Abstract
Purpose
Although intracorporeal anastomosis (IA) appears to guarantee a faster recovery compared to extracorporeal anastomosis (EA), the data are still unclear. Thus, we performed a systematic review of the literature with meta-analysis to evaluate the recovery benefits of intracorporeal anastomosis.
Materials and methods
A systematic search was performed in electronic databases (PubMed, Web of Science, Scopus, EMBASE) using the following search terms in all possible combinations: “laparoscopic,” “right hemicolectomy,” “right colectomy,” “intracorporeal,” “extracorporeal,” and “anastomosis.” According to the pre-specified protocol, all studies evaluating the impact of choice of intra- or extracorporeal anastomosis after right hemicolectomy on time to first flatus and stools, hospital stay, and postoperative complications according to Clavien-Dindo classification were included.
Results
Sixteen articles were included in the final analysis, including 1862 patients who had undergone right hemicolectomy: 950 cases (IA) and 912 controls (EA). Patients who underwent IA reported a significantly shorter time to first flatus (MD = − 0.445, p = 0.013, Z = − 2.494, 95% CI − 0.795, 0.095), to first stools (MD = − 0.684, p < 0.001, Z = − 4.597, 95% CI − 0.976, 0.392), and a shorter hospital stay (MD = − 0.782, p < 0.001, Z = −3.867, 95% CI − 1.178, − 0.385) than those who underwent EA. No statistically significant differences in complications between the IA and EA patients were observed in the Clavien-Dindo I-II group (RD = − 0.014, p = 0.797, Z = − 0.257, 95% CI − 0.117, 0.090, number needed to treat (NNT) 74) or in the Clavien-Dindo IV-V (RD = − 0.005, p = 0.361, Z = − 0.933, 95% CI − 0.017, 0.006, NNT 184). The IA procedure led to fewer complications in the Clavien-Dindo III group (RD = − 0.041, p = 0.006, Z = − 2.731, 95% CI − 0.070, 0.012, NNT 24).
Conclusions
Although intracorporeal anastomosis appears to be safe in terms of postoperative complications and is potentially more effective in terms of recovery after surgery, further ad hoc randomized clinical trials are needed, given the heterogeneity of the data available in the current literature.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It is well known that the laparoscopic approach for colon resection improves short-term outcomes compared to open surgery [1].
Although currently considered a feasible and effective surgery, in terms of short- and long-term results, laparoscopic right colectomy is performed by a small number of surgeons [1,2,3,4,5]; in the vast majority of cases, this technique is performed with an extracorporeal anastomosis (EA) [6] due to technical difficulties and the frequent need to perform laparoscopic hand-sewn sutures.
Several studies have been published that compare intracorporeal anastomosis (IA) versus EA in laparoscopic right colectomy and most are very recent. Although intracorporeal anastomosis appeared to guarantee a faster recovery after surgery, the data are still unclear. The primary aim of the study is to evaluate recovery benefits after total laparoscopic right colectomy. Thus, we have performed a systematic review with a meta-analysis of the literature.
Methods
A protocol for this review was prospectively developed detailing the specific objectives, the criteria for study selection, the approach to assess study quality, the outcomes, and the statistical methods.
Search strategy
To identify all available studies, a detailed search pertaining to laparoscopic right hemicolectomy with total intracorporeal anastomosis and extracorporeal anastomosis was conducted according to PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines [7].
A systematic search was performed in electronic databases (PubMed, Web of Science, Scopus, EMBASE) using the following search terms in all possible combinations: “laparoscopic,” “right hemicolectomy,” “right colectomy,” “intracorporeal,” “extracorporeal,” and “anastomosis.” The search strategy was developed without any language restrictions. Additionally, the reference lists of all retrieved articles were manually reviewed. In the case of missing data, study authors were contacted by e-mail to try to retrieve original data. The “related article” function from PubMed was used to broaden the search, and the reference lists of all potential eligible studies published between January 1995 and March 2017 were manually reviewed.
Two independent authors analyzed each article and performed the data extraction independently. In case of disagreement, a third investigator was consulted. Discrepancies were resolved by consensus.
