Abstract
Background
Laparoscopic right hemicolectomy (LRHC) is increasingly performed for the treatment of right colon disease. Nevertheless, standardization of the surgical technique regarding the performance of intracorporeal (IC) or extracorporeal (EC) anastomosis is lacking. The purpose of this study was to compare short-term postoperative outcomes in patients who had laparoscopic right colectomy either with IC or EC.
Methods
This was a retrospective, non-randomized and multicenter study conducted from January 2005 to December 2015 on the CLIMHET study group cohort from five tertiary centers in France. Data were collected for all patients with LRHC to compare patient characteristics, intraoperative data and postoperative outcomes in terms of medical and surgical complications, duration of hospitalization and mortality. A multivariate analysis was performed to compare the results in the two groups.
Results
Of the 597 patients undergoing LRHC, 150 had IC and 447 had EC. The incidence of medical complications (cardiac, vascular, and pulmonary complications) was lower in the IC group than in the EC group (13 vs 20%, p = 0.049). This difference remained significant in multivariate analysis after adjusting to field characteristics and patient histories (p = 0.009). Additionally, a shorter hospital stay (7 vs 8 days, p = 0.003) was observed in the IC group as compared to the EC group. This difference remained significant in favor of the IC group in multivariate analysis (p = 0.029). There was no difference between the groups as regards: surgical complications (p = 0.76), time of mobilization (p = 0.93), reintervention rate (p = 1) and 90-day mortality (p = 0.47).
Conclusions
Our results show that IC anastomosis in LRHC is associated with fewer medical complications and shorter hospital stays compared to EC anastomosis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Laparoscopic right hemicolectomy (LRHC) has gained general acceptance and is increasingly performed to treat benign and malignant colorectal disease, with oncological outcomes comparable to open surgery [1]. LRHC also improves postoperative recovery, with less postoperative pain, shorter hospital stay and decreased postoperative morbidity [1,2,3]. Nevertheless, standardization of the surgical technique for LRHC, in particular regarding the intracorporeal or extracorporeal ileocolic anastomosis, is lacking. The performance of intracorporeal or extracorporeal anastomoses in LRHC can involve broad variations of the procedure, ranging from a hand-assisted procedure, with hand-assisted dissection and mobilization of the specimen, to totally laparoscopic surgery. The first meta-analyses published, which included heterogeneous studies, reported no evidence regarding the benefits of intracorporeal (IC) versus extracorporeal (EC) anastomosis after LRHC in terms of postoperative morbidity [4]. However, more recent meta-analyses, reported a benefit for IC anastomosis concerning postoperative morbidity [5,6,7]. The purpose of the present retrospective, non-randomized, multicentric study was to compare the short-term postoperative results obtained in two homogeneous groups of patients undergoing LRHC in tertiary centers using either IC or EC anastomoses.
Materials and methods
Patients
The study population was retrieved from the CLIMHET Study Group database which included patients LRHC between January 2005 and December 2015 in five tertiary University Hospital centers in France (Clermont-Ferrand University Hospital, Strasbourg University Hospital-IRCAD, Henri-Mondor Hospital in Créteil, European Hospital Georges Pompidou in Paris, and Tours University Hospital). This study was conducted in accordance with the ethical principles determined by the Declaration of Helsinki. According to French law no formal ethics approval was required for this study.
For the present analyses, all patients who had had elective LRHC for colon cancer, inflammatory bowel disease or polyps located in the ascending colon (from the ileocecal valve to the right colonic flexure) were included. Patients with synchronous colon cancers, metastatic disease, locally advanced cancer requiring multivisceral resections or who had repeat surgery for a tumor recurrence were excluded. Conversion was defined as completion of the right colectomy procedure through either an enlarged incision or an abdominal incision of ≥ 6 cm, and when conversion was necessary, the patients were also excluded. Two groups were compared: laparoscopic right colectomy with IC or EC anastomosis.
The following variables were analyzed: age, sex, body mass index (BMI), obesity (BMI > 30 kg/m2), American Society of Anesthesiologists (ASA) score, smoking, diabetes mellitus, arteriopathy, coronaropathy, previous laparotomy or laparoscopy, American Joint Committee on Cancer (AJCC) staging, lesion location (e.g., caecum, ascending colon, right colonic flexure (= hepatic flexure), ileocaecal valve), operating time, anastomotic characteristics (e.g., manual or mechanical anastomosis), perioperative antibiotics, perioperative transfusions, and perioperative intravenous fluids.
