Abstract
Peripheral nerve injuries are often associated with injuries of adjacent tissue. As a result of anatomic proximity between nerves and vascular structures, there is a high chance of combined injuries of these structures (23 %). The aim of our study is to describe and analyze associated nerve and vascular injuries of the upper extremity in patients treated at the Clinic of Neurosurgery in Belgrade over a 10-year period. This study included 83 patients that received surgical treatment at the Clinic of Neurosurgery in Belgrade after having been diagnosed with upper extremity nerve injury. The study included all patients that satisfied these criteria over a period of 10 years. The patients with associated vascular injuries, 36 of them, were considered our study group, while 47 patients without associated vascular injuries were considered our control group. Finally, we compared treatment outcome between these groups. The final outcome evaluation was performed 2 years after surgical treatment. In our study group, 84.8 % surgical nerve repair was successful (fair, good, and excellent outcome), while in the control group (patients without vascular injury), surgical nerve repair was successful in 87.9 %. The overall satisfactory neurological outcome (M3–M5) was present in 86.6 % of nerve repairs. Our study shows that there is no significant difference between the treatment outcome in patients with associated nerve and vascular injuries and patients with isolated nerve injuries if they are diagnosed in time and treated appropriately. Successful treatment can only be accomplished through a multidisciplinary approach undertaken by a highly qualified medical team.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Peripheral nerve injuries are complex injuries that are often associated with injuries of adjacent tissue [10, 37]. As a result of anatomic proximity between nerves and vascular structures, there is high chance of combined injuries of these structures–23 % [35]. Upper extremity injuries can sometimes be life threatening [2, 12] but even more often they can compromise the quality of life. The injured nerve palsy and, especially, arm amputation due to irreversible ischemia after the injury of vascular structures are the main causes of disability [12]. The mortality and morbidity of patients with associated nerve and vascular injuries are in correlation with the timing of the surgical treatment [12]. According to most authors, one of the indications for primary nerve repair is suspected associated vascular injury. If there is no vascular injury, and no apparent indication for transection of the nerve, nerve repair is usually performed with a delay from 3 weeks up to 6 months after detailed evaluation of the extent of the injury [37].
As it is commonly known, injuries of the extremities are especially frequent during war time. Therefore, it is hard to determine exact prevalence of these injuries. Analyzing the data in the literature concerning injuries of the upper extremities, we found that the prevalence of injury of the upper extremities ranges from 1.56 to 39 % [6]. Apart from the prevalence, upper extremity injuries in war and in peace time also differ in their etiology and mechanism. In war time, upper extremity injuries are mostly caused by high energy forces—missiles and explosions [32], while in peace time they are more likely caused by sharp objects, falls, or traffic accidents [7, 16, 26]. Different injury etiologies cause different types of vascular trauma and nerve injury. The controversy over the optimal management of severe upper extremity injuries revolves around two basic approaches. One involves aggressive treatment directed at limb salvage and restoration of intrinsic function, whereas the other proposes more conservative measures—hemorrhage control and little if any attempt to repair nerves because of the belief that ultimately these are functionless extremities [18]. When it comes to combined peripheral nerve and vascular injuries, in the published literature, there is only limited data with little emphasis on the treatment of nerve injuries.
The aim of our study is to describe and analyze associated nerve and vascular injuries of the upper extremity in patients treated at the Clinic of Neurosurgery, Clinical Center of Serbia, over a 10-year peacetime period. The analysis concerns the etiology, the mechanisms, and the results of surgical treatment of these injuries.
Material and methods
This study included 83 consecutive patients that received surgical treatment at the Clinic of Neurosurgery, Clinical Center of Serbia, after having been diagnosed with upper extremity nerve injury. The study included all patients that satisfied these criteria over a period of 10 years, from January 1, 2001 to December 31, 2010. The patients with associated vascular injuries, 36 of them, were considered our study group, while 47 patients without associated vascular injuries were considered our control group. Finally, we compared treatment outcome between these groups.
