Abstract
The number of patients with severe invasive infections (mainly exhibiting bacteremia) with Streptococcus dysgalactiae subsp. equisimilis (SDSE) has been increasing worldwide. We herein report the clinical aspects of invasive infections (cellulitis, pneumonia, and urosepsis) occurring with SDSE in 13 elderly patients (mean age 84 years, range 69–99 years) diagnosed at a hospital for elderly individuals during the period January 2005–June 2009. Ten subjects had underlying diseases, including neurologic disorders, diabetes mellitus, and others. Eleven patients presented to the hospital emergency department, and the most common symptom was high fever or respiratory distress. Primary care and emergency department doctors treating elderly patients with high fever should keep in mind invasive SDSE infection as a differential diagnosis, especially when an elderly person has underlying illnesses. To detect SDSE in elderly subjects, blood cultures should be obtained before the administration of antimicrobials because, as we found, the patients’ symptoms were limited.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Streptococcus dysgalactiae subsp. equisimilis (SDSE) was proposed in 1996 as a new taxon involved in human streptococcal infections [1]. This microorganism has Lancefield group C or G antigen, exhibits strong β-hemolysis, and shows streptokinase activity in human plasminogen and proteolytic activity in human fibrin. We have just completed whole-genome analyses of the original two isolates [GGS_124 (GenBank accession no AP010935) and RE378] of SDSE, demonstrating a rate of overlap between this subspecies and group A streptococcal genomes of 61–63%; overlap between the subspecies and group B streptococcal genomes was 15%. Similarly to group A streptococci, SDSE possesses virulence factors such as M protein, streptolysin O, streptolysin S, streptokinase, hyaluronidase, and C5a peptidase. SDSE has been established as possible normal flora of the skin, oropharynx, and gastrointestinal and genitourinary tracts. This pathogen was identified in respiratory tract specimens from patients with noninvasive SDSE diseases [2]. Invasive SDSE infections, mainly exhibiting bacteremia, are now being observed increasingly worldwide [3, 4]. Invasive infections represent the isolation of SDSE from a normally sterile site (i.e., blood, cerebrospinal fluid, joint fluid, ascites, or pleural effusion) [3, 4]. Here we report clinical aspects of invasive infections caused by SDSE in 13 elderly patients diagnosed at a hospital for elderly individuals between January 2005 and June 2009.
Streptococcal isolates with Lancefield group C or G antigen and β-hemolysis were isolated from blood specimens, and detailed information was collected from the hospital clinical laboratory database. SDSE was speciated based on results of biologic tests, including bacitracin resistance, pyrrolidonyl-arylamidase test (negative), Voges–Proskauer test (negative), and β-d-glucuronidase test (positive). In addition, the emm gene, which encodes M protein—a major bacterial virulence factor—was typed, as previously described [4, 5]. To assess the similarity of isolates, DNA profiles after digestion with the restriction enzyme SmaI were compared by pulsed-field gel electrophoresis (PFGE) [6]. Patients’ clinical features were reviewed using medical records. Clinical data (age, underlying disease, onset situation, main symptom, and vital signs) and laboratory data [white blood cell count (WBC), neutrophil count, C-reactive protein (CRP), platelet count (Plt), hemoglobin (Hb), and others] were obtained at the time blood cultures were performed for each patient. Also, the diagnosis of invasive infection was reviewed by a physician expert in infectious diseases.
