Abstract
Background
Chronic kidney disease patients share clinical and pathological features with the general aging population. Increased oxidative DNA damage, accumulation of cell cycle-arrested cells and decreased Klotho expression are assumed to be age-related factors that are reportedly linked to kidney disease. This study sought to determine the association between these age-related factors and renal damage in patients with IgA nephropathy (IgAN).
Methods
We performed a cross-sectional analysis of 71 patients who were diagnosed with IgAN by renal biopsy. Expression of 8-hydroxydeoxyguanosine (8-OHdG, a marker of oxidative DNA damage), p16 (a marker of cell cycle-arrest) and Klotho (an anti-aging protein) were evaluated by immunohistochemical staining of renal biopsy samples. We correlated the changes in expression of these markers with Lee’s pathologic grades and the Oxford classification. We also investigated the independent association between these markers and interstitial fibrosis using multiple linear regression analysis.
Results
8-OHdG and p16 increased but Klotho decreased with progression of pathologic grade. Expression of 8-OHdG and p16 increased with the deterioration of mesangial hypercellularity and segmental glomerulosclerosis. In addition, p16 increased but Klotho decreased with progression of tubular atrophy/interstitial fibrosis. In univariate regression analysis, age, body mass index, systolic blood pressure, urinary protein excretion and expression of 8-OHdG, p16 and Klotho showed significant correlations with interstitial fibrosis. Multivariable regression analyses revealed that aging, increased renal expression of p16 and decreased expression of Klotho were independently correlated with interstitial fibrosis.
Conclusions
The age-related factors might play important roles in the development of IgAN.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic kidney disease (CKD) is defined as reduced glomerular filtration rate (GFR), increased urinary albumin excretion, or both. The prevalence of CKD is estimated to be 8–16 % worldwide and is thereby recognized as a global health concern [1]. Previous studies have demonstrated that the mean loss of GFR is 0.75 mL/min per year with aging in a healthy population and that the proportion of CKD patients in people over age 70 is more than 40 % [2]. Furthermore, CKD presents increased risks for acute kidney injury (AKI) and kidney cancer [3, 4]. Although the aging population shares clinical features with CKD patients [5], the molecular mechanisms underlying the aging process that contribute to the reduction of renal function and increased risks for AKI and kidney cancer remain unclear.
Regardless of the primary disease, renal fibrosis is known to be a final common pathway to renal insufficiency. Pathologically, renal fibrosis is characterized by glomerulosclerosis, tubular atrophy and interstitial fibrosis [6]. In the elderly, fibrosis is also observed in renal biopsies of transplantation donors, suggesting that molecular changes with aging contribute to renal fibrosis [7]. Importantly, recent studies have shown that various stresses can cause age-related cellular and molecular alterations [8]. These findings led to the hypothesis that changes associated with aging are increased in the development of renal fibrosis.
Previous studies have found that oxidative DNA damage and accumulation of cell cycle-arrested cells increase whereas Klotho expression decreases in an age-dependent manner [9, 10].
Mitochondria-generated reactive oxygen species (ROS) induce oxidative DNA damage, playing an important role in progression of renal fibrosis [11]. In addition, permanent and irreversible cell cycle arrest is a central paradigm of cellular senescence in vitro [9]. The accumulation of cell cycle-arrested cells is reportedly associated with renal fibrosis through secretion of fibrogenic factors [12]. In contrast, Klotho is identified as an anti-aging factor [10] and confers beneficial effects on renal fibrosis [13, 14]. Increased oxidative DNA damage, the accumulation of cell cycle-arrested cells and decreased Klotho expression are assumed to be age-related factors that are likely linked to renal fibrosis. However, no previous study has examined whether these factors are simultaneously associated with renal fibrosis.
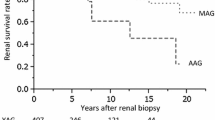
Immunoglobulin A nephropathy (IgAN) is the most common primary glomerulonephritis in many countries. The proportion of IgAN patients is estimated to be approximately 30 % among the patients who undergo renal biopsy [15]. The prognosis of IgAN is not optimistic, and 20–40 % of patients progress to end-stage renal disease (ESRD) within 20 years of diagnosis [16]. It has been reported that pathologic grading by Lee et al. [17, 18] to evaluate renal damage and to predict renal outcome is quite useful. For more accurate prediction of renal outcome, mesangial hypercellularity, segmental glomerulosclerosis, endocapillary hypercellularity and tubular atrophy/interstitial fibrosis have recently been defined as pathologic variables in the Oxford classification of IgAN [19]. Among those, interstitial fibrosis is reported to show the strongest correlation with renal outcomes [20]. However, the association between age-related factors and interstitial fibrosis remains unclear. In addition to aging, it is well known that obesity, hypertension and proteinuria influence renal outcome, including reduced estimated glomerular filtration rate (eGFR), increased creatinine or starting dialysis [21, 22]. Therefore, age-related factors and clinical parameters that independently correlate with interstitial fibrosis should be determined by multivariable analysis.
