Abstract
Background
We prospectively evaluated the safety and efficacy of percutaneous cryoablation combined with transcatheter renal arterial embolization for the treatment of tumors ≥ 3 cm in diameter.
Methods
We included patients aged ≥ 20 years with histologically proven renal cell carcinoma with a tumor diameter ≥ 3 cm who were inoperable or refused surgery. Prior to ablation, transcatheter arterial embolization was performed using a mixture of absolute ethanol and iodized oil. All cryoablation procedures were performed percutaneously under computed tomography fluoroscopy guidance. The primary endpoint was safety, which was evaluated for adverse events using CTCAE version 4.0. The secondary endpoint was survival; overall survival, progression-free survival, and cancer-specific survival were calculated.
Results
From October 2013 to March 2016, 19 patients (mean age, 75 ± 13 years; 5 women, 14 men) were prospectively enrolled. The mean tumor diameter was 3.9 ± 0.7 (range 3.1–5.3) cm. Four grade 3 hematologic adverse events occurred, while no symptomatic grade ≥ 3 events occurred. The median follow-up period was 68 (range 52–84) months. During the follow-up period, two patients developed local tumor progression at 3 and 42 months after the initial ablative procedure; no patient showed distant metastasis. Two patients died from causes other than RCC. Overall survival, progression-free survival, and cause-specific survival were 100%, 95%, and 100% at 3 years, and 95%, 84%, and 100% at 5 years, respectively.
Conclusion
Percutaneous cryoablation combined with prior TAE for the treatment of tumors ≥ 3 cm in diameter was safe and achieved favorable survival.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In 2019, more than 370,000 new patients were diagnosed with renal cancer worldwide [1]. Although surgery remains the standard of care for renal cell carcinoma (RCC), percutaneous cryoablation (PCA) has become common for its treatment. Several studies have demonstrated good mid- and long-term oncologic outcomes [2,3,4,5], and several guidelines recognize the effectiveness of PCA under limited conditions, such as for patients at high surgical risk who are unsuitable as candidates for observation or who want proactive treatment [6,7,8]. However, in large-sized RCC, PCA has been associated with decreased treatment efficacy [3, 9, 10] and increased complication rates [11,12,13,14]. Additionally, both tumor extension outside the pseudocapsule and multifocal disease could be seen in RCC ≥ 4 cm in diameter [15, 16].
Transcatheter arterial embolization (TAE) prior to percutaneous ablation has been shown to improve oncologic outcomes in hepatocellular carcinoma, a typical hypervascular tumor [17,18,19]. Although the additional therapeutic effect of TAE on PCA against RCC has not been proven [20,21,22,23], it is clear that TAE has an ischemic effect on the tumor; it has been reported that TAE may reduce the risk of bleeding and facilitate tumor localization during computed tomography (CT)-guided percutaneous ablation if performed using radiopaque ethiodized oil [21,22,23,24]. The outcomes of PCA combined with prior TAE have not been fully evaluated; therefore, we prospectively evaluated the safety and efficacy of PCA with prior TAE for treatment of RCC ≥ 3 cm in diameter.
Materials and methods
Study design
The study was approved by the institutional review board of our institution and conducted in accordance with the Declaration of Helsinki. This study was registered in the University Hospital Medical Information Network Clinical Trials Registry (Study ID: 000012230). Written informed consent was obtained from all the patients prior to registration.
Endpoints
The primary endpoint was safety, and the secondary endpoint was survival. The safety component of this study was conducted on nine patients using the three-by-three method proposed by JIVROSG, which has been described previously [25]. The number of cases required for the evaluation of serious adverse events and efficacy rate was determined by a binomial test (null hypothesis H0: P = π0, alternative hypothesis H1: P = π), which is a one-sample test. For adverse events, if π0 = 0.10 and π = 0.30 (the predicted value of complications is 10%, and the test is discontinued if it is 30% or more), α = 0.05, β = 0.20, and n = 30. On the other hand, regarding the effective rate, if π0 = 0.50 and π = 0.80, then α = 0.05, β = 0.20, and n = 19. The required number of cases was 19; however, 21 cases were planned for as the number of cases was expected to deviate by 10%.
