Abstract
Purpose
Patients admitted to intensive care unit (ICU) with Klebsiella pneumoniae infections are characterized by high mortality. The aims of the present study were to investigate the population pharmacokinetics parameters and to assess the probability of target attainment of meropenem in critically ill patients to provide information for more effective regimens.
Methods
Twenty-seven consecutive patients were included in the study. Meropenem was administered as 3-h intravenous (i.v.) infusions at doses of 1–2 g every 8 or 12 h. Meropenem plasma concentrations were measured by a high-performance liquid chromatography (HPLC) method, and a population pharmacokinetics analysis was performed using NONMEM software. Meropenem plasma disposition was simulated for extended (3 h; 5 h) or continuous i.v. infusions, and the following parameters were calculated: time during which free drug concentrations were above minimum inhibitory concentration (MIC) (fT > MIC), free minimum plasma concentrations above 4× MIC (fCmin > 4× MIC), probability of target attainment (PTA), and cumulative fraction of response (CFR).
Results
Gender and severity of sepsis affected meropenem clearance, whose typical population values ranged from 6.22 up to 12.04 L/h (mean ± standard deviation (SD) value, 9.38 ± 4.47 L/h). Mean C min value was 7.90 ± 7.91 mg/L, suggesting a high interindividual variability. The simulation confirmed that 88 and 97.5 % of patients achieved effective C min > 4× MIC values after 3- and 5-h i.v. infusions of meropenem 2 g × 3/day, respectively. On the contrary, the same total daily doses reached the target C min > 4× MIC values in 100 % of patients when administered as continuous i.v. infusions.
Conclusions
Several factors may influence meropenem pharmacokinetics in ICU patients. Continuous i.v. infusions of meropenem seem to be more effective than standard regimens to achieve optimal therapeutic targets.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The development of infections in critically ill patients is a dramatic problem since mortality and morbidity rates remain high. Moreover, the antibiotic therapy may not be always effective, because pathophysiological changes associated with the course of the disease may often alter drug pharmacokinetics [1, 2].
Meropenem is a broad-spectrum beta-lactam antibiotic widely used for the treatment of nosocomial infections, due to its rapid and good distribution in most body tissues and fluids [3, 4]. From a pharmacokinetic/pharmacodynamic (PK/PD) point of view, meropenem is a time-dependent antibacterial drug, whose efficacy is predicted by the time during which the free drug plasma concentration is maintained above the minimum inhibitory concentration (MIC) between two consecutive doses (fT > MIC) [5–8]. To ensure a bactericidal effect, the fT > MIC should be higher than 40 % [9]. Furthermore, efficacy may be anticipated by the minimum plasma concentration (C min) targeted to values at least four times the MIC value (C min > 4× MIC) [10].
Previous studies suggest that the pharmacokinetics of meropenem in critically ill patients differs to healthy volunteers [1]. In fact, pathophysiological changes in patients admitted to intensive care units (ICUs) have a profound effect on both volume of distribution (V) and clearance (Cl) of meropenem [11], thus reducing the percentage of patients who may reach the PK/PD target values associated with a therapeutic benefit. Therefore, a TDM-guided antimicrobial therapy may minimize pharmacokinetic variability and maximize therapeutic benefits. Such a strategy may spare critically ill patients from therapeutic failures due to the unpredictable pharmacokinetics and prevent the occurrence of resistance due to suboptimal dosages [12, 13]. In addition, the development of a meropenem population pharmacokinetic (POP/PK) model in critically ill patients may be considered a rational approach to optimize individual dosing regimens [14, 15].
The main aims of the present study were (1) to develop a POP/PK model of meropenem in patients admitted to ICU and (2) to define a PK/PD target attainment (PTA) for different administration schedules.
Patients and methods
Patients and anti-infective treatment
The present study was a prospective, monocentric trial, conducted at the IRCCS AOU San Martino-IST Hospital, Genoa, Italy. The study consecutively enrolled patients with sepsis, severe sepsis, or septic shock (according to the definitions of the American College of Critical Care Medicine Consensus Conference Committee - 2001 SCCM/ESICM/ACCP/ATS/SIS) [16], admitted to the ICU wards. Inclusion criteria were as follows: patients admitted to ICUs who developed a Klebsiella pneumoniae (KP) nosocomial infection treated with meropenem alone or in combination depending on the resistance profile of the bacterial strain, meropenem administration for at least 2 days, and bacteremia confirmed by at least one positive blood culture. Patients undergoing dialysis procedures were excluded. The study was approved by the Ethics Committee of the IRCCS AOU San Martino-IST Hospital, and a signed informed consent from patients or their relatives was obtained before enrolment, according to local regulations and Ethics Committee recommendations.
