Abstract
Background
Colorectal cancer is common, and its incidence is increasing throughout the world. The liver is a major metastatic site, and colorectal liver metastasis (CRLM) has a poor prognosis. Although liver resection is the most effective therapy for CRLM, postoperative recurrence is common. Thus, prognostic markers for CRLM are greatly needed. D-dimer, a fibrin cleavage product, has been shown to be related to colorectal tumor progression, and is also associated with malignant progression and recurrence in various cancers. Therefore, we evaluated the value of D-dimer in predicting the prognosis in CRLM.
Methods
We retrospectively evaluated 90 cases of resected CRLM to determine the correlation between D-dimer and patient survival. The cut-off value for D-dimer levels was determined using receiver operating characteristic curve analysis.
Results
Significant differences occurred in the recurrence group with higher D-dimer levels (P = 0.00736*), while the optimal cut-off value was 0.6 µg/mL. High D-dimer levels (≥ 0.6 µg/mL) were associated with poor recurrence-free survival (RFS; P = 0.0000841*) and cancer-specific survival (CSS; P = 0.00615*). In the multivariate analysis, D-dimer correlated with CRLM prognosis and independently predicted RFS (P = 0.0179*).
Conclusion
High D-dimer levels were associated with poor RFS and CSS. D-dimer was an independent prognostic factor of RFS. Therefore, D-dimer may help predict recurrence and prognosis in patients with CRLM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer is common and its incidence is increasing [1]. Fifty percent of all patients with colorectal cancer develop metastasis, and colorectal liver metastasis (CRLM) is the most frequent [2]. Liver resection is the most effective therapy for CRLM, and the 5-year survival rate is as high as 50% [3]. However, postoperative recurrence is common and remains an important issue to be addressed. Previously, several prognostic factors of recurrence were reported including carcinoembryonic antigen (CEA), metastatic number, tumor size or lymph node metastasis [4, 5]. In these previous reports, prognostic models have been described based on calculus while using these prognostic factors; however, these models have not been broadly adopted in the clinical settings. Therefore, to improve patient prognosis, we must identify simple prognostic markers in CRLM.
D-dimer, a fibrin cleavage product, is a clinically important marker used to diagnose pulmonary thromboembolism [6]. Recently, D-dimer levels were reported to be strongly related to various types of colorectal cancers [7, 8]. In addition, D-dimer levels show correlation with tumor progression, recurrence, and prognosis in other cancers (lung cancer [9, 10], prostate cancer [11], and gastric cancer [12]). However, there have been no reports evaluating the correlation between D-dimer levels and CRLM recurrence.
Therefore, we aimed to evaluate D-dimer levels in patients with CRLM to predict the prognosis of CRLM, following liver resection. We also evaluated the association between D-dimer levels and recurrence, clinicopathological factors, inflammatory factors, and patient survival in CRLM.
Materials and methods
Patients and samples
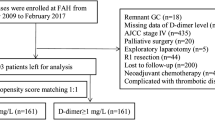
We retrospectively evaluated 90 consecutive patients with liver metastasis of colorectal cancer who underwent curative liver resection at our department from 2006 to 2017. The patients were aged 38–83 years. The various blood examinations (including D-dimer) were measured before a month of operation. The surgical techniques applied were partial resection (46 cases), subsegmentectomy (14 cases), segmentectomy (17 cases), and lobectomy (13 cases). The locations of the primary cancer were, the cecum (6 cases), ascending colon (6 cases), transverse colon (4 cases), descending colon (4 cases), sigmoid colon (14 cases), and rectum (26 cases). Tumor staging was performed based on the criteria of the Union for International Cancer Control tumor-node-metastasis staging system (seventh edition). The recurrence was observed in 51 cases, and the location of the metastasis were, liver (19 cases), lung (22 cases), peritoneum (4 cases), lymph node (12 cases), colon local site (2 case), and others [brain (2 cases), bone (2 cases), abdominal wall (1 case), pleura (1 case)]. The adjuvant chemotherapy was performed to 69 cases as follows: FOLFOX (5 cases), bevacizumab plus FOLFOX (1 cases), Capecitabine (9 cases), XELOX (18 cases), bevacizumab plus XELOX (3 cases), FOLFIRI (3 cases), cetuximab plus FOLFIRI (2 cases), bevacizumab plus SOX (1 case), TS-1 (4 cases), UFT (8 cases), UFT/UZEL (6 cases) and 5-FU/LV (1 case). All patients provided written informed consent for the treatment and data analyses, while the study design was approved by our Clinical Ethics Committee (http://ciru.dept.showa.gunma-u.ac.jp/guidance/storage-sample/list.html).
