Abstract
Reactive lymphoid hyperplasia (RLH) is a rare, benign, lymphocytic tumour-like lesion reported in various organs. It has been previously identified in 18 cases in the English-language literature, but only 5 of them were related to oncological disease. No previous cases have been described of RLH occurring in ovarian cancer patients. We describe a case of hepatic RLH which developed in a patient treated for ovarian cancer 11 years previously. Radiological features on computed tomography (CT) scan and PET–CT (positron emission tomography–computed tomography) were strongly suggestive of oncological disease, in contrast to magnetic resonance imaging (MRI); the volume increment of the nodular lesion and the rise in carbohydrate antigen 125 corroborated the hypothesis of malignancy. The patient was subjected to resection of the 7th segment of the liver and the final histological report showed RLH. RLH should be considered in the presence of hepatic lesions in suspected ovarian cancer recurrence. Imaging techniques should be thoroughly investigated to exclude tumor recurrence promptly, in order to avoid unnecessary surgery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The liver is the fourth most common site of metastasis in recurrent ovarian cancer (OC) [1]: clinical data from living patients have shown an incidence of hepatic metastasis of approximately 9.4% [2]; moreover, several autopsy studies have indicated a major incidence of liver metastasis in relapsed OC ranging from 48% to 58.4% [1, 2].
In this report we described the case of a 58-year-old woman subjected to surgical hepatic resection for an isolated lesion on the 7th segment of the liver, mimicking an ovarian cancer relapse confined to hepatic tissue; this initial hypothesis was corroborated by the imaging findings and by the rise in tumour markers. Finally, the definitive histological report confirmed reactive lymphoid hyperplasia (RLH), a rare, benign, lymphocytic tumour-like lesion. Hepatic RLH has been previously identified in 18 other cases in the English-language literature [3–5], but only 5 [4–7] of them were related to oncological disease, without gynaecological malignancies.
Case report
A 58-year-old woman was admitted to our Institution in April 1995 with adnexal complex masses, ascites and carbohydrate antigen (CA) 125 values of 927 U/ml. She underwent primary cytoreductive surgery, with residual tumour smaller than 0.5 cm. The histological examination documented a serous papillary ovarian carcinoma, moderately differentiated, stage IIIC according to FIGO (International Federation of Obstetricians and Gynecologists) staging. She was also subjected to six cycles of adjuvant platinum-based chemotherapy according to the PAC (cisplatin, doxorubicin, and cyclophosphamide) schedule. Standard subsequent follow-ups were all negative until March 2007, when there was a rise in CA-125 to 70.7 U/ml (normal level <35); an abdominal ultrasound examination demonstrated an hypoechoic nodular lesion, 4 × 7 mm in diameter, in the right lobe of the liver. Subsequently, in April 2007, several laboratory data including liver functions tests were remarkable, especially aspartate amino-transferase (230 U/l, normal range 10–45 U/l) and alanine amino-transferase (298 U/l, normal range 10–43 U/l); in contrast, hepatic markers and antinuclear and antimitochondrial antibodies were all negative. No predisposing factors for hepatic cirrhosis, steatohepatitis or dysmetabolic diseases were identified.
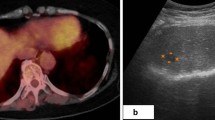
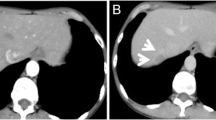
The patient underwent an abdomino-pelvic computed tomography (CT) scan which showed a vascularised hypodense lesion (25 mm) in the 7th segment of the liver with hepatic hilar lymphadenopathy; subsequently, a nodular area of 15 × 17 mm in diameter, with a slightly high intensity in T2-weighted images and low intensity in T1-weighted images, was observed on magnetic resonance imaging (MRI). The radiological team initially concluded a diagnosis of a benign mass, probably of adenomatous origin (Fig. 1). In May 2007, the serum CA-125 level rose to 126 U/ml. The patient finally underwent whole-body positron emission tomography–computed tomography (PET–CT) which showed aspecific left laterocervical hyperfixation and an hypodense lesion at the 7th segment, of 19 mm, with high metabolic uptake and multiple para-aortic lesions with standardised uptake value (SUV) up to 7.2. Since metastatic liver tumor could not be excluded, the patient underwent surgery in June 2007, with a wedge resection of the 7th segment of the liver.
