Abstract
Purpose
Posterior pelvic exenteration (PPE) for locally advanced rectal cancer is a technical and challenging procedure. The safety and feasibility of laparoscopic PPE remain to be determined. This study aims to compare short-term and survival outcomes of laparoscopic PPE (LPPE) with open PPE (OPPE) in female patients.
Method
From January 2015 to December 2020, data from 105 female patients who underwent PPE at three institutions were retrospectively analyzed. The short-term and oncological outcomes between LPPE and OPPE were compared.
Results
A total of 54 cases with LPPE and 51 cases with OPPE were enrolled. The operative time (240 vs. 295 min, p = 0.009), blood loss (100 vs. 300 ml, p < 0.001), surgical site infection (SSI) rate (20.4% vs. 58.8%, p = 0.003), urinary retention rate (3.7% vs. 17.6%, p = 0.020), and postoperative hospital stay (10 vs. 13 days, p = 0.009) were significantly lower in the LPPE group. The two groups showed no significant differences in the local recurrence rate (p = 0.296), 3-year overall survival (p = 0.129), or 3-year disease-free survival (p = 0.082). A higher CEA level (HR 1.02, p = 0.002), poor tumor differentiation (HR 3.05, p = 0.004), and (y)pT4b stage (HR 2.35, p = 0.035) were independent risk factors for disease-free survival.
Conclusion
LPPE is safe and feasible for locally advanced rectal cancers and shows lower operative time and blood loss, fewer SSI complications, and better preservation of bladder function without compromising oncological outcomes.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Posterior pelvic exenteration (PPE) is more frequently reported in gynecological tumors [1,2,3], and PPE for rectal cancers has received less attention in terms of both surgical techniques and oncological outcomes. With the popularization of and advancements in early diagnosis and neoadjuvant therapy, the incidence of locally advanced rectal cancer (LARC) has decreased. Because of the unique anatomical characteristics of female patients, the possibility of total pelvic exenteration (TPE) is relatively rare, while combined resection of the uterus and vagina is more common. Therefore, a study focusing on PPE for female patients with LARC is essential.
The short-term advantages of laparoscopic rectal cancer resection and long-term oncological outcomes that are not compromised have been confirmed in multiple prospective multicenter controlled studies [4,5,6,7]. However, all studies excluded patients with clinical stage T4 (cT4) tumors. Recently, with advancements in laparoscopic technology and application of high-definition laparoscopy and high-energy devices, an increasing number of laparoscopic posterior pelvic exenteration (LPPE) procedures have been reported in the field of gynecological tumors [8], but only a few reports with small sample sizes or just case reports have described the use of LPPE procedures in rectal cancers [9,10,11]. Moreover, the long-term oncological outcomes of LPPE remain unclear, and PPE is more challenging than TPE for R0 resection because of organ preservation.
In this cohort study from China PelvEx collaborative, we conducted a comparative study of the surgical results and oncological outcomes between LPPE and OPPE for female patients with LARC. We also evaluated prognostic factors for PPE.
Patients and methods
Study design and participants
This was a multicenter, retrospective study from a prospectively collected institutional database and tumor registry for female patients with LARC at three institutions of the China PelvEx collaborative between January 2015 to December 2020. Consecutive female patients with LARC undergoing PPE were identified. The inclusion criteria were as follows: (1) radical resection; (2) female patients with LARC (cT4b); (3) histologically proven adenocarcinoma. The exclusion criteria were as follows: (1) total pelvic exenteration (TPE); (2) patients with simultaneous distant metastasis; (3) patients with recurrent rectal cancer; (4) proctectomy with oophorectomy; (5) PPE with sacrectomy. Preoperative multidisciplinary consultations were performed for all patients. Multidisciplinary consultations included colorectal surgery, medical oncology, radiotherapy, gynecology, urology, and plastic surgery. Treatment strategies for each patient such as the choice of surgical approach (open or laparoscopic) and whether preoperative chemoradiotherapy was performed were determined by multidisciplinary team meetings (MDT). We determined the surgical procedure also on the basis of the laparoscopic exploration. All patients provided written informed consent, and the study was approved by the Ethics Committee of Cancer Hospital, Chinese Academy of Medical Sciences, Peking University First Hospital, and Gansu Provincial Hospital (ethical approval number 22/442-3644).
