Abstract
Background
Transanal (Ta) pelvic exenteration is a promising, minimally invasive method for treating locally advanced colorectal cancer. However, since it is technically difficult to perform, Ta pelvic exenteration is rarely reported in locally advanced T4 rectal cancer cases. The aim of this study was to evaluate the feasibility of transabdominal laparoscopy-assisted Ta pelvic exenteration.
Methods
Six patients (4 males and 2 females) had laparoscopy-assisted Ta total or posterior pelvic exenteration for locally advanced or recurrent colorectal cancer cases at the Nagasaki University Hospital between September 2018 and August 2019. Clinical and pathological outcomes were measured and analyzed.
Results
The median operation time and intraoperative blood loss were 481 (range 456–709) minutes and 352.5 (range 257–1660) ml, respectively. R0 resection was achieved in all cases, and no patient required open surgery. Two patients had grade 3 complications (Clavien-Dindo) or higher. There was no mortality, and no reoperation was required.
Conclusions
The results suggest that laparoscopic-assisted Ta pelvic exenteration is an acceptable procedure, may help overcome the current technical difficulties, and may improve outcomes in patients with locally advanced rectal cancer.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pelvic exenteration (PE) is an effective, but invasive surgical treatment for locally advanced T4 colorectal carcinoma. Laparoscopic extended surgery for rectal cancer has been described to have fewer complications than open surgery [1, 2]. However, technical difficulties arise in cases involving a narrow pelvis or large tumors, especially when the tumor is located in the lower rectum. Transanal total mesorectal excision (TaTME) was developed as a new minimally invasive surgery (MIS), which potentially overcomes the limitations of laparoscopic surgery, with a wider circumferential resection margin (CRM) [3,4,5,6,7]. TaTME has the advantage of optimal visualization of the surgical site during lower rectal dissection, and relatively straightforward maneuvering of surgical instruments due to the transanal (Ta) approach [8]. Nevertheless, the Ta approach can often lead to an incision in deeper layers that are outside of the colon, inducing urethral and nerve injury, mainly due to the limited and unfamiliar “reversed” surgical view from the anal side. Thus, TaTME optimization is essential. A two-team approach of TaTME combined with laparoscopy may potentially overcome the aforementioned limitations.
To the best of our knowledge, there are only a few case reports on the use of trans anal total pelvic exenteration in locally advanced T4 rectal cancer cases [9, 10], and the benefits of the two-team approach are yet to be highlighted. As locally advanced T4 cancer is associated with a high risk of a positive circumferential resection margin (CRM) [11, 12], TaTME, which excels in securing CRM, may improve surgical outcomes, including a reduction of local recurrence [13]. Here, we report our experience of laparoscopic-assisted Ta PE in six cases, to evaluate its feasibility in the treatment of locally advanced T4 colorectal cancer.
Material and methods
Patient characteristics
Six patients (4 males and 2 females, median age 68.5 (range 67–70) years, with a median body mass index of 20.9 (range 16.5–24.4) kg/m2) with locally advanced rectal cancer, had Ta PE at the Nagasaki University Hospital, Japan between September 2018 and August 2019. All patients with rectal cancer, defined as a biopsy-proven adenocarcinoma, had preoperative staging of local and distant disease, including a computed tomography (CT) scan of the chest and abdomen and magnetic resonance imaging (MRI) of the pelvis. All patients had advanced mrT4 rectal cancer, along with infiltration in anterior organs such as the prostate and vagina. None of the patients had levator muscle or anal canal invasion, and the median distance of the distal tumor margin from the anal verge was 45 (range 30–70) mm. The patients had cStageII (n = 2), cStageIII (n = 2), cStageIV (n = 1) (paraaortic lymph node metastasis), and recurrent cancer (n = 1), respectively. Five patients were given neoadjuvant chemotherapy (NAC) (n = 3) or neoadjuvant chemoradiotherapy (NACRT) (n = 2) but one patient refused to have neoadjuvant treatment. Medical records of all patients enrolled in this study were reviewed retrospectively, including patient characteristics, postoperative complications, as well as surgical and oncological outcomes. Postoperative complications were defined according to the Clavien–Dindo classification [14]. Death within 90 days after operation was defined as operative mortality. The clinical characteristics of the enrolled patients are presented in Table 1. The study and surgical methods were approved by the ethics committee of the Nagasaki University hospital (Office of Human Subjects Protection, Registration number: 19102112). As per the guidelines of the ethics committee for official informed consent and disclosure, information regarding the study was made available on the institution’s website. Patients were able to withdraw their consent for participation in the study by following the instructions listed on the website.