In this study, we assessed the level of 8-hydroxydeoxyguanosine (8-OHdG) (a marker of oxidative DNA damage), p16 (a marker of cell cycle-arrest) and Klotho expression in the pathogenesis of IgAN. The data thereby obtained also allowed us to determine the association of age, body mass index (BMI), systolic blood pressure (SBP), urinary protein excretion, and renal levels of 8-OHdG, p16 and Klotho with interstitial fibrosis by multiple linear regression analysis.
Materials and methods
Study design and patient population
We performed a cross-sectional analysis of 71 patients (40 male, 31 female) who were diagnosed with IgAN. All patients underwent renal biopsy for the first time at Hiroshima University Hospital from April 2008 to December 2010. Mesangial proliferative glomerulonephritis with positive immunofluorescent staining of mesangial deposits of IgA were diagnostic criteria for IgAN. Patients who had secondary IgAN, such as Henoch–Schönlein purpura nephritis or lupus nephritis, were excluded. We classified patients in five groups in accordance with the pathologic classification method reported by Lee et al. [17]. For patients with hypertension, one or more antihypertensive drugs were administered, i.e., angiotensin-converting enzyme inhibitors or angiotensin-receptor blockers or calcium channel blockers. At the time of renal biopsy, none of the patients were receiving oral immunosuppressive therapy. After the renal biopsy, three patients started oral corticosteroids, and nineteen started pulse steroid therapy combined with tonsillectomy. The study was approved by the Ethics Committee of Hiroshima University (H-852).
Reagents
The following antibodies and reagents were used in this study: anti-8-OHdG mouse monoclonal antibody (Japan Institute for the Control of Aging, Shizuoka, Japan), anti-p16 mouse monoclonal antibody (F-12, Santa Cruz Biotechnology Inc., Santa Cruz, CA, USA), and anti-Klotho monoclonal antibody (Clone KM2076, Transgenic Inc., Kobe, Japan).
Immunohistochemistry
Renal tissue biopsy samples were fixed in 10 % formalin, washed in ethanol and embedded in paraffin. Four-micron-thick sections were used for immunohistochemistry. Paraffin sections were de-waxed in xylene and rehydrated, and endogenous peroxidase activity was blocked by incubation in 0.6 % H2O2 in methanol for 20 min. The sections were boiled in sodium citrate solution for 30 min and then returned to room temperature.
For detection of 8-OHdG, the streptavidin–biotin (SAB) method was used (Histofine kit, Nichirei Biosciences Inc., Tokyo, Japan). After blocking with 10 % normal rabbit serum for 20 min, the sections were incubated with a 1/100 dilution of anti-8-OHdG antibody at 4 °C overnight. After washing in phosphate-buffered saline (PBS), the sections were incubated with biotin-conjugated anti-mouse IgG + IgA + IgM for 30 min. Next, the sections were incubated with a streptavidin-conjugated peroxidase for 30 min, and then developed with 3, 3-diaminobenzidine tetrahydrochloride (DAB) (Sigma-Aldrich, St. Louis, MO, USA) to produce a brown color.
For detection of p16 and Klotho, the avidin–biotin complex (ABC) method was used. After antigen retrieval and washing with PBS, the following steps were carried out using a Vectastain ABC kit (Vector Laboratories, Burlingame, CA, USA). Nonspecific binding was blocked by incubation (30 min) with normal horse serum for p16 staining whereas normal rabbit serum was used for Klotho staining. The sections were incubated with 1/300 dilution of mouse anti-p16 antibody or 1/25 dilution of rat anti-Klotho antibody at 4 °C overnight. After washing in PBS, the sections were incubated with the secondary antibody, i.e., biotinylated anti-mouse IgG for p16 or anti-rat IgG for Klotho for 30 min. After washing in PBS, the sections were incubated with the ABC for 30 min. Following a PBS rinse, the sections were developed with DAB.
For evaluation of fibrosis, kidney sections were stained with Masson’s trichrome (MT) in routine diagnostics procedures.