Individual meropenem dose was decided by infectivologists on the basis of clinical indications, infection severity, and sensitivity of bacterial strain. The Vitek 2 automated system (bioMérieux, Marcy L’Etoile, France) was used for identification and antimicrobial susceptibility testing of bacterial strain; minimum inhibitory concentrations (MICs) were classified according to established breakpoints by Performance Standards for Antimicrobial Susceptibility Testing: Twenty-second Informational Supplement (Clinical and Laboratory Standards Institute [CLSI] M100-S22) [17]. Patients received conventional dosing of meropenem (1 or 2 g) as an intravenous 3-h infusion two or three times a day. Further dose adjustment was considered in enrolled patients according to creatinine clearance when required and under the supervision of the infectivologists.
Pharmacokinetic sampling and concentrations analysis
Meropenem plasma concentrations were determined for each patient, after at least three completed infusions of the drug (second day); blood samples were collected according to the following scheme: immediately after the end of infusion; 1, 3, and 5 h after the end of infusion; and immediately before the next administration of meropenem. For each sample, an aliquot of 4 mL of blood was drawn into heparinized tubes, which were centrifuged at 1000g for 10 min, and the resulting plasma was stored at −80 °C. Sample analysis was performed at the Clinical Pharmacology and Toxicology Unit, University of Genoa.
Meropenem plasma concentrations were determined with a validated high-performance liquid chromatography (HPLC) method previously described by Legrand et al. [18], with minor modifications (see Supplementary Material).
The calibration curves of peak areas vs. meropenem concentrations were linear from 0.5 up to 100 mg/L, giving a correlation coefficient r 2 = 0.999. The results, as far as precision and accuracy, are concerned, are derived from the measured concentrations of the validation samples, and were acceptable according to The International Conference on Harmonisation (ICH) Harmonised Tripartite Guideline Q2(R1) and Washington criteria [19, 20].
Population pharmacokinetic analysis
Pharmacokinetic analysis of meropenem plasma concentrations was performed according to a non-linear mixed-effects modeling approach using NONMEM version 7.2 software [21], together with PsN and Xpose4 packages [22, 23]. All concentration values were adjusted to their respective 98 % values in order to take into account the plasma protein binding of meropenem, which is approximately 2 % of total plasma concentration.
From the initial model (one-compartment, first-order elimination with additive error model), several possible combinations of structural and stochastic models were evaluated (one- and two-compartment, first-order and non-linear elimination with additive, proportional, and mixed error models), as well as the interindividual variability (IIV) of pharmacokinetic parameters. The following covariates were tested within the models: gender, age, height, weight, body mass index, serum creatinine, creatinine clearance (calculated according to the Cockcroft and Gault formula), serum albumin, and severity of sepsis (i.e., sepsis, severe sepsis, or septic shock). A generalized additive modeling (GAM) using the Xpose4 package screened the covariates for their leverage on pharmacokinetic parameters of meropenem [24], and then, they were included stepwise with backward elimination from the final model. In particular, continuous variables were centered on their median value and their effect was evaluated by linear and non-linear relationships (i.e., piecewise linear, exponential, and power models). The improvement across the different models was judged by a decrease in objective function value (OFV) greater than 3.81 units (p < 0.05), while a decrease of 6.63 points was adopted in backward exclusion (p < 0.01). The difference in OFV (ΔOFV) was reported for all models with respect to the former basic model (i.e., 1-compartment model with additive error model, without IIV and covariates). The Xpose4 package was used to evaluate model performance by goodness-of-fit plots, visual predictive check (VPC), and bootstrap results from 4000 simulated datasets. Finally, eta-shrinkage values were calculated to identify and quantify model overfitting.
