Abstract
Background
There are few studies on serum vascular endothelial growth factors and receptors (VEGF/VEGFRs) in patients with uterine cervical cancer (CC). The aim of this study was to determine whether VEGF/VEGFRs could be used as prognostic biomarkers in patients with CC.
Methods
A total of 107 patients with stage IB to IIB CC, who underwent radical hysterectomy at Tottori University Hospital between 2006 and 2015, were included in this study. Serum samples were collected prior to radical hysterectomy, and levels of VEGF-A, VEGF-C, VEGFR-1, and VEGFR-2 were analyzed by enzyme-linked immunosorbent assays. We evaluated the association between the levels of these angiogenic factors and clinicopathologic variables. Survival analysis of 93 patients treated between 2006 and 2013 was performed.
Results
The levels of VEGF-A in patients with bulky tumor, pelvic lymph-node involvement (PLNI), and parametrial infiltration (PI) were significantly higher than those in patients without these factors (P = 0.022, P = 0.020, and P = 0.0013, respectively). The overall survival (OS) of patients with high VEGF-A and VEGFR-2 defined by median levels was significantly lower than the OS of patients with low levels of VEGF-A and VEGFR-2 (P = 0.014, P = 0.012, respectively). Multivariate analysis revealed that PLNI, serum VEGF-A levels, and serum VEGFR-2 levels were independent prognostic factors for OS (hazard ratio for VEGF-A 3.42, 95% CI 1.07–13.2; hazard ratio for VEGFR-2 6.37, 95% CI 1.59–43.5).
Conclusion
Our results suggest that serum VEGF-A and VEGFR-2 may be promising prognostic biomarkers for CC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cervical cancer is a common gynecological cancer, with 527,600 newly diagnosed cases and the cause of 265,700 deaths worldwide in 2012 [1]. Cytologic screening have decreased the morbidity of cervical cancer in developed countries, and DNA testing for high-risk human papillomavirus (HPV) would accelerate detection of precancerous lesions. However, it remains a considerable issue for women who do not have access to an effective screening program. Although early stage and locally advanced cervical cancer might be cured with radical hysterectomy or chemoradiotherapy, patients with metastatic lesions and those with persistent or recurrent disease have limited options.
HPVs are small double-stranded DNA viruses that have been strongly linked to the etiology of cervical cancer [2]. In addition to cell proliferation and suppression of apoptosis, the HPV E6 oncoprotein contributes to tumor angiogenesis by direct stimulation of the vascular endothelial growth factor (VEGF) gene [3].
Angiogenesis is one of the processes that are critical for the growth, invasion, and metastasis of solid tumors, including cervical cancer [4, 5]. VEGF and its receptors is one of the major pathways involved in tumor angiogenesis. The VEGF family comprises in mammals five members: VEGF-A, placenta growth factor, VEGF-B, VEGF-C, and VEGF-D [6]. VEGF ligands, on binding to their three primary receptors and two co-receptors, initiate signal transduction. VEGF-A binds to both vascular endothelial growth factor receptor-1 (VEGFR-1), also known as Flt-1, and VEGFR-2, known as Flk-1, involved in tumor invasion and migration. VEGFR-1 is primary involved in development and is not seen as critical in tumor angiogenesis. VEGFR-3, which binds VEGF-C and VEGF-D, is innate to lymphatic endothelial cells and plays a role in lymph-node metastasis [7]. VEGFR-1 and VEGFR-2 are principally expressed on blood vascular endothelium, whereas VEGFR-3 is expressed on lymphatic endothelium [8].
Recently, various molecular targeted agents have been developed and used in the treatment of a variety of malignancies. Bevacizumab, a recombinant humanized monoclonal antibody that targets VEGF-A, shows clinical benefit in patients with colon, lung, breast, and ovarian cancer [4]. The Gynecologic Oncology Group (GOG) 240 study demonstrated a significant improvement in progression-free survival (PFS) and overall survival (OS) with the addition of bevacizumab to chemotherapy in patients with recurrent, persistent, or advanced stage primary cervical cancer [9]. Although VEGF can be targeted in the treatment of cervical cancer, a biomarker that predicts the sensitivity of the tumor has not yet been identified.