Statistical analysis
All statistical analyses were performed with EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan), which is a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria) [13]. Level of significance was evaluated by performing Student’s t test, analysis of variance, Mann–Whitney U test, and by determining the Pearson’s correlation coefficient. Survival curves were created by applying the Kaplan–Meier method and analyzed by performing the log-rank test. Prognostic factors were examined in univariate and multivariate analyses, using a Cox proportional hazards model. The cut-off value for D-dimer was evaluated using the receiver operating characteristic (ROC) curve analysis. Differences were considered significant at P < 0.05.
Results
D-dimer levels by postoperative recurrence groups
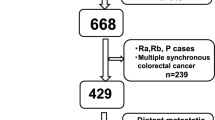
The average preoperative D-dimer level was 1.21 µg/mL (range 0–9.3 µg/mL). Compared to the no-recurrence group, the recurrence group had significantly higher D-dimer levels (P = 0.00736*; Fig. 1a). Other coagulation markers (FDP, platelet counts, PT and APTT) had no correlation to recurrence. The optimal cut-off value for D-dimer levels was 0.6 µg/mL [area under the curve (AUC) 0.664, sensitivity 0.683, specificity 0.714; Fig. 1b]. This cut-off value was used for the following analyses. Two typical cases (one is a low D-dimer case and the other is a high D-dimer case) are shown in the Supplementary Figure.
Significant difference occurred in the recurrence group with higher D-dimer levels than in the no-recurrence group (P = 0.00736; a). The optimal cut-off value for D-dimer levels (0.6 µg/mL) was determined using the receiver operating characteristic curve analysis [area under the curve (AUC) 0.664, sensitivity 0.683, specificity 0.714; b]
Clinicopathological factors by D-dimer groups
The significant differences in various clinicopathological factors with D-dimer levels are shown in Table 1. Significant differences occurred in various clinicopathological factors with the high D-dimer group (≥ 0.6 µg/mL) including CEA (P = 0.0027*) and synchronous metastasis (P = 0.022*). A borderline significant difference was also found in primary tumor location (left-sided colon) with the high D-dimer group (P = 0.0655). In contrast, liver metastasis factor, tumor size, tumor number and venous thrombosis (VTE) showed no significant differences by D-dimer levels. Moreover, no significant differences were also observed according to D-dimer levels in inflammatory factors, the neutrophil/lymphocyte ratio (NLR), and modified Glasgow Prognostic Score (mGPS). In addition, D-dimer had negative correlations with albumin (R2 − 0.434, P = 0.0000294*; Fig. 2a) and size of liver metastases (R2 0.217, P = 0.0401*; Fig. 2b).
Associations between D-dimer levels and postoperative recurrence and prognosis
The ability of D-dimer levels to predict postoperative recurrence-free survival (RFS) and cancer-specific survival (CSS) is shown in Fig. 3. Compared to the low D-dimer group, the high D-dimer group showed poorer RFS (P = 0.0000841*; Fig. 3a) and poorer CSS (P = 0.00615*; Fig. 3b). D-dimer levels exhibited a stronger correlation with RFS (Table 2) and CSS (Table 3) after liver resection for CRLM. D-dimer predicted recurrence in the univariate and multivariate analyses [hazard ratio (HR) 3.08, 95% confidence interval (CI) 1.52–6.67, P = 0.00179*; Table 2]. Furthermore, as shown in Table 2, D-dimer provided greater predictive value than CEA (HR 1.81, 95% CI 0.934–3.51, P = 0.0784), primary T factor (HR 1.83, 95% CI 0.999–3.39, P = 0.0539), and adjuvant therapy (HR 0.400, 95% CI 0.195–0.822, P = 0.0127*). In Table 3, D-dimer shows correlation with CSS in the univariate analysis and tends to relate with CSS in the multivariate analysis (HR 2.51, 95% CI 0.879–7.15, P = 0.0857*; Table 3).