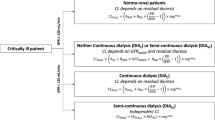
The final model was used to simulate meropenem plasma disposition in 4000 patients according to the procedure previously described [8]. In particular, sex and severity of sepsis were chosen in a random manner by appropriate command lines included within the NONMEM control file. In a similar way, patient’s age and serum albumin values were obtained according to value distribution of the corresponding parameter in the original population enrolled in the present study. Moreover, dosing regimens of meropenem were investigated as 3- and 5-h i.v. infusions (1- or 2-g doses two or three times per day) or continuous infusions (3- or 6-g doses per day). For all of these regimens, fT > MIC and fCmin > 4× MIC values were calculated in simulated patients. For every simulated patient, the individual fT > MIC (fT > MIC i ) value was obtained according to the following formula:
where LN is the natural logarithm, Cl i and V i are, respectively, the individual drug clearance and volume of distribution, and DI is the time interval between two consecutive doses (i.e., 8 or 12 h) [25]. For the calculation of fCmin > 4× MIC values, the predicted C min values were directly obtained from NONMEM output. For both PK/PD parameters, the probability of target attainment (PTA) and cumulative fraction of response (CFR) were calculated according to Mouton et al. [8], on the basis of EUCAST MIC value distribution [26] (see Supplementary Table 1). A threshold value for PTA of 95 % was considered to compare results among the different schedules of drug administration investigated in the present simulation.
Statistics
Demographic data of patients, covariates, and study results are presented as mean ± standard deviation (SD) or median values and range (or 95 % confidence interval), on the basis of the parameter described. Unpaired Student’s t test was used to compare variables according to gender. A P value lower than 0.05 was considered to be statistically significant. As stated above, the final population pharmacokinetic model was used to fit the observed data obtained after a 3-h infusion and to simulate the pharmacokinetic parameters after continuous infusions. The aim was to investigate whether the continuous infusions gave an advantage in the attainment of PK/PD target values over the extended infusions. Therefore, sample size was calculated by considering an α error of 0.5, a power of 0.8, and a mean difference of at least 15 % (±15 % as SD) in the main PK/PD parameters between the observed 3-h extended infusions and the simulated 5-h extended and continuous infusions of meropenem. Twenty patients were required to be enrolled to reject the null hypothesis that the difference was zero.
Results
The present study was conducted on 27 consecutive patients admitted to different ICUs of IRCCS AOU San Martino-IST Hospital, Genoa, from April 2013 to December 2014. All of the patients received meropenem 2–6 g/day as 3-h i.v. infusions alone (2 patients) or in association with colistin + tigecycline (7 patients), gentamicin + tigecycline (14 patients), gentamicin + tigecycline + fosfomycin (1 patient), gentamicin + tigecycline + ertapenem (2 patients), and tigecycline + ertapenem (1 patient). Only one patient received meropenem 9 g/day.
Main characteristics and descriptive statistics of principal covariates investigated in our patients are reported in Table 1, and significant gender differences were observed for body weight, height, and body surface area. The table also reports number of patients with sepsis, severe sepsis, or septic shock and severity of disease according to the Acute Physiology and Chronic Health Evaluation (APACHE) II classification [27] and Simplified Acute Physiology Score (SAPS) II Score [28], Charlson comorbidity index [29], Glasgow Coma Scale (GCS), and meropenem dosage. Twenty-eight days after the admission to ICU, five of the 27 patients (18.5 %) died.
Population pharmacokinetic analysis and simulation
One hundred and eighteen blood samples were obtained after the administration of a meropenem dose at steady state in 27 patients (median number of samples per patient, 4, range 2–5). Clinical records of some patients were lacking of covariate values (i.e., height, body weight, serum albumin, serum creatinine in two, one, one, and one subjects, respectively). In those cases, the gender-related median value of the covariate was adopted.