Thirteen strains of SDSE and the corresponding elderly patients were studied. The clinical features and outcomes for invasive SDSE infections are shown with microbiologic data in Table 1. Twelve isolates had Lancefield group G antigen. The emm genotypes (stG10.0 and others) and SmaI-digested PFGE DNA profiles for 7 isolates (numbers 7–13) varied between strains, suggesting the possible invasion of a different colonized strain in each patient rather than the clonal expansion of a specific subpopulation of isolates. The mean age of the infected patients was 84 years (range 69–99 years); 7 were female; and 10 had underlying diseases including neurologic disorders, diabetes mellitus, and others. Eleven patients with SDSE infections presented to the hospital emergency department, indicating that the infection was mainly community-acquired. The most common symptom was high fever or respiratory distress, without other complaints. Mean body temperature and heart rate were 38.9°C (range 36.4–40.1°C) and 93 beats/min (range 72–120 beats/min). Cellulitis, pneumonia, and urosepsis (n = 4 for each) constituted the main invasive infections. In subjects with pneumonia, chest roentgenograms disclosed patchy infiltrates. Mean WBC, neutrophil count, CRP, Plt, and Hb were 12.2 × 109 cells/l (range 5.7–19.2 × 109 cells/l), 10.9 × 109 cells/l (range 4.6–15.6 × 109 cells/l), 6.27 mg/dl (range 0.35–28.34 mg/dl), 210 × 109 cells/l (range 59–510 × 109 cells/l), and 11.2 g/dl (range 7.4–13.4 g/dl), respectively. As treatment, β-lactam antibiotics including penicillins or cephalosporins were administered parenterally in all subjects. No patients died of an invasive infection; any deaths involved other causes. No recurrent SDSE infections were found. The clinical aspects of the invasive SDSE infections in the elderly subjects were considered to be characterized as follows; onset in older-age patients, presence of underlying illnesses, community-acquired onset, and limited patients’ symptoms.
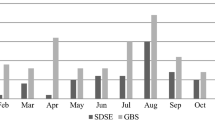
In a recent report from Finland considering non-necrotizing bacterial cellulitis, SDSE was observed most often, being isolated in 22% of cultures from either skin lesions or blood [7]. Also, pneumonia and thoracic empyema caused by SDSE were reported from Japan [8, 9]. Similar to the findings of previous reports [8], chest radiographs in our patients with pneumonia indicated patchy infiltrates. The pulmonary lesions may have been induced by the aspiration of SDSE as possible normal flora of the oropharynx, because the functions of both swallowing and coughing are reduced in the elderly. The mortality of invasive group G streptococcal infections was reported previously as 8–18% [1, 10, 11]. Active laboratory-based surveillance for invasive SDSE, Streptococcus pyogenes (GAS), and S. agalactiae (GBS) infections was conducted for 1 year (August 2006–July 2007) in 142 medical institutions participating in the Invasive Streptococcal Disease Working Group established at the 19th annual meeting of the Japanese Society for Clinical Microbiology, in order to compare the clinical aspects of invasive infections caused by the three species [12]. While 231 invasive SDSE infections were identified, 97 other patients had GAS and 151 had GBS. All patients with invasive SDSE infection were adults (median age 75 years), while GBS infected some patients 4 months old or younger in addition to adults. Underlying diseases were present in 78.8% of the patients with invasive SDSE illnesses; underlying medical conditions were less frequent in subjects with GAS infections than in patients with SDSE or GBS. In addition, all cases of SDSE, GAS, or GBS diseases were community-acquired and 42 patients (18%) with SDSE infections presented to the hospital emergency department, a fraction similar to the proportions of subjects presenting to the emergency department with infections involving the other two bacterial groups.
There are some limitations regarding the clinical features of the SDSE invasive infections reported in the elderly subjects in our study. There may have been a selection bias for the enrolled patients, because our institute is already established as one of the expert hospitals for elderly individuals. In order to clarify risk factors in the subjects susceptible to SDSE, we did not design a setting for control patients, who were frequency matched to the case subjects by age and gender.
In conclusion, based on the detailed information of invasive SDSE infection in our observations, primary care and emergency department doctors treating elderly patients with high fever should keep in mind invasive infections caused by SDSE as a differential diagnosis, especially when the elderly person has underlying illnesses, although we note that no characteristic features giving clues to the diagnosis were found in the present study. To detect this pathogen in elderly subjects, blood cultures should be obtained before the administration of antimicrobials because, as we found, the patients’ symptoms were limited to high fever or respiratory distress.
References
Vandamme P, Pot B, Falsen E, Kersters K, Devriese LA. Taxonomic study of Lancefield streptococcal groups C, G, and L (Streptococcus dysgalactiae) and proposal of S. dysgalactiae subsp. equisimilis subsp. nov. Int J Syst Bacteriol. 1996;46:774–81.
