Abstract
Background
Rectoanal intussusception (RAI) is a common finding on evacuation proctography in patients with defecation disorders. However, it remains unclear whether intussusception morphology affects the severity of fecal incontinence (FI). The aim of this study was to examine the effect of morphology during defecation on the severity of FI in patients with RAI.
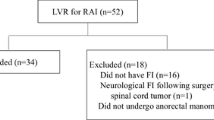
Methods
We included 80 patients with FI who were diagnosed as having RAI on evacuation proctography. Various morphological parameters were measured, and the level of RAI was divided by the extent of descent onto (level I) or into (level II) the anal sphincter. FI symptoms were documented using the FI Severity Index (FISI).
Results
Twenty-eight patients had level I and 52 had level II RAI. The mean (range) FISI score was 24.0 (8–47). FISI scores tended to be significantly higher in level II than in level I [26.3 (10–47) vs. 21.8 (8–42); p = 0.05]. The mean anterior intussusception descent was significantly greater in level II than in level I [24.2 (9.2–39.5) vs. 17.7 (7.8–39.4) mm; p < 0.0001]. Regression analysis showed that anterior intussusception descent was predictive of increased FISI scores.
Conclusions
The severity of FI may be affected by anterior intussusception descent in patients with RAI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rectal intussusception (RI) is an infolding of the rectal wall that may occur during defecation. In patients with disordered anorectal function, RI is a common finding on evacuation proctology [1], the current ‘gold standard’ investigation for identifying this condition [2]. RI may cause symptoms of obstructive defecation (OD) and fecal incontinence (FI) [1–3]. RI can be classified into rectorectal intussusception (RRI) and rectoanal intussusception (RAI), and the latter is further divided into level I (descends onto the sphincter/anal canal) and level II (descends into the sphincter/anal canal) [4]. In patients with RAI failing conservative treatment, surgery is considered [5, 6].
Rectal intussusception (RI) has been seen in asymptomatic individuals at proctography [4], and the clinical and pathological significance of this finding has been questioned [7]. Recent studies have addressed the differences in anorectal morphology during defecation between patients with evacuation disorder and asymptomatic individuals, and intussusception thickness was significantly greater in patients with symptomatic RI [7, 8].
However, it remains unclear whether the severity of symptoms is affected by the difference in anorectal morphology in patients with RAI. A previous retrospective study classified RAI into two groups based on intussusception descent during defecation (<10-mm descent of the rectal wall or ≥10-mm descent) and showed that the incidence of FI was the same in the two groups [9]. Nevertheless, more patients with RAI than with RRI had FI [10]. The aim of the study was to explore the effect of the morphology of RAI during defecation on the severity of FI in patients with RAI.
Materials and methods
Patients seen in the proctology clinic with symptoms of rectal evacuatory disorder underwent evacuation proctography as a part of the investigation protocol. Data for the patients with RAI were prospectively entered into a pelvic floor database. The level of RAI was divided into level I or level II. FI symptoms were divided into urge and passive incontinence. A functional inventory of FI symptoms was documented using the Fecal Incontinence Severity Index (FISI) score [11]. Each patient underwent anorectal manometry. Examinations were performed with the patient in the lateral position, and no bowel preparation was used. Anal pressure was measured with a catheter-tip pressure transducer. A transanal ultrasound examination was not performed routinely.
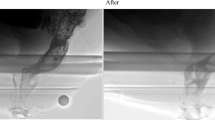
Proctography technique was standardized. The small bowel was opacified with a mixture containing 100 mL Barister™ (Barium sulfate 100 % w/w; Fushimi Health Care Ltd., Kagawa, Japan) and 10 mL Urografin (60 % w/w; Bayer Pharmaceutical Ltd. Japan), ingested 30 min prior to the procedure. The patient was placed in the left lateral position on the fluoroscopic table; barium installation (50 mL) and air insufflation were performed to improve the quality of the contrast image. Synthetic stool consisting of barium sulfate, porridge oats, and water was inserted into the rectum using a 50-mL bladder syringe. A total of 150 mL was introduced. The patient was then seated on a radiolucent commode on a fluoroscopic X-ray table. Lateral X-rays of the pelvis in resting, squeezing, and pushing positions were taken. The patient was then asked to bear down maximally during evacuation. Images from proctography were analyzed by one of the authors (T. T.), who is experienced in the evaluation [12] and was blinded at that time to the symptomatology of the individual patients. Measurements were taken using the X-ray flat-panel detector (Toshiba Ultimax, Toshiba Medical Systems, Japan) calibrated to a metal globe or a paper clip of known dimensions screened within the image field during proctography.