The final model was a one-compartment model with mixed error model and IIV for both Cl and V. The mixed error model (run 003) was associated with a significant improvement (ΔOFV = −35.24) with respect to the additive (the first model) and proportional error model (ΔOFV = −27.54, run 002). Interestingly, a two-compartment model did not achieve a significant improvement in terms of ΔOFV (−2.90, run 004) with respect to the corresponding one-compartment model. Further improvement was observed after the introduction of IIV for Cl, alone (ΔOFV = −71.51, run 006) and in combination with IIV for V (ΔOFV = −116.40, run 007). As stated above, the modeling procedure was guided by the GAM analysis performed on both Cl and V, and several covariates did seem to have an influence on the pharmacokinetics of meropenem. When every covariate was tested within the model in a stepwise procedure, the following ones were found to significantly affect the pharmacokinetics of meropenem: serum albumin on V (ΔOFV = −147.05, run 021), gender on Cl (ΔOFV = −155.44, run 031), patients’ age on V (ΔOFV = −162.95, run 033), and, finally, sepsis on Cl (ΔOFV = −169.44, run 059). The improvement in goodness-of-fit plots witnessed the leverage of those covariates on drug pharmacokinetics (Fig. 1), although the presence of over- and under-prediction over time is detectable and they likely depend on the one-compartment model (Fig. 1d). Furthermore, an exponential relationship was chosen for patients’ age and serum albumin, because it gave the better results in terms of standard errors, residuals, and goodness-of-fit plots with respect to other kinds of linear and non-linear relationships. However, it is worth noting that other possible covariates failed to improve the fitting of observed data despite a strong mechanistic and physiologic rationale and the variability among the present patients (Table 1) supported their inclusion within the model as already published [30]. In particular, the introduction of serum creatinine (ΔOFV = −89.70, run 009) and creatinine clearance (ΔOFV = −108.80, run 011) did not improve the fitting performance of the model without covariates (i.e., ΔOFV = −116.40, run 007). Values of fixed and random effects, together with bootstrap results, are presented in Table 2. The final model was as follows:
Goodness-of-fit plots of the final population pharmacokinetic model obtained simulating 4000 datasets on the basis of the original dataset as a template. Population (a) and individual prediction (b) plots are presented together with absolute individual weighted residual (|iWRES|) versus individual predictions (c) and weighted residuals (WRES) versus time after dose (d) graphs. Black thin and thick lines, lines of identity and linear regression lines (a, b) or loess line (c), respectively. Plots show lines of identity (black thin lines, a) and linear regression lines (black thick lines, b) and loess line (black thick lines, c, d)
where THETA(4) was 1 for men and 1.760 for women, while THETA(6) was 0.427 or 1 in the presence of sepsis or severe sepsis/septic shock, respectively. ALB and AGE are serum albumin and patients’ age, respectively, while ETA(1) and ETA(2) represent the IIV for Cl and V of meropenem, respectively. It is worth noting that meropenem clearance in women was greater than that measured in men (approximately 38 %) and that gender-based difference in the pharmacokinetics of drugs is not usual, and it likely reflects the large interpatient variability in a limited number of patients. Indeed, women had a higher drug clearance, but that difference was not statistically different because of the large interpatient variability (i.e., coefficient of variability of Cl in men and women accounted for 27.4 and 57.3 %, respectively). Therefore, the relationship between gender and drug clearance does serve to improve the fitting of the observed data in the present population of patients, while the analyses in a larger group of individuals could confirm or deny the relationship itself.
Furthermore, the IIV values of Cl and V decreased from 82.24 and 102.47 % up to 44.39 and 66.51 %, respectively, while the corresponding η-shrinkage values in the final model account for 4.22 and 8.16 %. The goodness of the final model to fit individual plasma concentration profiles was demonstrated by values of main pharmacokinetic parameters (Table 3) that are similar to those already published in the literature [31] and further sustained by the bootstrap and VPC analyses (Table 2 and Fig. 2).
Prediction-corrected visual predictive checks (90 % prediction interval) based on the final population pharmacokinetic model superimposed on prediction-corrected observed meropenem plasma concentrations. The figure shows the observed data (dashes); the median, 5th, and 95th percentile of the observed data (lines); and the 95 % confidence intervals around the simulated median (dark gray) and 5th and 95th percentiles (light gray)
The simulation of minimum plasma concentrations of meropenem returned mean ± SD values ranging from 3.11 ± 4.80 up to 33.57 ± 18.61 mg/L for a 5-h extended infusion of 1 g every 12 h or a continuous infusion of 6 g/day, respectively. Figure 3 presents PTA curves for both fT > MIC and fCmin > 4× MIC PK/PD parameters across the entire distribution of K. pneumoniae MIC values obtained from EUCAST [26]. Furthermore, Table 4 reports CFR values obtained on the basis of simulation for different therapeutic schedule. In particular, 5-h extended infusions were simulated according to the maximum time length of meropenem solution stability at room temperature (5.15 h) [32]. Results clearly show that the highest probability to achieve pre-defined target values both in terms of fT > MIC and fCmin > 4× MIC was associated with the shorter time interval between two consecutive doses (i.e., 8 h). On the basis of this observation, simulated continuous infusions of meropenem for total daily doses of 3 and 6 g led to an improvement in fCmin > 4× MIC values when compared with those obtained after 3- and 5-h extended infusions. Furthermore, trough values after continuous infusions remain above the 95 % threshold up to MIC values of 4 and 8 mg/L, respectively. These results suggest that although the fT > MIC values between extended and continuous infusions do not change in the present simulation, continuous infusions nearly abolished plasma concentration fluctuations, hence ensuring the achievement of higher C min values and, consequently, CFR values (Table 4).