Preoperative management
Preoperative multidisciplinary consultation was performed for all patients. Neoadjuvant chemoradiotherapy (nCRT) was suggested for patients with clinical stage T4b disease. We used a standard, long course regimen of 5-fluorouracil (5-FU)-based chemotherapy with a total dose of 45–54 Gy of external beam radiation. After nCRT, patients were reassessed using pelvic MRI. Surgery was performed approximately 6–12 weeks after nCRT.
Definitions
To date, there is no definition of PPE that is universally agreed upon. Some scholars still propose the definition in gynecological tumors for rectal cancer surgery [12,13,14], while others use the definite invasion of coccyx, presacral fascia, retrosacral space, and sacrum as PPE [15, 16]. In this study, the following definitions were used:
LARC: Those that are predicted by MRI to require an extended surgical resection beyond the total mesorectal plane to achieve an R0 resection.
PPE: Defined as the removal of the reproductive organs and rectum, sparing the bladder.
Pathological resection margin status: R0, microscopically clear resection margins of at least 1 mm; R1, microscopically involved resection margin with tumor within 1 mm of the resection margin; R2, macroscopically involved resection margin.
Overall survival (OS): The time from the date of surgery to the date of death from any cause.
Disease free survival (DFS): The time from the date of surgery to the date of pelvic recurrence and/or distant disease or death due to pelvic recurrence and/or distant disease.
Local recurrence (LR): Defined as tumor regrowth within the pelvis, perineum, or a para-anastomosis location, while any other recurrence was defined as distant metastasis.
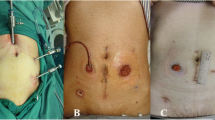
Surgical procedure
All surgical procedures were performed by three surgeons (XW, BD, and JT) with more than 10 years of experience in performing OPPE and LPPE and at least 1000 cases of rectal cancer resection. After induction of general anesthesia, the patient was placed in a modified lithotomy, 30° Trendelenburg position, and five ports were placed according to routine practice for laparoscopic proctectomy. The surgeon stood on the patient’s right, the first assistant on the left, and the second assistant on the cranial side. A monitor was placed next to the patient’s left foot. A pneumoperitoneum was created at a pressure of 14 mmHg. The surgical procedure was generally similar in the three institutions and open or laparoscopic PPE was performed in line with previously reported methods [17, 18].
The procedure began with medial-to-lateral dissection of the rectosigmoid to the lateral abdominal wall, followed by mesorectal excision, paying attention to protect the hypogastric nerves and pelvic plexus. The retrorectal space was dissected 5 cm beyond the edge of the tumor or until the levator ani muscle was exposed. The pararectal spaces were dissected on both sides after dissection of the lateral and middle rectal arteries. The infundibulopelvic ligament with the ovarian vascular pedicle and round ligament were identified and cut. The anterior perineal and vesicovaginal spaces were dissected to expose the anterior vaginal walls. The parametrial tissue and paracolpium were excised without damaging the inferior hypogastric plexus after sealing the uterine vessels adjacent to the cervix using a bipolar coagulation system. The removal of vaginal wall depends on the extent of invasion, and the vaginal stump was sutured with V-Loc absorbable suture or reconstructed with V–Y plasty [19]. The decision whether to complete anterior resection or abdominal perineal resection depends on the tumor site and length of the residual rectum.
Follow-up
Data for various clinicopathological parameters, including age, body mass index (BMI), American Society of Anesthesiologists (ASA) score, neoadjuvant treatment, tumor size, pathologic stage, serum hemoglobin (Hb), albumin (Alb), carcinoembryonic antigen (CEA), and carbohydrate antigen 19-9 (CA19-9) levels as well as perioperative results, including operative time, conversion to open surgery, blood loss, and postoperative complications were collected. Complications were assessed according to the Clavien–Dindo classification [20]. Minor surgical morbidity was defined as grade I or II, and major morbidity was defined as grade III, IV, or V. Patients were followed up regularly. All patients were followed up by phone or at the outpatient department every 3 months in the first year after the operation, every 6 months in the second year, and at least once a year thereafter. Follow-up was till patient’s death or December 1, 2022. The primary endpoint was 3-year DFS. The secondary endpoints were surgical complications.
Statistical analysis
IBM SPSS Statistics 25 (IBM, Inc., Armonk, NY, USA) was used for statistical analyses. Pearson’s Chi-square and Fisher’s exact tests were used to compare categorical variables. The Mann–Whitney U test or Student’s t test was used for continuous variables. The probabilities of local recurrence rate (LRR), OS, and DFS were assessed using the Kaplan–Meier method, and differences were compared using the log-rank test for statistical significance. Statistically significant variables in the univariate analysis were subsequently tested by multivariable analysis using a Cox regression model. Statistical significance was set at p < 0.05.