Quantification
All tissues examined contained at least ten glomeruli that did not exhibit sclerosis based on light microscopic examination (200× magnification). NIH ImageJ Version 1.45 software was used for lesion quantification and data are expressed as the percent area that immunostained positively. Using MT staining, evaluation of fibrosis was performed as the proportion that was blue. Each tissue was evaluated as described in the Oxford classification of IgAN [23]. Mesangial hypercellularity was scored positive if more than 50 % of the glomeruli showed mesangial hypercellularity (Oxford M0, M1). The presence of tuft adhesion and segmental glomerulosclerosis was investigated (Oxford S0, S1). Oxford T0–T2 was classified as the cortical area percentage indicating tubular atrophy or interstitial fibrosis (T0, 0–25 %; T1, 26–50 %; T2, >50 %). Because there were few cases indicating endocapillary hypercellularity, statistical analysis could not be performed in the Oxford E.
Statistical analysis
All variables were expressed as mean ± SD or median (range; interquartile range). Statistical analysis was performed with analysis of variance (ANOVA) followed by the Tukey–Kramer honestly significant difference test to compare the levels of 8-OHdG, p16 and Klotho between the IgAN subgroups and pathological score. Univariate linear regression analysis was performed to identify significant associations between interstitial fibrosis and the following variables: age, BMI, SBP, total urinary protein excretion, and % areas positive for 8-OHdG, p16 and Klotho. Multiple linear regression analysis was performed for significant variables. Statistical significance was set at the level of P < 0.05. All analyses were carried out with Statistical Package for the Social Sciences (SPSS) software (Version 21.0; IBM, International Business Machines Corp., Armonk, New York, USA).
Results
Clinical characteristics at biopsy
The clinical characteristics of patients with IgAN are summarized in Table 1. In this patient population, the average clinical values were as follows: 33 ± 12 years of age, BMI was 21.67 ± 2.95 kg/m2, SBP was 115 ± 13 mmHg, diastolic blood pressure (DBP) was 68 ± 10 mmHg, creatinine clearance (Ccr) was 97.48 ± 28.54 mL/min, eGFR was 78.93 ± 22.79 mL/min/1.73 m2 and median urinary protein excretion was 0.26 (range 0–2.75; interquartile range 0.10–0.64) g/24 h. We divided the patients into five groups based on Lee’s classification to evaluate pathologic grade. In short, age, Ccr, eGFR, urinary protein excretion and interstitial fibrotic area showed significant differences with the progression of pathologic grade, whereas BMI, SBP and DBP did not differ with grade (Table 1).
Expression of 8-OHdG in IgAN patients at different grades
8-OHdG staining, a marker of oxidative DNA damage, was carried out to investigate its association with renal fibrosis. Expression of 8-OHdG increased with the deterioration of tissue grade. In the low-grade groups, positive staining was mainly observed in the nuclei of the glomerulus and some tubules. With progression of pathologic grade, the 8-OHdG-positive area increased in the interstitium and tubular cytoplasm (Fig. 1a). 8-OHdG-positive cells were observed in low grades and their expression remarkably increased in grades III, IV and V (Fig. 1b).
Expression of 8-OHdG, p16 and Klotho in IgAN patients with deterioration of Lee’s pathologic grade. Representative photomicrographs of immunostaining show typical expression of 8-OHdG, p16 and Klotho in pathologic grades I, III, and V (a) Original magnification ×200. Quantification of 8-OHdG- (b), p16- (c) and Klotho-positive (d) areas are presented in each grade of IgAN. Values are expressed as mean ± SD. *P < 0.05 by ANOVA with Tukey’s post hoc test
Expression of p16 in IgAN patients at different grades
Immunohistochemical analysis of p16 was performed to detect cell cycle-arrested cells. In patients with IgAN, along with the deterioration of the tissue, the expression of p16 significantly increased. In low-grade IgAN patients, p16-positive staining of nuclei was seen in some tubules and glomeruli, but not in the interstitium, whereas positive staining was seen in parts of the cytoplasm of renal tubules and interstitium in patients with grades III, IV and V (Fig. 1a). Expression of p16 in patients with grades IV and V showed significant upregulation compared with that in patients with grade III or less (Fig. 1c).