Probability of target attainment for fT > MIC (a) and fCmin > 4× MIC (b) in 4000 simulated patients, according to the investigated schedules of meropenem administration and MIC value distribution obtained from EUCAST. Filled symbols, 3-h i.v. infusions of 1 g × 2 (square), 1 g × 3 (triangle), 2 g × 2 (circle), and 2 g × 3 (diamond). Open symbols, 5-h i.v. infusions of 1 g × 3 (circle) and 2 g × 3 (diamond) or continuous i.v. infusions of 3 g/day (triangle) and 6 g/day (square)
Discussion
In the present study, we found that continuous i.v. infusions of meropenem at doses of 6 g/day seem to be more effective than standard regimens (1–3 g twice or thrice per day as 3-h i.v. infusions) to achieve target PK/PD values.
Meropenem remains a suitable choice for treatment of severe infections in critically ill patients because it exerts a time-dependent killing against both Gram-positive and Gram-negative bacterial strains. However, several factors may significantly influence meropenem pharmacokinetics, hence exposing the patient to a non-negligible risk of treatment failure especially when severe or life-threatening infections are diagnosed. The present study identified significant covariates that may influence meropenem disposition in ICU patients affected by K. pneumoniae infection, thus improving the stratification of patients according to their risk of receiving suboptimal treatments.
It is worth noting that sepsis is considered a hyperdynamic condition associated with an increased clearance of drugs and their corresponding volume of distribution [11]. Furthermore, drug disposition may display a large interindividual and intraindividual variability due to the severity of the sepsis and or the general clinical conditions of patients [33]. However, in a previous study [34], 15 critically ill patients who received meropenem 1000 mg twice a day as a 30-min i.v. infusion had lower values of clearance and volume of distribution with respect to those measured in the present ones, despite that the severity of infection was similar according to the Charlson and SAPS II scores. That difference still remains also when the comparison is made considering those of our patients that received meropenem 1000 mg two or three times per day. It is likely that the limited number of patients and their variable clinical conditions could be claimed as responsible for these discrepancies. Indeed, the severity of infection (i.e., sepsis versus severe sepsis or septic shock) was identified as having a leverage on drug clearance in our model, because individuals with septic shock or severe sepsis showed an increase in drug clearance with respect to the remaining individuals (9.71 ± 4.61 vs. 8.96 ± 4.45 L/h, respectively). However, the difference in Cl between the two groups was not significant because of the large variability (CV%, 47.5–49.6 %). At the same time, V was increased in the presence of severe sepsis or septic shock. Intriguingly, another smaller study performed in nine patients found Cl and V mean values lower than the present one [35], and the severity of the infection was not identified as a significant covariate for meropenem pharmacokinetics. Therefore, the present results are suggesting for the first time that the severity of the infection should be taken into account to choose the most appropriate dose of meropenem, and this is the most important difference with respect to previous works [34, 35]. Furthermore, the large interpatient variability in the pharmacokinetics of meropenem does suggest the adoption of therapeutic drug monitoring protocols. Finally, creatinine clearance has been identified as a significant covariate for drug clearance in several previous POP/PK models [14, 30], but not in the present one. Although there are differences listed above, the present values of the main pharmacokinetics parameters are in agreement with those already published [31].