Endpoints
Postoperative morbidity and mortality were defined as events occurring during the hospital stay or within 90 days after resection. Short-term outcomes included postoperative morbidity according to the Clavien–Dindo classification, 30-day postoperative severe morbidity (Clavien–Dindo ≥ 3), time to first flatus, postoperative ileus, length of hospital stay, anastomotic leak, anastomotic bleeding, wound infection and postoperative mortality [8].
Medical complications included cardiac, vascular, urinary and pulmonary events. All complications were assessed by a clinician and prospectively registered in the databases at discharge or during the first outpatient visit. Surgical complications included ileus, wound infections, anastomotic leakage and evisceration. Postoperative outcomes included the following: reintervention rate, time to resume a regular diet, time to first mobilization, time to flatus, time to the first stools, intensive care unit (ICU) stay, overall length of hospital stay, and the number of lymph nodes harvested.
Surgical techniques
Two standardized surgical techniques were performed and compared: IC and EC anastomosis. During the study period, the choice of technique was made according to the surgeon’s preference. The learning curve for either of these two surgical techniques was considered to be achieved after 30 procedures [9]. Under both approaches, the Veress needle technique was used to create pneumoperitoneum, and four ports in total were generally employed. The placement of the ports was the same for both approaches: two 12-mm ports were inserted in the left abdominal wall along the pararectal line (symmetrically, one below for a 30° camera and the other above the umbilicus) and a 10-mm port in median suprapubic position. A 5-mm assistant port was placed in the right hypochondrium (Fig. 1).
The first step consisted of exposing the vascular pedicles of the ileocolic trunk and right colic trunk; the right trunk of the medium colic pedicle was then ligated intracorporeally. The second step consisted of complete mobilization of the right colon and of the final ileal loop, performed in a medial-to-lateral manner. The Cattell-Braasch manoeuver was then performed; this consists in lowering the hepatic flexure after the incision of the colo-hepatic peritoneum and thus exposing the duodenum [10]. After the specimen was completely mobilized, the right colon and final ileal loop were transected using a linear stapler.
IC anastomosis
The IC anastomosis was performed using a stapler or with 4-0 absorbable sutures and the mesenteric breach was closed. The specimen was then completely mobilized and freed before extraction. The wound was then protected before extracting the specimen.
EC anastomosis
During EC construction of the anastomosis, after the protection of the abdominal wall, the specimen was extracted via an abdominal incision with subsequent extracorporeal bowel transsection.
The anastomosis was then performed either with a stapler or manual suture.
In the case of mechanical anastomosis, the enterotomy used to introduce the stapler was closed with sutures. An abdominal drain was not routinely inserted.
Perioperative management
No preoperative bowel preparation was performed. The patients were admitted in the afternoon of the day before the procedure. Deep venous prophylaxis with low-molecular-weight heparin (4000 IU) was started the evening before surgery and pursued until the postoperative day (POD) 30. Antibiotic prophylaxis with 2 g cefazolin and 500 mg metronidazole was administered before the induction of anesthesia. A nasogastric tube was always removed at the end if no longer required. The urinary catheter was generally removed on POD 1. No spinal anesthesia was associated with general anesthesia. Fluids were infused throughout the procedure at a rate of 10 ml/kg/h. All the centers were experts in enhanced recovery after surgery (ERAS).
Statistical analysis
For descriptive statistics, continuous variables are presented as medians (ranges) and categorical variables as numbers and percentages. Binary, multimodal and linear regression analyses were performed to control the effects of covariates on operative and postoperative outcomes; multivariate analyses included those variables which reached a significant p value under univariate analysis. In addition, a multivariate analysis of demographic, clinical and pathological variables was used to identify independent factors associated with the incidence of postoperative complications. A p value < 0.05 was considered to be significant.
Results
Demographic data
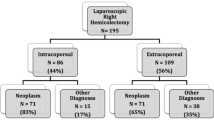
A total of 637 patients had LRHC between January 2005 and December 2015, 40 of whom were converted to open surgery and therefore excluded from this study. Therefore, 597 patients were included (Fig. 2).
There were 306 males and 291 females with a mean age of 69 years (range: 21–96 years). Their mean BMI was 25.4 kg/m2 (range: 15–45 kg/m2).