MRI images. Axial T1-weighted image (a) shows an hypointense nodular area on the 7th segment of the liver and (b) a hyperintense signal on coronal T2-weighted imaging (c) a progressive isointensity in the parenchymal-venous phase and (d) ring enhancement in the delayed phase after 1 h in the coronal plane
The patient’s post-operative course was good and she was discharged on the 8th post-operative day.
Histological and immunohistochemical analyses were performed by two independent senior pathologists. The resected area measured 30 × 28 × 17 mm. Macroscopic examination demonstrated a yellowish-white, not encapsulated, well-circumscribed nodular lesion, measuring 12 mm in diameter. On microscopic evaluation, hyperplastic lymphoid follicles were observed with secondary follicles primed for germinal centre formation. Focal lymphoid infiltration was seen in the portal area, surrounding the lymphoid nodule; peripheral multi-nucleate giant cells were also observable. On immunohistochemical examination, CD3-positive cells were mainly localized in the parafollicular area and CD20 immunostaining was positive for B follicles, while bcl-2 staining was negative. All these aspects were relevant to excluding a well-defined follicular lymphoma, and a diagnosis of “reactive lymphoid hyperplasia” (RLH) of the liver (Fig. 2) was definitively established.
The tumor marker CA-125 returned to its normal range 3 months after surgery. To date, after 28 months of follow-up, the patient is still disease-free.
Discussion
Ovarian cancer is the second most common cause of death in women with gynaecological malignancies worldwide. Despite aggressive initial treatment, the majority of patients remain with persistent disease or develop fatal recurrence. Usually, the disease remains confined to the peritoneal cavity and lymph nodes, but recently some evidence regarding metastatic patterns of ovarian carcinoma has indicated the liver as the fourth (48%) most common site of recurrence of ovarian disease, after the peritoneum (97–99%), the abdominal lymph nodes (74%) and the bowel (55%) [1].
In this paper, the presence of a small, isolated lesion on the 7th segment of the liver, concomitant with multiple lymphadenopathy, was initially presumed to be a liver-localized recurrence of primitive ovarian cancer. For this reason, the general surgeon’s and the oncological radiologist’s team finally decided on surgery, with the entire resection of the 7th segment. However, the final histological evaluation showed RLH, a benign lymphocytic tumour-like lesion with polyclonal features.
To the best of our knowledge only 5 cases of hepatic implantation of RLH have been previously described as coincident with a preceding diagnosis of oncological disease, such as renal cell carcinoma [6], colon and gastric cancer [5, 7] and finally in a patient with multiple carcinoma [6] (Table 1). Moreover, our report is the first experience of hepatic RLH occurring in previous ovarian cancer mimicking relapse of carcinoma.
Reactive lymphoid hyperplasia of the liver is described as a rare benign lesion presenting as a small nodule. It is also known as nodular lymphoid hyperplasia and pseudolymphoma, but it is inflammatory and reactive rather than neoplastic. It is moreover distinct from pseudotumor and, unlike this entity, it lacks the clinical and pathological features of inflammation, which include fever, myofibroblastic proliferation, xanthogranulomatous change and occlusive portal phlebitis. Finally, it has a favorable prognosis but, to date, there are no imaging modalities able to predict exactly the benign features of this disease.
In our reported case, the hypothesis of malignancy was corroborated by several aspects. Primarily, on the basis of the radiological appearance by CT scan and PET–CT, tumour could not be definitively excluded. Also suggestive of malignancy was the rapid increase in size of the nodular lesion, evidenced by comparing the CT scans with the preceding ultrasound scans. Finally, all these elements were concomitant with the increase in the tumor marker CA-125, which has been demonstrated to strongly predict ovarian cancer relapse [8].