Operative technique
The Ta approach was selected in cases where more than 20 mm of the distal resected margin was expected to be available for anal-preserving surgery. Ta PE was performed by two teams (abdominal and perineal teams), led by two specialists in colorectal and endoscopic surgery, who were certified by the Japanese Society of Endoscopic Surgery. The procedure is shown in detail in the video. Patients were placed in the lithotomy position; three surgeons operated from the abdominal side (abdominal team) and two from the perineal side (perineal team). TPE and posterior pelvic exenteration (PPE) were then conducted, as follows.
Men (TPE)
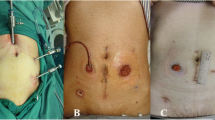
Four men were included in the study, and the Ta approach was performed in all of them. A pneumorectum/pneumoperitoneum was created by AirSeal® (Conmed, Utica, NY, USA) at a pressure of 10 mmHg and a CO2 flow of 5–10 L/min. A Lone Star Retractor (Lone Star Medical Products, Houston, TX, USA) was used for exposure. In the Ta approach, a Ta platform (GelPOINT path; Applied Medical, Rancho Santa Margarita, CA, USA) was introduced into the anal canal. The perineal team first processed the anal stump and dissected the posterior side of the rectum. The anterior side of the rectum, urethra, and dorsal venous complex (DVC) were then divided, and the Retzius cavity was dissected. Meanwhile, the abdominal team identified and transected the root of the inferior mesenteric vein. Following a medial-to-lateral approach, the sigmoid-rectosigmoid colon was mobilized by the perineal team. Pelvic lymph node dissection was performed bilaterally along the pelvic wall, and the specimen was removed in cooperation with the abdominal side. Finally, the anastomosis was completed using hand-sewing or single-stapling techniques and a urinary diversion was performed from the abdominal side by creating an ileal conduit (Figs. 1, 2).
Surgical procedure of the two-team surgery during TaTME. a full-thickness circumferential incision is performed 1 cm distal to the purse-string suture (b) The urethra is exposed, clipped, and divided (c) The dorsal venous complex (DVC) behind the urethra is divided using Sonicision™ (Medtronic) without ligation
Women (PPE)
Two women were included in the study and Ta PPE was performed in all cases. A pneumorectum was created, and a Ta platform was introduced into the anal canal. The perineal team first performed a full-thickness incision around the anal stump and dissected the posterior aspect of the rectum. Dissection was minimized at the anterior rectal wall; a Ta platform was placed in the vagina, and the vaginal canal was incised endoscopically. The cranial aspect of the front layer of the vagina was then dissected, and the vesico-uterine pouch was opened. The subsequent operative steps were performed similarly to those in the male patients.
Results
Operative results
The operative results are shown in Table 2. There were no conversions to open surgery. Lateral pelvic node (LPN) and paraaortic lymph-node dissections were performed in five (83.3%) and one (16.7%) patient, respectively. In four cases of TPE with bladder invasion, urinary diversions were performed using an ileal conduit. Since in the remaining two cases of PPE the tumor invaded the ureters, a uretero-ureterostomy or uretero-neocystostomy was performed for reconstruction. The median operation time and intraoperative blood loss were 481 (range 456–709) minutes and 352.3 (range 257–1660) ml, respectively. Based on the Clavien–Dindo classification, complications of all grades were observed in 4 (66.7%) and grade 3a were observed in 2 (33.3%) patients, (e.g., lymphocele and pelvic infection). Two patients (33.3%) had a perineal wound and urinary tract infection (grade 2), respectively, that were managed with conservative treatment (Table 2). In addition, serious complications such as ureteral/anastomotic leaks were not observed in any cases, no patients required reoperation, and there was no operative mortality. The median postoperative hospital stay was 22 (range 13–36) days.