The indications for surgery were neoplasm in 451 cases (75.54%), including 1 patient with a neuroendocrine tumor, polyps in 93 cases (15.58%) cases, and inflammatory bowel disease in 53 cases (8.88%). Among the 451 right colon cancers, 43 were stage 0, 109 were stage I, 178 were stage II, and 120 were stage III according to the TNM classification [11].
Among patients having LRHC, lesions were located in the caecum in 244 (41%), 156 (26%) in the ascending colon in 156 (26%), 71 (12%) at the hepatic flexure in 71 (12%), 36 (6%) in the right transverse colon in 36 (6%), and 90 (15%) at the ileocæcal valve. Only three patients received neoadjuvant chemotherapy.
Both types of anastomosis were performed in each expert center, following the gradual introduction of the IC anastomosis technique since 2005. An IC anastomosis was performed in 150 patients (25.13%) and an EC anastomosis in 447 patients (74.87%). There were more males (p = 0.005) and a higher BMI (p = 0.003) in the IC group, but otherwise the patients in the two groups were demographically comparable (Table 1).
Intraoperative data
During IC anastomoses, a mechanical (88.67% versus 46.7%; p < 0.001), side-to-side (IC = 99.3%, EC = 88.6%; p < 0.001), isoperistaltic (IC 87.2%, EC = 45.8%; p < 0.001) anastomosis was generally performed.
During EC anastomoses, vascular ligation was mostly performed intracorporeally (87%). The rate of manual and mechanical techniques was comparable and a side-to-side anastomosis was mostly performed (88.6%).
The duration of the surgical intervention was longer in the EC group with a median of 150 min in the IC anastomosis group and 195 min in the EC anastomosis group (p < 0.001). Transfusion rates were similar in the two groups (p = 0.25). These results are shown in Table 2.
Postoperative outcomes
Postoperative outcomes are summarized in Table 3. A significant difference was found regarding the incidence of medical complications, with a higher incidence of cardiac, vascular and pulmonary complications in the EC anastomosis group (13% versus 20%; p = 0.049). This difference remained significant after adjusting for field characteristics (age, sex, BMI, smoking, diabetes, arteriopathy, coronaropathy or history of previous surgery), under multivariate analysis (p = 0.009; Fig. 3). A shorter period elapsed before the resumption of a regular diet in the IC group (1 versus 3 days; p = 0.001). In addition, a shorter hospital stay (median of 7 versus 8 days; p = 0.003) was observed in the IC group. This difference remained significant under multivariate analysis (p = 0.029; Fig. 4). Surgical complications rates were similar between the two groups (p = 0.76). The most common complication in both groups was prolonged ileus with 23 cases (15.3%) in the IC anastomosis group and 89 cases (19.9%) in the EC anastomosis group (p = 0.83). There were no differences between the groups in terms of time for mobilization (p = 0.93), reintervention rate (8 versus 24; p = 1) and 90-day mortality (p = 0.47).
Discussion
Our results from five tertiary centers involving expert surgeons in the achievement of a specific procedure show a benefit of the IC approach in terms of medical complications, hospital stay and operative time.
The principal strength of this multicenter study was that all patient data were collected over a short period of time and from five different tertiary centers involving experts in either IC or EC anastomosis techniques. There were therefore no technical changes to practice during the study period and the results obtained were a good reflection of current practice. To our knowledge and to date, this is the largest series published on this subject.
The main weakness of this study was its non-randomized design. However, randomization would have been difficult to interpret because the surgeons might have performed a technique in which they were not specialized. Our results were only conclusive after the learning curve had been achieved in tertiary center experts in laparoscopy. Although both techniques were practiced in each center, surgeons only used the technique they preferred. Differences in experience between surgeons could, therefore, have constituted a bias by influencing postoperative outcomes as a function of the learning curve. This study was retrospective and some information such as readmission rate and long-term complications (hernias, recurrence) was not available hence a prospective study including this information is needed.
In addition, the lengths of hospital stay and postoperative ileus could have been reduced during this 10-year period as a result of improvements in care and adherence to the ERAS program.
Laparoscopic colectomy is increasingly being considered as the gold standard for both benign and malignant colonic lesions [12]. Several studies have produced definitive results on the superiority of a laparoscopic approach over traditional open colectomy in terms of a more rapid return of bowel function, smaller incisions with less postoperative pain and better aesthetics, fewer pulmonary complications, and shorter hospital stay [13,14,15,16,17].