Data extraction and quality assessment
According to the pre-specified protocol, all studies evaluating the impact of choice of intra- or extracorporeal anastomosis after right hemicolectomy on recovery, including the time to first flatus, stools, mobilization and length of hospital stay, and postoperative complications, according to Clavien-Dindo classification, were included. Case reports, case series without a control group, and animal studies were excluded.
To be included in the analysis, the study had to provide values (mean with standard deviation or standard error or p value) of the time to first flatus and/or stools and length of hospital stay for each procedure (intra- or extracorporeal anastomosis after right hemicolectomy) and/or the prevalence of complications, according to Clavien-Dindo classification. In each study, data regarding sample size and major clinical and demographic variables were extracted. Data expressed as medians (with range) were converted to means (with standard deviation) according to Hozo [8].
Formal quality score adjudication was not used, since previous investigations failed to demonstrate its usefulness [9].
Statistical analysis and risk of bias assessment
Statistical analysis was carried out using Comprehensive Meta-analysis [Version 2.2, Biostat Inc., Englewood, NJ, USA, 2005].
Differences among cases and controls were expressed as the mean difference (MD) with pertinent 95% confidence intervals (95% CI) for continuous variables and as risk difference (RD) with pertinent 95% CI for dichotomous variables, according to Messori et al. [10]. In this case, number needed to treat (NNT) was calculated to assess the number of patients who should be treated in order to obtain one patient more with good outcomes, in line with the standard procedure according to Citrome et al. [11].
The overall effect was tested using Z scores and significance was set at P < 0.05. Statistical heterogeneity between studies was assessed with the chi square Cochran’s Q test and with the I 2 statistic, which measures the inconsistency across study results and describes the proportion of total variation in study estimates that is due to heterogeneity rather than sampling error. An I 2 value of 0% indicates no heterogeneity, a value of 25% indicates low heterogeneity, 25–50% indicates moderate heterogeneity, and 50% indicates high heterogeneity.
Publication bias was assessed by Egger’s test and represented graphically by funnel plots of the standardized mean differences versus the standard error. Visual inspection of funnel plot asymmetry was performed to address possible small-study effects, and Egger’s test was used to assess publication bias over and above any subjective evaluation. A p < 0.005 was considered statistically significant [12]. In the case of significant publication bias, Duval and Tweedie’s trim and fill method was used to allow for the estimation of an adjusted effect size [13].
To be as conservative as possible, the random-effect method was used for all analyses to take into account the variability among included studies.
Meta-regression analyses
We hypothesized that differences among included studies may be affected by demographic variables (mean age, male gender, BMI) and clinical data (American Society of Anesthesiologists (ASA) score, tumor T status and its localization or previous abdominal surgery). To assess the possible effect of such variables in explaining different results observed across studies, we planned to perform meta-regression analyses after implementing a regression model with changes in the time to first flatus and/or stools and length of hospital stay or postoperative complications according to Clavien-Dindo classification as dependent variables (y), expressed as MD or RD, and mean age, male gender, BMI, mean ASA score, previous abdominal surgery, localization of tumor, and tumor stage T as independent variables (x). This analysis was performed with Comprehensive Meta-analysis [Version 2.2, Biostat Inc., Englewood, NJ, USA, 2005]. Moreover, to avoid false positive correlations between independent and dependent variables, Monte Carlo simulation was performed. This analysis was performed with Stata [Version 12, Stata Corp., Lakeway Drive College Station, Texas, USA, 2010].
Results
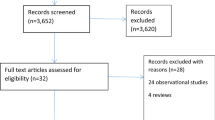
After excluding duplicate results, the search retrieved 490 articles. Of these studies, 339 were excluded because they were off the topic after scanning the title and/or the abstract, and 128 were excluded because they were reviews/comments/case reports or they lacked data of interest. Another 7 studies were excluded after full-length paper evaluation. Thus, 16 articles were included in the final analysis, encompassing 1862 patients who underwent right hemicolectomy, including 950 cases (patients who had undergone IA) and 912 controls (patients who had undergone EA) (Fig. 1).