Pathological findings
The pathological results are shown in Table 3. The median distance of the distal resection margin from the tumor was 27.5 (range 10–70) mm. The median tumor size was 50 (range 20–120) mm. Although five out of six patients had mrT4b tumors on radiological staging, the pathological findings based on the pathological tumor-node-metastasis classification were as follows: ypT4a: 1/6 (16.7%) and ypT4b: 3/6 (50.0%). Except for one case with recurrent cancer, the pathological stages were ypStage I in one case, ypStageII in two cases and ypStageIII in two cases.
Discussion
Brunschwig first described PE in 1948 as “the most radical surgical attack so far described for pelvic cancer” [15]. The overall mortality rate associated with PE surgery was 23% [15]. Currently, PE continues to be the only curative treatment for advanced or recurrent pelvic cancer. In the early 2000s, the PE-associated mortality rate decreased to approximately 5%, due to improvements in surgical techniques and the postoperative care of these patients [16] and was found to be 0–8.7% in a recent systematic review [17] Several reports on use of laparoscopic surgery for TPE as minimally invasive surgery have been published; however, it remains difficult to manipulate forceps within a narrow pelvis, which tends to prolong the operative time [2, 18,19,20].
Therefore, we evaluated the feasibility of laparoscopic-assisted Ta PE in overcoming the current difficulties of PE. Recently, Uematsu et al. reported a case of Ta PE with laparoscopic assistance in a patient with T4 rectal cancer, noting the excellent surgical view with potential benefits in reducing the operation time and complications [9]. They also reported a case of trans-perineal (Tp)-TPE in the prone jack-knife position; in this case, the Tp and laparoscopy procedures were sequential. The study indicated that the technically challenging urethral and DVC division could be safely performed from the perineal side [10]. Mehta et al. reported good results for Tp-TPE for rectal primary and recurrent and anal cancers [21]. Nevertheless, details of procedure time, blood loss, and duration of admission for Ta/Tp-TPE have not been addressed to date. Our case series focused on the benefits of a simultaneous two-team approach and demonstrated the potential of decreasing blood loss and operation time. The median operative time and blood loss were lower in our study than those of other studies, in which values ranged from 565.2 to 935 min and 547.3 to 930 ml, respectively. Moreover, in these previous studies, the postoperative complication rates and the mean postoperative hospitalization ranged from 36.4% to 66.7% and 15.3 to 29 days, respectively [2, 18,19,20]. Although we cannot directly compare our results with those of other published studies, it appears that the two-team Ta PE approach with laparoscopic assistance may potentially reduce the operation time, blood loss, and hospital stay, by preventing serious complications.
Postoperative urological complications such as urinary tract infection, leakage, and stenosis are the most common in patients having PE; therefore, careful reconstruction is required. In cases with TPE, cystectomy followed by reconstruction with an ileal conduit is a primary option, a procedure associated with relatively few urological complications [22] and no serious urinary tract complications were observed in any of the patients in our series.
Although all patients examined in this cohort had mrT4 tumors, only three (50%) were found to have pT4b tumors on pathological examination. In non-responders to adjuvant therapy, extended-TME is associated with a high risk of recurrence. It is, therefore, important to select a procedure beyond TME, such as extra-levator abdominoperineal excision (ELAPE), PPE, or TPE [23]. In our study, ELAPE was not considered since preoperative MRI did not show levator muscle or anal canal involvement. We also observed that R0 resection and securing CRM could be achieved in all patients who had two-team surgery. The results of a meta-analysis for oncological outcomes showed that patients who had TaTME have a significantly higher rate of complete specimens, increased distance from the tumor to CRM, and less positive CRM involvement [24].
In contrast, there are some reports of multifocal recurrence peculiar to TaTME; thus, it is necessary to pay sufficient attention to its adaptation and the handling of the rectal stump [25]. The Ta approach is an MIS that can provide an excellent surgical field with adequate magnified scope vision in all directions; therefore, it provides a significant advantage for securing a CRM. The median distance of distal resection in our study was reasonably adequate. Additionally, it is easier to dissect the pelvic outer frame, such as the pelvic fascia, sacral periosteum, and pelvic floor muscles, via the anal side than through the abdominal approach [26]. However, the advantages of the Ta approach may be associated with certain complications; for instance, it may be difficult to return to the optimal layer after traversing a deeper layer during dissection. With the two-team method employed in the current study, the view and surgical lighting from the abdominal side served as a guide for the perineal team to select the appropriate layer for a safe dissection.