Jamali et al. [18] revealed that laparoscopic right colectomy with EC anastomosis is considered to be technically more difficult than laparoscopic sigmoidectomy, and that this difficulty increases significantly when the anastomosis is performed IC. This may explain why only a few surgeons have performed IC anastomoses to date [19].
This study consisted of a multicenter observational analysis of data from five tertiary centers in France involving a large cohort of 597 patients. The technique most widely employed in France remains EC anastomosis, which explains why the groups were not homogeneous in terms of the numbers of patients. EC anastomosis is more common because of the technical difficulties connected with IC anastomosis and the need in most cases to perform laparoscopic hand-sewn sutures, even in the case of a mechanical anastomosis. In terms of patient characteristics, stages of cancers and intraoperative data, the two groups were homogeneous and therefore comparable.
Vascular exposure was mostly achieved intracorporeally in our study. This was understandable due to the problems inherent in exposing the base of the mesentery via a small incision, especially in the case of obesity. Therefore, according to our study, most surgeons believe that the mesentery and ileocolic vessels should be divided intracorporeally.
The hypothesis underlying the development of a totally LRHC technique with IC anastomosis was that it could achieve more rapid recovery of intestinal function because traction on the colon and mesocolon is reduced, thus enabling greater postoperative comfort for the patient [20]. Our results totally supported this hypothesis, as patients experienced a more rapid recovery and shorter hospital stays after IC anastomosis, with no differences in terms of surgical outcomes. These findings reinforce those of a previous study which included colectomies by straight laparoscopy for colon cancer, adding colectomies for benign pathologies, and notably inflammatory bowel disease in the current study [21]. Although patients had a significantly higher BMI in the IC group, the duration of the surgical procedure was significantly shorter. This suggests that this technique is safe and less time-consuming in obese patients. In addition, a Pfannenstiel incision to extract the specimen was significantly more frequent in the IC group than in the EC group (48% versus 2%; p < 0.001). This lower rate was associated with less pain, resulting in potentially improved pulmonary recovery. Moreover, the occurrence of incisional hernia is much lower with a Pfannenstiel incision than with midline (umbilical) wounds [22, 23].
Postoperative medical complications were significantly more frequent in the EC group, probably because EC procedures require a larger incision. However, the rate of more severe complications was no higher in this group, which supports the fact that both techniques are safe.
Conclusions
LRHC with IC anastomosis could become the reference technique once surgical teams have completed the learning curve and achieved operative times comparable to those of right colectomies with EC anastomoses. IC is associated with faster recovery, a shorter hospital stay, and less medical morbidity. Our results suggest that IC anastomosis in LRHC is superior to EC anastomosis. This study clearly provides the rationale for a randomized prospective clinical trial.
References
Lee KH, Ho J, Akmal Y, Nelson R, Pigazzi A (2013) Short- and long-term outcomes of intracorporeal versus extracorporeal ileocolic anastomosis in laparoscopic right hemicolectomy for colon cancer. Surg Endosc 27(6):1986–1990
Chung CC, Ng DCK, Tsang WWC, Tang WL, Yau KKK, Cheung HYS et al (2007) Hand-assisted laparoscopic versus open right colectomy: a randomized controlled trial. Ann Surg 246(5):728–733
Schwenk W, Haase O, Neudecker J, Müller JM (2005). Short term benefits for laparoscopic colorectal resection. Cochrane Database Syst Rev (3):CD003145
Feroci F, Lenzi E, Garzi A, Vannucchi A, Cantafio S, Scatizzi M (2013) Intracorporeal versus extracorporeal anastomosis after laparoscopic right hemicolectomy for cancer: a systematic review and meta-analysis. Int J Colorectal Dis 28(9):1177–1186
Milone M, Elmore U, Vignali A, Gennarelli N, Manigrasso M, Burati M et al (2018) Recovery after intracorporeal anastomosis in laparoscopic right hemicolectomy: a systematic review and meta-analysis. Langenbecks Arch Surg 403(1):1–10