Study group population
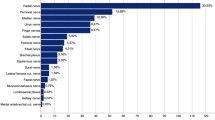
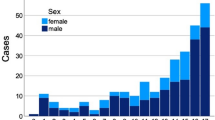
All 36 patients in our study were male. The youngest patient was 18 and the oldest 47 years old, with the mean age of 32.9 years. The injuries of the dominant hand were more frequent (58.33 %). Out of 36 patients, 34 were treated in other medical center for severe ischemia. The injuries were most frequently caused by a sharp object, in 47.2 % of cases. The second most frequent cause of injury was gunshot injury, in 30.5 % of cases. Blunt trauma was the cause of injury in 22.2 % cases (Table 1). The most common localization of injury was at the arm level, in 42.5 % of the cases, while 33.3 % had brachial plexus injury and 17.5 % had injury at the forearm level (Table 2). During the primary treatment, only one nerve repair was attempted. In one other case, nerve stumps were identified and marked by colored sutures, but in the majority of patients, the extent of nerve injury was not identified during the initial treatment.
The most commonly injured arterial blood vessel was the brachial artery, in 41.7 % of cases, followed by the subclavian artery (25.0 %) and the axillary and radial artery (11.1 % each). The most frequently injured vein in our study was subclavian vein (27.5 %) (Table 3). All vascular injuries were treated primarily in other medical centers (Table 4).
During the secondary surgical procedure, the injured vascular elements were re-operated in six cases, while in other 28 patients’ blood vessels were only dissected from the scar tissue. There were four cases in which angiography studies showed poor blood flow of the previously repaired vessel, so secondary vascular surgical procedure was performed—reparation using a venous graft. Also, there was one case where thrombectomy was performed. In one case, a traumatic AV fistula was formed, so during the secondary treatment a ligature of the traumatic AV fistula and reconstruction of artery and vein with interposition of venous graft was done.
During the secondary procedure, 45 nerve repairs were performed. No direct suture was possible. Neurolysis and dissection of the scar tissue as only surgical procedure was performed in 1.1 % of procedures. Nerve grafting was used for repair of 46.7 % of injured nerve elements. In 42.2 % of injured nerve elements, the extent of injury necessitated a complex nerve repair (nerve grafting and nerve transfer combined) (Table 5). The majority of patients underwent secondary surgical treatment in the period between 6 and 9 months after the injury; 6 patients were operated within the first 3 months, 11 patients were operated between 3 and 6 months after the injury, and 6 patients were operated after more than 9 months after injury.
In addition to the nerve and vascular injury, in several cases, other tissues were affected as well. The most common injury was bone fracture, 62.5 % requiring surgical osteosynthesis during the primary treatment. There were six cases of hemothorax, requiring thoracic drainage. In one case, an emergency fasciotomy was performed due to the development of compartment syndrome, and also in one case, industrial injury created large skin defect that was repaired using Tiersch skin grafting.
Control group
Control group consisted of 44 males and 3 females. The youngest patient was 19 and the oldest 52 years old, with the mean age of 33.4 years. The injuries were most frequently caused by a sharp object, in 40.4 % of cases, followed by equally frequent gunshot injury and blunt trauma that was the cause of the injury in 29.8 % of cases (Table 6). The most common localization of injury was at the arm level, in 48.9 % of the cases, while 36.2 % had brachial plexus injury and 14.9 % had injury at the forearm level (Table 7).
During the surgical treatment, 57 nerve repairs were performed. No direct suture was possible. Neurolysis and dissection of the scar tissue as only surgical procedure was performed in 14.0 % of procedures. Nerve grafting was used for repair of 47.4 % of injured nerve elements. In 38.6 % of injured nerve elements, the extent of injury necessitated a complex nerve repair (nerve grafting and nerve transfer combined) (Table 8). In addition to the nerve injury, in several cases other tissues were affected as well. The most common injury was bone fracture that occurred in 18 cases, 38.9 % requiring surgical osteosynthesis during the initial treatment. Also, in one case, a large skin defect had to be repaired using Tiersch skin grafting.
The majority of patients, 42.6 %, underwent secondary surgical treatment in the period between 6 and 9 months after the injury; 7 patients were operated within the first 3 months, 12 patients between 3 and 6 months after the injury, and 8 patients were operated after more than 9 months after injury.
