Abstract
Background
Mesenchymal stem-cell (MSC) therapy for perianal fistulas in Crohn’s disease (CD) remains controversial. We performed this meta-analysis to evaluate the efficacy and safety of MSC therapy for the treatment of perianal fistulas in CD.
Methods
Electronic databases were searched for studies that reported efficacy and/or safety of MSC therapy for perianal CD (pCD). We used the metaprop command of the meta package in R and RevMan to assess the efficacy and safety. Subgroup analyses were performed for exploration of heterogeneity regarding all outcomes.
Results
After screening, 13 trials were included in our study. RevMan for meta-analysis showed that: (1) patients had healed perianal fistulas after MSC treatment, with an odds ratio (OR) of 2.05 (P = 0.0002; 95% confidence interval (CI) 1.41, 3.00) vs controls; (2) pelvic magnetic resonance imaging (MRI) used to evaluate the healing of fistulas showed that MSC therapy had a higher healing rate (HR) compared to control (OR = 1.95; P = 0.0007; 95% CI 1.33, 2.87). R software for meta-analysis showed that 63% (95% CI 0.53, 0.74) of patients achieved clinical healing as a result of local therapy with MSCs. Random-effects pooled rates of clinical response were 30% (95% CI 0.18, 0.48). Pelvic MRI used to evaluate fistula healing showed a HR of 56% (95% CI 0.46, 0.69). The HR with autologous MSCs was higher than with allogeneic MSCs (79% vs 52%; P < 0.05). Uniform injection of MSCs according to the size of fistulas improve the HR (80% vs 55%; P < 0.05) compared with fixed-dose MSCs. There was no significant increase in adverse events (OR = 1.14; P = 0.54; 95% CI 0.75, 1.74) in patients treated with MSCs and no major MSC-related adverse event has been reported so far.
Conclusions
Local administration of MSCs is an effective and safe method for pCD. It also represents hope for effective treatment of refractory pCD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Crohn’s disease (CD) is an immune-mediated chronic recurrent, systemic disease characterized by gastrointestinal inflammation. Perianal fistula is a common complication of CD, and is estimated to affect up to 26–28% of patients in the first two decades after diagnosis [1, 2]. The treatment of pCD includes conventional medical treatment strategies (e.g., antibiotics and immunomodulators) and anti-tumour necrosis factor agents (anti-TNF), or surgical treatments. However, up to 60–70% of patients relapse after stopping medical treatment, and only a few patients achieve long-term remission [3]. Surgical treatment is associated with problems of poor healing and a high rate of recurrence. In addition, impaired sphincter muscle function following surgery causes postoperative anal incontinence in about 10–35% patients. In some severe cases, fecal diversion may be used to manage CD [4], but recurrence is high with restoration of continuity, and up to 20–40% of these patients will eventually undergo a proctectomy [5]. Therefore, management of refractory pCD and the realization of long-term healing have remained a challenging problem.
In recent years, tremendous progress has been made in the field of regenerative medicine and stem-cell biology. Stem-cell therapy has become a hot research topic. Stem cells are a unique group of undifferentiated cells that have capacity of self-renewal and they can be broadly categorized as embryonic or adult-derived stem cells. Among adult stem cells, the best defined cells are the hematopoietic stem cells (HSCs), MSCs, and intestinal stem cells. Given that MSCs are able to down-regulate immune responses, anti-inflammatory properties, and promote tissue healing [6,7,8,9,10], they are most commonly used to treat pCD. MSCs can achieve the reconstruction of intestinal immunity, to avoid immune-mediated intestinal inflammation, and may achieve long-term healing of pCD, significantly improving the quality of life of patients. Therefore, MSCs may serve as an alternative treatment for refractory pCD. Multiple studies have been conducted to assess efficacy and safety of MSC therapy in pCD, but the outcomes still remain controversial. We performed a systematic review and meta-analysis of the literature to determine the efficacy and safety of MSC therapy.
Materials and methods
We followed the preferred reporting items for systematic reviews and meta-analysis (PRISMA) guidelines [11].