Results
Patient characteristics
A total of 157 consecutive female patients who underwent pelvic exenteration (PE) were identified. Thirteen cases who underwent total pelvic exenteration (TPE), 15 with Krukenberg tumor invading the rectum, and 10 with other metastasis were excluded. Finally, 105 patients (54 with LPPE and 51 with OPPE) were enrolled in study. A flowchart of the study is shown in Fig. 1. The baseline patient characteristics are summarized in Table 1. nCRT was performed in 31 out of 105 patients, of which only 1 patient had pathological complete response. The LPPE and OPPE groups showed no significant differences in age, BMI, ASA score, comorbidities, neoadjuvant therapy, tumor size, tumor differentiation, (y)pT4b stage, (y)pN+ stage, history of abdominal surgery, and laboratory test results. In the entire cohort, the proportion of cases showing (y)pT4b stage was 63.8% (67/105).
Perioperative and pathological results
The intraoperative data and pathologic results are shown in Table 2. None of the patients in the LPPE group required conversion to open surgery. The median operative time in the LPPE group was significantly shorter (240 vs. 295 min, p = 0.009). The median intraoperative blood loss in the LPPE group was significantly less (100 vs. 300 ml, p < 0.001). The two groups showed no significant differences in the number of retrieved lymph nodes, positive lymph nodes, colorectal reconstruction, and vaginal reconstruction. The negative rate of circumferential resection margin (CRM) in the LPPE group was 94.4%, more than 84.3% in the OPPE group, while the difference was not statistically significant (p = 0.090).
Postoperative recovery and complications
Data for postoperative convalescence and complications are shown in Table 3. No mortality occurred in either of the groups. The total in-hospital complication rate was 39.0% (41/105). The total surgical site infection (SSI) rate was 13.3% (14/105). The two groups showed no significant differences in the major complication rate (3/54 vs. 4/51, p = 0.938) or reoperation rate (2/54 vs. 3/51, p = 0.672). The overall postoperative complication rate (11/54 vs. 30/51, p < 0.001) and SSI complication rate (including abdominal incision, perineal incision, and pelvic and urinary infection, 2/54 vs. 12/51, p = 0.003) were both significantly lower in the LPPE group. The total colorectal anastomotic leakage rate was 10.5% (6/57). Both LPPE and OPPE groups had three cases of colorectal anastomotic leakage (3/27 vs. 3/30, p = 1.000). The rate of urinary retention was significantly lower in the LPPE group (2/54 vs. 9/51, p = 0.020). The time to first flatus (2 vs. 3 days, p = 0.001), time to first liquid diet intake (3 vs. 4 days, p = 0.001), and postoperative hospital stay (10 vs. 13 days, p = 0.009) were significantly shorter in the LPPE group.
Oncological outcomes
The median follow-up period was 41 months (interquartile range 19–63 months) in the entire cohort, 38 months (interquartile range 15–52 months) in the LPPE group, and 46 months (interquartile range 20–94 months) in the OPPE group. The two groups showed no significant differences in the rate of LRR, OS, and DFS (Fig. 2a–c). The 3-year LRR in the LPPE and OPPE groups were 19.2% and 26.9%, respectively. The 3-year OS were 76.3% and 64.4% and 3-year DFS were 63.8% and 48.3% in the LPPE and OPPE groups, respectively.
Univariate and multivariable analyses of the prognostic factors influencing OS and DFS are presented in Table 4. In the univariate analysis, higher CEA level and CA19-9 level, poor differentiation, (y)pT4b and N1–2 significantly affected both OS and DFS (p < 0.05). Positive CRM also significantly affected OS (p < 0.05). Multivariable analysis revealed that higher CEA levels (HR 1.02, 95% CI 1.01–1.03; p = 0.002) and poor differentiation (HR 3.05, 95% CI 1.43–6.52; p = 0.004) were independent risk factors for OS. For DFS, higher CEA level (HR 1.02, 95% CI 1.01–1.03; p < 0.001), poor differentiation (HR 2.96, 95% CI 1.41–6.18; p = 0.004), and (y)pT4b stage 0 (HR 2.35, 95% CI 1.06–5.19; p = 0.035) were independent risk factors.