The following morphological parameters were measured according to the study by Dvorkin et al. [8]: (1) thickness of both the anterior and posterior components of the intussusception, measured at the upper point of invagination between the intussuscipiens edge and the intussusception contour (Fig. 1a: T), with thickness greater than 3 mm diagnosed as a full-thickness intussusception (less than 3 mm was designated as a mucosal prolapse); (2) the distance from the point of ‘take-off’ of the intussusception to the anorectal junction (defined radiologically as the point where the posterior rectal outline formed an angle with the anus) (Fig. 1b: L); and (3) intussusception descent taken from the point of ‘take-off’ to the most distal point of the intussusception (Fig. 1a: D1, D2).
Evacuation proctography showing a anterior intussusception descent (D1), posterior intussusception descent (D2), and intussusception thickness (T), b during mid-evacuation showing the ‘take-off’ of the impending intussusception L distance from the point of ‘take-off’ of the intussusception to the anorectal junction
All measurements were taken from the maximal straining image during defecation. In addition, pelvic floor descent during defecation was estimated by the extent to which the anorectal junction descended in relation to the inferior margin of the ischial tuberosity. Rectocele was classified as small (<2 cm in depth), moderate sized (2–4 cm in depth), or large (>4 cm in depth). The size was calculated in a standard fashion in the anterior–posterior dimension by measuring the distance between the most ventral part of the anterior rectal wall and an extrapolated line of the expected portion of the rectal wall [13]. Enterocele was diagnosed when the extension of the loop of small bowel was located between the vagina and rectum [1]. Informed consent was obtained from all patients. This study was approved by the Ethics Committee of Kameda Medical Center.
Statistical analysis
Statistical analysis was performed using SPSS version 11.0 (SPSS Inc., Chicago, IL, USA). The continuous variables were expressed as means (range). Univariate associations were analyzed using Student’s t test or Pearson’s correlation coefficients for continuous variables and the Chi-square or Fisher’s exact test for categorical variables. A stepwise multiple regression analysis was used to establish which morphological parameters of RAI best predicted the severity of FI. In the regression analysis, FISI scores were selected as the dependent variables. Independent variables included intussusception thickness, intussusception descent, and point of ‘take-off,’ for both anterior and posterior components. Age, sex, level of RAI, pelvic floor descent, grade of rectocele, the presence of enterocele, incomplete rectal emptying, the use of laxatives, maximum resting pressure, and maximum squeeze pressure were analyzed as additional covariates. p < 0.05 was taken as significant for all tests except the stepwise multiple regression, where valuables were entered at a p value ≤0.01 to reduce the risk of type I errors.
Results
Demographic and clinical findings
Between June 2011 and June 2015, 292 patients underwent evacuation proctography, and 142 (49 %) were found to have RAI. Of these, 62 had OD alone, while 80 had FI (34 with FI alone, and 46 with mixed FI and OD) and were included in the study. The patients’ mean age was 75 (48–95) years. Twenty-eight patients had level I and 52 had level II RAI. The mean FISI score was 24.0 (8–47). FISI scores tended to be significantly greater in level II than in level I cases. The type of FI was passive 65 (81 %), urgent 13 (16 %), and both 2 (3 %), respectively (Table 1). On the evaluation of FISI scores, 23 (29 %) patients had used laxatives.