Several studies indicated that VEGF overexpression in tumor tissue samples can be a diagnostic or predictive biomarker for cervical cancer [10, 11], but there are few studies on serum VEGF in patients with cervical cancer. The advantages of a serum biomarker are as follows. First, samples can be collected non-invasively from patients, and second, physicians can monitor changes in tumor biology by repeating the test throughout treatment. Therefore, we conducted the present study to explore the utility of serum VEGFs and receptors (VEGF/VEGFRs) and to evaluate their utility as prognostic biomarkers of cervical cancer.
Materials and methods
Patients and sample collection
A total of 107 patients with International Federation of Gynecology and Obstetrics (FIGO) stage IB to IIB cervical cancer, who underwent radical hysterectomy at Tottori University Hospital between 2006 and 2015, were enrolled in this study. Patients with bulky tumor (> 40 mm) or having stage IIB disease received neoadjuvant chemotherapy (NAC) consisting of platinum- and taxane-based regimens. Adjuvant concurrent chemoradiotherapy or radiotherapy was given in cases with pelvic lymph-node involvement (PLNI) or parametrial infiltration (PI). The survival of 93 patients treated between 2006 and 2013, with median follow-up duration of 1743 days, was analyzed. The study was approved by the Institutional Review Board of Tottori University Hospital. All patients gave written informed consent before the collection of specimens according to the institutional guidelines.
Blood samples for analysis of VEGF/VEGFRs were collected prior to radical hysterectomy. The sample of patients who received NAC was collected just before NAC. Samples were left to coagulate for 30–60 min, followed by centrifugation. The serum samples were aliquoted and immediately stored at − 80 °C. Tumor samples were collected from non-necrotic cancer tissue during the surgery, rinsed with phosphate-buffered saline, and stored at − 80 °C prior to analysis.
Enzyme-linked immunosorbent assays (ELISA)
Serum VEGF-A, -C, VEGFR-1, and VEGFR-2 concentrations were measured with the Quantikine Human VEGF-A, -C, VEGFR-1 and VEGFR-2 kits (R&D Systems, Minneapolis, MN, USA). Serum samples were diluted fivefold for VEGF-C determinations. Working standards were prepared according to the manufacturer's instructions. A total of 100 μL of Assay Diluent RD1W was added into a 96-well plate coated with a monoclonal antibody against an individual growth factor or soluble receptor. Serum samples, standards, and controls were dispensed in duplicate and incubated for 120 min at room temperature. The plate was washed three times in wash buffer. A volume of 200 μL of a VEGF/VEGFR conjugate was added to each well and incubated for 120 min. Washings were repeated. A volume of 200 μL of substrate solution provided with the kit was added in the dark, and the reaction was stopped after 30 min of incubation. Bound VEGF/VEGFRs were detected by measuring the absorbance at 450 nm in a photometer and the concentration was determined from the standard curve. All samples were examined in triplicate and the mean values were used for statistical analysis.
Real-time reverse transcriptase-polymerase chain reaction (RT-PCR)
Messenger RNA (mRNA) expression of VEGF-A was determined with real-time RT-PCR. Total RNA was isolated from frozen tissue using the RNeasy Mini Plus Kit (Qiagen, Hilden, Germany) according to the manufacturer’s instructions. Complementary DNA was synthesized from the isolated RNA by RT with the High Capacity cDNA Reverse Transcription Kit (Applied Biosystems, Foster City, CA, USA). Quantitative real-time PCR was performed using TaqMan probes for the target genes and for the endogenous control gene (VEGF-A, Hs00900054_ml and GAPDH, Hs99 999905_ml) as previously described [12].
The calculations for determining the relative level of gene expression were performed using the cycle threshold (Ct) method. The mean Ct values from triplicate measurements were used to calculate the relative expression of VEGF-A with normalization to GAPDH using the 2−ΔΔCt method. We calculated ΔΔCt using the maximum ΔCt value among all samples as positive control.
