable request, and readers can contact the author for access.
References
Chaudhari CS, Gadgil NM, Kumavat PV, Kshirsagar GR, Dhamne S (2017) Clinicopathological study of nephrotic syndrome in Indian children: a tertiary care experience. Annals of Pathology and Laboratory Medicine 4:A28-8. https://doi.org/10.21276/apalm.2017.995
Niaudet P, Boyer O (2016) Idiopathic nephrotic syndrome in children: clinical aspects. In: Avner ED, Harmon WE, Niaudet P, Yoshikawa N, Emma F, Goldstein SL (eds) Pediatric nephrology, 7th edn. Springer, Heidelberg, pp 840–869
Trautmann A, Boyer O, Hodson E, Bagga A, Gipson DS, Samuel S, Wetzels J, Alhasan K, Banerjee S, Bhimma R, Bonilla-Felix M, Cano F, Christian M, Hahn D, Kang HG, Nakanishi K, Safouh H, Trachtman H, Xu H, Cook W, International Pediatric Nephrology Association (2023) IPNA clinical practice recommendations for the diagnosis and management of children with steroid-sensitive nephrotic syndrome. Pediatr Nephrol 38:877–919. https://doi.org/10.1007/s00467-022-05739-3
Trautmann A, Vivarelli M, Samuel S, Gipson D, Sinha A, Schaefer F, Hui NK, Boyer O, Saleem MA, Feltran L, Müller-Deile J, Becker JU, Cano F, Xu H, Lim YN, Smoyer W, Anochie I, Nakanishi K, Hodson E, Haffner D, International Pediatric Nephrology Association (2020) IPNA clinical practice recommendations for the diagnosis and management of children with steroid-resistant nephrotic syndrome. Pediatr Nephrol 35:1529–1561. https://doi.org/10.1007/s00467-020-04519-1
Rheault MN (2017) Nephrotic syndrome. In: Kher KK, Schnaper HW, Greenbaum LA (eds) Clinical pediatric nephrology, 3rd edn. CRC Press, Taylor & Francis Group, Boca Raton, pp 285–296
Kashif AW, Ranjan A, Kalra S, Shravani Uttpal D, Malik A (2022) Clinicopathological spectrum and treatment outcome of idiopathic steroid-resistant nephrotic syndrome in children at a tertiary care center. Med J Armed Forces India 78:291–295. https://doi.org/10.1016/j.mjafi.2020.11.004
Ashry BG (2021) Clinico-pathological patterns of childhood idiopathic steroid-resistant nephrotic syndrome: a retrospective single-center experience. Sohag Med J 25:45–53. https://doi.org/10.21608/smj.2021.87546.1270
Esezobor C, Ademola AD, Adetunji AE, Anigilaje EA, Batte A, Jiya-Bello FN, Furia FF, Muoneke U, McCulloch M, Nourse P, Obiagwu P, Odetunde O, Okyere P, Solarin A, Tannor EK, Noone D, Gbadegesin R, Parekh RS, Human Hereditary and Health in Africa Kidney Disease Research Network (2021) Management of idiopathic childhood nephrotic syndrome in sub-Saharan Africa: Ibadan consensus statement. Kidney Int 99:59–67. https://doi.org/10.1016/j.kint.2020.07.045
Saeed B (2020) Genetic screening in children with challenging nephrotic syndrome. Saudi J Kidney Dis Transpl 31:1189–1197. https://doi.org/10.4103/1319-2442.308327
Trautmann A, Bodria M, Ozaltin F, Gheisari A, Melk A, Azocar M, Anarat A, Caliskan S, Emma F, Gellermann J, Oh J, Baskin E, Ksiazek J, Remuzzi G, Erdogan O, Akman S, Dusek J, Davitaia T, Özkaya O, Papachristou F, PodoNet Consortium (2015) Spectrum of steroid-resistant and congenital nephrotic syndrome in children: the PodoNet registry cohort. Clin J Am Soc Nephrol 10:592–600. https://doi.org/10.2215/CJN.06260614
Macumber IR, Flynn JT (2020) Systemic hypertension. In: Behrman RE, Kliegman RM, St Geme JW, Blum NJ, Shah SS, Tasker RC et al (eds) Nelson textbook of pediatrics, 21st edn. Elsevier, Philadelphia, pp 2490–2499
Taner S, Kocaaslan NE, Kabasakal C, Keskinoğlu A, Şen S, Bulut IK (2023) Evaluation of children with nephrotic syndrome: a single center experience. J Pediatr Res 10:118–124. https://doi.org/10.4274/jpr.galenos.2023.37928
Ibeneme CA, Ezuruike EO, Onuh EF (2021) Steroid response rate in childhood nephrotic syndrome at a tertiary hospital in South-Eastern Nigeria. Nigerian J Med 30:86–90. https://doi.org/10.4103/NJM.NJM_180_20