Relationship between postoperative survival and D-dimer levels. Kaplan–Meier curves for the low and high D-dimer groups are shown. a High D-dimer levels were associated with poor recurrence-free survival (RFS; P = 0.0000841) and b high D-dimer levels were also associated with poor cancer-specific survival (CSS; P = 0.00615)
Associations between D-dimer levels and adjuvant chemotherapy on postoperative recurrence and prognosis
The correlation between postoperative prognosis and adjuvant chemotherapy was also analyzed. The adjuvant chemotherapy group showed improvement in RFS (P = 0.00203*; Fig. 4a) but had no correlation to CSS (P = 0.318; Fig. 4b). Moreover, in the D-dimer low group (less than 0.6 µg/mL), adjuvant chemotherapy led to improvement in DFS (P = 0.018*; Fig. 4c) and did not relate to CSS (P = 0.249; Fig. 4d). In the D-dimer high group (above 0.6 µg/mL), adjuvant therapy had no correlation to both DFS (P = 0.0618; Fig. 4e) and CSS (P = 0.857; Fig. 4f).
Relationship between postoperative survival and adjuvant chemotherapy. Adjuvant chemotherapy group showed improvement in RFS (P = 0.00203*; a) but had no correlation to CSS (P = 0.318; b). In addition, Kaplan–Meier curves for adjuvant chemotherapy are shown in each D-dimer low group (less than 0.6 µg/mL) and D-dimer high group (above 0.6 µg/mL). In the D-dimer low group, adjuvant chemotherapy was associated with improving poor recurrence-free survival (RFS; P = 0.018; c) but was not associated with cancer-specific survival (CSS; P = 0.249; d). In the D-dimer high group, adjuvant chemotherapy was not associated with RFS (P = 0.0618; e) and CSS (P = 0.857; f)
Discussion
In the present study, we showed that high D-dimer levels (≥ 0.6 µg/mL) were associated with postoperative recurrence after hepatic resection for CRLM. Thus, D-dimer levels might be a clinically useful prognostic marker for CRLM.
Zacharski et al. reported that cancer cells promote coagulation by inactivating the fibrinolytic system (e.g., via urokinase-type plasminogen activator); and different carcinoma types may promote coagulation via numerous mechanisms [14]. Gene et al. also reported that breast and prostate cancers were associated with elevated levels of coagulation factors (e.g., vascular endothelial growth factor, interleukin-6, soluble P-selectin, fibrinogen, and D-dimer) [15]. Thus, cancer cells appear to activate coagulation. Moreover, Mytnik et al. reported that colorectal cancer activates several coagulation factors, including plasminogen activator inhibitor-1, prothrombin fragments, and protein C [16]. The correlation between colorectal cancer and D-dimer was first reported by Edwards et al. in 1993 [17], and the initial finding was supported by the findings of subsequent studies. In colorectal cancer, D-dimer was shown to be a prognostic factor after the resection of the primary lesion [7, 18,19,20,21], and an indicator of therapeutic effect of chemotherapy [22].
In previous studies, several prognostic factors of CRLM were reported, including metastatic number, differentiation, resected margin, and the tumor marker, CEA [1, 2]. Moreover, several studies have proposed the use of calculus or nomogram to determine prognosis based on the above risk factors [4, 5, 23]. However, the relationship between D-dimer and CRLM had not been reported previously. In the present study, high D-dimer level correlated with poorer RFS and CSS among patients with CRLM and was an independent prognostic factor of RFS in multivariate analysis. In addition, D-dimer level was a more significant predictor than CEA, primary T factor, or adjuvant therapy. Blackwell et al. also reported that D-dimer reflected the prognosis of metastatic colorectal carcinoma more than CEA [20]. Therefore, D-dimer levels could conveniently predict the prognosis in CRLM.