Immunohistochemistry
A part of each sample was fixed with 10% formalin and embedded in paraffin. For routine histologic studies, 3-μm-thick sections were stained with hematoxylin and eosin. After the sections were deparaffinized and endogenous peroxidase activity was blocked, they were pretreated with citrate buffer (0.01 M, pH 6.0) in a water bath for 40 min at 100 °C. Thereafter, the sections were incubated at 4 °C overnight with a rabbit polyclonal antibody against VEGF-A (clone A-20; diluted 1:100, Santa Cruz Biotechnology, Santa Cruz, CA, USA). To detect binding of the primary antibody, the sections were incubated with EnVision + Dual Link System-HRP Rabbit/Mouse (Dako, Glostrup, Denmark) for 30 min and then with 3,3′-diaminobenzidine (DAB) solution (liquid DAB + substrate, imidazole–HCL, Dako) for 5 min. Finally, the sections were counterstained with hematoxylin. For the negative control, the primary antibodies were replaced with phosphate-buffered saline. We used a section of colon cancer tissue as the positive control of VEGF-A.
To evaluate the staining of cancer cells, a semi-quantitative scoring method called the immunoreactive score (IRS) was performed according to Remmele and Stegner [13]. The IRS is obtained by the product of intensity of immunostaining (none = 0; weak = 1; moderate = 2; strong = 3) and percentage of positive tumor cells (none = 0; 1–10% = 1; 11–50% = 2; 51–80% = 3; > 80% = 4).
Statistical analysis
All statistical analyses were performed with Prism version 5 (GraphPad Software Inc., San Diego, CA, USA) and JMP version 11 program (SAS Institute Inc., Cary, NC, USA). Because the Shapiro–Wilk test for normality indicated that serum concentrations of VEGF/VEGFRs were not normally distributed, the Mann–Whitney U test was applied to investigate the significance of differences in VEGF/VEGFRs according to each clinicopathologic variable. Patient survival distribution was calculated using the Kaplan–Meier method. The significance of the survival distribution in each group was tested by the log-rank test. Multivariate analysis was performed to fit a Cox proportional hazards model. A P value of < 0.05 was considered statistically significant.
Results
One hundred and seven patients with International Federation of Gynecology and Obstetrics (FIGO) stage IB to IIB cervical cancer were enrolled in our study. They underwent radical hysterectomy at Tottori University Hospital between 2006 and 2015.
The clinical characteristics of the patients are summarized in Table 1. The median age at the initial diagnosis was 46 years (range 27–69 years). According to FIGO staging, there were 62 patients (57.9%) with stage IB1 cancer, 16 patients (14.9%) with stage IB2, nine patients (8.4%) with stage IIA, and 20 patients (18.6%) with stage IIB cancer. Thirty-five patients (32.7%) had bulky tumor (tumor size > 40 mm). Twenty-three patients (21.4%) had PLNI, and 16 patients (15%) had PI. Patients with bulky tumor or PI received neoadjuvant chemotherapy.
Median levels of serum VEGF-A, VEGF-C, VEGFR-1, and VEGFR-2 were 313 (43–1227), 8122 (43–1227), 68 (0–132.6), and 6210 (3684–10,227) pg/mL, respectively. The levels of VEGF-A in patients with bulky tumor, PLNI, and PI were significantly higher than the levels in patients without these factors. There was no correlation between the level of serum VEGF-C and clinicopathological features. The level of serum VEGFR-2 in patients with PLNI was significantly higher than the level in patients without PLNI. On the other hand, the level of serum VEGFR-1 in patients with either bulky tumor or PLNI was significantly lower than the level in patients without the corresponding factor (Table 2). There was no correlation between patient age and the levels of serum VEGF/VEGFRs. We examined the association between clinicopathological factors and prognosis. Tumor stage, histological type, and tumor size were not prognostic factors of cervical cancer. Patients with PLNI and PI had a significantly poor prognosis (Table 3).
