Abstract
This study was a pharmacokinetic (PK)–pharmacodynamic (PD) target attainment analysis of meropenem in Japanese adult patients. Plasma drug concentration data (265 samples from 42 patients) were used for population PK modeling and Monte Carlo simulation to assess the probability of attaining the PK–PD target (40% of the time above the MIC for the bacterium). The final population PK model identified creatinine clearance (Clcr, ml/min) and body weight (BW, kg) as the most significant covariates: Cl (l/h) = 0.0905 × Clcr + 2.03, V c (l) = 0.199 × BW, Q (l/h) = 4.02, and V p (l) = 4.55, where Cl is the clearance, V c and V p are the volumes of distribution of the central and peripheral compartments, respectively, and Q is the intercompartmental clearance. The Monte Carlo simulation developed the PK–PD breakpoints (the highest MIC values at which the probabilities of target attainment in plasma are 80% or more) for meropenem regimens, the values of which varied with the Clcr and BW of the patient. The simulation also demonstrated that 0.25 g every 12 h (0.5-h infusion) achieved a target attainment probability of 82.4–100% against Escherichia coli, methicillin-susceptible Staphylococcus aureus, Haemophilus influenzae, and Streptococcus pneumoniae isolates. However, against Pseudomonas aeruginosa isolates, 0.5 g every 8 h or 1 g every 8 h was required to achieve 80% or more probability in most typical patients. These results provide a PK–PD-based strategy for tailoring a meropenem regimen according to Clcr and BW of a Japanese adult patient and susceptibility of the causative bacteria.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Meropenem is a commonly used carbapenem for the treatment of various infections such as pneumonia, sepsis, urinary-tract infections, and intra-abdominal infections in adult patients [1]. The approved regimen for intravenous meropenem in Japan is 0.5–2 g daily in two to three divided doses. Antibacterial regimens should be tailored and optimized on a case-by-case basis to maximize the agent’s microbiological effects and clinical outcomes, and potentially provide a cost-effective medical benefit. However, information is limited on choosing the appropriate meropenem dosage for Japanese adult patients. This choice necessitates actively considering such factors as patient characteristics and susceptibility to meropenem of the bacteria involved.
Integration of pharmacokinetic (PK) and pharmacodynamic (PD) targets derived from both PK data and exposure–response data can be utilized to support antibacterial dosage choice and optimize the dosing regimen. This PK–PD target attainment analysis [2, 3], particularly using a statistical technique called the Monte Carlo simulation, has also been applied to meropenem. However, earlier analyses [4–9] had several problems. Drug concentration data were obtained from a small number of healthy subjects. In the Monte Carlo simulations, the mean ± standard deviations of individual pharmacokinetic parameters (the standard two-stage method) were used, although the method yields a large bias toward their interindividual variability [10]. Moreover, covariates to affect the drug pharmacokinetics were ignored. For an appropriate PK–PD target attainment analysis of meropenem, it is necessary to use the mean population PK parameters, their variability, and potential covariates in adult patients.
The aim of this study was thus to perform a PK–PD target attainment analysis of meropenem in Japanese adult patients. We first developed a population PK model to accurately describe the drug disposition in adult patients. Incorporating the developed model into a Monte Carlo simulation, we then estimated the probabilities of target attainment for meropenem regimens and assessed their expected population probabilities against the MIC distributions for common bacterial isolates.
Patients, materials, and methods
Study subjects
This study was approved by the ethics committees of the study institutes and conducted in compliance with the Declaration of Helsinki, and all subjects provided written informed consent. Forty-two Japanese adults (including febrile neutropenic patients, surgical patients, and patients with pneumonia or urinary-tract infections) received 0.25, 0.5, or 1 g meropenem (0.5- or 1-h infusion) every 8 or 12 h. Four to ten samples of blood were drawn in heparinized tubes. After centrifugation, each plasma sample was removed, stabilized with an equal volume of 1 mol/l MOPS buffer (pH 7.0), and frozen until assay. Demographic and physiopathological parameter data, such as sex, age, body weight, blood urea nitrogen, serum creatinine, and creatinine clearance, were recorded for all subjects.