Literature search
To identify relevant studies, a comprehensive electronic search of Pubmed, Cochrane Library, Embase, and CNKI was performed from their inception to October, 2018. Combinations of the following search terms were used: (all fields): (“inflammatory bowel disease” OR “Crohn’s disease” OR “Crohn disease”) and (“mesenchymal stem/stromal cells” OR “stem cell” OR “stromal cell”) and (“perianal fistula” OR “Crohn’s perianal fistula”) and any appropriate abbreviations.
Study selection
Inclusion criteria were: (1) human studies; (2) randomized controlled trials (RCTs), non-randomized experimental studies, and so on; (3) established diagnosis of CD perianal fistula by accepted criteria, with no limits on the age and gender of patients; (4) MSCs were used for treatment of pCD; (5) interventions: local therapy with MSCs for pCD; (6) efficacy and/or safety were reported; and (7) the primary endpoint was clinical efficacy (fistula healing, clinical response) of MSCs for the treatment of pCD, and the secondary endpoint was safety. Exclusion criteria were: (1) non-human studies; (2) use of total-body irradiation or myeloablative regimens; (3) not belonging to pCD (e.g., rectovaginal fistula or enterocutaneous fistulas); (4) and efficacy of MSCs as systemic infusion for CD.
Data extraction and quality assessment
One reviewer (Z.H) extracted data through a standardized data collection form, and then, another reviewer (Z.L) checked the data for accuracy. Any inconsistent results were handled by discussion. These forms included: (1) author; (2) journal; (3) study characteristics (year, location, and type of study); (4) patient demographics (number of patients, age); (5) number of healthy controls (if any); (6) type and source of MSCs; (7) efficacy outcome; (8) dosage and modalities of administration; (9) the use of concomitant therapy with anti-TNF; (10) follow-up time and recurrence; (11) refractory disease (defined as patients who had been unresponsive to or unsuitable for all the previous medical treatment including anti-TNF or unsuccessfully treated by surgery; and (12) adverse events (AEs) (defined as an untoward medical occurrence associated with the use of MSCs whether related to the MSCs or not).
Assessment of the quality of studies was performed using the Cochrane risk of bias tool [12].
Statistical analysis
The meta-analysis was performed using the metaprop command of the meta package in R (version 3.4.2) [13] and RevMan5.3 (Cochrane Collaboration, Oxford, UK) to assess the efficacy (clinical healing and response) and safety (AEs, studies with a comparison arm were included in the meta-analysis). OR and related 95% CIs were calculated to compare MSCs with control cohorts. Log transformation was used to calculate pooled proportions under the fixed and random-effects model [14]. The Chi-square test (P < 0.05 indicating statistical significance) and the I2 statistic (an I2 of ≥ 50%, < 50% indicating substantial and low heterogeneity, respectively) were used to qualitatively and quantitatively evaluate statistical heterogeneity, respectively. Subgroup data were analyzed using the Chi-square test at the subgroup analysis, and P < 0.05 was considered statistically significant.
Results
Literature search
The initial literature retrieval identified 2644 citations. After reading through the title and abstract to exclude the articles, these not meet the inclusion criteria. Of the final 13 studies selected for inclusion in the review [15,16,17,18,19,20,21,22,23,24,25,26,27]. Five studies were RCTs [16, 18, 23, 24, 27], and eight studies were non -randomized experimental studies [15, 17, 19,20,21,22, 25, 26]. The detailed literature screening process is shown in Fig. 1. Eleven studies used adipose-derived MSCs [15, 16, 18,19,20,21,22, 24,25,26,27], and eight studies used autologous MSCs [15,16,17,18, 20,21,22, 26]. Five studies used allogeneic MSCs [19, 23,24,25, 27] and two studies used bone-marrow-derived MSCs [17, 23]. In seven studies, an-TNF had been stopped since enrolment [15,16,17, 19,20,21, 25], and six studies maintained stable dose of anti-TNF during the entire study period [18, 22,23,24, 26, 27]. In four studies, the dosage of MSCs was determined based on the fistula size [20,21,22, 25], which was estimated from the diameter and length of the fistula. Eight studies used the fixed dose of MSCs [15,16,17,18,19, 23, 24, 27]. One study used MSC-coated matrix fistula plugs [26]. Study demographics and clinical characteristics are summarized in Table 1.