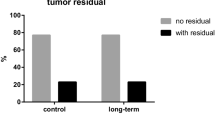
For survival analysis, we set the cut-off value of VEGF/VEGFRs at the median level according to the previous study [13]. The estimated 5-year OS rate of patients with high VEGF-A levels (higher than the median level) was 72.8% and the rate of those with low VEGF-A levels was 92.9%. The estimated 5-year OS rate of patients with high VEGFR-2 levels was 73.8% and the rate of those with low VEGFR-2 levels was 94.7%. The OS of patients with high VEGF-A and VEGFR-2 levels was significantly lower than the OS of patients with low levels (Table 3, Fig. 1a). Twenty-eight of 93 patients who had PLNI or PI received adjuvant radiotherapy. Pretreatment serum VEGF/VEGFRs values did not affect OS for these patients.
a Overall survival of patients with high VEGF-A levels was significantly lower than those with low levels, and the overall survival of patients with high VEGFR-2 levels was significantly lower than those with high levels. However, there were no significant relationships between overall survival and VEGF-C or VEGFR-1. b Immunohistochemistry revealed that the VEGF-A protein was expressed mainly in cancer cells. Representative sections of FIGO stage IB1, squamous cell carcinoma scored as IRS: 12 (×40)
Multivariate analysis revealed that PLNI, serum VEGF-A levels, and serum VEGFR-2 levels were independent prognostic factors for OS [hazard ratio (HR) for VEGF-A 3.42, 95% CI 1.07–13.2, P = 0.038; HR for VEGFR-2 6.37, 95% CI 1.59–43.5, P = 0.007, Table 3).
We examined mRNA expression of VEGF-A in tumor tissue for comparison with serum VEGF-A levels. Total RNA of sufficient quality and quantity for real-time RT-PCR could be obtained from fresh frozen tissue samples in 39 out of 107 cases. Therefore, we also examined these 39 cases for the immunohistochemical expression of VEGF-A. There was no significant correlation between mRNA or protein expression and serum levels of VEGF-A. The mRNA or protein expression levels were not related to any clinicopathologic variables in this cohort (Table 4, Fig. 1b).
Discussion
In the present study, we investigated the serum concentrations of VEGF-A, VEGF-C, VEGFR-1, and VEGFR-2 in patients with stage IB1 to IIB cervical cancer. There are few reports, indicating that serum VEGF-A remains an independent prognostic factor for cervical cancer after using multiple VEGF/VEGFRs concomitantly detected in serum samples as explanatory variables in multivariate analysis. Our results demonstrated that VEGF-A was higher in patients with bulky tumor, PLNI, or PI than in patients without these factors that both VEGF-A and VEGFR-2 predict significantly worse OS and that serum VEGF-A and VEGFR-2 are independent prognostic factors in patients with cervical cancer in terms of OS.
Zusterzeel et al. examined serum VEGF-A in 167 patients with stage IB to IV cervical cancer. In their report, serum VEGF-A was significantly higher in patients with advanced tumor stage, large tumor size (greater than 2 cm in diameter), and vascular space invasion. In addition, serum VEGF-A was associated with OS and retained its prognostic value for OS in multivariate analysis (HR 1.92, 95% CI 1.01–3.64, P = 0.04). They concluded that serum VEGF-A levels correlated with more advanced and more aggressive cervical cancer and it might be a useful prognostic factor in these patients [14]. The present study showed that serum VEGF-A was an independent prognostic factor for OS (HR 3.42, 95% CI 1.07–13.2, P = 0.038), which is congruent with the result reported by Zusterzeel et al. [15].
The association of clinicopathologic factors with serum VEGF-A or C in the previous reports has not been consistently demonstrated [14, 15]. Lebrecht's study included 38 patients with stage Ia to IIa who underwent radical hysterectomy and 46 patients with stage IIb to IV who underwent primary irradiation [15]. Mitsuhashi et al. examined serum VEGF-A and VEGF-C in 78 patients with cervical cancer. They reported that serum levels of VEGF-A and VEGF-C significantly correlated with FIGO stage and tumor size, but not with PLNI. Pretherapeutic levels of VEGF-C also significant correlated with disease recurrence or persistence after treatment [16]. The present study showed that serum VEGF-C did not correlate with stage, tumor size, PLNI, or PI. Our study focused on stage IB to IIB patients who underwent radical hysterectomy. In other words, we did not examine patients with advanced stage. This may explain why serum VEGF/VEGFRs did not correlate with tumor stage unlike other studies. On the other hand, Zusterzeel, Lebrecht, and Mitsuhashi paper included patients with stage III/IV who underwent definitive chemoradiotherapy, which means lymph-node status was pathologically unknown in considerable numbers of their patients. This may explain why serum VEGF-A or C did not correlate with lymph-node involvement unlike our study.