Meropenem assay
The total concentrations of meropenem in plasma were determined using our high-performance liquid chromatography method, as reported previously [11]. In brief, plasma sample (400 µl) was transferred to an ultrafiltration device and centrifuged. Then, the filtered solution (20 µl) was injected onto a chromatograph with a C18 column at 40°C and an ultraviolet absorbance detector at 300 nm. The mobile phase was a mixture of 10 mM phosphate buffer (pH 7.4) and acetonitrile (90:10). The limit of quantification was 0.05 µg/ml, the accuracy was 97.7–106.3%, and the precision was <7.2%.
Population pharmacokinetic (PK) modeling
Population PK modeling was performed using the first-order conditional estimation (FOCE) method in the NONMEM program (version 6.2.0; ICON Development Solutions, Ellicott, MD, USA). Both one- and two-compartment models were fitted to the data when choosing the basic structural PK model. Model discrimination was assessed using Akaike information criterion (AIC) values. The interindividual variability was modeled exponentially:
where θ i is the fixed-effects parameter for the ith subject, θ is the mean value of the fixed-effects parameter in the population, and η is a random interindividual variable, which is normally distributed with mean 0 and variance ω 2. The residual (intraindividual) variability was modeled with a proportional error model:
where C obs,ij and C pred,ij denote the jth observed and predicted concentrations for the ith subject, and ε is a random intraindividual error which is normally distributed with mean 0 and variance σ 2.
The influences of the patient characteristics on the individual PK parameters obtained from the basic structural model were explored graphically. The covariates showing a correlation with the PK parameters were introduced into the model. The significance of the influence of the covariates was evaluated by the changes of −2 log likelihood (the minimum value of the objective function: OBJ). An OBJ decrease of more than 3.84 from the basic structural model (P < 0.05; χ 2 test) was considered statistically significant during the forward inclusion process. The full model was built by incorporating the significant covariates, and the final model was developed by a backward elimination method. The covariates in the full model were excluded from the model one at a time, and an OBJ increase of more than 6.63 from the full model (P < 0.01; χ 2 test) was considered statistically significant. Goodness of fit was evaluated by checking the plots of observed, predicted, and individual predicted concentrations, and weighted residual.
A nonparametric bootstrap resampling technique was performed to validate the reliability and stability of the population PK model developed. The program Wings for NONMEM (version 612; Holford NH, University of Auckland, Auckland, New Zealand) was used to create resampled new data sets. The 95% confidence intervals of PK parameters from 1,000 bootstrap replicates were compared with the estimates of the final model.
Microbiological data
Five common types of pathogenic bacteria were selected, and the MIC distribution data of their clinical isolates were derived from recent susceptibility surveillance in Japan, including the study institutes: [12] Pseudomonas aeruginosa (n = 322 isolates; range 0.06–128 µg/ml; MIC50 = 1 µg/ml; MIC90 = 16 µg/ml), Haemophilus influenzae (n = 252; range 0.015–2 µg/ml; MIC50 = 0.12 µg/ml; MIC90 = 0.5 µg/ml), Streptococcus pneumoniae (n = 181; range 0.06–1 µg/ml; MIC50 = 0.06 µg/ml; MIC90 = 0.5 µg/ml), Escherichia coli (n = 141; range 0.03–0.06 µg/ml; MIC50 = 0.03 µg/ml; MIC90 = 0.03 µg/ml), and methicillin-susceptible Staphylococcus aureus (MSSA) (n = 58; range 0.06–0.12 µg/ml; MIC50 = 0.12 µg/ml; MIC90 = 0.12 µg/ml).