Comparison of MSCs vs control (local therapy)
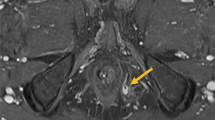
Five RCTs [16, 18, 23, 24, 27] reported raw data on fistulas healing of patients with MSCs. Using RevMan for meta-analysis, in a fixed-effects model, MSCs group were more effective for fistulas healing than placebo with an OR of 2.05 (95% CI 1.41, 3.00), with no heterogeneity between the studies (I2 = 0%) (Fig. 2). Pelvic MRI is a non-invasive, highly accurate examination for the diagnosis and classification of fistula and, therefore, considered to be the imaging gold standard for CD fistulas [28]. It also facilitates early detection of fistula recurrence. Four RCTs using MRI to evaluate the healing of fistulas were pooled [18, 23, 24, 27], yielding an OR of 1.95 (95% CI 1.33, 2.87) for achieving fistulas healing in patients who received MSCs vs control (Fig. 3), no heterogeneity (I2 = 0%).
Efficacy of MSCs for pCD (local therapy)
Thirteen studies reported raw data on clinical healing of patients after MSCs therapy with substantial heterogeneity (I2 = 67%), and the pooled HR was 63% (95% CI 0.53, 0.74) (Fig. 4). Eleven studies [15,16,17, 19,20,21,22,23,24,25, 27] reported raw data on clinical response of patients treated with MSCs. A random-effects pooled rate of clinical response was 30% (95% CI 0.18, 0.48) (Fig. 5). When MRI was used to evaluate the healing of fistulas, the random-effects pooled rate of healing was 56% (95% CI 0.46, 0.69) (8 studies [17,18,19, 23,24,25,26,27]) (Fig. 6).
Subgroup analysis of efficacy of MSCs for pCD (local therapy)
In a fixed-effects model, autologous MSCs [15,16,17,18, 20,21,22, 26] were more effective for the healing of perianal fistulas than allogeneic MSCs [19, 23,24,25, 27] (79% vs 52%), with a significantly statistical difference (P < 0.05) (Fig. 7). Two studies [17, 23] reported raw data on the outcome of patients with bone-marrow-derived MSCs. The pooled rate of clinical healing was 57% compared to 64% for patients who underwent adipose-derived MSCs, with no statistically significant differences (P > 0.05) (data not shown). Six studies [18, 22,23,24, 26, 27] reported raw data on the healing of pCD that maintained stable dose of anti-TNF during the entire study period, the pooled rate of clinical healing was 63% compared to 61% (in 7 studies [15,16,17, 19,20,21, 25]) of patients who had been stopped an-TNF after enrolment, with no statistically significant differences (P > 0.05) (data not shown). In a fixed-effects model, the dosage of MSCs [20,21,22, 25] determined based on the fistula size were more effective for the healing of perianal fistulas than fixed-dose of MSCs [15,16,17,18,19, 23, 24, 27] (80% vs 55%), with a significantly statistical difference (P < 0.05) (Fig. 8).
Safety of MSCs for pCD (local therapy)
The included studies demonstrate a good safety and tolerability profile of MSC treatment for pCD. In our study, safety is assessed through AEs analysis: there were no significant increases in AEs (OR = 1.14; 95% CI 0.75, 1.74; P = 0.54) when MSC and non-MSC cohorts were compared (Fig. 9). No MSC-related AE has been reported so far. Common AEs such as anal pain, anal bleeding, fever, abdominal pain, diarrhea, and perianal abscess are mostly transient and rarely result in patients needing hospitalization or in disability. In addition, these AEs are associated with local injection procedures of MSCs (e.g., curettage of a fistula and closure of an internal opening) or the progression of the disease itself rather than the MSCs themselves. Complications often associated with surgery such as fecal incontinence have not been reported in MSCs’ studies. Considering their immunosuppressive properties, it is not clear whether MSCs increase the risks of malignancy at present. Some animal studies suggested that MSCs could promote tumour growth [29, 30], but this has never been confirmed by clinical studies. One patient treated with 1 × 107 MSCs developed an adenocarcinoma of the cecum with peritoneal carcinomatosis > 15 months after the surgical intervention [23]. Baseline and week-12 endoscopy of the rectum revealed no abnormalities. In addition, the last endoscopy of the entire colon and the biopsies taken at that time was completely normal. Moreover, given that MSCs have a very limited lifespan in the body and the patient had a family history of colon cancer, we think that the occurrence of the tumour is associated with genetic factors rather than with MSCs. One patient in the study by de la Portilla et al. [19] was diagnosed with uterine leiomyomata during follow-up. It should be taken into account that uterine fibroids are noncancerous growths of the uterus that often appear during childbearing years and are not associated with an increased risk of uterine cancer In view of these considerations, this study did not reveal any specific signs of carcinogenicity. A follow-up of up to 4 years suggests that MSCs have no carcinogenic risk [18]. However, we should consider that in this study, the number of patients is small, and there is no standard on the evaluation of safety. Therefore, in the future, we need more patients with long-term follow-up, to thoroughly evaluate the safety of MSC treatment for pCD.