Surgical procedure
All 36 patients from the study group were initially treated in other medical centers. During this treatment, only vascular injuries were treated while due to unavailability of required technical equipment with the exception in two cases, nerve injury was not addressed. The mechanism of the major blood vessel injury dictated the choice of vascular reconstructive procedure: direct suture in uncomplicated cases, graft interposition or bypass in cases of more extensive damage. The use of autologous venous graft was the priority. The use of synthetic graft was acceptable only when the venous graft was unavailable. Lesser blood vessels that could not be repaired were ligated.
After the initial trauma recovery, detailed evaluation followed and secondary surgical treatment was performed if there were no signs of recovery or if only partial recovery occurred and the deficits were thought to be potentially reversible. The diagnostic methods used in the evaluation of these patients included the following: detailed patient history and neurological examination, electrophysiological studies (electromyoneurography (EMNG), evoked potential studies), radiological examinations (x-ray, computed tomography (CT), magnetic resonance imaging (MRI)), ultrasonographic examinations (including Color Doppler Sonography/CDS/of the injured extremity), and selective upper extremity angiography.
Primary vascular surgical procedure
Vessels were repaired according the principles of vascular surgery. Whenever possible, autologous venous graft was insisted on; usually, it was the saphenous vein. Synthetic materials were used in proximal positions (axillar and subclavian vein) or in the lack of autologic material. Both arterial and vein reconstruction were given equal priority. All patients were heparinized during the operation. The most common procedure was the reconstruction of brachial segment, usually with the reversed saphenous vein. The use of synthetic graft was acceptable only when venous graft was unavailable. Special care was taken for vein reconstruction was since vein drainage is the most important factor for limb physiological function. Lesser blood vessels that could not be repaired were ligated. The cell saving system was routinely used to decrease the need for heterologic transfusions. Wide range antibiotics were mandatorily used to prevent infection, which could initiate secondary bleeding as the most feared complication. Postoperative anticoagulation by means of low weight heparin was used in protective doses. In cases of late revascularization, there was danger of compromising blood circulation due to the development of compartment syndrome. Prompt decompression was achieved by means of fasciotomy. To improve recovery time, free skin transplant is a good solution, after edema decrement. Elastic bandage is useful as an adjuvant measure. According to general principles in vascular surgery, angiogram was made in every case. On the other hand, color duplex scan (CDS) was used to provide information regarding the venous system.
Secondary surgical procedure
Secondary surgical procedure was performed jointly by the same neurosurgeon and a vascular surgeon at the Clinic of Neurosurgery in Belgrade. Vascular surgeon’s assistance was particularly significant during the dissection of scar tissue and for proper manipulation with the vascular grafts. Additional vascular repair was done in selected cases. Concerning nerve repair, no direct suture was possible, but other procedures—neurolysis, nerve grafting, and nerve transfer—were performed.
Two weeks after the secondary surgical treatment, all patients underwent physical therapy at a rehabilitation center for at least 3 weeks. They continued with physical therapy at home. The first follow-up evaluation was performed 3months, the second after 6 months, and the third 1 year after surgery. These follow-up exams involved clinical, neurological, and EMNG examination. The final outcome evaluation was performed 2 years after surgical treatment.
Statistical analysis and outcome evaluation
Detailed patient information was obtained from patients’ medical records and it included the following: general patient data, trauma etiology (sharp injury, shotgun injury, traffic accident, fall etc.), injury localization (nerve and blood vessel involved, level of injury, type of injury), other associated injuries, type of surgical treatment, and treatment outcome.
Postoperative motor function of the injured extremity was evaluated using Louisiana State University Medical Center System for motor function. Motor function grade M2 to M5 was considered successful recovery after peripheral nerve repair.
In the evaluation of the results of the surgical treatment of brachial plexus injuries, we used our modification of Louisiana State University Medical Center Grading System, because of complexity of the shoulder function involving several muscles, the role of two muscles (biceps and brachialis) in elbow flexion, and their different importance for the range and endurance of motion. Modified motor grades are (1) “bad” denotes no movement or weightless movement; (2) “fair” denotes movement against gravity with the ability to hold position, active abduction up to 45°, elbow flexion up to 90°, the range of external rotation from full internal rotation up to 45°; (3) “good” denotes movement against resistance with the ability to repeat movements in succession, active abduction of more than 45°, full range elbow flexion, external rotation up to 90, and (4) “excellent” denotes near normal function with external rotation over 90°. Fair, good, and excellent results were considered to represent recovery. According to our grading system, recovery roughly corresponds to M2 or more grade of recovery according to the Louisiana State University Medical Center grading system and to M3 or more grade of recovery according to the British Medical Research Council system.