Study characteristics
Six studies had a prospective design [14,15,16,17,18,19] and the other ten were retrospective [20,21,22,23,24,25,26,27,28,29] (Table 1 ). The only randomized controlled trial study analyzing the role of intracorporeal stapled versus extracorporeal stapled anastomosis after laparoscopic right colectomy was the one from Vignali et al. [17]. Major characteristics of study populations are shown in Table 2. The number of patients ranged from 30 to 512, the mean age ranged from 59 to 74.5 years, and the prevalence of male gender ranged from 28.57 to 69.57%. Mean BMI ranged from 20.3 to 28.64 kg/m2. The prevalence of malignant disease ranged from 60.7 to 100%. Only eight studies reported the exact localization of the cancer [14, 15, 17,18,19, 21, 22, 28], and only six studies reported the complete TNM [14, 15, 18, 20,21,22]. Technical aspects of each surgical technique are summarized in Supplementary Table T1. In all studies, the anastomosis is performed using a stapler in a side-to-side fashion. Regarding the closure of enterotomies, there is large variation among published series. Regarding site extraction, most authors prefer to extract the specimen using a Pfannenstiel incision in patients with IA. Only one group [14] used the right lower quadrant trocar site for this purpose, and the other three studies [16, 18, 28] used the periumbilical median incision. On the other hand, in the case of EA, there is larger variation. Most authors reported that the specimen was extracted using a periumbilical median incision [16, 17, 23, 24, 27,28,29]; Roscio [22] used the upper right quadrant for this purpose; Scatizzi [14] used the right flank incision; and Vergis [24] used the midline incision. Fabozzi [20] did not report these data.
Postoperative recovery outcomes
Postoperative recovery outcomes are shown in Fig. 2. The time to first flatus was analyzed by nine studies [14, 15, 17, 18, 20, 21, 24, 26, 28], encompassing 1148 patients (581 IA and 567 EA); this value was significantly different between the two groups, in favor of IA (MD = − 0.445, p = 0.013, Z = − 2.494, 95% CI − 0.795, 0.095). Heterogeneity among these studies was statistically significant (I 2 = 94.042%; p < 0.001).
The time to first stools was reported by five studies [17, 18, 20, 22, 29], encompassing 342 patients (177 IA and 165 EA); there was a statistically significant difference between the two groups in favor of IA (MD = − 0.684, p < 0.001, Z = − 4.5971, 95% CI − 0.976, 0.392), and there was significant heterogeneity among the studies (I 2 = 68.112%; p = 0.014).
The time to first mobilization was analyzed only by Milone et al. [15], and thus, it was not possible to meta-analyze these data.
Length of hospital stay was analyzed by 15 studies [14,15,16, 18,19,20,21,22,23,24,25,26,27,28,29], encompassing 1802 patients (920 IA and 882 EA); the length of hospital stay was significantly shorter in the IA group than in the EA group (MD = − 0.782, p < 0.001, Z = − 3.867, 95% CI − 1.178, − 0.385).
Postoperative complications
Postoperative complications according to Clavien-Dindo score were reported by five studies [15, 16, 18, 22, 23], encompassing 914 patients (482 IA and 432 EA); these data are shown in Fig. 3.
No statistically significant differences in postoperative complications between the IA and EA procedures were observed in the Clavien-Dindo I-II group (RD = − 0.014, p = 0.797, Z = − 0.257, 95% CI − 0.117, 0.090, NNT = 74), the Clavien-Dindo III group (RD = − 0.041, p = 0.006, Z = − 2.731, 95% CI − 0.070, − 0.012, NNT = 24), or the Clavien-Dindo IV-V group (RD = − 0.005, p = 0.351, Z = − 0.933, 95% CI − 0.017, 0.006, NNT = 184).
Postoperative pain according to a visual analogue scale (VAS) was analyzed only by Fabozzi et al. [20]; therefore, it was not possible to analyze this aspect.