Expression of Klotho in IgAN patients at different grades
Although Klotho shows renoprotective effects against various insults in experimental models, Klotho expression in biopsy samples of IgAN patients has not been analyzed. Immunostaining showed that Klotho was expressed in the cytoplasm of tubular cells in patients with low-grade disease. Expression decreased as the disease progressed (Fig. 1a). Mean expression of Klotho showed a phased decrease in the progression of pathologic damage (Fig. 1d).
Relationship between the levels of 8-OHdG, p16 and Klotho and the changes in pathologic variables of the Oxford classification
We investigated expression of 8-OHdG, p16 and Klotho and their relationship to pathologic variables of the Oxford classification. With respect to the mesangial hypercellularity, the staining areas of 8-OHdG and p16 in M1 showed significant upregulation compared with those in M0 (Fig. 2a). In terms of segmental glomerulosclerosis, expression of 8-OHdG and p16 showed significant differences between S0 and S1 (Fig. 2b). With regard to tubular atrophy and interstitial fibrosis scores, the expression of p16 increased in T2 compared with T0 or T1 (Fig. 2c), whereas the expression of Klotho in T1 or T2 was decreased compared with T0.
Expression of 8-OHdG, p16 and Klotho in IgAN patients with changes in pathologic variables of the Oxford classification. Data show positive areas of 8-OHdG (white bars), p16 (slash bars) and Klotho (black bars) with progression of pathologic scores of mesangial hypercellularity (a), segmental glomerulosclerosis (b) and tubular atrophy/interstitial fibrosis (c). Values are expressed as means ± SD. *P < 0.05 compared with score zero by ANOVA with Tukey’s post hoc test. † P < 0.05 compared with score one by ANOVA with Tukey’s post hoc test
Correlation of MT staining with clinical parameters 8-OHdG, p16 and Klotho
For the identification of factors that showed a strong effect on interstitial fibrosis, we examined the correlation of MT and clinical parameters, 8-OHdG, p16 and Klotho. In univariate regression analysis, age (P < 0.0001), BMI (P = 0.025), SBP (P = 0.002), urinary protein excretion (P = 0.002), 8-OHdG (P = 0.031) and p16 (P < 0.0001) showed a positive correlation with the MT-positive fibrotic area. In contrast, Klotho showed a negative correlation with renal fibrosis (P < 0.0001). When these parameters were entered into a multiple regression analysis, age (P = 0.001), p16 (P = 0.016) and Klotho (P = 0.019) were independently associated with interstitial fibrosis (Table 2).
Discussion
We have demonstrated that 8-OHdG and p16 increased but Klotho decreased with the progression of pathologic damage in IgAN patients. In addition, oxidative DNA damage and cell cycle-arrested cells increased in patients with mesangial hypercellularity and segmental glomerulosclerosis, whereas cell cycle-arrested cells increased but Klotho expression decreased with the extent of tubular atrophy/interstitial fibrosis. In univariate regression analysis, age, BMI, SBP, urinary protein excretion, 8-OHdG, p16 and Klotho showed significant correlation to the MT-positive area. Next, we performed multiple regression analysis to determine the independent factors that were associated with interstitial fibrosis. We found that in addition to aging per se, the accumulation of cell cycle-arrested cells and decreased Klotho expression were associated with interstitial fibrosis in patients with IgAN. These findings suggest that age-related factors might play important roles in the development of IgAN.
The present study revealed that p16 increased with the progression of pathologic variables for both glomerular and tubulo-interstitial injury, and that accumulation of p16-positive cells was independently correlated with interstitial fibrosis. These findings indicate that p16 expression is induced by both glomerular and tubulo-interstitial injury. P16 is an inhibitor of cyclin-dependent kinases 4/6, inducing G1 cell cycle-arrest [9]. Regardless of the length of the telomeres, cell cycle arrest can occur rapidly in response to cellular stress, which is called “stress-induced cellular senescence” [8]. The cellular senescence regulated by p16 has a preferred aspect for longevity to counter injury in the short term. In fact, Terada et al. showed that forced overexpression of p16 reduced mesangial cell proliferation [24]. In the development of interstitial fibrosis, p16 knockout mice show increased fibrosis induced by unilateral ureteral obstruction (UUO), a model of acute fibrosis [25]. However, p16 expression is regulated by hypermethylation via the polycomb repressor complex, and accumulates in the tissue [9]. Because cell cycle-arrested cells are referred to as senescence-associated secretory phenotype including the release of several inflammatory cytokines [26], increased numbers of senescent cells in the kidney can be detrimental in the long term. Previous studies have reported that accumulation of cell cycle-arrested cells increases sensitivity to renal injury [8, 12] and that senescent fibroblasts promote carcinogenesis [27]. These findings raise the possibility that AKI and kidney cancer are more frequent in CKD patients.