Discussion
In this meta-analysis, we used different softwares to analyze the efficacy of MSCs for pCD. However, there are several limitations: (1) studies used different types and sources of MSCs including adipose tissue, bone marrow from autologous as well as allogeneic; (2) the timepoint of fistula healing fluctuates significantly (8 weeks–40 months); (3) different definitions of fistula healing, only eight studies used pelvic MRI, and the rest defined healing as reepithelialization of external opening; (4) different dosages and modalities of administration; (5) exclusion of younger patients; and (6) through the Cochrane risk of bias tool, we can see that the eight non-randomized experimental studies included are studies with poor stability and quality.
Now, as stem-cell-based treatments are gaining a strong foothold in fistula management worldwide, more clinical studies are being performed to further ascertain the efficacy and safety of MSC therapy for pCD. Standardization is crucial to assess the efficacy of current and future local treatment strategies. Therefore, with the goal of optimizing this emerging therapy, we need to propose a standardized definition of AEs, and need more objective definitions of the healing of pCD (e.g., endoscopy, C-reactive protein, fecal calprotectin, and imaging including MRI) in future studies.
Several meta-analysis have shown that MSCs are effective and safe for the treatment of pCD [31,32,33,34,35]. However, the results of these studies are still quite different, the explanation for this result may be due to the different sources, different differentiation and regeneration capacity of MSCs and different clinical trials for the isolation of MSCs, different culture programs, and the patient’s age, severity of the disease and other factors may also affect the efficacy of MSCs. In our review, autologous, MSCs have shown more promising results than allogeneic MSCs in pCD fistulas. Moreover, the use of autologous MSCs is more acceptable and there is no ethical conflict. However, the possibility of disease-related effects on autologous MSCs must be taken into account. In addition, autologous MSCs are not immediately available upon request, because isolation and expansion of MSCs to a sufficient numbers of cells require weeks that may result in treatment delay. In addition, due to the inflamed intestinal mucosa, patients’ nutritional status can be poor and patients are frequently very thin, so it is often difficult to gain access to an adequate amount of MSCs. Allogeneic MSCs, easily obtained from a healthy donor, is a product accessible to more patients. Thus, an easily available treatment can be rapidly administered from a completely validated cell bank and provides an affordable therapy to large numbers of patients. In some trials, MSCs from young healthy donors that may have better immunomodulatory and regenerative potential [36, 37] may be selected to avoid the effects of the underlying autoimmune disease. Therefore, our study shows that the efficacy of autologous MSCs is better than that of allogeneic MSCs, but we need to consider the timeliness and cost-effectiveness of treatment to optimize the treatment. There were no statistically significant differences in the HR in our study when the origin of MSCs used (adipose-derived vs bone-marrow-derived) was considered. It should be noted that human adipose tissue is plentiful and easily accessible, and contains a large number of stem cells compared to other tissues in the body. Obtaining adipose tissue minimizes side effects on donors (regardless whether patient or healthy donor). To obtain bone-marrow MSCs in some special donors such as patients with a history of myocardial infarction is dangerous. More and more data are becoming available on the differences between bone-marrow- and adipose tissue-derived MSCs, including on their immunomodulatory properties. One study [37] suggests that adipose tissue-derived MSCs might be superior to bone-marrow MSCs in suppressing immune responses in vitro. Therefore, adipose tissue-derived MSCs can be considered a priority in the future. There were only two studies [17, 23] used bone-marrow-derived MSCs, which was a limitation of our study. More RCTs should compare their efficacy and safety. MSCs were used alongside with anti-TNF in some clinical studies, and they share common targets. Their interaction should be studied carefully. In our review, combined anti-TNF with MSCs had no synergistic effect on the healing of fistulas. Most patients included in our study were refractory to anti-TNF. Treatment of anti-TNF does not seem to affect the long-term efficacy of MSCs for refractory patients, and the long-term application of anti-TNF caused by economic problems and AEs. The exposure of MSCs to physiological concentrations of anti-TNF agents does not affect their survival and their inhibitory capacities on peripheral blood mononuclear cell proliferation [38]. However, whether there is a synergistic effect in combination with MSCs in patients with a response to anti-TNF remains to be determined by further studies.