Sunaoshi K, Murayama SY, Adachi K, Yagoshi M, Okuzumi K, Chiba N, et al. Molecular emm genotyping and antibiotic susceptibility of Streptococcus dysgalactiae subsp. equisimilis isolated from invasive and noninvasive infections. J Med Microbiol. 2010;59:82–8. doi:10.1099/jmm.0.013201-0.
Ikebe T, Murayama S, Saitoh K, Yamai S, Suzuki R, Isobe J, et al. Surveillance of severe invasive group-G streptococcal infections and molecular typing of the isolates in Japan. Epidemiol Infect. 2004;132:145–9.
Broyles LN, Van Beneden C, Beall B, Facklam R, Shewmaker PL, Malpiedi P, et al. Population-based study of invasive disease due to β-hemolytic streptococci of groups other than A and B. Clin Infect Dis. 2009;48:706–12.
Sunaoshi K, Aburahashi H, Kobayashi R, Yamamoto Y, Okuzumi K, Yoshida A, et al. Emm typing by genetic identification of Streptococcus dysgalactiae subsp. equisimilis and susceptibility to oral antibiotics. Kansenshogaku Zasshi. 2006;80:488–95.
Murayama SY, Seki C, Sakata H, Sunaoshi K, Nakayama E, Iwata S, et al. Capsular type and antibiotic resistance in Streptococcus agalactiae isolates from patients with invasive infections, ranging from newborns to the elderly. Antimicrob Agents Chemother. 2009;53:2650–3.
Siljander T, Karppelin M, Vähäkuopus S, Syrjänen J, Toropainen M, Kere J, et al. Acute bacterial, nonnecrotizing cellulitis in Finland: microbiological findings. Clin Infect Dis. 2008;46:855–61.
Matsui D, Kitasato Y, Honda S, Ueno K, Tanaka A, Edakuni N, et al. A case of bacterial pneumonia caused by Streptococcus dysgalactiae subsp. equisimilis, showing patchy consolidations resembling organizing pneumonia. Nihon Kokyuki Gakkai Zasshi. 2007;45:36–42.
Ueno K, Kawayama T, Edakuni N, Koga T, Aizawa H. A case of thoracic empyema with gas formation associated with Streptococcus dysgalactiae subsp. equisimilis. Kansenshogaku Zasshi. 2006;80:527–30.
Skogberg K, Simonen H, Renkonen OV, Valtonen VV. Beta-haemolytic group A, B, C and G streptococcal septicaemia: a clinical study. Scand J Infect Dis. 1988;20:119–25.
Ekelund K, Skinhøj P, Madsen J, Konradsen HB. Invasive group A, B, C and G streptococcal infections in Denmark 1999–2002: epidemiological and clinical aspects. Clin Microbiol Infect. 2005;11:569–76.
Takahashi T, Sunaoshi K, Sunakawa K, Fujishima S, Watanabe H, Ubukata K. Clinical aspects of invasive infections with Streptococcus dysgalactiae ssp. equisimilis in Japan: differences with respect to Streptococcus pyogenes and Streptococcus agalactiae infections. Clin Microbiol Infect. doi:10.1111/j.1469-0691.2009.03047.x.
Acknowledgments
This study was funded in part by a grant under the category, ‘‘Research Project for Emerging and Re-emerging Infectious Diseases’’ (H-19-002), from the Japanese Ministry of Health, Labour and Welfare (to Dr. K. Ubukata) and a Grant-in-Aid for Scientific Research (B) from the Ministry of Education, Culture, Sports, Science and Technology of Japan (number 21390306, to Dr. T. Takahashi). The authors thank Akiko Ono, Keisuke Okada, and Miho Yoshino for assistance with the manuscript preparation.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Takahashi, T., Asami, R., Tanabe, K. et al. Clinical aspects of invasive infection with Streptococcus dysgalactiae subsp. equisimilis in elderly patients. J Infect Chemother 16, 68–71 (2010). https://doi.org/10.1007/s10156-009-0016-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10156-009-0016-1