Meta-regression analyses
Regression models showed that the time to first flatus was influenced by age (p < 0.001; Z = 5.44), male gender (p < 0.001; Z = 5.47), BMI (p < 0.001; Z = 5.33), previous abdominal surgery (p < 0.001; Z = 5.07), localization of the tumor in the caecum/right colon/appendix (p < 0.001; Z = 5.28) or in hepatic flexure/proximal transverse (p < 0.001; Z = − 5.22), tumor stage T0 (p < 0.001; Z = 3.83), T1-T2 (p < 0.001; Z = − 5.02), and T3-T4 (p < 0.001; Z = 5.08). The time to first stool was influenced by age (p = 0.02; Z = 2.19), male gender (p = 0.005; Z = 2.79), BMI (p = 0.02; Z = 2.17), and previous abdominal surgery (p = 0.01; Z = 2.39). Hospital stay was influenced by age (p < 0.001; Z = 4.47), BMI (p = 0.004; Z = 2.87), ASA score (p < 0.001; Z = 4.14), previous abdominal surgery (p < 0.001; Z = 3.64), tumor stage T0 (p = 0.001; Z = 3.23), T1-T2 (p < 0.001; Z = − 4.42), and T3-T4 (p < 0.001; Z = 4.58). Clavien-Dindo I-II complications were influenced by ASA score (p = 0.04; Z = 1.97) and previous abdominal surgery (p = 0.002; Z = 3.06), while none of the clinical and demographic variables influenced the complications in the Clavien-Dindo III and IV-V groups. All the other covariates tested did not impact the outcomes analyzed. The results of Monte Carlo simulation confirmed that hospital stay was influenced by BMI (p = 0.021) and ASA score (p = 0.025), while the other covariates tested did not impact the outcome analyzed.
Publication bias
Since publication bias is known to affect the results of meta-analyses, we attempted to assess this potential bias using funnel plot analysis. Visual inspection of funnel plots of effect size versus standard error for studies evaluating selected outcomes suggested a symmetric distribution of studies around the effect size (Supplementary Fig. F1), and Egger’s test confirmed the absence of publication bias (p always > 0.05).
Discussion
Laparoscopic colonic resection is increasingly regarded as the gold standard for benign and malignant colonic lesions [25,26,27,28,29,30,31]. Thanks to the use of the circular stapler, total laparoscopic colectomy is now a common practice in laparoscopic surgery of the left colon and rectum. On the other hand, in laparoscopic right colon surgery, intracorporeal anastomosis (IA) is rarely performed due to technical difficulties and the need to perform laparoscopic hand-sewn sutures [30].
In recent years, numerous studies have been published comparing intracorporeal versus extracorporeal anastomosis after laparoscopic right colectomy [14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29]. It is important to highlight that no randomized clinical trials were available in current literature, excluding the interim analysis provided by Vignali et al. [17].
Based on these studies, some meta-analyses [30,31,32,33,34] have been performed focusing on short-term outcomes, morbidity, and mortality after IA compared to EA. Based on these initial results, there seems to be an advantage in favor of IA, since it is apparently associated with the best recovery and shorter hospital stay, without any increase in major complications.
However, authors failed to draw a final conclusion about the differences between IA and EA, since data reported about the advantages on recovery were conflicting and unclear.
To the best of our knowledge, there is no study focused on the benefits of IA after right hemicolectomy in terms of recovery. Thus, we performed a systematic review with a meta-analysis of the literature specifically addressing the recovery benefits after total laparoscopic right colectomy with intracorporeal anastomosis.
By pooling together data from 1862 total laparoscopic right colectomies, we have been able to provide an estimation of recovery after intracorporeal versus extracorporeal anastomosis.
To evaluate recovery, we have meta-analyzed data about the restoration of bowel function (time to first flatus and time to first stool), mobilization, length of hospital stay, pain scores, and Clavien-Dindo scale.
Concerning bowel function, both the time to first flatus and the time to first stool were significantly better after the IA procedure than after the EA procedure. However, data about the time to first flatus have been collected by nine studies [14, 15, 17, 18, 20, 21, 24, 26, 28], encompassing 1148 patients (581 IA and 567 EA), and the time to first stool was reported in five studies [17, 18, 20, 22, 29], encompassing 342 patients (177 IA and 165 EA).