Discussion
PPE has been reported more frequently in cases of advanced gynecological tumors such as ovarian cancer, cervical cancer, and vaginal tumors [8, 21,22,23,24,25]. For rectal cancers, it is not common to focus only on PPE, which is usually analyzed and discussed together with TPE [26,27,28], and the understanding of PPE is usually insufficient among colorectal surgeons. As a result of the specific anatomy of the female pelvis, the indications of TPE for LARC invading the bladder are less common. In this series, TPE represented only 3.4% of PE cases. Therefore, it is necessary to further elaborate the surgical techniques, postoperative complications, and survival outcomes of PPE in female patients. In recent years, the popularity of laparoscopic techniques and technological advances in instrumentation, such as higher-resolution magnified views, the da Vinci surgical system, and energy platforms, have broadened its use and made more complex and extensive surgeries possible [1, 29,30,31,32,33]. Most reports about LPPE involve gynecologic surgery. Some colorectal surgeons have shown that LPPE for LARC is feasible with less morbidity and acceptable short-term outcomes; however, the sample size was small (less than 10 cases) [11]. To date, there is still a lack of surgical and oncological evidence for LPPE in comparison with traditional OPPE. In this comparative study from China PelvEx collaborative, 54 cases of LPPE and 51 cases of OPPE were enrolled, which, to the best of our knowledge, makes it the first and largest comparative study between LPPE and OPPE. Our study showed that LPPE can be selectively implemented by experienced surgeons with lower operative time, blood loss, and SSI, better preservation of bladder function, and quicker postoperative convalescence without compromising oncological outcomes.
An important indicator for evaluating the quality of surgery is the R0 resection rate [34]. Unlike TPE, PPE can be performed as an organ-sparing surgery that preserves the integrity of the bladder and its innervating nerves. Therefore, in some respects, R0 resection in PPE is more difficult than in TPE. In PPE, to preserve the bladder and pelvic plexus nerves, the dissecting plane may be closer to the parametrial tissue and paracolpium, thus affecting R0 resection. Although the difference in positive CRM rates between LPPE and OPPE was not significant (3/54 vs. 8/51, p = 0.090), as the number of cases increased, it may be practicable for the laparoscopic group to obtain a safer CRM. Therefore, patients in the LPPE group are likely to have better survival expectations. The experience of the laparoscopic technique in lateral lymph node dissection (LLND) made us more familiar with the anatomic structure in the lateral pelvic compartment and the lateral dissecting line shifting from the total mesorectal excision (TME) plane to the parietal pelvic fascia plane. The uterine vessels were dissected at the root of the inner iliac artery, and more lymph adipose tissue around the paracolpium was cleared. Moreover, meticulous dissection in the narrow pelvis under laparoscopy also helped determination of the invaded boundary and facilitated proper decision-making.
In comparison with other studies on the short-term advantages of laparoscopy, the time to first flatus, time to first liquid diet, and intraoperative blood loss in the LPPE group were significantly lower than those in the OPPE group. Although the two groups showed no significant differences in the overall and major complications, the rates of postoperative infectious complications (2/54 vs. 12/51, p = 0.003) and urinary retention (2/54 vs. 9/51, p = 0.020) were lower in the LPPE group. These results were consistent with those of other studies on LLND in laparoscopic or robotic surgery. The concerns regarding techniques for LPPE can be summarized as follows: First, the bilateral hypogastric nerve and neurovascular bundle should be carefully preserved when dissecting the retrorectal and pararectal space according to the principle of TME. Second, the inferior hypogastric plexus should be isolated from the lateral vaginal wall and the branches to the vagina should be dissected while preserving the vesical branches. Third, meticulous dissection and a magnified view of the narrow pelvis under laparoscopy are more favorable for plexus preservation.
The LPPE and OPPE groups showed no significant differences in oncological outcomes, including the LRR, OS, and DFS. The DFS in the LPPE group was higher than that in the OPPE group, although the difference was not statistically significant (p = 0.082). On the one hand, the lower positive CRM rate in LPPE may be favorable for better LRR and DFS. More precise dissection under laparoscopy might facilitate more thorough radical resection of the tumor. Thus, more cases, a longer follow-up period, and a case-matched comparison are needed in further studies to confirm the oncological outcomes of LPPE.
The limitations of this study are related to the retrospective study design, patient selection bias, and the relatively shorter follow-up duration in the LPPE group. Second, with the improvement of surgical technology, the update of laparoscopic equipment, the proportion of laparoscopic surgery has gradually increased, and the enrollment of cases cannot be completely consistent in time. Third, the limited data on the evaluation of bladder function may have affected the results, and whether the results apply to male patients will be clarified through further research. Lastly, less than a third of LARC received nCRT, which may introduce bias into the neoadjuvant role on survival analysis. Nevertheless, this study introduced the largest series of LPPE to date, and is the first to evaluate the surgical results and oncological outcomes between LPPE and OPPE.