The administration of meropenem as continuous infusions allows the maintenance of plasma concentrations above the MIC for target organisms while it prevents the highest concentrations that may result in adverse reactions without an improvement in bactericidal activity [33, 36]. In fact, simulated continuous i.v. infusions of meropenem 3–6 g/day nearly abolish plasma fluctuations and this fact allows the achievement of fCmin > 4× MIC values above the 95 % for K. pneumoniae strains whose MIC values are 4–8 mg/L. Furthermore, previous results demonstrated that patients with severe bacterial infections experienced a significantly greater clinical cure rate (82 vs. 33 %; p = 0.002) and bacteriological eradication (97 vs. 44 %; p < 0.001) when meropenem achieved T > MIC values ≥100 % with respect to lower T > MIC values [37]. Therefore, plasma meropenem concentrations higher than MIC values for the entire dosing interval between two consecutive administrations should be regarded as a mandatory goal for an effective and appropriate antimicrobial chemotherapy, as demonstrated in cystic fibrosis patients who received meropenem as continuous infusions at daily doses of 3 and 6 g [38]. Although continuous infusions may improve meropenem efficacy, the present model suggests that meropenem pharmacokinetics is significantly influenced by several factors, and highest doses should be used to achieve effective fCmin > 4× MIC values in ICU patients. However, as pointed out by several Authors [37, 39], the achievement of highest T > MIC and fCmin > 4× MIC values is negatively influenced by the presence of bacterial strains with high MICs. Highest dosages are not usually prescribed for the augmented risk of toxic effects; hence, the alternative and effective strategy is to use carbapenems in association with other drugs [40].
Finally, the present study shows some pitfalls that should be discussed. The small number of enrolled patients is a limitation even if it can offer interesting information about meropenem pharmacokinetics in critically ill patients with sepsis. Second, a resistant vs. sensitive output has been obtained by the Vitek2 system instead of the determination of actual MIC values, as it happens by using the broth microdilution or the E-test assays. However, the present study was aimed at simulating different dosing regimens rather than studying the PK/PD correlation in the enrolled patients. Third, in contrast with other antimicrobial drugs, such as vancomycin, meropenem solutions have a limited stability at room temperature [39]. This means that the carbapenem should be reconstituted at least five times a day to allow a continuous infusion, hence increasing the workload of caregivers.
In conclusion, the present study suggests that continuous i.v. infusions of meropenem may have a greater probability than extended infusions (i.e., 3–5 h) to be effective in critically ill patients and that the severity of the sepsis seems to influence the pharmacokinetics of the drug. However, the treatment of the less-sensitive bacterial strains requires polychemotherapies, which represent the most appropriate way to obtain a higher rate of clinical cure, to overcome treatment failures, and to reduce the incidence of drug resistance. Finally, the present study shows the wide interpatient variability in drug disposition among critically ill patients, and it strongly supports the adoption of therapeutic drug monitoring protocols for meropenem schedules.
References
Binder L, Schwörer H, Hoppe S, Streit F, Neumann S, Beckmann A, et al. (2013) Pharmacokinetics of meropenem in critically ill patients with severe infections. Ther Drug Monit 35:63–70
Udy AA, Roberts JA, Lipman J (2013) Clinical implications of antibiotic pharmacokinetic principles in the critically ill. Intensive Care Med 39:2070–2082
Drusano GL, Hutchison M (1995) The pharmacokinetics of meropenem. Scand J Infect Dis Suppl 96:11–16
European Medicines Agency (2009) Meropenem summary of product characteristics http://www.ema.europa.eu/docs/en_GB/document_library/Referrals_document/Meronem_30/WC500018555.pdf. Accessed 2 April 2015
Jaruratanasirikul S, Limapichat T, Jullangkoon M, Aeinlang N, Ingviya N, Wongpoowarak W (2011) Pharmacodynamics of meropenem in critically ill patients with febrile neutropenia and bacteraemia. Int J Antimicrob Agents 38:231–236