Furthermore, it is important to underscore how these two parameters have been strongly influenced by demographic data and other covariates. In fact, the time to first flatus was influenced by age, male gender, BMI, previous abdominal surgery, localization of the tumor, and tumor stage, while the time to first stool was influenced by age, male gender, BMI, and previous abdominal surgery.
Hospital stay was analyzed by 15 studies [14,15,16, 18,19,20,21,22,23,24,25,26,27,28,29], encompassing 1802 patients (920 IA and 882 EA), and was significantly shorter in the IA group than in the EA group. It is worth mentioning that demographic and pathologic characteristics (age, BMI, ASA score, previous abdominal surgery, and tumor stage) influenced the length of hospital stay once again.
Data about first mobilization were collected only by Milone et al. [15], so it was not possible to include this criteria in this meta-analysis. Nonetheless, we think it is important to underscore that the time until the first mobilization after a right colon resection proved to be significantly shorter after a total laparoscopic procedure.
Although postoperative pain was reported by five studies [15, 19, 20, 22, 26], no one unit has been used precluding the possibility of making a statistical analysis. Due to this heterogeneity in terms of pain measurement, it was not possible to meta-analyze pain data. Even so, taken singularly, study results seem to be in favor of IA.
In the study by Roscio et al. [22], pain was included in the Clavien-Dindo scale and resulted in no significant difference between IA and EA. Marchesi et al. [19] used the number of intravenous ketorolac vials as a pain measure. Additionally, in this case, there was no significant difference between the groups. In Milone et al. [15], pain was considered as the need for extra analgesia in the postoperative period, and pain was significantly higher after LACR. Chang et al. used the Changhai Pain Scale [35] and found significantly less pain after IA. The study by Fabozzi et al. [20] is the only study using the VAS scale as a pain measurement. Additionally, in this case, there was a significant difference in terms of postoperative pain in favor of TLCR.
Postoperative complications according to Clavien-Dindo score were reported by five studies [15, 16, 18, 22, 23]. Of interest, Clavien-Dindo grades I and II include pain, nausea/vomiting, wound infection, and bleeding, which are the more common symptoms that can influence recovery after surgery. In our meta-analyses, no significant differences were reported about postoperative complications according to Clavien-Dindo I-II. It is important to emphasize that the number of patients involved was 914, which is likely too few to obtain a robust result, considering the fact that more than half of this number (512 patients) came from only one author [15].
Although the results of our meta-analysis seem to be in favor of IA rather than EA, in terms of recovery, since it is associated with earlier bowel function and shorter hospital stay, the data collected by the studies included in this meta-analysis are extremely heterogeneous in terms of recovery. Thus, it is hard to draw final conclusions about recovery after IA in right colon cancer and if it really is faster compared to EA for the same type of surgery.
In conclusion, to obtain a final answer about the superiority of IA compared to EA in terms of safety and feasibility by randomized clinical trial, we advocate a call to action to determine if there is an actual advantage in terms of recovery after IA compared to EA after a laparoscopic colon resection. To do so, there must be standardization in the data collected concerning recovery. First, to indicate bowel recovery, only the time preceding the first flatus should be reported, and it should be indicated in all studies. Mobilization is an important factor that very few studies have considered. Clavien-Dindo scale is a classification of surgical complications [36]; it includes all kinds of minor complications in grades I and II, most of which are connected to the lengthening of hospital stay. In our opinion, to evaluate recovery, a correctly reported Clavien-Dindo scale is an essential parameter. In the same way, we believe that pain should always be evaluated using the VAS scale, which is an accurate international scale.
It is worth mentioning that recovery is a metric that also depends on multiple factors, such as patient literacy, government-owned institutions versus private institutions, patient occupation, and the type of recovery protocols used (enhanced recovery versus standard recovery); we tried to analyze these aspects. In detail, we found that all the studies involved public hospitals. Regarding enhanced recovery after surgery (ERAS) protocol, none of the authors included adhered strictly to ERAS protocol, but all applied “ERAS-like” postoperative management with early postoperative mobilization and early oral intake of fluids and then solid diet. Regarding comorbidities, all of the studies excluded patients with severe cardiovascular disease that contraindicated laparoscopy and patients with T4 tumors. Although most studies are retrospective analyses, thus preventing the exclusion of allocation bias, patient characteristics (BMI, ASA score, and T stage) were similar among the groups in all studies. Patient literacy and occupation were not reported. Thus, given that all factors were not specifically addressed in the analyzed studies, we cannot exclude the biases that were related to recovery outcomes.