Seven patients had associated urinary incontinence, eight had hemorrhoids, and one had pelvic organ prolapse. Overall, 30 (38 %) patients had had previous surgery including appendectomy (8), hysterectomy (6), transvaginal surgery for pelvic organ prolapse (4), surgery for hemorrhoids or anal fistula (8), oophoro-salpingectomy (5), anterior resection (1), and sphincter repair (1). The mean number of vaginal deliveries among 68 female patients was 1.8 (0–5). One patient had an obstetric injury. After the evaluation, 43 (54 %) patients underwent surgery including laparoscopic ventral rectopexy (n = 35) and stapled transanal rectal resection (n = 6) in our institution.
The mean maximum resting and squeeze pressure was 57 (32–99) and 204 (55–747) cmH2O, respectively. Fifty-two (65 %) patients with RAI had normal resting pressure and 48 (60 %) had normal squeeze pressure (the defined in-hospital normal ranges were 55–110 and 150–300 cmH2O, respectively). There was no significant difference between the resting pressures at the two RAI levels. A transanal ultrasound scan was done in 25 patients (31 %), and no sphincter defect was found in any patient.
Intussusception morphology
The morphology of the intussusception is shown in Table 2. The anterior intussusception descent and posterior intussusception thickness were significantly greater in level II than in level I RAI, respectively. However, no differences were observed in the position of the point of inversion and anterior intussusception thickness between the groups. Rectocele grade, the presence of enterocele, and the incidence of incomplete rectal emptying were not significantly different between the groups.
When the morphology of RAI was compared between the 80 patients with FI and 62 patients without FI (OD alone), the incidence of level II was significantly greater in the former group than that in the latter group (52/80 vs. 23/62, p = 0.001). Similarly, the patients with FI had greater pelvic floor descent [22.9 (−16.1–45.4) vs. 19.1 (0–42.9) mm, p = 0.03] and anterior intussusception descent [21.9 (7.4–39.5) vs. 17.0 (7.0–52.8) mm, p < 0.0001], compared to those without FI, respectively.
Pearson’s correlation coefficients
The correlations between FISI scores and variable morphological parameters or anal pressure are shown in Table 3. Anterior and posterior intussusception descent was significantly associated with FISI scores, respectively, i.e., the greater the depth, the greater the FISI scores.
Regression analysis
The results of stepwise multiple regression analysis done using morphological and demographic variables are shown in Table 4. The anterior intussusception descent was significantly associated with increased FISI scores.
Discussion
To the best of our knowledge, this is the first study to demonstrate that anterior intussusception descent is predictive of increased FISI scores.
Fecal incontinence (FI) was the most common symptom at presentation in patients with RAI, in line with recent reports [1, 3, 8]. FI was found in about half of the patients with RAI, with the majority complaining of passive incontinence in this study. Passive incontinence suggests dysfunction of the internal sphincter. In this study, 28 (35 %) patients with RAI had lower than normal resting pressure. Although this was not associated with increased FISI scores, the effect of RAI on continence may occur partly through a reduction in internal sphincter tone. Harmstom et al. [14] have shown that there is a significant reduction in resting pressure with increased prolapse in RI.
RAI may cause passive FI more commonly by inappropriate activation of the rectoanal inhibitory reflex (RAIR), as previously suggested by Faroux et al. [15]. The present evacuation proctography findings showed that the site of ‘take-off’ appeared at about 5 cm from the anorectal junction anteriorly, consistent with previous reports [2, 8]. This anatomical point corresponds anteriorly with the distal limit of the peritoneum within the pouch of Douglas, and it may be the weakest point in the structures supporting the rectum. It is possible that the higher intra-abdominal pressure created during daily life may expose this anterior aspect of the rectal wall to forces consistent with the development of anterior or circumferential RAI and may trigger the RAIR. In fact, the anterior rectal wall descended easily on anoscopic observation in patients with RAI, when they were asked to bear down even in the lateral position. Therefore, the more the anterior intussusception descends, the more easily the reflex would be triggered. An additional possibility is that the intussusception may present constantly within the distal rectum or anal canal, leading to the RAIR and FI. In fact, RAI is occasionally noted during physical examination. Posterior intussusception descent was not significantly associated with FI in the present study. The reason for this is not certain, but as mentioned earlier, posterior intussusception may not occur independently during daily life, and in circumferential intussusception the initiative may be taken by the anterior RAI, which appears to be a more important factor in the development of FI.