Conclusion
Our results showed that LPPE is safe and feasible for selected LARC cases in female patients when performed by highly skilled surgeons, presenting a shorter operative time, less blood loss, lower surgical site infection, better preservation of bladder function, and quicker postoperative recovery without compromising the oncological outcomes. Further studies with a larger sample size and a longer follow-up period are needed to corroborate our findings.
Data availability
The database is available if properly requested and can be directly addressed to the corresponding author’s email address.
References
Cianci S, Arcieri M, Vizzielli G et al (2021) Robotic pelvic exenteration for gynecologic malignancies, anatomic landmarks, and surgical steps: a systematic review. Front surg 8:790152
Tortorella L, Casarin J, Mara KC et al (2019) Prediction of short-term surgical complications in women undergoing pelvic exenteration for gynecological malignancies. Gynecol Oncol 152:151–156
Houvenaeghel G, Gutowski M, Buttarelli M et al (2009) Modified posterior pelvic exenteration for ovarian cancer. Int J Gynecol Cancer 19:968–973
Bonjer HJ, Deijen CL, Abis GA et al (2015) A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med 372:1324–1332
Jeong SY, Park JW, Nam BH et al (2014) Open versus laparoscopic surgery for mid-rectal or low-rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): survival outcomes of an open-label, non-inferiority, randomised controlled trial. Lancet Oncol 15:767–774
Hida K, Okamura R, Sakai Y et al (2018) Open versus laparoscopic surgery for advanced low rectal cancer: a large, multicenter, propensity score matched cohort study in Japan. Ann Surg 268:318–324
Vennix S, Pelzers L, Bouvy N et al (2014) Laparoscopic versus open total mesorectal excision for rectal cancer. Cochrane Database Syst Rev. 4:5200
Puntambekar S, Rajamanickam S, Agarwal G et al (2011) Laparoscopic posterior exenteration in advanced gynecologic malignant disease. J Minim Invasive Gynecol 18:59–63
Fujimoto T, Tanuma F, Otsuka N et al (2019) Laparoscopic posterior pelvic exenteration for primary adenocarcinoma of the rectovaginal septum without associated endometriosis: a case report. Mol clin oncol 10:92–96
Zhou H, Shi Y, Wu Y et al (2022) Laparoscopic posterior pelvic exenteration and total vaginectomy for rectal squamous cell carcinoma: a video vignette. Colorectal Dis 24:1259
Pokharkar A, Bankar S, Rohila J et al (2020) Laparoscopic posterior pelvic exenteration (complete and supralevator) for locally advanced adenocarcinoma of the rectum in females: surgical technique and short-term outcomes. J Laparoendosc Adv Surg Tech A 30:558–563
Yang TX, Morris DL, Chua TC (2013) Pelvic exenteration for rectal cancer: a systematic review. Dis Colon Rectum 56:519–531
Kazi M, Kumar NAN, Rohila J et al (2021) Minimally invasive versus open pelvic exenterations for rectal cancer: a comparative analysis of perioperative and 3-year oncological outcomes. BJS Open. 5(5):074
Tang J, Liu J, Du B et al (2022) Short- and long-term outcomes of laparoscopic versus open pelvic exenteration for locally advanced rectal cancer: a single-center propensity score matching analysis. Tech Coloproctol 27:43
PelvEx Collaborative (2019) Surgical and survival outcomes following pelvic exenteration for locally advanced primary rectal cancer: results from an international collaboration. Ann Surg 269(2):315–321
Koh CE, Solomon MJ, Brown KG et al (2017) The evolution of pelvic exenteration practice at a single center: lessons learned from over 500 cases. Dis Colon Rectum 60(6):627–635
Pokharkar A, Bankar S, Rohila J et al (2020) Laparoscopic posterior pelvic exenteration (complete and supralevator) for locally advanced adenocarcinoma of the rectum in females: surgical technique and short-term outcomes. J Laparoendosc Adv Surg Tech A 30(5):558–563
Moriya Y, Isgiguro S (2013) Pelvic exenteration: total/anterior/posterior. In: Khatri VP (ed) Atlas of advanced operative surgery. Elsevier, Philadelphia, pp 438–446
Westra I, Huisinga RL, Dunker MS et al (2020) Combined use of a petal flap and V-Y advancement flap for reconstruction of presacral defects following rectal resection. Tech Coloproctol 24:593–597
Clavien PA, Barkun J, de Oliveira ML et al (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250:187–196