A reasonable method of prompt discrimination would have been to perform an hepatic biopsy, but evidence of sampling error or failure to obtain a suitable specimen are frequently described for this invasive procedure [4, 6]; this is particularly notable when considering the rarest pathologies, such as the one described in our case, which need several fragments of tissue in order to achieve a thorough and accurate immunohistochemical analysis.
In conclusion, all these considerations persuaded the authors to require surgery as essential for a proper diagnosis and to definitively exclude or confirm the hypothesis of malignancy; furthermore, in the case of malignancy, the patient would have been considered as platinum-sensitive and, based on previous experiences [9, 10], radical debulking surgery could have had a therapeutic effect.
This case suggests that RLH should be considered in the differential diagnosis of hepatic lesions in women with suspected ovarian cancer recurrence. Although many advances have been made in imaging techniques, it also strongly supports the predictive value of the classical imaging modalities, such as ultrasound, CT and MRI, and the promising PET–CT, which should be still acutely investigated in order promptly to rule out tumor recurrence and avoid unnecessary surgery.
Abbreviations
- RLH:
-
Reactive lymphoid hyperplasia
- CT:
-
Computed tomography
- PET–CT:
-
Positron emission tomography–computed tomography
- MRI:
-
Magnetic resonance imaging
- OC:
-
Ovarian cancer
- FIGO:
-
International Federation of Obstetricians and Gynecologists
- PAC:
-
Cisplatin, doxorubicin, and cyclophosphamide
- CA 125:
-
Carbohydrate antigen 125
- SUV:
-
Standardised uptake value
References
Güth U, Huang DJ, Bauer G et al (2007) Metastatic patterns at autopsy in patients with ovarian carcinoma. Cancer 110(6):1272–1280
Park CM, Kim SH, Moon MH et al (2003) Recurrent ovarian malignancy: patterns and spectrum of imaging findings. Abdom Imaging 28(3):404–415 (review)
Machida T, Takahashi T, Itoh T et al (2007) Reactive lymphoid hyperplasia of the liver. World J Gastroenterol 13(40):5403–5407
Sato K, Ueda Y, Yokoi M et al (2006) Reactive lymphoid hyperplasia of the liver in a patient with multiple carcinomas: a case report and brief review. J Clin Pathol 59(9):990–992
Takahashi H, Sawai H, Matsuo Y et al (2006) Reactive lymphoid hyperplasia of the liver in a patient with colon cancer: report of two cases. BMC Gastroenterol 6:25
Pantanowitz L, Saldinger PF, Kadin ME (2001) Pathologic quiz case: hepatic mass in a patient with renal cell carcinoma. Arch Pathol Lab Med 125:577–578
Kim SR, Hayashi Y, Kang KB et al (1997) A case of pseudolymphoma of the liver with chronic hepatitis C. J Hepatol 26:209–214
Gadducci A, Cosio S, Carpi A et al (2004) Serum tumor markers in the management of ovarian, endometrial and cervical cancer. Biomed Pharmacother 58:24–38
Benedetti Panici P, De Vivo A, Bellati F et al (2007) Secondary cytoreductive surgery in patients with platinum-sensitive recurrent ovarian cancer. Ann Surg Oncol 14(3):1136–1142
Chi DS, McCaughty K, Diaz JP et al (2006) Guidelines and selection criteria for secondary cytoreductive surgery in patients with recurrent, platinum-sensitive epithelial ovarian carcinoma. Cancer 106(9):1933–1939
Conflict of interest
No author has any conflict of interest.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Marchetti, C., Manci, N., Di Maurizio, M. et al. Reactive lymphoid hyperplasia of liver mimicking late ovarian cancer recurrence: case report and literature review. Int J Clin Oncol 16, 714–717 (2011). https://doi.org/10.1007/s10147-011-0191-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-011-0191-9