Nevertheless, its mechanism is still unclear. Recent reports have shown high D-dimer levels are related to poor prognosis, probably based on chemoresistance in various cancers, and/or circulating tumor cells (CTC). Inanc M et al. reported D-dimer was a marker of chemosensitivity [24] and Zhu L et al. reported high D-dimer correlates to poor prognosis when treated with bevacizumab [25]. Tomimaru Y et al. proved D-dimer could be used as a predictor for neoadjuvant chemosensitivity in esophageal cancer by evaluating pathological response [26]. In our study, low D-dimer cases were shown to improve DFS by adjuvant chemotherapy, but high D-dimer cases had no correlation prognosis and adjuvant chemotherapy. Tissue factors play a role in chemoresistance thorough hypercoagulopathy state, and a high level of VEGF was also predictive of chemoresistance on breast cancer [27]. From these things, D-dimer reflected hypercoagulopathy state on cancer patient and as a result, high D-dimer level lead to chemoresistance.
Among the clinicopathological factors examined, significant differences occurred with D-dimer in CEA (P = 0.0027*) and synchronous metastasis; therefore, D-dimer levels may reflect cancer progression. CEA has been reported in several studies as a prognostic factor in colorectal cancer, and found to be correlated with CRLM prognosis [28, 29]. Recently, right-sided colon cancer was reported to have a poor prognosis [30] and different molecular biological background (KRAS/BRAF mutation, and p53) compared with left-sided cancer [31]. In this study, right-sided cancer in the primary anatomical site showed tendency to have difference with high D-dimer level (P = 0.0655).
The circulating tumor cells (CTCs) are proved to relate to tumor progression and prognosis in various cancers. Recently, it is reported CTCs had relation to hypercoagulability and D-dimer could be excellent predicator [11, 32]. In colorectal cancer, CTC positive cases had poor prognosis after liver resection to CRLM [33, 34]. In our study, D-dimer may indicate poor prognosis or hypercoagulability as a consequence of reflecting CTCs behavior.
This study has several limitations. Because it is a retrospective study, we could not evaluate D-dimer level on postoperative state. In addition, it is unclear how tumor progression is mechanistically related to D-dimer levels. Therefore, further prospective studies are needed to evaluate the underlying mechanism.
Recently, the antitumor effect of anticoagulant was reported in an investigation aimed at determining the correlation between cancer and hypercoagulability [35]. In addition, Klerk et al. reported that low molecular weight heparin increased survival time for solid tumor patients [36]. In small cell lung cancer, the combination of chemotherapy and heparin led to improved antitumor effect [37]. Moreover, according to Rothwell et al., long-term administration of aspirin reduced the risk of colorectal cancer development [38]. These findings, regarding coagulation and cancer, indicate coagulative factors as promising therapeutic targets and D-dimer as a predictive marker of therapeutic response in cancer.
Although liver resection greatly improves the prognosis of CRLM, it is of importance to prevent recurrence after resection. Therefore, we sought to find clinically useful factors for predicting recurrence after the resection of CRLM. Moreover, our data showed D-dimer high cases did not have enough effect of adjuvant chemotherapy as compared to D-dimer low groups. The anticoagulant therapy may be new target instead of chemotherapy for high D-dimer cases.
In conclusion, our study provides the first evidence that D-dimer may be a novel biomarker of prognosis in CRLM in various aspects. We showed that high D-dimer level was associated with poor RFS and CSS in patients with CRLM. Therefore, D-dimer may be a useful biomarker of recurrence and prognosis in CRLM. Our findings also indicate that coagulation factors may be promising targets for controlling cancer progression.