Probability of target attainment analysis using a Monte Carlo simulation
A Monte Carlo simulation was conducted using the final population PK model to estimate the probability-of-target-attainment profile for each meropenem regimen (0.5-h infusion)–MIC combination. The following process was repeated 10,000 times with Crystal Ball 2000 software (Oracle, Redwood Shores, CA, USA). A set of fixed-effects parameters was generated randomly according to each mean estimate (θ) and interindividual variance (ω) of the final population PK model. The steady-state unbound drug concentration versus time curve was simulated using the fixed-effects parameters, where a value of 2.4% protein binding in humans [13] was employed. The time point at which the free drug concentration coincided with a specific MIC value was determined, and the time for which the free drug concentration remained above the MIC (fT > MIC) was finally calculated as the cumulative percentage of a 24-h period [14]. The probability of target attainment (%) was determined as the fraction that achieved at least 40% fT > MIC (the bactericidal target [1, 6, 8, 9, 15–17]) of 10,000 estimates.
For each meropenem regimen, the highest MIC at which the probability of target attainment achieved 80% or more probability was defined as the PK–PD breakpoint (µg/ml) [18]. For each bacterium, the probability at a specific MIC was multiplied by the fraction of the population of bacterium in each MIC category, and the sum of individual products was defined as the expected population probability of target attainment (%) [14].
Results
The demographic and physiopathological parameters of the study subjects (26 men and 16 women) were as follows: age 62.2 ± 19.6 years (mean ± SD) (range 23.0–88.0 years); body weight 56.0 ± 10.4 kg (38.5–84.6 kg); blood urea nitrogen 15.5 ± 7.2 mg/dl (5.8–36.1 mg/dl); serum creatinine 0.87 ± 0.41 mg/dl (0.46–2.30 mg/dl); and creatinine clearance (Clcr) 77.7 ± 32.3 ml/min (15.5–137.7 ml/min). A total of 265 plasma drug concentration data (Fig. 1) were used for the population PK modeling.
Because AIC values indicated that the two-compartment model (AIC, 516) described the data better than the one-compartment model (AIC, 763), the two-compartment model was chosen as the basic structural model. Therefore, the PK parameters were clearance (Cl, l/h), volume of distribution of the central compartment (V c, l), intercompartmental clearance (Q, l/h), and volume of distribution of the peripheral compartment (V p, l).
As the scatter plots (Fig. 1) showed that the drug elimination was slower in patient group with Clcr of <50 ml/min than in patient group with Clcr of >100 ml/min, incorporation of creatinine clearance (Clcr) into Cl caused the largest OBJ change (∆OBJ, −40.8) in the forward inclusion process to build the covariate model. Age and body weight (BW) each also had a significant effect on Cl, but neither of them was additionally incorporated into Cl to avoid a collinearity effect, because age and BW each showed a high correlation with Clcr. Meanwhile, incorporation of BW into V c caused the largest OBJ change (∆OBJ, −17.6). However, none of the examined covariates had a significant effect on V p and Q. During the backward deletion process, every covariate and coefficient remained in the model, causing significant OBJ increase. Therefore, the final model was as follows:
The mean and variability of the final population PK parameters and 95% confidence interval estimated from bootstrap replicates are summarized in Table 1. Diagnostic plots indicated that the final model accurately reflected the data (Fig. 2).
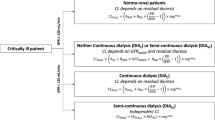
Based on the final model, four typical patients were supposed with Clcr (50 or 100 ml/min) and BW (40 or 80 kg) combinations. Figure 3 illustrates the influences of Clcr–BW combinations on meropenem pharmacokinetics and pharmacodynamics. Given a 0.5-h infusion of 0.5 g meropenem and MIC = 4 µg/ml, the mean values of fT > MIC (percentage of an 8-h period) were: 30.7% in patient A (Cl = 11.1 l/h and V c = 7.96 l given in Table 1); 40.8% in patient B (Cl = 11.1 l/h, V c = 15.9 l); 55.3% in patient C (Cl = 6.56 l/h, V c = 7.96 l); and 70.5% in patient D (Cl = 6.56 l/h, V c = 15.9 l).