Klotho expression showed a significant decrease in the progression of tubular atorophy/interstitial fibrosis, but not glomerular variables. Because Klotho is mainly expressed in the distal tubules, its reduction may reflect tubulo-interstitial damage but not glomerular injury. Recent studies found that after UUO, renal fibrosis intensifies in klotho gene-deficient heterozygous mice [13] and that renal fibrosis is improved by the injection of the Klotho protein [14]. Klotho is known as a multi-functional protein that inhibits signaling pathways of TGF-β1, Wnt and insulin/insulin-like growth factor-1 [10]. Among those, TGF-β1 plays an important role in the development of fibrosis. We have found that Klotho can bind to the TGF-β type II receptor, thereby inhibiting TGF-β1 signaling [14]. In addition to its anti-fibrotic effects, several studies have observed protective effects of Klotho on AKI and carcinogenesis in experimental rodent models, indicating that AKI and carcinogenesis are more likely to occur when Klotho expression is low [28, 29].
We showed a correlation between the increased immunoreactivity of 8-OHdG and the deterioration of glomerular variables. However, multivariate regression analysis did not identify that it as an independent factor that correlated with renal fibrosis. These results suggest that oxidative DNA damage increased in response to glomerular injury in IgAN patients. On the other hand, previous reports showed that oxidative DNA damage is linked to chronic fibrotic disease [11] as well as to an increased risk of developing cancer [30]. Oxidative DNA damage also occurs in normal individuals due to endogenous production of ROS by mitochondria. In fact, our data showed that 8-OHdG-positive cells were present in patients with lower pathologic grades despite higher levels occurring with progression of pathologic damage. These results suggest that oxidative DNA damage is partially involved in the development of renal fibrosis even though it does not show an independent correlation statistically.
In summary, we analyzed renal biopsy samples from patients with IgAN and examined the expression of age-related factors. We observed that 8-OHdG and p16 increased but Klotho decreased with progression of pathologic grade. Our analysis of the association between age-related factors and pathologic variables of the Oxford classification showed that oxidative DNA damage and cell cycle-arrested cells increased in patients with a deterioration of glomerular variables. In contrast, cell cycle-arrested cells increased but Klotho expression decreased with the extent of tubulo-interstitial variables. Although age, BMI, SBP, urinary protein excretion, 8-OHdG, p16 and Klotho showed significant correlation with interstitial fibrosis in univariate regression analysis, only aging, increased p16 and decreased Klotho were independently correlated with interstitial fibrosis in patients with IgAN. Because age is independently correlated with interstitial fibrosis, age-related factors were incompletely characterized. However, accumulation of cell cycle-arrested cells and decreased Klotho expression in the kidneys likely participate in the development of interstitial fibrosis in IgAN patients. These findings suggest that age-related factors might play important roles during the development of renal damage in patients with IgAN.
References
Jha V, Garcia-Garcia G, Iseki K, et al. Chronic kidney disease: global dimension and perspectives. Lancet. 2013;382:260–72.
Coresh J, Selvin E, Stevens LA, et al. Prevalence of chronic kidney disease in the United States. JAMA. 2007;298:2038–47.
Hsu RK, Hsu CY. Proteinuria and reduced glomerular filtration rate as risk factors for acute kidney injury. Curr Opin Nephrol Hypertens. 2011;20:211–7.
Klatte T, Marberger M. Renal cell carcinoma of native kidneys in renal transplant patients. Curr Opin Urol. 2011;21:376–9.
Anderson S, Eldadah B, Halter JB, et al. Acute kidney injury in older adults. J Am Soc Nephrol. 2011;22:28–38.
Liu Y. Renal fibrosis: new insights into the pathogenesis and therapeutics. Kidney Int. 2006;69:213–7.
Rule AD, Amer H, Cornell LD, et al. The association between age and nephrosclerosis on renal biopsy among healthy adults. Ann Intern Med. 2010;152:561–7.
Yang H, Fogo AB. Cell senescence in the aging kidney. J Am Soc Nephrol. 2010;21:1436–9.
Collado M, Blasco MA, Serrano M. Cellular senescence in cancer and aging. Cell. 2007;130:223–33.
Kuro-o M. Klotho and aging. Biochim Biophys Acta. 2009;1790:1049–58.