There are still many unsolved questions concerning the modalities of administration and dosage. In our review, there were two administration methods. One was locally injected MSCs; the fistula tract was thoroughly curetted and irrigated under anesthesia; and the internal opening was closed MSCs which were injected into the submucosa surrounding the internal opening and the fistula track wall. The other method was using MSC-coated matrix fistula plugs. In this study, the volume of injected MSCs proportional to fistula size improved the HR compared with fixed-dose MSCs. CD fistulas usually involve multiple trajectories over a wide range of regions, so treatment of the fistula with a fixed small dose of cells may not be sufficient. We believe that cell number in proportion to fistula size can improve the efficacy, because cells can be injected evenly into the fistula. Therefore, our study provides guidance for the modalities of administration of MSCs. Due to the limitations of studies, it is difficult to provide recommendations on the optimal dose. However, Molendijk et al. [23] reported that local therapy with 3 × 107 MSCs showed superior fistulas healing compared with 9 × 107 MSCs treatment (80% vs 20%. The authors argued that higher cell concentrations could result in a lower survival rate and/or cell function and that a larger number of cells could be immunogenic resulting in increased clearance or deactivation of the cells. This provides a guidance in choosing the optimal dosage of MSCs for the treatment of pCD.
Studies included in our meta-analysis used variable definitions of fistulas healing. We showed that when pelvic MRI was used to evaluate fistula healing, the HR fell. We think that healed fistula was defined as complete closure evident on clinical examination and reepithelialization of the external opening of the fistula was not objective and accurate, as it cannot replace the inside of the entire fistula. Pelvic MRI is considered be the imaging gold standard for CD fistula, but MRI is insensitive to reduced fistula caliber. Therefore, we need improved instruments for evaluation of perianal CD fistula healing. Parks’ classification of the anatomy of perianal fistulas: (1) intersphincteric; (2) transsphincteric; (3) suprasphincteric; (4) extrasphincteric; and (5) not involving the sphincter complex is a clinically useful classification of perianal fistulas in CD and can help the treating physician to determine optimal management strategy disease. However, due to the limitations of our study, differences in classification of pCD were not analyzed in detail and compared with the differences in response to MSC treatment. RCTs are needed to clarify the mechanism of MSCs for treating CD fistulas by directly comparing the therapeutic effects between MSCs and immunomodulators, biologics, and surgical procedures. Comprehensive consideration of factors that affect the healing of fistulas (such as gender, age, diameter/length of fistula, type of fistula, CD duration, CDAI activity, and other factors), and the selection of appropriate MSCs (type, source, dose, frequency of injection, and mode of delivery) for patients receive the optimal treatment must be further investigated.
Assessment of study quality
There was overall high risk of performance bias, detection bias, and reporting bias in the studies included in the review (Fig. 10a, b).
Conclusions
The results of this study are encouraging, and MSCs appear to offer a safe and effective treatment approach for pCD fistulas. Based on subgroup analysis, autologous, adipose MSCs had relatively higher rates of clinical healing. MSC dosage in proportion to fistula size also had higher rates of clinical healing. The efficacy of MSCs does not seem to be influenced by prior unsuccessful treatment with anti-TNF and may be an attractive option for patients failing this treatment. However, these findings should be interpreted with much caution owing to the limited number of studies and potential biases, More RCTs are needed to support our conclusions.