Statistical analysis was performed using the IBM SPSS v22 Statistic tool. The following tests were performed: analysis of descriptive values (number and percentage of cases, mean, minimal and maximal values), Chi-square test, Pearson’s test, Fisher test, and Mann Whitney test.
Results
The final outcome evaluation in our study group was performed 2 years after the secondary surgical treatment (Table 9). Overall successful treatment was achieved in 39 (84.8 %) of nerve repairs. Bad treatment outcome was found in 7 (15.2 %) nerve repairs, fair treatment in 14 (30.4 %) nerve repairs, good in 23 (50.0 %), and excellent in 2 (4.3 %). Successful treatment (fair, good and excellent outcome) was found in 4 out of 5 cases (80.0 %) where only neurolysis was performed, and also in 27 cases out of 31 nerve grafting (87.1 %), and 28 out of 30 nerve transfers (93.5 %). Considering cases where nerve transfer was performed, successful treatment was achieved in 16 out of 18 nerve transfers (88.9 %) where axillar nerve was used, and in 17 out of 19 nerve transfers (89.5 %) where musculocutaneous was used. In the similar fashion, we evaluated treatment outcome in our control group, 2 years after surgical treatment (Table 10). Overall successful treatment was achieved in 51 (87.9 %) of nerve repairs. Bad treatment outcome was found in 7 (12.1 %) nerve repairs, fair treatment in 15 (25.8 %) nerve repairs, good in 33 (56.9 %) and excellent in 3 (5.2 %). Successful treatment (fair, good, and excellent outcome) was found in 6 out of 8 cases (75.0 %) where only neurolysis was performed, and also in 23 cases out of 27 nerve grafting (85.2 %), and 22 out of 23 nerve transfers (95.7 %). Considering cases where nerve transfer was performed, successful treatment was achieved in 21 out of 22 nerve transfers (95.5 %) where axillar nerve was used and in 22 out of 23 nerve transfers (95.7 %) where musculocutaneous was used.
In the study group, 86.1 % cases surgical nerve repair was successful (fair, good, and excellent outcome), while in the control group (patients without vascular injury), surgical nerve repair was successful in 87.2 % (Table 11).
Table 12 shows grade of recovery in our study, according to mechanism of injury. In our study group, successful recovery of sharp nerve injuries—lacerations was accomplished in 82.4 %, blunt injuries in 62.5 %, and gunshot injuries in 90.9 % of cases. In our control group, there is slightly better rate of recovery—in case of lacerations 89.4 %, blunt injuries 85.7 %, and gunshot injuries 85.7 %. Further statistical analysis was not possible due to small frequencies.
The overall successful treatment outcome in both groups was present in 86.6 % of nerve repairs.
In order to confirm that our two groups were comparable, we performed statistical analysis for already known factors (except vascular injury) that could influence treatment outcome. Study and control group were no significantly different according to age (T test for two independent samples, p = 0.756, p > 0.05), etiology of injury (Chi-square test, p = 0.918, p > 0.05), mechanism of injury (Chi-square test, p = 0.718, p > 0.05), preoperative neurological deficit (Fisher’s exact test, p = 0.693, p > 0.05), type of nerve injury (Chi-square test, p = 0.590, p > 0.05), level of injury (Fisher’s exacts test, p = 0.980 m p > 0.05), injured nerve (Chi-square test, p = 0.480, p > 0.05), and timing of nerve repair (Chi-square test, p = 0.932, p > 0.05).
Finally, using Chi-square test, the statistical analysis showed that there was no significant difference in treatment outcome in patients with associated vascular injuries compared to isolated nerve injuries alone in our study (Chi-square test, p = 0.972, p > 0.05).