There have been few reports on serum levels of VEGFRs in patients with cervical cancer. Braicu et al. analyzed the expression profile of matrix metalloproteinases, cell adhesion molecules, and the VEGF family in patients with high-risk stage Ib to IIb cervical cancer. They demonstrated that serum VEGFR-1 levels of higher than 100 pg/mL and tissue inhibitor of metalloproteinases 2 (TIMP2) levels of lower than 90 ng/mL were significantly associated with poor OS and PFS in univariate analysis. In multivariate analysis, serum TIMP2 expression was the only independent prognostic factor for OS [17]. Although the exact role of VEGFR-1 in angiogenesis is unclear, VEGFR-2 has a predominant role in VEGF-induced angiogenic and vascular permeability effects. Indeed, several studies have indicated that VEGFR-2 is associated with OS in patients with ovarian cancer [12, 18]. Therefore, we examined the serum levels of both VEGFR-1 and VEGFR-2. The present data showed that a low level of VEGFR-2 was significantly associated with better OS and that VEGFR-2 was an independent prognostic factor for OS by multivariate analysis.
Based on the results of the GOG 240 study, the combination of bevacizumab with chemotherapy has become the standard treatment for advanced or recurrent cervical cancer. However, a biomarker that predicts the sensitivity of the tumor to bevacizumab has not yet been identified in patients with cervical cancer. Besides the well-known adverse events of bevacizumab (e.g., thrombosis and gastrointestinal perforation), vaginal fistula is characteristic and an irreversible adverse event in patients with cervical cancer, especially after radiotherapy [9]. Thus, it is important to select patients who would benefit from bevacizumab from the perspective of the economy and patient quality of life.
Regarding VEGF/VEGFRs in blood samples, predictive value of baseline plasma VEGF-A levels in patients with gastric cancer and non-small-cell lung cancer was reported [19, 20]. Because the present study did not include patients treated with bevacizumab, we could not know whether serum VEGF-A and VEGFR-2 are predictive biomarkers for the efficacy of bevacizumab. The sample size and study design are also limitations of our study. A larger sample size and a prospective design may provide more reliable or conclusive evidence.
We showed that both a high level of serum VEGF-A and serum VEGFR-2 predict significantly worse OS and that these are independent prognostic factors for OS in patients with early stage invasive cervical cancer. These results imply that serum VEGF-A and serum VEGFR-2 are potential prognostic biomarkers for cervical cancer. Further studies to validate the data and to determine an appropriate cut-off value are needed. In addition, the hypothesis that serum VEGF-A and serum VEGFR-2 are predictive biomarkers for bevacizumab should be tested by collecting samples from patients treated with the agent.