Inclusion and exclusion criteria
The inclusion criteria were as follows: (1) histologically proven RCC; (2) measurable tumor diameter of ≥ 3 cm and ≤ 7 cm; (3) inoperable or refusal of surgery; (4) age ≥ 20 years; (5) Eastern Cooperative Oncology Group performance status of 0 or 1; (6) acceptable laboratory parameters, tested within 14 days prior to the initial procedure (leukocyte count ≥ 2.5 × 109/L, platelet count ≥ 5.0 × 109/L, hemoglobin level ≥ 75 g/L, total bilirubin level ≤ 34.2 µmol/L, and prothrombin time-international normalized ratio ≤ 1.5); and (7) written informed consent.
The exclusion criteria were as follows: (1) presence of extra-renal tumor spread; (2) presence of venous tumor thrombus; (3) presence of a vital organ or major vessels along the planned penetrating route; (4) allergy to iodine or alcohol; (5) presence of severe comorbidities such as congestive heart failure (New Yolk Heart Association class ≥ III) or active infection other than chronic viral hepatitis; (5) presence of other cancers, except for tumors after curative resection, carcinoma in situ, or controllable breast and prostate cancer under treatment; (6) body temperature ≥ 38 °C; (7) difficulty in imaging evaluation; (8) pregnancy or possible pregnancy; and (9) being considered ineligible for this study by their attending physician.
Protocol treatment
All protocol treatments were performed on an inpatient basis. TAE was performed prior to PCA. Per protocol, the treatment interval between TAE and PCA should be a maximum of 30 days. The method of anesthesia during TAE or CA was determined by the operator and anesthesiologist, depending on the expected periprocedural pain. TAE was performed using a mixture of absolute ethanol and iodized oil (Lipiodol; Guerbet, Villepinte, France) at a ratio of 7:3. After the catheter tip was placed as selectively as possible to avoid embolization of blood vessels into the normal renal parenchyma, the embolic material was injected until blood flow stasis was achieved. All PCA sessions were performed percutaneously using an argon- and helium-based cryoablation system (CryoHit, Galil Medical, Arden Hills, MN, USA) with 17-gauge cryoprobes (Ice-Rod or Ice-Seed, Galil Medical). The type and number of cryoprobes used and the array of cryoprobes inserted depended on the consensual decision of experienced interventional radiologists. None of the patients were administered prophylactic antibiotic drugs before or after the procedure.
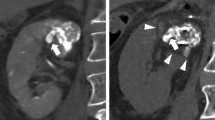
The cryoprobe was placed under CT fluoroscopy (Aquilion 64, Canon Medical Systems, Otawara, Japan) guidance. If the tumor was adjacent to a non-target organ, such as the colon, diluted contrast medium (typically 2% concentration) or carbon dioxide gas was infused to displace the organ away from the expected ablation zone (i.e., via hydrodissection or pneumo (balloon) dissection). After the cryoprobes were placed at the target site, PCA was performed in two freeze cycles separated by more than 2 min of passive thawing. The freezing time was 10–15 min for each cycle. After each freezing cycle, we confirmed that the low-attenuation area (i.e., the ice-ball) involved the tumor with a circumferential ablative margin on axial, coronal, and sagittal conventional CT images of 5-mm slice thickness. The ablation margin was set to 6 mm or more, as much as possible. If the ablative margin surrounding the target tumor was insufficient, cryoprobes were reinserted into the region where the ablation zone was insufficient, followed by additional freeze-and-thaw cycles. CT was repeated immediately after the procedure to evaluate adverse events. Furthermore, the initial efficacy was evaluated using CT or magnetic resonance imaging (MRI) 2 days after the session.
Data collection and outcome evaluation
Before protocol treatment, previous medical history, comorbidities, maximum tumor diameter, tumor histology, tumor location [26], and R.E.N.A.L nephrometry score [27] were recorded. Physical examination, urinalysis, and blood tests, including blood count and biochemical examination, were performed 1 and 3 days and 1, 3, 6, 12, and 24 months after PCA. CT or MRI examinations were performed 1, 3, 6, 12, and 24 months after PCA. We then conducted periodic follow-ups every 12 months as much as possible. Image evaluation was performed by the attending physician and at least one radiologist experienced in diagnostic imaging. Technical success was defined as the absence of residual tumor enhancement on the initial imaging evaluation at 2 days.
Regarding safety assessments, the incidence of adverse events was calculated based on the worst grade in each clinical course for all patients. The severity of all adverse events was evaluated according to the Common Terminology Criteria for Adverse Events, version 4.0. To evaluate renal function, each estimated glomerular filtration rate (eGFR) after the treatment was compared to the previous eGFR. The equation used for eGFR was as follows: glomerular filtration rate (mL/min/1.73 m2) = 194 × SCr−1.094 × age−0.287 (× 0.739, if female) [28].