Lomaestro BM, Drusano GL (2005) Pharmacodynamic evaluation of extending the administration time of meropenem using a Monte Carlo simulation. Antimicrob Agents Chemother 49:461–463
MacGowan A (2011) Revisiting beta-lactams—PK/PD improves dosing of old antibiotics. Curr Opin Pharmacol 11:470–476
Mouton JW, Dudley MN, Cars O, Derendorf H, Drusano GL (2005) Standardization of pharmacokinetic/pharmacodynamic (PK/PD) terminology for anti-infective drugs: an update. J Antimicrob Chemother 55:601–607
Drusano GL (2003) Prevention of resistance: a goal for dose selection for antimicrobial agents. Clin Infect Dis 36(Suppl. 1):S42–S50
Craig WA (1998) Pharmacokinetic/pharmacodynamic parameters: rationale for antibacterial dosing of mice and men. Clin Infect Dis 26:1–10
Blot SI, Pea F, Lipman J (2014) The effect of pathophysiology on pharmacokinetics in the critically ill patient–concepts appraised by the example of antimicrobial agents. Adv Drug Deliv Rev 77:3–11
Roberts JA, Ulldemolins M, Roberts MS, McWhinney B, Ungerer J, Paterson DL, et al. (2010) Therapeutic drug monitoring of beta-lactams in critically ill patients: proof of concept. Int J Antimicrob Agents 36:332–339
De Waele JJ, Carrette S, Carlier M, Stove V, Boelens J, Claeys G, et al. (2014) Therapeutic drug monitoring-based dose optimisation of piperacillin and meropenem: a randomized controlled trial. Intensive Care Med 40:380–387
Crandon JL, Ariano RE, Zelenitsky SA, Nicasio AM, Kuti JL, Nicolau DP (2011) Optimization of meropenem dosage in the critically ill population based on renal function. Intensive Care Med 37:632–638
Roberts JA, Kirkpatrick CM, Roberts MS, Robertson TA, Dalley AJ, Lipman J (2009) Meropenem dosing in critically ill patients with sepsis and without renal dysfunction: intermittent bolus versus continuous administration? Monte Carlo dosing simulations and subcutaneous tissue distribution. J Antimicrob Chemother 64:142–150
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, et al. (2003) 2001 SCCM/ESICM/ACCP/ATS/SIS International sepsis definitions Conference. Intensive Care Med 31(4):1250–1256
CLSI (2012) Performance standards for antimicrobial susceptibility testing: twenty-second Informational Supplement. CLSI document M100–22. Wayne, PA, Clinical and Laboratory Standards Institute
Legrand T, Chhun S, Rey E, Blanchet B, Zahar JR, Lanternier F, et al. (2008) Simultaneous determination of three carbapenem antibiotics in plasma by HPLC with ultraviolet detection. J Chromatogr B Analyt Technol Biomed Life Sci 875:551–556
International Conference on Harmonization (ICH). Harmonised tripartite guideline: validation of analytical procedures: text and methodology Q2(R1) 6 1996. ICH Official web site Available: http://www.ich.org. Accessed 8 May 2015
Shah VP, Midha KK, Dighe S (1992) Conference report: analytical methods validation: bioavailability, bioequivalence, and pharmacokinetic studies. J Pharm Sci-US 81:309–312
Beal SL, Sheiner LB, Boeckmann AJ (2009) NONMEM users guides. Ellicott City, MD:ICON Development Solutions 1989
Jonsson EN, Karlsson MO (1999) Xpose—an S-PLUS based population pharmacokinetic/pharmacodynamic model building aid for NONMEM. Comput Methods Prog Biomed 58:51–64
Lindbom L, Ribbing J, Jonsson EN (2004) Perl-speaks-NONMEM (PsN)—a Perl module for NONMEM related programming. Comput Methods Prog Biomed 75:85–94
Bergstrand M, Hooker AC, Wallin JE, Karlsson MO (2011) Prediction-corrected visual predictive checks for diagnosing nonlinear mixed-effects models. AAPS J 13:143–151
Mouton JW, Punt N (2001) Use of the t > MIC to choose between different dosing regimens of beta-lactam antibiotics. J Antimicrob Chemother 47:500–501
European Committee on Antimicrobial Susceptibility Testing (2016) Data from the EUCAST MIC distribution website, http://www.eucast.org. Accessed February 25, 2015
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) APACHE II: a severity of disease classification system. Crit Care Med 13:818–829
Le Gall JR, Lemeshow S, Saulnier F (1993) A new Simplified Acute Physiology score (SAPS II) based on a European/North American multicenter study. JAMA 270:2957–2963