Simulation curves in four typical patients (a–d) after a 0.5-h infusion of 0.5 g meropenem. Each simulation curve was drawn using the mean fixed-effects parameters given in Table 1. The dotted line represents 4 µg/ml. Clcr creatinine clearance; BW body weight
Consequently, the probability of target attainment versus MIC profiles (Fig. 4) and the PK-PD breakpoints (Table 2) for meropenem regimens were changed by Clcr and BW. In the case of 0.5 g every 8 h, the BW increase from patient A (40 kg) to patient B (80 kg) raised the PK–PD breakpoint from 1 to 2 µg/ml, and then the Clcr decrease from patient B (100 ml/min) to patient D (50 ml/min) raised the PK–PD breakpoint from 2 to 4 µg/ml.
Table 3 shows the expected population probabilities of target attainment against common pathogenic bacteria. In all patients, the probability values for 0.25 g every 12 h were >82% against E. coli, MSSA, H. influenzae, and S. pneumoniae isolates. However, the values were lower against P. aeruginosa isolates. The minimum regimens required to achieve 80% or more probability were 0.5 g every 8 h for patients C and D, and 1 g every 8 h for patient B.
Discussion
The population PK model developed for meropenem in Japanese adult patients identified Clcr and BW as the most significant covariates affecting the pharmacokinetics. Based on the developed model, the Monte Carlo simulation determined the PK–PD breakpoints for meropenem regimens, the MIC values of which varied with the Clcr and BW of the patient. The simulation also demonstrated that 0.25 g every 12 h (0.5-h infusion) achieved a target attainment probability of >82% against E. coli, MSSA, H. influenzae, and S. pneumoniae isolates. However, against P. aeruginosa isolates, 0.5 g every 8 h or 1 g every 8 h was required to achieve 80% or more probability in most typical patients.
Earlier PK studies of meropenem found that meropenem followed a two-compartment model [19, 20]: the drug was eliminated renally with a 12-h urinary recovery of 62.2–78.2% [19, 21], and the drug clearance was lowered according to the degree of renal dysfunction [22, 23]. In earlier population PK analyses, body weight was the most significant covariate affecting volume of distribution in both Caucasian adult patients [16] and Korean febrile neutropenic patients [17]. The results of the population PK modeling (Table 1) are consistent with these earlier findings. The two-compartment model described the current data better than did the one-compartment model. Although age often plays an important role in pharmacokinetics, renal function (Clcr) had a more direct effect than age on meropenem pharmacokinetics. The mean renal clearance was estimated as 77.6% of the total clearance [(0.0905 × Clcr)/(0.0905 × Clcr + 2.03) using the mean Clcr of 77.7 ml/min].
The final population PK model lacked bias, regardless of the drug concentration (Fig. 2c) and time (Fig. 2d), and the observed drug concentration was almost identical to the individual predicted concentration after the Bayesian step (Fig. 2b). In addition, all relative standard error (standard error/estimate, %) values via the covariance step in the NONMEM modeling were <48%, and all parameter estimates were in the range of the 95% confidence interval using the bootstrap method (Table 1), indicating the reliability and stability of the final model. Therefore, we consider the final model to have a good predictive performance for PK–PD assessment use.
The Monte Carlo simulation demonstrated that the probabilities of target attainment for 0.25 g every 8 h (0.75 g/day) and 0.5 g every 8 h (1.5 g/day) were comparable to those for 0.5 g every 12 h (1 g/day) and 1 g every 12 h (2 g/day), respectively (Fig. 4), suggesting that the dosing interval is a more important point than the daily dose in the dosing strategy for meropenem, which exhibits time-dependent killing. From the viewpoint of cost-effective benefit, every 8 h regimens would be preferable to every 12 h regimens, unless frequent administration is unacceptable due to the increase in the patient’s burden and the medical workload.