Statistical analysis
Overall survival (OS), progression-free survival (PFS), and cause-specific survival (CSS) rates were estimated using Kaplan–Meier analysis. The eGFR was evaluated using a paired Student’s t test. All statistical analyses were performed using SPSS software (version 26.0; IBM Corp, Armonk, NY, USA).
Results
Patient and tumor characteristics
Nineteen patients were enrolled in this study between October 2013 and March 2016. The characteristics of all patients and tumors are shown in Table 1. All patients had a single RCC. Three patients were judged inoperable by a urologist; the remaining 16 patients were operable but refused surgical therapy. Fifteen of 19 (79%) patients had the following comorbidities or medical histories: hypertension (n = 4), cancers other than RCC (stomach, colon, and prostate) and angina (n = 3), diabetes mellitus and cerebral infarction (n = 2), cerebral hemorrhage, aortic dissection, hypertrophic cardiomyopathy, arrythmia, glaucoma, Crohn disease, rheumatoid arthritis and hyperlipidemia (n = 1). Only one patient had a history of nephrectomy with contralateral renal cancer. None of the patients had hereditary RCC syndrome, such as von Hippel–Lindau disease. The histology of RCC was clear cell carcinoma in 14 patients, papillary carcinoma in 4 patients, and unclassified renal cell carcinoma in 1 patient.
TAE sessions
TAE sessions were performed under moderate sedation with local anesthesia (n = 14), epidural anesthesia (n = 3), and general anesthesia (n = 2). The amount of ethanol and lipiodol mixture used was 3.3 ± 2.0 (0.7–7.6) ml. Additional embolic materials were used in four sessions (platinum coil in 3 and platinum coil with gelatin sponge particle in 1) to prevent the injected ethanol from overflowing and flowing into non-tumor vessels. As a result, the tumor blood vessels disappeared immediately after TAE in all cases.
PCA sessions
PCA was performed under moderate sedation with local anesthesia in all cases. The interval between TAE and PCA was 4 ± 2 (median, 4; range 1–8) days. A total of 19 initial PCA sessions were performed using 3–5 cryoprobes (median, 4). Hydrodissection was performed in 17 (89%) sessions, and balloon dissection was performed in one (5%). In each case, organs such as the colon could be properly separated from the frozen area, and no organ damage was observed. No adverse events associated with these procedures were seen. PCA was performed without repositioning cryoprobes in ten (53%) sessions, while repositioning of cryoprobes followed by additional freeze-and-thaw cycles was required once in seven (37%) sessions and twice in two (10%). As no residual enhancement was demonstrated on the initial imaging evaluation in any patient, the technical success rate was 100%.
Safety
Four grade 3 hematologic adverse events occurred, while no symptomatic grade ≥ 3 events occurred (Table 2). In these four cases, the elevated test values increased to a maximum 1 day after PCA and then decreased over time. The adverse events are summarized in Table 2.
Renal function
Compared with the mean eGFR prior to PCA of 63.0 ± 16.9 ml/min/1.73 m2, the eGFR of 1 month, 3 months, 1 year, and 2 years were 59.3 ± 18.2 (p = 0.013), 59.3 ± 18.6 (p = 0.004), 57.3 ± 19.0 (p < 0.001), and 54.8 ± 18.2 ml/min/1.73 m2 (p < 0.001), respectively. None of the patients underwent hemodialysis.
Survival
The mean follow-up period was 69 ± 9 (median, 68; range 52–84) months (Table 1). During the follow-up period, two patients developed local tumor progression after the initial ablative procedure. In one case, a thin crescent-shaped residual tumor was detected at 3 months at the site in contact with the right lobe of the liver, and an additional PCA was performed. In the other case, a locally progressed tumor was detected at 46 months. Additional ablation treatment was performed using microwave ablation, considering that the tumor was in contact with the renal vein. In these two patients, no further local progression was observed at the last follow-up. No patient showed distant metastasis during follow-up. As a result, the rates of PFS and disease-free survival were the same. One patient developed de novo RCC with a different histological type in the contralateral kidney. The tumor spontaneously regressed after intratumoral hemorrhage and was thus left untreated. Another patient developed colon cancer 2 years after initial PCA. One patient died of aspiration pneumonia at 52 months, and another died of arrhythmia at 63 months. The remaining patients were alive at the last follow-up visit. Accordingly, OS, PFS, and CSS were 100%, 95%, and 100% at 3 years, and 95%, 84%, and 100% at 5 years, respectively (Fig. 1).