Pat B, Yang T, Kong C, et al. Activation of ERK in renal fibrosis after unilateral ureteral obstruction: modulation by antioxidants. Kidney Int. 2005;67:931–43.
Yang L, Besschetnova TY, Brooks CR, et al. Epithelial cell cycle arrest in G2/M mediates kidney fibrosis after injury. Nat Med. 2010;16:535–43.
Sugiura H, Yoshida T, Shiohira S, et al. Reduced Klotho expression level in kidney aggravates renal interstitial fibrosis. Am J Physiol Renal Physiol. 2012;302:F1252–64.
Doi S, Zou Y, Togao O, et al. Klotho inhibits transforming growth factor-beta1 (TGF-beta1) signaling and suppresses renal fibrosis and cancer metastasis in mice. J Biol Chem. 2011;286:8655–65.
Sugiyama H, Yokoyama H, Sato H, et al. Japan renal biopsy registry and japan kidney disease registry: Committee Report for 2009 and 2010. Clin Exp Nephrol. 2013;17:155–73.
Koyama A, Igarashi M, Kobayashi M. Natural history and risk factors for immunoglobulin A nephropathy in Japan. Am J Kidney Dis. 1997;29:526–32.
Lee SM, Rao VM, Franklin WA, et al. IgA nephropathy: morphologic predictors of progressive renal disease. Hum Pathol. 1982;13:314–22.
Lee HS, Lee MS, Lee SM, et al. Histological grading of IgA nephropathy predicting renal outcome: revisiting H. S. Lee’s glomerular grading system. Nephrol Dial Transplant. 2005;20:342–8.
Cattran DC, Coppo R, Cook HT, et al. The Oxford classification of IgA nephropathy: rationale, clinicopathological correlations, and classification. Kidney Int. 2009;76:534–45.
Alamartine E, Sauron C, Laurent B, et al. The use of the Oxford classification of IgA nephropathy to predict renal survival. Clin J Am Soc Nephrol. 2011;6:2384–8.
Bonnet F, Deprele C, Sassolas A, et al. Excessive body weight as a new independent risk factor for clinical and pathological progression in primary IgA nephritis. Am J Kidney Dis. 2001;37:720–7.
Berthoux F, Mohey H, Laurent B, et al. Predicting the risk for dialysis or death in IgA nephropathy. J Am Soc Nephrol. 2011;22:752–61.
Roberts IS, Cook HT, Troyanov S, et al. The Oxford classification of IgA nephropathy: pathology definitions, correlations, and reproducibility. Kidney Int. 2009;76:546–56.
Terada Y, Yamada T, Nakashima O, et al. Overexpression of cell cycle inhibitors (p16INK4 and p21Cip1) and cyclin D1 using adenovirus vectors regulates proliferation of rat mesangial cells. J Am Soc Nephrol. 1997;8:51–60.
Wolstein JM, Lee DH, Michaud J, et al. INK4a knockout mice exhibit increased fibrosis under normal conditions and in response to unilateral ureteral obstruction. Am J Physiol Renal Physiol. 2010;299:F1486–95.
Rodier F, Campisi J. Four faces of cellular senescence. J Cell Biol. 2011;192:547–56.
Parrinello S, Coppe JP, Krtolica A, et al. Stromal-epithelial interactions in aging and cancer: senescent fibroblasts alter epithelial cell differentiation. J Cell Sci. 2005;118:485–96.
Hu MC, Shi M, Zhang J, et al. Klotho deficiency is an early biomarker of renal ischemia-reperfusion injury and its replacement is protective. Kidney Int. 2010;78:1240–51.
Zhu Y, Xu L, Zhang J, et al. Klotho suppresses tumor progression via inhibiting PI3K/Akt/GSK3β/Snail signaling in renal cell carcinoma. Cancer Sci. 2013;104:663–71.
Miyake H, Hara I, Kamidono S, et al. Prognostic significance of oxidative DNA damage evaluated by 8-hydroxy-2’-deoxyguanosine in patients undergoing radical nephrectomy for renal cell carcinoma. Urology. 2004;64:1057–61.
Acknowledgments
This work was supported by Tsuchiya Memorial Medical Foundation (to S.D.), and Ryokufukai Medical Foundation (to K.K.)
Conflict of interest
All authors have declared that no conflict of interest exists.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Yamada, K., Doi, S., Nakashima, A. et al. Expression of age-related factors during the development of renal damage in patients with IgA nephropathy. Clin Exp Nephrol 19, 830–837 (2015). https://doi.org/10.1007/s10157-014-1070-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-014-1070-2