Abbreviations
- CRLM:
-
Colorectal liver metastasis
- CEA:
-
Carcinoembryonic antigen
- ROC:
-
Receiver operating characteristic
- VTE:
-
Venous thrombosis
- NLR:
-
Neutrophil/lymphocyte ratio
- mGPS:
-
Modified Glasgow Prognostic Score
- RFS:
-
Recurrence-free survival
- CSS:
-
Cancer-specific survival
- CTCs:
-
Circulating tumor cells
References
Akgul O, Cetinkaya E, Ersoz S et al (2014) Role of surgery in colorectal cancer liver metastases. World J Gastroenterol 20(20):6113–6122
McNally SJ, Parks RW (2013) Surgery for colorectal liver metastases. Dig Surg 30(4–6):337–347
Simmonds PC, Primrose JN, Colquitt JL et al (2006) Surgical resection of hepatic metastases from colorectal cancer: a systematic review of published studies. Br J Cancer 94(7):982–999
Fong Y, Fortner J, Sun RL et al (1999) Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Ann Surg. 230(3):309–318 (discussion 318–321)
Nagashima I, Takada T, Adachi M et al (2006) Proposal of criteria to select candidates with colorectal liver metastases for hepatic resection: comparison of our scoring system to the positive number of risk factors. World J Gastroenterol 12(39):6305–6309
Pulivarthi S, Gurram MK (2014) Effectiveness of d-dimer as a screening test for venous thromboembolism: an update. N Am J Med Sci 6(10):491–499
Motavaf E, Sunesen KG, Stender MT et al (2014) Prognostic value of preoperative D-dimer and carcinoembryonic antigen levels in patients undergoing intended curative resection for colorectal cancer: a prospective cohort study. Int J Colorectal Dis 29(11):1427–1432
Yamamoto M, Yoshinaga K, Matsuyama A et al (2012) Plasma D-dimer level as a mortality predictor in patients with advanced or recurrent colorectal cancer. Oncology 83(1):10–15
Zhou YX, Yang ZM, Feng J et al (2013) High plasma D-dimer level is associated with decreased survival in patients with lung cancer: a meta-analysis. Tumour Biol 34(6):3701–3704
Ma X, Li Y, Zhang J et al (2014) Prognostic role of D-dimer in patients with lung cancer: a meta-analysis. Tumour Biol 35(3):2103–2109
Khoury JD, Adcock DM, Chan F et al (2010) Increases in quantitative D-dimer levels correlate with progressive disease better than circulating tumor cell counts in patients with refractory prostate cancer. Am J Clin Pathol 134(6):964–969
Go SI, Lee MJ, Lee WS et al (2015) D-dimer can serve as a prognostic and predictive biomarker for metastatic gastric cancer treated by chemotherapy. Med (Baltimore) 94(30):e951
Kanda Y (2013) Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant 48(3):452–458
Zacharski LR, Wojtukiewicz MZ, Costantini V et al (1992) Pathways of coagulation/fibrinolysis activation in malignancy. Semin Thromb Hemost 18(1):104–116
Caine GJ, Lip GY, Stonelake PS et al (2004) Platelet activation, coagulation and angiogenesis in breast and prostate carcinoma. Thromb Haemost 92(1):185–190
Mytnik M, Stasko J (2011) D-dimer, plasminogen activator inhibitor-1, prothrombin fragments and protein C—role in prothrombotic state of colorectal cancer. Neoplasma 58(3):235–238
Edwards CM, Warren J, Armstrong L et al (1993) D-dimer: a useful marker of disease stage in surgery for colorectal cancer. Br J Surg 80(11):1404–1405
Kilic M, Yoldas O, Keskek M et al (2008) Prognostic value of plasma D-dimer levels in patients with colorectal cancer. Colorectal Dis 10(3):238–241
Xu G, Zhang YL, Huang W (2004) Relationship between plasma D-dimer levels and clinicopathologic parameters in resectable colorectal cancer patients. World J Gastroenterol 10(6):922–923
Blackwell K, Hurwitz H, Lieberman G et al (2004) Circulating D-dimer levels are better predictors of overall survival and disease progression than carcinoembryonic antigen levels in patients with metastatic colorectal carcinoma. Cancer 101(1):77–82
Oya M, Akiyama Y, Yanagida T et al (1998) Plasma D-dimer level in patients with colorectal cancer: its role as a tumor marker. Surg Today 28(4):373–378