The differences in the PK–PD target attainment among the bacteria resulted from their varying specific susceptibilities to meropenem (Table 3). A regimen of 0.25 g every 12 h would be sufficient against high-susceptibility bacteria such as E. coli, MSSA, H. influenzae, and S. pneumoniae (MIC90 ≤ 0.5 µg/ml). However, when there is a suspicion of infection with meropenem-resistant bacteria such as P. aeruginosa (MIC90 = 16 µg/ml), we recommend 0.5 g every 8 h to a patient with low Clcr and 1 g every 8 h to a patient with high Clcr, although 1 g every 8 h is higher than the maximal 2 g/day in Japan (but the dosage is equal to 3 g/day for intra-abdominal infections [24] and is within 6 g/day for bacterial meningitis [25] in other countries). Otherwise, when the MIC of the patient’s causative pathogen including P. aeruginosa is determined, the newly developed PK–PD breakpoints (Table 2) can help us to choose a more appropriate meropenem regimen based on the MIC value.
In an effort to provide an overview of the population pharmacokinetics and pharmacodynamics of meropenem in adult patients, the analysis employed only four typical patients and five common pathogenic bacteria. However, we can estimate the PK parameters of a patient from their Clcr and BW values (Table 1), and the probability of target attainment versus MIC profiles (Fig. 4) can be useful when the MIC value for a bacterium is given, regardless of its susceptibility pattern.
In conclusion, Clcr and BW were the most significant factors affecting the population pharmacokinetics of meropenem in Japanese adult patients, and consequently the PK–PD breakpoints for meropenem regimens varied with the Clcr and BW of the patient. A regimen of 0.25 g every 12 h (0.5-h infusion) achieved a target attainment probability of >82% against E. coli, MSSA, H. influenzae, and S. pneumoniae isolates. However, against P. aeruginosa isolates, 0.5 g every 8 h or 1 g every 8 h was required to achieve a high probability. The results of the analysis are considered to provide a PK–PD-based strategy for tailoring a meropenem regimen according to the Clcr and BW of a Japanese adult patient and susceptibility of the causative bacteria (suspected because of the patient’s symptoms or identified with the MIC data). The implications of our findings and proposals need to be confirmed in clinical settings.
References
Nicolau DP. Pharmacokinetic and pharmacodynamic properties of meropenem. Clin Infect Dis. 2008;47(Suppl 1):S32–40.
Ikawa K, Morikawa N, Ikeda K, Ohge H, Sueda T, Suyama H, et al. Pharmacokinetic-pharmacodynamic target attainment analysis of biapenem in adult patients: a dosing strategy. Chemotherapy. 2008;54:386–94.
Ikawa K, Morikawa N, Uehara S, Monden K, Yamada Y, Honda N, et al. Pharmacokinetic-pharmacodynamic target attainment analysis of doripenem in infected patients. Int J Antimicrob Agents. 2009;33:276–9.
Mikamo H, Totsuka K. The comparison of optimized pharmacodynamic dosing strategy for meropenem using Monte Carlo simulation (in Japanese). Jpn J Antibiot. 2005;58:159–67.
Mikamo H, Tanaka K, Watanabe K. Efficacy of injectable carbapenems for respiratory infections caused by Streptococcus pneumoniae and Haemophilus influenzae with Monte Carlo simulation (in Japanese). Jpn J Antibiot. 2007;60:47–57.
Sumitani Y, Kobayashi Y. Analysis on the effective dosage regimens for meropenem, biapenem and doripenem against P. aeruginosa infection based on pharmacokinetics and pharmacodynamics theory (in Japanese). Jpn J Antibiot. 2007;60:394–403.
Watanabe A, Fujimura S, Kikuchi T, Gomi K, Fuse K, Nukiwa T. Evaluation of dosing designs of carbapenems for severe respiratory infection using Monte Carlo simulation. J Infect Chemother. 2007;13:332–40.
Nagasawa Z, Kusaba K, Aoki Y. Susceptibility of clinical isolates of Pseudomonas aeruginosa in the Northern Kyushu district of Japan to carbapenem antibiotics, determined by an integrated concentration method: evaluation of the method based on Monte Carlo simulation. J Infect Chemother. 2008;14:238–43.
Nakamura T, Shimizu C, Kasahara M, Okuda K, Nakata C, Fujimoto H, et al. Monte Carlo simulation for evaluation of the efficacy of carbapenems and new quinolones against ESBL-producing Escherichia coli. J Infect Chemother. 2009;15:13–7.