In conclusion, although intracorporeal anastomosis could be considered as safe as extracorporeal anastomosis, with this meta-analysis, we could only assess the recovery after IA in laparoscopic right colon surgery, which is still controversial, due to the huge heterogenous data reported by previous studies.
References
Tinmouth J, Tomlinson G (2004) Laparoscopically assisted versus open colectomy for colon cancer. N Engl J Med 351(9):933–934. https://doi.org/10.1056/NEJM200408263510919
Jamali FR, Soweid AM, Dimassi H, Bailey C, Leroy J, Marescaux J (2008) Evaluating the degree of difficulty of laparoscopic colorectal surgery. Arch Surg 143(8):762–767. https://doi.org/10.1001/archsurg.143.8.762
Chang K, Fakhoury M, Barnajian M, Tarta C, Bergamaschi R (2013) Laparoscopic right colon resection with intracorporeal anastomosis. Surg Endosc 27(5):1730–1736. https://doi.org/10.1007/s00464-012-2665-x
Tarta CM, Bishawi M, Bergamaschi R (2013) Intracorporeal ileocolic anastomosis: a review. Tech Coloproct 17(5):479–485. https://doi.org/10.1007/s10151-013-0998-7
Simorov A, Shaligram A, Shostrom V, Boilesen E, Thompson J, Oleynikov D (2012) Laparoscopic colon resection trends in utilization and rate of conversion to open procedure: a national database review of academic medical centers. Ann Surg 256(3):462–468. https://doi.org/10.1097/SLA.0b013e3182657ec5
Carnuccio P, Jimeno J, Parés D (2014) Laparoscopic right colectomy: a systematic review and meta-analysis of observational studies comparing two types of anastomosis. Tech Coloproctol 18(1):5–12. https://doi.org/10.1007/s10151-013-1029-4
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097. https://doi.org/10.1371/journal.pmed.1000097
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range and the size of sample. BMC Med Res Methodol 5(1):13. https://doi.org/10.1186/1471-2288-5-13
Juni P, Witschi A, Bloch R et al (1999) The hazards of scoring the quality of clinical trials for meta-analysis. JAMA 282(11):1054–1060. https://doi.org/10.1001/jama.282.11.1054
Messori A, Maratea D, Fadda V, Trippoli S (2013) Using risk difference as opposed to odds-ratio in meta-analysis. Int J Cardiol 20(1):127. https://doi.org/10.1016/j.ijcard.2012.06.078
Citrome L, Ketter TA (2013) When does a difference make a difference? Interpretation of number needed to treat, number needed to harm, and likelihood to be helped or harmed. Int J Clin Pract 67(5):407–411. https://doi.org/10.1111/ijcp.12142
Sterne JA, Egger M, Smith GD (2001) Systematic reviews in health care: investigating and dealing with publication and other biases in meta-analysis. BMJ 323(7304):101–105. https://doi.org/10.1136/bmj.323.7304.101
Duval S, Tweedie R (2000) Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 56(2):455–463. https://doi.org/10.1111/j.0006-341X.2000.00455.x
Scatizzi M, Kroning KC, Borrelli A, Andan G, Lenzi E, Feroci F (2010) Extracorporeal versus intracorporeal anastomosis after laparoscopic right colectomy for cancer: a case-control study. World J Surg 34(12):2902–2908. https://doi.org/10.1007/s00268-010-0743-6