Urge incontinence in patients with RAI is harder to explain, although the incidence was low in this study. A reduction in rectal wall compliance, due to chronic irritation, of the prolapsed rectal wall has been suggested in a previous study [3].
Other mechanisms leading to FI may be manometric alterations such as abnormal rectal waves, intermittent relaxation of the internal sphincter [16], or incomplete rectal emptying [17], which were not, however, correlated with the severity of FI in this study.
Laparoscopic ventral rectopexy (LVR) for the treatment of RAI has been reported to improve FI. Formijne Jonkers et al. [18] have recently reported that 157 patients underwent LVR for RAI, and FI improved or was cured in 78 % of the patients. Similar functional results were reported by other authors [5, 6, 19, 20]. These results suggest that the correction of the anterior rectum may be more important for the treatment of FI.
It would be natural that either intussusception descent or thickness of both components becomes greater with increasing prolapse. However, there was no significant difference in the anterior intussusception thickness between the levels of RAI in this study. This may be understandable given that the anterior intussusception was thicker than the posterior in either level of RAI (p < 0.0001), and rectocele or enterocele was frequently associated with RAI, irrespective of its level. The reason for no significant difference in the posterior intussusception descent between the levels of RAI was uncertain, but the mesorectum may have an inhibitory effect on the descent.
The majority of patients with RAI who had FI in this study were female as in previous studies [3, 9]. Women are more commonly affected than men, mainly because of the damaging effect of pregnancy/vaginal delivery on the pelvic floor and anal sphincter complex, in combination with the deleterious effect of menopause [21]. The weakness of the pelvic floor and rectovaginal fascia allows descent of the middle compartment and the development of RI, rectocele, enterocele, and/or vaginal prolapse [22]. In our study, the patients with level II RAI tended to be significantly older than those with level I which was supported by the previous study which showed a strong relationship between age and prolapse grade [23]. In addition, FISI scores were almost significantly higher in level II than in level I (p = 0.05), and may become significant with increasing sample size. Inappropriate RAIR may be triggered more easily in patients with level II than those with level I.
It has been suggested that evacuation proctology should be one of the standard investigations for FI, because 27–63 % of patients with FI had proctologic evidence of RAI [10, 24]. In our institution, routine evacuation proctography has been used in these patients since 2011.
There are certain limitations to our study. It was a small study with a lack of data on transanal ultrasound. Also, the interpretation of the effect of the morphology of RAI on FI is limited because factors such as barium compound thickness and the degree of patient straining at the time of evacuation proctography may have an effect on morphological measurements or the level of RAI. Furthermore, RAI alone would not be the cause of FI, because 62 patients with OD alone were found to have RAI. As mentioned above, the level of RAI, pelvic floor descent, or anterior intussusception descent may have an additional effect on the appearance of FI.
Conclusions
The severity of FI may be affected by anterior intussusception descent in patients with RAI. Further studies are necessary to confirm the results.