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Zhou QT, He B, Zhang C, Zhai SD, Liu ZY, Zhang J (2011) Pharmacokinetics and pharmacodynamics of meropenem in elderly Chinese with lower respiratory tract infections: population pharmacokinetics analysis using nonlinear mixed-effects modelling and clinical pharmacodynamics study. Drugs Aging 28:903–912
Novelli A, Adembri C, Livi P, Fallani S, Mazzei T, De Gaudio AR (2005) Pharmacokinetic evaluation of meropenem and imipenem in critically ill patients with sepsis. Clin Pharmacokinet 44:539–549
Pea F, Viale P (2009) Bench-to-bedside review: appropriate antibiotic therapy in severe sepsis and septic shock-dose the dose matter? Crit Care 32:214
Sinnollareddy MG, Roberts MS, Lipman J, Roberts JA (2012) β-lactam pharmacokinetics and pharmacodynamics in critically ill patients and strategies for dose optimization: a structured review. Clin Exp Pharmacol Physiol 39:489–496
Goncalves-Pereira J, Silva NE, Mateus A, Pinho C, Povoa P (2014) Assessment of pharmacokinetic changes of meropenem during therapy in septic critically ill patients. BMC Pharmacol Toxicol 15:21
Jaruratanasirikul S, Thengyai S, Wongpoowarak W, Wattanavijitkul T, Tangkitwanitjaroen K, Sukarnjanaset W, et al. (2015) Population pharmacokinetics and Monte Carlo dosing simulations of meropenem during the early phase of severe sepsis and septic shock in critically ill patients in intensive care units. Antimicrob Agents Chemother 59:2995–3001
Thalhammer F, Traunmüller F, EI Menyawi I, Frass M, Hollenstein UM, Locker GJ, et al. (1999) Continuous infusion versus intermittent administration of meropenem in critically ill patients. J Antimicrob Chemother 43:523–527
Chytra I, Stepan M, Benes J, Pelnar P, Zidkova A, Bergerova T, et al. (2012) Clinical and microbiological efficacy of continuous versus intermittent application of meropenem in critically ill patients: a randomized open-label controlled trial. Crit Care 16:R113
Kuti JL, Nightingale CH, Knauft RF, Nicolau DP (2004) Pharmacokinetic properties and stability of continuous-infusion meropenem in adults with cystic fibrosis. Clin Ther 26:493–501
Taccone FS (2012) Continuous infusion of meropenem in critically ill patients: practical considerations. Crit Care 16:444
Tumbarello M, Viale P, Viscoli C, Trecarichi EM, Tumietto F, Marchese A, et al. (2012) Predictors of mortality in bloodstream infections caused by Klebsiella pneumoniae carbapenemase-producing K. pneumoniae: importance of combination therapy. Clin Infect Dis 55:943–950
Acknowledgments
The authors should thank the patients, their relatives, and nurse staff for their invaluable support in this study.
Author’s contribution
Authors | Conception and design of study | Acquisition of data: laboratory or clinical | Analysis of data | Drafting of article and/or critical revision | Final approval of manuscript |
|---|---|---|---|---|---|
Francesca Mattioli | X | X | X | X | |
Carmen Fucile | X | X | X | X | |
Valerio Del Bono | X | X | X | ||
Valeria Marini | X | X | |||
Andrea Parisini | X | X | X | ||
Alexandre Molin | X | X | X | ||
Maria Laura Zuccoli | X | X | |||
Giulia Milano | X | X | |||
Romano Danesi | X | X | |||
Anna Marchese | X | X | |||
Marialuisa Polillo | X | X | |||
Claudio Viscoli | X | X | |||
Paolo Pelosi | X | X | |||
Antonietta Martelli | X | X | |||
Antonello Di Paolo | X | X | X | X |
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Disclosure
The study did not provide any source of funding by sponsor.
Conflict of interest
Antonello Di Paolo is a board member for Novartis Pharma Spa. The other authors have none to declare.
Headings
- Meropenem pharmacokinetics is highly variable in ICU patients with severe infections, and some patients do not achieve effective meropenem plasma concentrations.
- The severity of infection does influence the pharmacokinetics of meropenem.
- Meropenem efficacy could be increased by the adoption of continuous infusions.
Electronic supplementary material
ESM 1
(DOCX 17 kb)
Rights and permissions
About this article
Cite this article
Mattioli, F., Fucile, C., Del Bono, V. et al. Population pharmacokinetics and probability of target attainment of meropenem in critically ill patients. Eur J Clin Pharmacol 72, 839–848 (2016). https://doi.org/10.1007/s00228-016-2053-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-016-2053-x