Souilmi FZ, Houssaini TS, Alaoui H, Harmouch T, Atmani S, Hida M (2015) Indications and results of renal biopsy in children: a single-center experience from Morocco. Saudi J Kidney Dis Transpl 26:810–815. https://doi.org/10.4103/1319-2442.160225
Saleem MA (2013) New developments in steroid-resistant nephrotic syndrome. Pediatr Nephrol 28:699–709. https://doi.org/10.1007/s00467-012-2239-0
Erkan E (2020) Nephrotic syndrome. In: Kliegman RM, St Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM (eds) Nelson textbook of pediatrics, 21st edn. Elsevier, Philadelphia, pp 2752–2760
Shatat IF, Becton LJ, Woroniecki RP (2019) Hypertension in childhood nephrotic syndrome. Front Pediatr 7:28. https://doi.org/10.3389/fped.2019.00287
Alchi B, Jayne D (2010) Membranoproliferative glomerulonephritis. Pediatr Nephrol 25:1409–1418. https://doi.org/10.1007/s00467-009-1322-7
Kidney Disease: Improving Global Outcomes (KDIGO) Glomerular Diseases Work Group (2021) KDIGO 2021 clinical practice guideline for the management of glomerular diseases. Kidney Int 100:S1–S276. https://doi.org/10.1016/j.kint.2021.05.021
Wang W, Xia Y, Mao J et al (2012) Treatment of tacrolimus or cyclosporine A in children with idiopathic nephrotic syndrome. Pediatr Nephrol 27:2073–2079. https://doi.org/10.1007/s00467-012-2228-3
Ravanshad Y, Zeraati A, Golsorkhi M, Ravanshad S, Azarfar A, Jafari H (2019) Comparative evaluation of tacrolimus and cyclosporine in patients with steroid-resistant nephrotic syndrome: a systematic review and meta-analysis. Rev Clin Med 6:123–134. https://doi.org/10.22038/rcm.2019.14142
Kallash M, Smoyer WE, Mahan JD (2019) Rituximab use in the management of childhood nephrotic syndrome. Front Pediatr 7:178. https://doi.org/10.3389/fped.2019.00178
Okutsu M, Kamei K, Sato M, Kanamori T, Nishi K, Ishiwa S, Ogura M, Sako M, Ito S, Ishikura K (2021) Prophylactic rituximab administration in children with complicated nephrotic syndrome. Pediatr Nephrol 36:611–619. https://doi.org/10.1007/s00467-020-04771-5
Basu B, Erdmann S, Sander A, Mahapatra TKS, Meis J, Schaefer F (2023) Long-term efficacy and safety of rituximab versus tacrolimus in children with steroid dependent nephrotic syndrome. Kidney Int Rep 8:1575–1584. https://doi.org/10.1016/j.ekir.2023.05.022
Abrantes MM, Cardoso LS, Lima EM, Silva PJM et al (2006) Predictive factors of chronic kidney disease in primary focal segmental glomerulosclerosis. Pediatr Nephrol 21:1003–1012. https://doi.org/10.1007/s00467-006-0138-y
Paik KH, Lee BH, Cho HY, Kang HG, Ha IS, Cheong HI, Jin DK, Moon KC, Choi Y (2007) Primary focal segmental glomerular sclerosis in children: clinical course and prognosis. Pediatr Nephrol 22:389–395. https://doi.org/10.1007/s00467-006-0301-5
Hjorten R, Anwar Z, Reidy KJ (2016) Long-term outcomes of childhood-onset nephrotic syndrome. Front Pediatr 4:53. https://doi.org/10.3389/fped.2016.00053
Acknowledgements
I would like to acknowledge that a version of this manuscript has been previously deposited on a pre-print server. I believe that sharing our findings in this way contributes to the dissemination of knowledge within the scientific community.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
Approval from the Medical Research Ethics Committee of Damascus University was obtained before the start of the study, without the need for informed written consent from patients’ caregivers, as the study was retrospective. Data collection from patient medical files was obtained provided that all patient data was treated according to the ethical guidelines with complete respect to patient privacy and confidentiality.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Competing interests
The author declares no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wannous, H. Idiopathic nephrotic syndrome in Syrian children: clinicopathological spectrum, treatment, and outcomes. Pediatr Nephrol 39, 2413–2422 (2024). https://doi.org/10.1007/s00467-024-06333-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-024-06333-5