Milone M, Elmore U, Di Salvo E, Delrio P, Bucci L, Ferulano GP, Napolitano C, Angiolini MR, Bracale U, Clemente M, D’Ambra M, Luglio G, Musella M, Pace U, Rosati R, Milone F (2015) Intracorporeal versus extracorporeal anastomosis. Results from a multicentre comparative study on 512 right-sided colorectal cancers. Surg Endosc 29(8):2314–2320. https://doi.org/10.1007/s00464-014-3950-7
Shapiro R, Keler U, Segev L, Sarna S, Hatib K, Hazzan D (2015) Laparoscopic right hemicolectomy with intracorporeal anastomosis: short- and long-term benefits in comparison with extracorporeal anastomosis. Surg Endosc 30(9):3823–3829. https://doi.org/10.1007/s00464-015-4684-x
Vignali A, Bissolati M, De Nardi P, Di Palo S, Staudacher C (2016) Extracorporeal vs. extracorporeal ileocolic stapled anastomoses in laparoscopic right colectomy: an interim analysis of a randomized clinical trial. J Laparoendosc Adv Surg Tech 26(5):1–6. https://doi.org/10.1089/lap.2015.0547
Magistro C, Lernia SD, Ferrari G, Zullino A, Mazzola M, De Martini P, De Carli S, Forgione A, Bertoglio CL, Pugliese R (2013) Totally laparoscopic versus laparoscopic-assisted right colectomy for colon cancer: is there any advantage in short-term outcomes? A prospective comparative assessment in our center. Surg Endosc 27(7):2613–2618. https://doi.org/10.1007/s00464-013-2799-5
Marchesi F, Pinna F, Percalli L, Cecchini S, Riccó M, Costi R, Pattonieri V, Roncoroni L (2013) Totally laparoscopic right colectomy: theoretical and practical advantages over the laparo-assisted approach. J Laparoendosc Adv Surg Tech 23(5):418–424. https://doi.org/10.1089/lap.2012.0420
Fabozzi M, Allieta R, Contul RB, Grivon M, Millo P, Lale-Murix E, Nardi M (2010) Comparison of short- and medium-term results between laparoscopically assisted and totally laparoscopic right hemicolectomy: a case-control study. Surg Endosc 24(9):2085–2091. https://doi.org/10.1007/s00464-010-0902-8
Chaves JA, Idoate CP, Fons JB et al (2011) A case-control study of extracorporeal versus intracorporeal anastomosis in patients subjected to right laparoscopic hemicolectomy. Cir Esp 89(1):24–30. https://doi.org/10.1016/j.ciresp.2010.10.003
Roscio F, Bertoglio C, De Luca A, Frattini P, Scandroglio I (2012) Totally laparoscopic versus laparoscopic assisted right colectomy for cancer. Int J Surg 10(6):290–295. https://doi.org/10.1016/j.ijsu.2012.04.020
Hanna MH, Hwang GS, Phelan MJ, Bui TL, Carmichael JC, Mills SD, Stamos MJ, Pigazzi A (2016) Laparoscopic right hemicolectomy: short- and long-term outcomes of intracorporeal versus extracorporeal anastomosis. Surg Endosc 30(9):3933–3942. https://doi.org/10.1007/s00464-015-4704-x
Vergis AS, Steigerwald SN, Bhojani FD, Sullivan PA, Hardy KM (2015) Laparoscopic right hemicolectomy with intracorporeal versus extracorporeal anastamosis: a comparison of short-term outcomes. Can J Surg 58(1):63–68. https://doi.org/10.1503/cjs.001914
Lee KH, Ho J, Akmal Y, Nelson R, Pigazzi A (2013) Short- and long-term outcomes of intracorporeal versus extracorporeal ileocolic anastomosis in laparoscopic right hemicolectomy for colon cancer. Surg Endosc 27(6):1986–1990. https://doi.org/10.1007/s00464-012-2698-1
Anania G, Santini M, Scagliarini L, Marzetti A, Vedana L, Marino S, Gregorio C, Resta G, Cavallesco G (2012) A totally mini invasive approach for colorectal laparoscopic surgery. World J Gastroenterol 18(29):3869–3874. https://doi.org/10.3748/wjg.v18.i29.3869.