Sheiner BL, Beal SL. Evaluation of methods for estimating population pharmacokinetic parameters. II. Biexponential model and experimental pharmacokinetic data. J Pharmacokinet Biopharm. 1981;9:635–51.
Ikeda K, Ikawa K, Morikawa N, Miki M, Nishimura S, Kobayashi M. High-performance liquid chromatography with ultraviolet detection for real-time therapeutic drug monitoring of meropenem in plasma. J Chromatogr B Analyt Technol Biomed Life Sci. 2007;856:371–5.
Yamaguchi K, Ishii Y, Iwata M, Watanabe N, Uehara N, Yasujima M, et al. Nationwide surveillance of parenteral antibiotics containing meropenem activities against clinically isolated strains in 2006 (in Japanese). Jpn J Antibiot. 2007;60:344–77.
Iba K, Yoshitake A. Pharmacokinetics of [14C]meropenem in dogs and monkeys (in Japanese). Jpn J Chemother. 1992;40(Suppl 1):145–53.
Mouton JW, Dudley MN, Cars O, Derendorf H, Drusano GL. Standardization of pharmacokinetic/pharmacodynamic (PK/PD) terminology for anti-infective drugs: an update. J Antimicrob Chemother. 2005;55:601–7.
Mikamo H, Yamagishi Y, Tanaka K, Watanabe K. Clinical investigation on target value of T > MIC in carbapenems (in Japanese). Jpn J Antibiot. 2008;61:73–81.
Li C, Kuti JL, Nightingale CH, Nicolau DP. Population pharmacokinetic analysis and dosing regimen optimization of meropenem in adult patients. J Clin Pharmacol. 2006;46:1171–8.
Lee DG, Choi SM, Shin WS, Lah HO, Yim DS. Population pharmacokinetics of meropenem in febrile neutropenic patients in Korea. Int J Antimicrob Agents. 2006;28:333–9.
Ikawa K, Morikawa N, Ikeda K, Ohge H, Sueda T. Development of breakpoints of cephems for intraabdominal infections based on pharmacokinetics and pharmacodynamics in the peritoneal fluid of patients. J Infect Chemother. 2008;14:141–6.
Nakashima M, Uematsu T, Kanamaru M, Ueno K. Clinical phase I study of meropenem (in Japanese). Jpn J Chemother. 1992;40(Suppl 1):258–75.
Mouton JW, van den Anker JN. Meropenem clinical pharmacokinetics. Clin Pharmacokinet. 1995;28:275–86.
Burman LA, Nilsson-Ehle I, Hutchison M, Haworth SJ, Norrby SR. Pharmacokinetics of meropenem and its metabolite ICI 213, 689 in healthy subjects with known renal metabolism of imipenem. J Antimicrob Chemother. 1991;27:219–24.
Ohkawa M, Tokunaga S, Hisazumi H. Effect of renal function on the pharmacokinetics of meropenem (in Japanese). Jpn J Chemother. 1992;40(Suppl 1):764–7.
Chimata M, Nagase M, Suzuki Y, Shimomura M, Kakuta S. Pharmacokinetics of meropenem in patients with various degrees of renal function, including patients with end-stage renal disease. Antimicrob Agents Chemother. 1993;37:229–33.
Tellado JM, Wilson SE. Empiric treatment of nosocomial intra-abdominal infections: a focus on the carbapenems. Surg Infect (Larchmt). 2005;6:329–43.
Tunkel AR, Hartman BJ, Kaplan SL, Kaufman BA, Roos KL, Scheld WM, et al. Practice guidelines for the management of bacterial meningitis. Clin Infect Dis. 2004;39:1267–84.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Ikawa, K., Morikawa, N., Ohge, H. et al. Pharmacokinetic–pharmacodynamic target attainment analysis of meropenem in Japanese adult patients. J Infect Chemother 16, 25–32 (2010). https://doi.org/10.1007/s10156-009-0022-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10156-009-0022-3