References
Schwartz DA, Loftus EV Jr, Tremaine WJ et al (2002) The natural history of fistulizing Crohn’s disease in Olmsted County, Minnesota. Gastroenterology 122:875–880
Hellers G, Bergstrand O, Ewerth S, Holmström B (1980) Occurrence and outcome after primary treatment of anal fistulae in Crohn’s disease. Gut 21:525–527
Domènech E, Hinojosa J, Nos P et al (2005) Clinical evolution of luminal and perianal Crohn’s disease after inducing remission with infliximab: how long should patients be treated? Aliment Pharmacol Ther 22:1107–1113
Van Assche G, Dignass A, Reinisch W et al (2010) The second European evidence-based consensus on the diagnosis and management of Crohn’s disease: special situations. J Crohns Colitis 4:63–101
Beaugerie L, Seksik P, Nion-Larmurier I et al (2006) Predictors of Crohn’s disease. Gastroenterology 131:334–335
Jiang XX, Zhang Y, Liu B et al (2005) Human mesenchymal stem cells inhibit differentiation and function of monocyte derived dendritic cells. Blood 105:4120–4126
Beyth S, Borovsky Z, Mevorach D et al (2005) Human mesenchymal stem cells alter antigen-presenting cell maturation and induce T-cell unresponsiveness. Blood 105:2214–2219
Spaggiari GM, Abdelrazik H, Becchetti F, Moretta L (2009) MSCs inhibit monocyte-derived DC maturation and function by selectively interfering with the generation of immature DCs: central role of MSC-derived prostaglandin E2. Blood 113:6576–6583
Melief SM, Geutskens SB, Fibbe WE, Roelofs H (2013) Multipotent stromal cells skew monocytes towards an anti-inflammatory interleukin-10-producing phenotype by production of interleukin-6. Haematologica 98:888–895
Melief SM, Schrama E, Brugman MH et al (2013) Multipotent stromal cells induce human regulatory T cells through a novel pathway involving skewing of monocytes toward anti-inflammatory macrophages. Stem Cells 31:1980–1991
Moher D, Liberati A, Tetzlaff J et al (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339:b2535
Shuster J (2011) Review: Cochrane handbook for systematic reviews for interventions, Version 5.1.0, published 3/2011. Julian P.T. Higgins and Sally Green, Editors. Res Synth Methods 2:126–130
Schwarzer G (2015) Meta: general package for meta-analysis. R Package Version 4.1-0. R Foundation, Vienna
Freeman MF, Tukey JW (1950) Transformations related to the angular and the square root. Ann Math Stat 21:607–611
Garcia-Olmo D, Garcia-Arranz M, Herreros D, Pascual I, Peiro C, Rodriguez-Montes JA (2005) A phase I clinical trial of the treatment of Crohn’s fistula by adipose mesenchymal stem cell transplantation. Dis Colon Rectum 48:1416–1423
Garcia-Olmo D, Herreros D, Pascual I et al (2009) Expanded adipose-derived stem cells for the treatment of complex perianal fistula: a phase II clinical trial. Dis Colon Rectum 52:79–86
Ciccocioppo R, Bernardo ME, Sgarella A et al (2011) Autologous bone marrow-derived mesenchymal stromal cells in the treatment of fistulising Crohn’s disease. Gut 60:788–798
Guadalajara H, Herreros D, De-La-Quintana P, Trebol J, GarciaArranz M, Garcia-Olmo D (2012) Long-term follow-up of patients undergoing adipose-derived adult stem cell administration to treat complex perianal fistulas. Int J Colorectal Dis 27:595–600
de la Portilla F, Alba F, Garcia-Olmo D, Herrerias JM, Gonzalez FX, Galindo A (2013) Expanded allogeneic adipose-derived stem cells (eASCs) for the treatment of complex perianal fistula in Crohn’s disease: results from a multicenter phase I/IIa clinical trial. Int J Colorectal Dis 28:313–323
Cho YB, Lee WY, Park KJ, Kim M, Yoo HW, Yu CS (2013) Autologous adipose tissue-derived stem cells for the treatment of Crohn’s fistula: a phase I clinical study. Cell Transpl 22:279–285
Lee WY, Park KJ, Cho YB et al (2013) Autologous adipose tissue-derived stem cells treatment demonstrated favorable and sustainable therapeutic effect for Crohn’s fistula. Stem Cells (Dayton, Ohio) 31:2575–2581