Furthermore, anal preserving TPE is considered a useful approach from the viewpoint of preserving anal function, and in terms of reduction of the pelvic dead space after pelvic exenteration that lowers the risk of infection.
There were several limitations to the present study. First, few patients were enrolled. Second, this study was retrospectively conducted at a single institution. Finally, the long-term outcomes need further evaluation to verify the feasibility and efficacy of a two-team Ta PE MIS in locally advanced rectal cancer cases. Nevertheless, this is the first study to show that a two-team Ta PE approach is a safe and feasible technique and may potentially improve surgical outcomes in both sexes.
Conclusions
Our results showed that laparoscopic-assisted Ta PE is an acceptable procedure that enables R0 resection in patients with locally advanced rectal cancer. This method may potentially overcome the current difficulties associated with such surgical procedures and improve patient outcomes.
Data availability
Not applicable.
Code availability
Not applicable.
References
Akiyoshi T, Nagasaki T, Ueno M (2015) Laparoscopic total pelvic exenteration for locally recurrent rectal cancer. Ann Surg Oncol 22:3896
Uehara K, Nakamura H, Yoshino Y, Arimoto A, Kato T, Yokoyama Y, Ebata T, Nagino M (2016) Initial experience of laparoscopic pelvic exenteration and comparison with conventional open surgery. Surg Endosc 30:132–138
Melich G, Hong YK, Kim J, Hur H, Baik SH, Kim NK, Sender Liberman A, Min BS (2015) Simultaneous development of laparoscopy and robotics provides acceptable perioperative outcomes and shows robotics to have a faster learning curve and to be overall faster in rectal cancer surgery: analysis of novice MIS surgeon learning curves. Surg Endosc 29:558–568
Heald RJ (2013) A new solution to some old problems: transanal TME. Tech Coloproctol 17:257–258
Rouanet P, Mourregot A, Azar CC, Carrere S, Gutowski M, Quenet F, Saint-Aubert B, Colombo PE (2013) Transanal endoscopic proctectomy: an innovative procedure for difficult resection of rectal tumors in men with narrow pelvis. Dis Colon Rectum 56:408–415
Dumont F, Goéré D, Honoré C, Elias D (2012) Transanal endoscopic total mesorectal excision combined with single-port laparoscopy. Dis Colon Rectum 55:996–1001
Emhoff IA, Lee GC, Sylla P (2014) Transanal colorectal resection using natural orifice translumenal endoscopic surgery (NOTES). Dig Endosc 26:29–42
Sohn DK, Park SC, Kim MJ, Chang HJ, Han KS, Oh JH (2019) Feasibility of transanal total mesorectal excision in cases with challenging patient and tumor characteristics. Ann Surg Treat Res 96:123–130
Uematsu D, Akiyama G, Sugihara T, Magishi A, Yamaguchi T, Sano T (2017) Transanal total pelvic exenteration: pushing the limits of transanal total mesorectal excision with transanal pelvic exenteration. Dis Colon Rectum 60:647–648
Uematsu D, Akiyama G, Sugihara T, Magishi A, Ono K, Yamaguchi T, Sano T (2019) Transperineal total pelvic exenteration in the prone jackknife position. Dis Colon Rectum 62:1135
de’Angelis N, Landi F, Vitali G.C, Memeo R, Martínez-Pérez A, Solis A, Assalino M, Vallribera F, Mercoli H.A, Marescaux J, Mutter D, Ris F, Espin E, Brunetti F (2017) Multicentre propensity score-matched analysis of laparoscopic versus open surgery for T4 rectal cancer. Surg Endosc 31:3106–3121
de Lacy FB, van Laarhoven JJEM, Pena R, Arroyave MC, Bravo R, Cuatrecasas M, Lacy AM (2018) Transanal total mesorectal excision: pathological results of 186 patients with mid and low rectal cancer. Surg Endosc 32:2442–2447
Zhang X, Gao Y, Dai XL, Zhang HT, Shang ZJ, Cai XY, Shen T, Cheng XS, Yu K, Li YF (2019) Short- and long-term outcomes of transanal versus laparoscopic total mesorectal excision for mid-to-low rectal cancer: a meta-analysis. Surg Endosc 33:972–985