Discussion
Although there are many reports on ablation treatment with prior TAE, the previous reports consist of case series and retrospective studies involving varying tumor sizes and ablation modalities [20,21,22,23,24]. On the other hand, there are several studies on cryoablation for T1b RCC with a size of 4–7 cm in diameter; however, the presence or absence of TAE was mixed [2,3,4,5, 9,10,11,12,13,14]. This study was performed in histologically proven cases with a tumor size limited to 3–7 cm, always proceeded by embolization and prospectively enrolled, and was considered clinically significant. In the present study, the lower limit of the tumor diameter was set to 3 cm instead of 4 cm, which is the boundary between T1a and T1b. The AUA guideline states that clinicians should consider thermal ablation as an alternate approach for the management of cT1a solid renal masses < 3 cm in size. In addition, the NCCN guideline stated that “ablation in masses > 3 cm is associated with higher rates of local recurrence/persistence and complication”. There are reports that the threshold value with a difference in effectiveness is 2.5 cm [9] and 3 cm [29, 30]. In addition, complications such as bleeding have been reported to increase when the tumor diameter exceeds 3 cm [11,12,13]. Therefore, in the current study, tumor diameter was defined as ≥ 3 cm.
TAE for RCC has been performed since the 1970s; however, it has been mainly used to reduce bleeding volume before nephrectomy or to palliate symptoms related to advanced-stage RCC [31]. Similar to the treatment for hepatocellular carcinoma, ablation treatment is now being performed in RCC, and TAE may also serve as a useful adjunctive technique to thermal ablative therapies performed in the setting of inoperable RCC; however, the synergistic effect is still controversial [20,21,22,23]. There is also no consensus on the embolic substance, and there are reports of embolization using gelatin sponge, lipiodol, and beads; however, the embolic effect and X-ray visibility vary [20,21,22,23,24]. In this study, a mixture of ethanol and lipiodol was used as the embolic material to improve the embolic effect of microcirculation and radiopacity, and it was not difficult to inject it through a microcatheter or a microballoon catheter.
Creatine kinase elevation was probably induced, because the tumor was large, and the frozen area could have contained muscles such as the psoas major muscle. Hydrodissection is typically used to protect the bowel and ureter. Although this technique may also be used to effectively protect the psoas muscles, it is not commonly practiced [32, 33]. Although tumors ≥ 3 cm in diameter are expected to bleed more than those < 3 cm in diameter, only one case with grade 2 bleeding occurred. We assumed that the lower hemorrhagic adverse events were associated with the effect of tumor embolization, as previously reported. Post-ablation syndrome [34, 35], including full-like symptoms, is mild and infrequent for the size of the tumor. This might be because tumor treatment was divided into 2 days for embolization and freezing, and the symptoms caused by tumor necrosis with associated cytokine production might have been alleviated. These AEs after PCA with prior TAE were tolerable in all patients. Renal function showed a significant decrease after protocol treatment, which was slightly decreased and seemed to be within the acceptable range.
Local tumor progression occurred in two cases, one of which was a crescent-shaped tumor in contact with the liver, and the other was a tumor in contact with the renal vein, suggesting that PCA was inadequate. During the ablation treatment, care was taken to keep the ablation margin at least 6 mm; however, it might have been insufficient at the site in contact with the liver and renal veins. This recurrence appears to be independent of the presence or absence of embolic therapy and may not have recurred if attention was paid to the localization of the tumor and a little more to ensuring a 6 mm ablation margin. Recently, the guidelines still state that ablation treatment has a higher local recurrence rate than surgical resection [6,7,8]. Fortunately, local tumor progression in the current study could be controlled by additional treatment; however, it is important to prevent local progression by performing additional freeze and thaw cycles with cryoprobe repositioning because surgical salvage of recurrent RCC after PCA is difficult for extensive perinephric fibrosis [36].
In the current study, the estimated CSS and OS rates were 100% and 100% at 3 years, and 100% and 95% at 5 years, respectively. Our results were comparable to previously reported PCA results and LPN/OPN results at 5 years (CSS: 97–100% in T1a, 87.6–99.3% in T1b, OS: 74–98.2%, and 85–96% in T1b) [37]. These studies of PCA and surgical treatment recruited over hundreds of patients with T1 RCC. In contrast, our study included only 19 patients for 2 years; however, all were strictly followed-up for more than 2 years; 18 (95%), including one deceased patient, were followed-up for more than 5 years.