Houvenaeghel G, de Nonneville A, Blache G et al (2022) Posterior pelvic exenteration for ovarian cancer: surgical and oncological outcomes. J Gynecol Oncol 33:e31
Minar L, Felsinger M, Rovny I et al (2017) Modified posterior pelvic exenteration for advanced ovarian malignancies: a single-institution study of 35 cases. Acta Obstet Gynecol Scand 96:1136–1143
Kato K, Nishikimi K, Tate S, Kiyokawa T, Shozu M et al (2015) Histopathologic tumor spreading in primary ovarian cancer with modified posterior exenteration. World J Surg Oncol. 13:230
Kato K, Tate S, Nishikimi K et al (2013) Bladder function after modified posterior exenteration for primary gynecological cancer. Gynecol Oncol 129:229–233
Revaux A, Rouzier R, Ballester M et al (2012) Comparison of morbidity and survival between primary and interval cytoreductive surgery in patients after modified posterior pelvic exenteration for advanced ovarian cancer. Int J Gynecol Cancer 22:1349–1354
Gheorghe M, Cozlea AL, Kiss SL et al (2021) Primary pelvic exenteration: our experience with 23 patients from a single institution. Exp Ther Med 22:1060
Yang K, Cai L, Yao L et al (2015) Laparoscopic total pelvic exenteration for pelvic malignancies: the technique and short-time outcome of 11 cases. World J Surg Oncol 13:301
Ghouti L, Pereira P, Filleron T et al (2015) Pelvic exenterations for specific extraluminal recurrences in the era of total mesorectal excision: is there still a chance for cure?: a single-center review of patients with extraluminal pelvic recurrence for rectal cancer from March 2004 to November 2010. Am J Surg 209:352–362
Sun Y, Yang HJ, Zhang ZC et al (2021) Fascial space priority approach for laparoscopic supralevator posterior pelvic exenteration with nerve sparing: anatomy and technique. Tech Coloproctol 25:747–748
Kondo A, Nishizawa Y, Tsunemori H et al (2019) Use of a linear stapler for urethral and dorsal vein complex transection during laparoscopic total pelvic exenteration in rectal cancer. Tech Coloproctol 23:487–490
Khadraoui W, Zeybek B, Mutlu L et al (2019) Robotic type II B posterior exenteration for recurrent vaginal cancer. Gynecol Oncol 155:384–385
Kammar P, Sasi S, Kumar N et al (2019) Robotic posterior pelvic exenteration for locally advanced rectal cancer - a video vignette. Colorectal Dis 21:606
Maurice MJ, Ramirez D, Gorgun E et al (2017) Robotic total pelvic exenteration with intracorporeal sigmoid conduit and colostomy: step-by-step technique. Urology 105:6–8
Simillis C, Baird DL, Kontovounisios C et al (2017) A systematic review to assess resection margin status after abdominoperineal excision and pelvic exenteration for rectal cancer. Ann Surg 265:291–299
Acknowledgements
The authors thank all members and staff in the China PelvEx collaborative for collecting data.
Funding
This study was supported by grants from the National Natural Science Foundation of China (No. 81903023, 82072732), Beijing Natural Science Foundation (L222054) and Wu Jieping’s Foundation Special for Clinical Research (No. 320.6750.2021-04-02).
Author information
Authors and Affiliations
Contributions
All authors contributed to the conception and design of the study. Material preparation, data collection, and analyses were performed by MZ, HC, JL, SM, XW, and JT. JT and XW wrote the first draft of the manuscript. All authors commented on the previous versions of the manuscript. All authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
All work was carried out in compliance with the Ethical Principles for Medical Research Involving Human Subjects outlined in the Helsinki Declaration in 1975 (revised in 2000). The study was approved by the Ethics Committee of Cancer Hospital, Chinese Academy of Medical Sciences, Peking University First Hospital, and Gansu Provincial Hospital (ethical approval number 22/442-3644).
Informed consent
All patients provided written informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhuang, M., Chen, H., Li, Y. et al. Laparoscopic posterior pelvic exenteration is safe and feasible for locally advanced primary rectal cancer in female patients: a comparative study from China PelvEx collaborative. Tech Coloproctol 27, 1109–1117 (2023). https://doi.org/10.1007/s10151-023-02824-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-023-02824-z