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Brunschwig A (1949) Complete excision of pelvic viscera in the male for advanced carcinoma of the sigmoid invading the urinary bladder. Ann Surg 129:499–504
López-Basave HN, Morales-Vásquez F, Herrera-Gómez Á, Rosciano AP, Meneses-García A, Ruiz-Molina JM (2012) Pelvic exenteration for colorectal cancer: oncologic outcome in 59 patients at a single institution. Cancer Manag Res 4:351–356
Platt E, Dovell G, Smolarek S (2018) Systematic review of outcomes following pelvic exenteration for the treatment of primary and recurrent locally advanced rectal cancer. Tech Coloproctol 22:835–845. https://doi.org/10.1007/s10151-018-1883-1
Yang K, Cai L, Yao L, Zhang Z, Zhang C, Wang X, Tang J, Li X, He Z, Zhou L (2015) Laparoscopic total pelvic exenteration for pelvic malignancies: the technique and short-time outcome of 11 cases. World J Surg Oncol 13:301
Ogura A, Akiyoshi T, Konishi T, Fujimoto Y, Nagayama S, Fukunaga Y, Ueno M (2016) Safety of laparoscopic pelvic exenteration with urinary diversion for colorectal malignancies. World J Surg 40:1236–1243
Ichihara M, Uemura M, Ikeda M, Miyake M, Kato T, Hamakawa T, Maeda S, Hama N, Nishikawa K, Miyamoto A, Miyazaki M, Hirao M, Sekimoto M (2019) Safety and feasibility of laparoscopic pelvic exenteration for locally advanced or recurrent colorectal cancer. Surg Laparosc Endosc Percutan Tech 29:389–392
Mehta AM, Hellawell G, Burling D et al (2018) Transperineal retropubic approach in total pelvic exenteration for advanced and recurrent colorectal and anal cancer involving the penile base: technique and outcomes. Tech Coloproctol 22:663–671. https://doi.org/10.1007/s10151-018-1852-8
S K.M (2017) Total Pelvic Exenteration for Locally Advanced and Recurrent Rectal Cancer: Urological Outcomes and Adverse Events. Eur Urol Focus 6–11
Denost Q, Kontovounisios C, Rasheed S, Chevalier R (2017) Individualizing surgical treatment based on tumour response following neoadjuvant therapy in T4 primary rectal cancer. Eur J Surg Oncol 43:92–99
Ma B, Gao P, Song Y, Zhang C, Zhang C, Wang L, Liu H (2016) Wang Z (2016) Transanal total mesorectal excision (taTME) for rectal cancer : a systematic review and meta-analysis of oncological and perioperative outcomes compared with laparoscopic total mesorectal excision. BMC Cancer 4(16):380
Wasmuth H.H, Færden A.E, Myklebust T, Pfeffer F, Norderval S, Riis R, Olsen O.C, Lambrecht J.R, Kørner H, Larsen S.G, Forsmo H.M, Bækkelund O, Lavik S, Knapp J.C, Sjo O, Rashid G (2019) Transanal total mesorectal excision for rectal cancer has been suspended in Norway. Br J Surg:121–130.
Yasukawa D, Hori T, Kadokawa Y, Kato S, Aisu Y, Hasegawa S (2019) Trans-perineal minimally invasive surgery during laparoscopic abdominoperineal resection for low rectal cancer. Surg Endosc 33:437–447
Funding
Not applicable.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
All procedures performed in the study involving human participants were in accordance with the ethical standards of the Trust and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from all patients for publication of the accompanying images.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 447002 kb)
Rights and permissions
About this article
Cite this article
Nonaka, T., Tominaga, T., Akazawa, Y. et al. Feasibility of laparoscopic-assisted transanal pelvic exenteration in locally advanced rectal cancer with anterior invasion. Tech Coloproctol 25, 69–74 (2021). https://doi.org/10.1007/s10151-020-02324-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-020-02324-4