Despite strict follow-up of prospectively registered patients, our study has several limitations. First, it was a single-arm design in a single institution, and the purpose was not compared to other treatment strategies, including active surveillance and nephron-sparing surgeries. Second, a small number of patients were enrolled in the study. The protocol was designed for a short registration period, because the treatment strategy could be altered over time. Finally, the median follow-up period of 60 months might be too short to evaluate the long-term (≥ 10 years) survival of patients with T1 RCC.
In conclusion, with a lower adverse event rate, PCA with prior TAE was a safe treatment for RCCs ≥ 3 cm in diameter, and the oncologic outcomes showed promising results.
References
Global Burden of Disease Cancer Collaboration, Fitzmaurice C, Abate D et al (2019) Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 29 cancer groups, 1990 to 2017: a systematic analysis for the global burden of disease study. Jama Oncol 5:1749–1768
Georgiades CS, Rodriguez R (2014) Efficacy and safety of percutaneous cryoablation for stage 1A/B renal cell carcinoma: results of a prospective, single-arm, 5-year study. Cardiovasc Intervent Radiol 37:1494–1499
Breen DJ, King AJ, Patel N et al (2018) Image-guided cryoablation for sporadic renal cell carcinoma: three- and 5-year outcomes in 220 patients with biopsy-proven renal cell carcinoma. Radiology 289:554–561
Lim E, Kumar S, Seager M et al (2020) Outcomes of renal tumors treated by image-guided percutaneous cryoablation: immediate and 3- and 5-year outcomes at a regional center. AJR Am J Roentgenol 215:242–247
Morkos J, Porosnicu Rodriguez KA, Zhou A et al (2020) Percutaneous cryoablation for stage 1 renal cell carcinoma: outcomes from a 10-year prospective study and comparison with matched cohorts from the national cancer database. Radiology 296:452–459
Campbell SC, Clark PE, Chang SS et al (2021) Renal mass and localized renal cancer: evaluation, management, and follow-up: AUA guideline: part I. J Urol 206:199–208
Campbell SC, Uzzo RG, Karam JA et al (2021) Renal mass and localized renal cancer: evaluation, management, and follow-up: AUA guideline: part II. J Urol 206:209–218
National Comprehensive Cancer Network Kidney cancer, 4.2022 version. https://www.nccn.org/professionals/physician_gls/pdf/kidney.pdf. Accessed Jan 2022
Tanagho YS, Roytman TM, Bhayani SB et al (2012) Laparoscopic cryoablation of renal masses: single-center long-term experience. Urology 80:307–314
Dreyfuss LD, Wells SA, Best SL et al (2019) Development of a risk-stratified approach for follow-up imaging after percutaneous thermal ablation of sporadic stage one renal cell carcinoma. Urology 134:148–153
Bandi G, Hedican S, Moon T et al (2008) Comparison of postoperative pain, convalescence, and patient satisfaction after laparoscopic and percutaneous ablation of small renal masses. J Endourol 22:963–967
Hegarty NJ, Gill IS, Desai MM et al (2006) Probe-ablative nephron-sparing surgery: cryoablation versus radiofrequency ablation. Urology 68:7–13
Atwell TD, Schmit GD, Boorjian SA et al (2013) Percutaneous ablation of renal masses measuring 3.0 cm and smaller: comparative local control and complications after radiofrequency ablation and cryoablation. AJR Am J Roentgenol 200:461–466
Kakarala B, Frangakis CE, Rodriguez R et al (2016) Hemorrhagic complications of percutaneous cryoablation for renal tumors: results from a 7-year prospective study. Cardiovasc Intervent Radiol 39:1604–1610
Li QL, Guan HW, Zhang QP et al (2003) Optimal margin in nephron-sparing surgery for renal cell carcinoma 4 cm or less. Eur Urol 44:448–451
Uzzo RG, Novick AC (2001) Nephron sparing surgery for renal tumors: indications, techniques and outcomes. J Urol 166:6–18
Yan S, Xu D, Sun B (2013) Combination of radiofrequency ablation with transarterial chemoembolization for hepatocellular carcinoma: a meta-analysis. Dig Dis Sci 58:2107–2113