Mochizuki S, Yoshino T, Kojima T et al (2010) Therapeutic significance of a D-dimer cut-off level of > 3 microg/ml in colorectal cancer patients treated with standard chemotherapy plus bevacizumab. Jpn J Clin Oncol 40(10):933–937
Beppu T, Sakamoto Y, Hasegawa K et al (2012) A nomogram predicting disease-free survival in patients with colorectal liver metastases treated with hepatic resection: multicenter data collection as a Project Study for Hepatic Surgery of the Japanese Society of Hepato-Biliary-Pancreatic Surgery. J Hepatobiliary Pancreat Sci 19(1):72–84
Inanc M, Er O, Karaca H et al (2013) D-dimer is a marker of response to chemotherapy in patients with metastatic colorectal cancer. J BUON 18(2):391–397
Zhu L, Liu B, Zhao Y et al (2014) High levels of D-dimer correlated with disease status and poor prognosis of inoperable metastatic colorectal cancer patients treated with bevacizumab. J Cancer Res Ther 10(Suppl):246–251
Tomimaru Y, Yano M, Takachi K et al (2008) Correlation between pretherapeutic d-dimer levels and response to neoadjuvant chemotherapy in patients with advanced esophageal cancer. Dis Esophagus 21(4):281–287
Dirix LY, Vermeulen PB, Pawinski A et al (1997) Elevated levels of the angiogenic cytokines basic fibroblast growth factor and vascular endothelial growth factor in sera of cancer patients. Br J Cancer 76(2):238–243
Sakamoto Y, Miyamoto Y, Beppu T et al (2015) Post-chemotherapeutic CEA and CA19-9 are prognostic factors in patients with colorectal liver metastases treated with hepatic resection after oxaliplatin-based chemotherapy. Anticancer Res 35(4):2359–2368
Zhang D, Yu M, Xu T et al (2013) Predictive value of serum CEA, CA19-9 and CA125 in diagnosis of colorectal liver metastasis in Chinese population. Hepatogastroenterology 60(126):1297–1301
Loupakis F, Yang D, Yau L et al (2015) Primary tumor location as a prognostic factor in metastatic colorectal cancer. J Natl Cancer Inst 107(3):pii: dju427
Shen H, Yang J, Huang Q et al (2015) Different treatment strategies and molecular features between right-sided and left-sided colon cancers. World J Gastroenterol 21(21):6470–6478
Kirwan CC, Clarke AC, Howell SJ et al (2016) PO-31—circulating tumour cells and hypercoagulability: a lethal relationship in metastatic breast cancer. Thromb Res 140(Suppl 1):S188
Seeberg LT, Brunborg C, Waage A et al (2017) Survival impact of primary tumor lymph node status and circulating tumor cells in patients with colorectal liver metastases. Ann Surg Oncol 24(8):2113–2121
Zhao R, Cai Z, Li S et al (2017) Expression and clinical relevance of epithelial and mesenchymal markers in circulating tumor cells from colorectal cancer. Oncotarget 8(6):9293–9302
Tieken C, Versteeg HH (2016) Anticoagulants versus cancer. Thromb Res 140(Suppl 1):S148–S153
Klerk CP, Smorenburg SM, Otten HM et al (2005) The effect of low molecular weight heparin on survival in patients with advanced malignancy. J Clin Oncol 23(10):2130–2135
van Doormaal FF, Di Nisio M, Otten HM et al (2011) Randomized trial of the effect of the low molecular weight heparin nadroparin on survival in patients with cancer. J Clin Oncol 29(15):2071–2076
Rothwell PM, Wilson M, Elwin CE et al (2010) Long-term effect of aspirin on colorectal cancer incidence and mortality: 20-year follow-up of five randomised trials. Lancet 376(9754):1741–1750
Acknowledgements
We thank Ms. Yukie Saito, Ms. Tomoko Yano, Ms. Tomoko Ubukata, and Ms. Yuki Saka for their excellent assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
About this article
Cite this article
Watanabe, A., Araki, K., Harimoto, N. et al. D-dimer predicts postoperative recurrence and prognosis in patients with liver metastasis of colorectal cancer. Int J Clin Oncol 23, 689–697 (2018). https://doi.org/10.1007/s10147-018-1271-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-018-1271-x