Jian-Cheng T, Shu-Sheng W, Bo Z, Jian F, Liang Z (2016) Total laparoscopic right hemicolectomy with 3-step stapled intracorporeal isoperistaltic ileocolic anastomosis for colon cancer: an evaluation of short-term outcomes. Medicine (Baltimore) 95(48):e5538
Trastulli S, Coratti A, Guarino S, Piagnerelli R, Annecchiarico M, Coratti F, di Marino M, Ricci F, Desiderio J, Cirocchi R, Parisi A (2015) Robotic right colectomy with intracorporeal anastomosis compared with laparoscopic right colectomy with extracorporeal and intracorporeal anastomosis: a retrospective multicentre study. Surg Endosc 29(6):1512–1521. https://doi.org/10.1007/s00464-014-3835-9
Erguner I, Aytac E, Baca B, Hamzaoglu I, Karahasanoglu T (2013) Total laparoscopic approach for the treatment of right colon cancer: a technical critique. Asian J Surg 36(2):58–63. https://doi.org/10.1016/j.asjsur.2012.09.004
Feroci F, Lenzi E, Garzi A, Vannucchi A, Cantafio S, Scatizzi M (2013) Intracorporeal versus extracorporeal anastomosis after laparoscopic right hemicolectomy for cancer: a systematic review and meta-analysis. Int J Color Dis 28(9):1177–1186. https://doi.org/10.1007/s00384-013-1651-7
Rondelli F, Trastulli S, Avenia N, Schillaci G, Cirocchi R, Gullà N, Mariani E, Bistoni G, Nova G (2012) Laparoscopic right colectomy more effective than open resection? A meta-analysis of randomized and nonrandomized studies. Color Dis 14(8):e447–e469. https://doi.org/10.1111/j.1463-1318.2012.03054.x
Ricci C, Casadei R, Alagna V, Zani E, Taffurelli G, Pacilio CA, Minni F (2017) A critical and comprehensive systematic review and meta-analysis of studies comparing intracorporeal and extracorporeal anastomosis in laparoscopic right hemicolectomy. Langenbeck’s Arch Surg 402(3):417–427. https://doi.org/10.1007/s00423-016-1509-x
Van Oostendorp S, Elfrink A, Borstlap W, Schoonmade L, Sietses C, Meijerink J, Tuynman J (2017) Intracorporeal versus extracorporeal anastomosis in right hemicolectomy: a systematic review and meta-analysis. Surg Endosc 31(1):64–77. https://doi.org/10.1007/s00464-016-4982-y
Wu Q, Jin C, Hu T, Wei M, Wang Z (2017) Intracorporeal versus extracorporeal anastomosis in laparoscopic right colectomy: a systematic review and meta-analysis. J Laparoendosc Adv Surg Tech A 27(4):348–357. https://doi.org/10.1089/lap.2016.0485
Lu X-Y, Zhao C-F, Zhang T-T et al (2003) The practicability of the Changhai Pain Scale in the clinical pain assessment. N J Chin HA 20:6–7
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibañes E, Pekolj J, Slankamenac K, Bassi C, Graf R, Vonlanthen R, Padbury R, Cameron JL, Makuuchi M (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250(2):187–196. https://doi.org/10.1097/SLA.0b013e3181b13ca2
Author information
Authors and Affiliations
Contributions
Milone M: conception, design, interpretation of the data, and drafting of the article; Elmore U, Vignali A, Gennarelli N, Manigrasso M, Burati M, and Milone F: acquisition, analysis, and interpretation of the data; Milone F and De Palma GD: interpretation of the data and critical revisions; Delrio P and Rosati R: critical revisions and final approval.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Electronic supplementary material
Supplementary Figure 1
(JPEG 153 kb)
Supplementary Figure F1
Funnel plots analysis. a) time to first flatus; b) time to first stools; c) hospital stay; d) Clavien I-II; e) Clavien III; f) Clavien IV-V (JPEG 205 kb)
Supplementary Table T1
Operative data (DOCX 20 kb)
Rights and permissions
About this article
Cite this article
Milone, M., Elmore, U., Vignali, A. et al. Recovery after intracorporeal anastomosis in laparoscopic right hemicolectomy: a systematic review and meta-analysis. Langenbecks Arch Surg 403, 1–10 (2018). https://doi.org/10.1007/s00423-017-1645-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-017-1645-y