Jiang G, Xu X, Ren S et al (2014) Combining transarterial chemoembolization with radiofrequency ablation for hepatocellular carcinoma. Tumour Biol 35:3405–3408
Peng ZW, Zhang YJ, Chen MS et al (2013) Radiofrequency ablation with or without transcatheter arterial chemoembolization in the treatment of hepatocellular carcinoma: a prospective randomized trial. J Clin Oncol 31:426–432
Gunn AJ, Mullenbach BJ, Poundstone MM et al (2018) Transarterial embolization of renal cell carcinoma as an adjunctive therapy prior to cryoablation: a propensity score matching analysis. Diagn Interv Radiol 24:357–363
Harmon TS, Matteo J, Meyer TE et al (2018) Pre-cryoablation embolization of renal tumors: decreasing probes and saving loads. Cureus 10:e3676
Miller JM, Julien P, Wachsman A et al (2014) The role of embolization in reducing the complications of cryoablation in renal cell carcinoma. Clin Radiol 69:1045–1049
Kobe A, Tselikas L, Deschamps F et al (2022) Thermal ablation combined with selective transarterial embolization of centrally located renal cell carcinomas measuring 3 cm or larger. Cardiovasc Intervent Radiol 45:371–379
Gunn AJ, Mullenbach BJ, Poundstone MM et al (2018) Trans-arterial embolization of renal cell carcinoma prior to percutaneous ablation: technical aspects, institutional experience, and brief review of the literature. Curr Urol 12:43–49
Gervais DA, McGovern FJ, Wood BJ et al (2000) Radio-frequency ablation of renal cell carcinoma: early clinical experience. Radiology 217:665–672
Kobayashi T, Arai Y, Takeuchi Y et al (2009) Phase I/II clinical study of percutaneous vertebroplasty (PVP) as palliation for painful malignant vertebral compression fractures (PMVCF): JIVROSG-0202. Ann Oncol 20:1943–1947
Kutikov A, Uzzo RG (2009) The R.E.N.A.L. nephrometry score: a comprehensive standardized system for quantitating renal tumor size, location and depth. J Urol 182:844–853
Matsuo S, Imai E, Horio M et al (2009) Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis 53:982–992
Gervais DA, McGovern FJ, Arellano RS et al (2005) Radiofrequency ablation of renal cell carcinoma: part 1, Indications, results, and role in patient management over a 6-year period and ablation of 100 tumors. AJR Am J Roentgenol 185:64–71
Best SL, Park SK, Youssef RF et al (2012) Long-term outcomes of renal tumor radio frequency ablation stratified by tumor diameter: size matters. J Urol 187:1183–1189
Goldstein HM, Medellin H, Beydoun MT et al (1975) Transcatheter embolization of renal cell carcinoma. Am J Roentgenol Radium Ther Nucl Med 123:557–562
Bodily KD, Atwell TD, Mandrekar JN et al (2010) Hydrodisplacement in the percutaneous cryoablation of 50 renal tumors. AJR Am J Roentgenol 194:779–783
Lee SJ, Choyke LT, Locklin JK et al (2006) Use of hydrodissection to prevent nerve and muscular damage during radiofrequency ablation of kidney tumors. J Vasc Interv Radiol 17:1967–1969
Zhong J, Bambrook J, Bhambra B et al (2018) Incidence of post-ablation syndrome following image-guided percutaneous cryoablation of renal cell carcinoma: a prospective study. Cardiovasc Intervent Radiol 41:270–276
Kawabata T, Hiraki T, Iguchi T et al (2020) Post-ablation syndrome after percutaneous cryoablation of small renal tumors: a prospective study of incidence, severity, duration, and effect on lifestyle. Eur J Radiol 122:108750
Nguyen CT, Lane BR, Kaouk JH et al (2008) Surgical salvage of renal cell carcinoma recurrence after thermal ablative therapy. J Urol 180:104–109 (discussion 109)
MacLennan S, Imamura M, Lapitan MC et al (2012) Systematic review of oncological outcomes following surgical management of localised renal cancer. Eur Urol 61:972–993
Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Gobara, H., Matsui, Y., Uka, M. et al. Percutaneous cryoablation combined with prior transcatheter arterial embolization for renal cell carcinomas of 3 cm or larger: a prospective study. Int J Clin Oncol 27, 1589–1595 (2022). https://doi.org/10.1007/s10147-022-02224-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-022-02224-7