van Oostendorp S, Elfrink A, Borstlap W, Schoonmade L, Sietses C, Meijerink J et al (2017) Intracorporeal versus extracorporeal anastomosis in right hemicolectomy: a systematic review and meta-analysis. Surg Endosc 31(1):64–77
Emile SH, Elfeki H, Shalaby M, Sakr A, Bassuni M, Christensen P et al (2019) Intracorporeal versus extracorporeal anastomosis in minimally invasive right colectomy: an updated systematic review and meta-analysis. Tech Coloproctol 23(11):1023–1035. https://doi.org/10.1007/s10151-019-02079-7
Dindo D, Demartines N, Clavien P-A (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Park Y, Yong YG, Yun SH, Jung KU, Huh JW, Cho YB et al (2015) Learning curves for single incision and conventional laparoscopic right hemicolectomy: a multidimensional analysis. Ann Surg Treat Res 88(5):269–275
Surgery for cancers of the gastrointestinal tract: a step-by-step approach—Google Livres [Internet]. [cited 2019 Jun 30]. https://books.google.fr/books/about/Surgery_for_Cancers_of_the_Gastrointesti.html?id=_XG1BQAAQBAJ&redir_esc=y. Cited 2019 30 Jun 2019
Stades du cancer colorectal—Cancer du côlon | Institut National Du Cancer [Internet]. https://www.e-cancer.fr/Patients-et-proches/Les-cancers/Cancer-du-colon/Stades-du-cancer-colorectal. Cited 8 May 2018
Rondelli F, Trastulli S, Avenia N, Schillaci G, Cirocchi R, Gullà N et al (2012) Is laparoscopic right colectomy more effective than open resection? A meta-analysis of randomized and nonrandomized studies. Colorectal Dis Off J Assoc Coloproctol G B Irel 14(8):e447–469
Carnuccio P, Jimeno J, Parés D (2014) Laparoscopic right colectomy: a systematic review and meta-analysis of observational studies comparing two types of anastomosis. Tech Coloproctol 18(1):5–12
Tinmouth J, Tomlinson G (2004) Laparoscopically assisted versus open colectomy for colon cancer. N Engl J Med. 351(9):933–934 (author reply 933–934)
Colon Cancer Laparoscopic or Open Resection Study Group, Buunen M, Veldkamp R, Hop WCJ, Kuhry E, Jeekel J et al (2009) Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomised clinical trial. Lancet Oncol. 10(1):44–52
Guller U, Jain N, Hervey S, Purves H, Pietrobon R (2003) Laparoscopic vs open colectomy: outcomes comparison based on large nationwide databases. Arch Surg Chic Ill 1960 138(11):1179–1186
Veldkamp R, Gholghesaei M, Bonjer HJ, Meijer DW, Buunen M, Jeekel J et al (2004) Laparoscopic resection of colon cancer: consensus of the European Association of Endoscopic Surgery (EAES). Surg Endosc 18(8):1163–1185
Jamali FR, Soweid AM, Dimassi H, Bailey C, Leroy J, Marescaux J (2008) Evaluating the degree of difficulty of laparoscopic colorectal surgery. Arch Surg Chic Ill 1960 143(8):762–767 (discussion 768)
Lang RA, Hüttl TP, Winter H, Meyer G, Jauch K-W (2005) How safe are laparoscopic intracorporeal anastomoses? Zentralbl Chir 130(1):65–70
Magistro C, Lernia SD, Ferrari G, Zullino A, Mazzola M, De Martini P et al (2013) Totally laparoscopic versus laparoscopic-assisted right colectomy for colon cancer: is there any advantage in short-term outcomes? A prospective comparative assessment in our center. Surg Endosc 27(7):2613–2618
Milone M, Elmore U, Di Salvo E, Delrio P, Bucci L, Ferulano GP et al (2015) Intracorporeal versus extracorporeal anastomosis. Results from a multicentre comparative study on 512 right-sided colorectal cancers. Surg Endosc 29(8):2314–2320
Vergis AS, Steigerwald SN, Bhojani FD, Sullivan PA, Hardy KM (2015) Laparoscopic right hemicolectomy with intracorporeal versus extracorporeal anastamosis: a comparison of short-term outcomes. Can J Surg J Can Chir 58(1):63–68
Ricci C, Casadei R, Alagna V, Zani E, Taffurelli G, Pacilio CA et al (2017) A critical and comprehensive systematic review and meta-analysis of studies comparing intracorporeal and extracorporeal anastomosis in laparoscopic right hemicolectomy. Langenbecks Arch Surg 402(3):417–427
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
All the authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bou Saleh, N., Voron, T., De’Angelis, N. et al. Intracorporeal versus extracorporeal anastomosis in laparoscopic right hemicolectomy: results from the CLIMHET study group. Tech Coloproctol 24, 585–592 (2020). https://doi.org/10.1007/s10151-020-02202-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-020-02202-z