References
Mellgren A, Bremmer S, Johansson C et al (1994) Defecography. Results of investigations in 2,816 patients. Dis Colon Rectum 37:1133–1341
Brodén B, Snellman B (1968) Procidentia of the rectum studied with cineradiography. A contribution to the discussion of causative mechanism. Dis Colon Rectum 11:330–347
Wijffels NA, Jones OM, Cunningham C, Bemelman WA, Lindsey I (2013) What are the symptoms of internal rectal prolapse? Colorectal Dis 15:368–373
Shorvon PJ, McHugh S, Diamant NE, Somers S, Stevenson GW (1989) Defecography in normal volunteers: results and implications. Gut 30:1737–1749
Slawik S, Soulsby R, Carter H, Payne H, Dixon AR (2008) Laparoscopic ventral rectopexy, posterior colporrhaphy and vaginal sacrocolpopexy for the treatment of recto-genital prolapse and mechanical outlet obstruction. Colorectal Dis 10:138–143
Collinson R, Wijffels N, Cunningham C, Lindsey I (2010) Laparoscopic ventral rectopexy for internal rectal prolapse: short-term functional results. Colorectal Dis 12:97–104
Pomerri F, Zuliani M, Mazza C, Villarejo F, Scopece A (2001) Defecographic measurements of rectal intussusception and prolapse in patients and in asymptomatic subjects. Am J Roentgenol 176:641–645
Dvorkin LS, Gladman MA, Epstein J, Scott SM, Williams NS, Lunniss PJ (2005) Rectal intussusception in symptomatic patients is different from that in asymptomatic volunteers. Br J Surg 92:866–872
Choi JS, Salum MR, Moreira H, Weiss EG, Nogueras JJ, Wexner SD (2000) Physiologic and clinical assessment of patients with rectoanal intussusception. Tech Coloproctol 4:29–33
Collinson R, Cunningham C, D’Costa H, Lindsey I (2009) Rectal intussusception and unexplained faecal incontinence: findings of a proctographic study. Colorectal Dis 11:77–83
Rockwood TH, Church JM, Fleshman JW et al (1999) Patient and surgeon ranking of the severity of symptoms associated with fecal incontinence: the Fecal Incontinence Severity Index. Dis Colon Rectum 42:1525–1532
Takahashi T, Yamana T, Sahara R, Iwadare J (2006) Enterocele: What is the clinical implication? Dis Colon Rectum 49:S75–S81
Bartram CI, Turnbull GK, Lennard-Jones JE (1988) Evacuation proctography: an investigation of rectal expulsion in 20 subjects without defecatory disturbance. Gastrointest Radiol 13:72–80
Harmston C, Jones OM, Cunningham C, Lindsey I (2011) The relationship between internal rectal prolapse and internal anal sphincter function. Colorectal Dis 13:791–795
Farouk R, Duthie GS, MacGregor AB, Bartolo DC (1994) Rectoanal inhibition and incontinence in patients with rectal prolapse. Br J Surg 81:743–746
Roberts JP, Williams NS (1992) The role and technique of ambulatory anal manometry. Baillieres Clin Gastroenterol 6:163–178
Dietz HP, Zhang X, Skek KL, Guzman RR (2015) How large does a rectocele have to be to cause symptoms? A 3D/4D ultrasound study. Int Urogynecol J 26:1355–1359
Formijne Jonkers HA, Poierrié N, Draaisma WA, Broeders IA, Consten EC (2013) Laparoscopic ventral rectopexy for rectal prolapse and symptomatic rectocele: an analysis of 245 consecutive patients. Colorectal Dis 15:695–699
Portier G, Kirzin S, Cabarrot P, Queralto M, Lazorthes F (2011) The effect of abdominal ventral rectopexy on faecal incontinence and constipation in patients with internal intra-anal rectal intussusception. Colorectal Dis 13:914–917
Tsunoda A, Ohta T, Kiyasu Y, Kusanagi H (2015) Laparoscopic ventral rectopexy for rectoanal intussusception: postoperative evaluation with proctography. Dis Colon Rectum 58:449–456
Jones OM, Cunningham C, Lindsey I (2011) The assessment and management of rectal prolapse, rectal intussusception, rectocoele, and enterocoele in adults. BMJ 342:c7099
González-Argenté FX, Jain A, Nogueras JJ, Davila GW, Weiss EG, Wexner SD (2001) Prevalence and severity of urinary incontinence and pelvic genital prolapse in females with anal incontinence or rectal prolapse. Dis Colon Rectum 44:920–926
Wijffels N, Collinson R, Cunningham C, Lindsey I (2010) What is the natural history of internal rectal prolapse? Colorectal Dis 12:822–830
Lazorthes F, Gamagami R, Cabarrot P, Muhammad S (1998) Is rectal intussusception a cause of idiopathic incontinence? Dis Colon Rectum 41:602–605
Acknowledgments
The authors would like to thank Dr. Yuko Tsunoda for the statistical analyses.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the Ethical Committee of Kameda Medical Center.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Tsunoda, A., Takahashi, T., Ohta, T. et al. Anterior intussusception descent during defecation is correlated with the severity of fecal incontinence in patients with rectoanal intussusception. Tech Coloproctol 20, 171–176 (2016). https://doi.org/10.1007/s10151-015-1423-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-015-1423-1