Cho YB, Park KJ, Yoon SN et al (2015) Long-term results of adipose-derived stem cell therapy for the treatment of Crohn’s fistula. Stem Cells Transl Med 4:532–537
Molendijk I, Bonsing BA, Roelofs H et al (2015) Allogeneic bone marrow-derived mesenchymal stromal cells promote healing of refractory perianal fistulas in patients with Crohn’s disease. Gastroenterology 149(918–27):e6
Panes J, Garcia-Olmo D, Van Assche G et al (2016) Expanded allogeneic adipose-derived mesenchymal stem cells (Cx601) for complex perianal fistulas in Crohn’s disease: a phase 3 randomised, double-blind controlled trial. Lancet (London, England) 388:1281–1290
Park KJ, Ryoo SB, Kim JS et al (2016) Allogeneic adipose-derived stem cells for the treatment of perianal fistula in Crohn’s disease: a pilot clinical trial. Colorectal Dis 18:468–476
Dietz AB, Dozois EJ, Fletcher JG et al (2017) Autologous mesenchymal stem cells, applied in a bioabsorbable matrix, for treatment of perianal fistulas in patients with Crohn’s disease. Gastroenterology 153:59–62.e2
Panés J, García-Olmo D, Van Assche G et al (2018) Long-term efficacy and safety of stem cell therapy (Cx601) for complex perianal fistulas in patients with Crohn’s disease. Gastroenterology 154:1334–1342.e4
Sinha R, Murphy P, Hawker P, Sanders S, Rajesh A, Verma R (2009) Role of MRI in Crohn’s disease. Clin Radiol 64:341–352
Ren G, Zhao X, Wang Y et al (2012) CCR29-dependent recruitment of macrophages by tumor-educated mesenchymal stromal cells promotes tumor development and is mimicked by TNFα. Cell Stem Cell 11:812–824
Song B, Kim B, Choi SH et al (2014) Mesenchymal stromal cells promote tumor progression in fibrosarcoma and gastric cancer cells. Korean J Pathol 48:217–224
Dave M, Mehta K, Luther J, Baruah A, Dietz AB, Faubion WA Jr (2015) Mesenchymal stem cell therapy for inflammatory bowel disease: a systematic review and meta-analysis. Inflamm Bowel Dis 21:2696–2707
Cao Y, Ding Z, Han C, Shi H, Cui L, Lin R (2017) Efficacy of mesenchymal stromal cells for fistula treatment of crohn’s disease: a systematic review and meta-analysis. Dig Dis Sci 62:851–860
Qiu Y, Li MY, Feng T et al (2017) Systematic review with meta-analysis: the efficacy and safety of stem cell therapy for Crohn’s disease. Stem Cell Res Ther 8:136
Lightner AL, Wang Z, Zubair AC, Dozois EJ (2018) A systematic review and meta-analysis of mesenchymal stem cell injections for the treatment of perianal Crohn’s disease: progress made and future directions. Dis Colon Rectum 61:629–640
Choi S, Jeon BG, Chae G, Lee SJ (2019) The clinical efficacy of stem cell therapy for complex perianal fistulas: a meta-analysis. Tech Coloproctol. https://doi.org/10.1007/s10151-019-01994-z
Wagner W, Bork S, Horn P et al (2009) Aging and replicative senescence have related effects on human stem and progenitor cells. PLoS One 4:e5846
Ivanova-Todorova E, Bochev I, Mourdjeva M et al (2009) Adipose tissue-derived mesenchymal stem cells are more potent suppressors of dendritic cells differentiation compared to bone marrow-derived mesenchymal stem cells. Immunol Lett 126:37–42
Duijvestein M, Molendijk I, Roelofs H et al (2011) Mesenchymal stromal cell function is not affected by drugs used in the treatment of inflammatory bowel disease. Cytotherapy 13:1066–1073
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The present paper as a review of the literature was exempt from approval.
Informed consent
For this review of literature, informed consent was not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cheng, F., Huang, Z. & Li, Z. Mesenchymal stem-cell therapy for perianal fistulas in Crohn’s disease: a systematic review and meta-analysis. Tech Coloproctol 23, 613–623 (2019). https://doi.org/10.1007/s10151-019-02024-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-019-02024-8