References
Global Cancer Facts & Figure 3rd edition. https://www.cancer.org/acs/groups/content/@research/documents/document/acspc-044738.pdf. Accessed 22 June 2019
Bosch FX, Lorincz A, Munoz N et al (2002) The causal relation between human papilloma virus and cervical cancer. J Clin Pathol 5:244–265
Lopez-Ocejo O, Viloria-Petit A, Bequet-Romero M et al (2000) Oncogenes and tumor angiogenesis: the HPV-16 E6 oncoprotein activates the vascular endothelial growth factor (VEGF) gene promoter in a p53-independent manner. Oncogene 19:4611–4620
Ellis LM, Hicklin DJ (2008) VEGF-targeted therapy: mechanisms of antitumor activity. Nat Rev Cancer 8:579–591
Folkman J, Watson K, Ingber D et al (1989) Induction of angiogenesis during the transition from hyperplasia to neoplasia. Nature 339:58–61
Lohela M, Bry M, Tammela T et al (2009) VEGFs and receptors involved in angiogenesis versus lymphangiogenesis. Curr Opin Cell Biol 21:154–165
Hicklin DJ (2005) Role of the vascular endothelial growth factor pathway in tumor growth and angiogenesis. J Clin Oncol 23(5):1011–1027
Veikkola T, Karkkainen M (2000) Regulation of angiogenesis via vascular endthelial growth factor receptors. Cancer Res 60:203–212
Tewari S, Sill MW, Long HJ et al (2014) Improved survival with bevacizumab in advanced cervical cancer. N Engl J Med 370:734–743
Lee IJ, Park KR, Lee KK et al (2002) Prognostic value of vascular endothelial growth factor in stage IB carcinoma of the uterine cervix. Int J Radiat Oncol Biol Phys 54:768–779
Tjalma W, Weyler J, Weyn B et al (2000) The association between vascular endothelial growth factor, microvessel density and clinicopathological features in invasive cervical cancer. Eur J Obstet Gynecol Reprod Biol 92:251–257
Komatsu H, Oishi T, Itamochi H et al (2017) Serum vascular endothelial growth factor-A as a prognostic biomarker for epithelial ovarian cancer. Int J Gynecol Cancer 27(7):1325–1332
Remmele W, Stegner HE (1987) Vorschlag zur einheitlichen Definition eines Immunreaktiven Score (IRS) für den immunhistochemischen Östrogenrezeptor-Nachweis (ER-ICA) im Mammakarzinomgewebe. Pathologe 8:138–140
Zusterzeel PL, Span PN, Dijksterhuis MG et al (2009) Serum vascular endothelial growth factor: a prognostic factor in cervical cancer. J Cancer Res Clin Oncol 135:283–290
Lebrecht A, Ludwig E, Huber A (2002) Serum vascular endthelial growth factor and serum leptin in patients with cervical cancer. Gynecol Oncol 85:32–35
Mitsuhashi A, Suzuka K, Yamazawa K et al (2005) Serum vascular endothelial growth factor (VEGF) and VEGF-C levels as tumor markers in patients with cervical carcinoma. Cancer 103:724–730
Braicu EI, Fotopoulou C, Chekerov R et al (2013) Role of serum concentration of VEGFR1 and TIMP2 on clinical outcome in primary cervical cancer: results of a companion protocol of the rando, ized, NOGGO-AGO phase III adjuvant trial of simultaneous cisplatin-based radiochemotherapy vs. carboplatin and paclitaxel containing sequential radiotherapy. Cytokine 61:755–758
Sallinen H, Heikura T, Koponen J et al (2014) Serum angiopoietin-2 and soluble VEGFR-2 levels predict malignancy of ovarian neoplasm and poor prognosis in epithelial ovarian cancer. BMC Cancer 14:696
Van Cutsem E, de Haas S, Kang YK et al (2012) Bevacizumab in combination with chemotherapy as first-line therapy in advanced gastric cancer: a biomarker evaluation from the AVAGAST randomized phase III trial. J Clin Oncol 30(17):2119–2127
Mok T, Gorbunova V, Juhasz E et al (2014) A correlative biomarker analysis of the combination of bevacizumab and carboplatin-based chemotherapy for advanced nonsquamous non-small-cell lung cancer: results of the phase II randomized ABIGAIL study (BO21015). J Thorac Oncol 9(6):848–855
Acknowledgements
We thank Dr. Eiji Nanba and Ms. Kaori Adachi of the Division of Functional Genomics, Research Center for Bioscience and Technology at Tottori University for assisting with real-time RT-PCR.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Sawada, M., Oishi, T., Komatsu, H. et al. Serum vascular endothelial growth factor A and vascular endothelial growth factor receptor 2 as prognostic biomarkers for uterine cervical cancer. Int J Clin Oncol 24, 1612–1619 (2019). https://doi.org/10.1007/s10147-019-01495-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-019-01495-x