Discussion
The brachial plexus and peripheral nerve injuries of the upper extremity can often lead to disability [21]. If the nerve injuries are associated with vascular trauma they may, in the case of ischemia, lead to inevitable arm amputation or even lethal outcome [9, 11, 30, 33]. Analyzing the data in the literature concerning upper extremity injuries, we found that the prevalence of upper extremities ranges from 1.56 to 39 % [6]. The main cause for this discrepancy is the difference in the frequency of occurrence of this type of injuries in war time and in peace time. In peace time, the most common peripheral nerve injuries of upper extremities are injuries of forearm [7, 19, 26]. Distal peripheral nerve injuries of the upper extremity are mostly caused by a sharp object, while injuries of the brachial plexus are mostly caused by traffic accidents [13]. In war time, on the other hand, upper extremity injuries are mostly shotgun injuries and injuries caused by explosive devices.
Previous studies show that the most common cause of forearm nerve injuries during times of peace are lacerations [10, 26]. This is also the case in our study—43.3 % patients were injured by a sharp object (knife, glass, or saw).
Previous studies show male preponderance in peripheral nerve injuries—approximately 80–95 % of injured patients are male [10, 16, 26, 37]. This was even more unambiguous in our study, since there were only three females in our study (96.4 % of our patients were male).
Injuries of the main vascular elements of upper extremities may be fatal, so early diagnosis and urgent interventions are crucial in their treatment and in the amputation prevention [8, 34]. Recognizing and diagnosing extremity vascular injury is particularly problematic in polytraumatized patients, especially those who are unconscious or confused, and in patients with blunt trauma. Blunt extremity trauma can be associated with bone fractures and joint dislocations, which may lead to severe blood vessel injury. Also, it is usually associated with worse outcome in comparison to penetrating injuries [5].
The spectrum of available diagnostic procedures for vascular injuries ranges from the very basic to the most sophisticated ones. Simple chest X-ray could be indicative for bleeding, leading to angiography or CT scan and surgical exploration as a final act. Bleeding from proximal parts of arterial tree could be more challenging, with no or very discreet signs [25, 33]. In our study group, 77.8 % of patients had an open injury, so the diagnosis of vascular injury did not present a difficulty (Table 1).
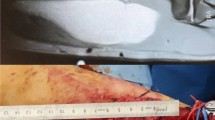
During the primary vascular procedures, the main goal was hemostasis, as a lifesaving procedure. Urgent vascular procedures were necessary due to the limited ischemic period, demanding prompt revascularization. Bone stabilization was essential prior to vascular reconstruction. In the majority of cases, the focus was on limb salvage procedure and there was no attempt of nerve reparation. An exception was made in one case of laceration (out of 17), where the nerve repair was performed since the nerve injury was obvious. In several cases nerve stumps were only marked with color sutures. A possible cause of unrecognized nerve injuries may have been the lack of necessary microsurgical training and equipment. Another possible reason for this may lie in the outdated but still widespread opinion that associated nerve and vascular injuries have poor prognosis and that attempting repair is not essential during initial treatment (Fig. 1).
In our study group, nerve reconstruction in the secondary surgical treatment was performed in collaboration with a vascular surgeon. During secondary surgeries, injured vascular elements was re-operated in 7 cases, while in other 29 patients, blood vessels were dissected and liberated from the scar tissue. Both series of surgeries were performed without vascular complications, infections, and severe ischemia of the arm and hand of injured patients. Previous studies do not concur regarding the impact of vascular injury on long term functional recovery. Some authors report that acute vascular injuries do not affect functional recovery [14, 29, 36], while others maintain that acute vascular injuries, although promptly surgically reconstructed, may have an adverse effect on functional recovery [17, 32]. On the other hand, these studies are in agreement that unrecognized and untreated acute vascular injuries (intimal tears, thrombosis, avulsion of vessel branches, AV fistula), which are usually caused by blunt trauma, may lead to delayed arterial occlusion and compartment syndrome [1], and consecutively compromise nerve recovery. Our study shows that there is no significant difference in treatment outcome in patients with associated nerve and vascular injuries compared to isolated nerve injuries if they are diagnosed in time and treated appropriately (Fig. 2) [14, 27, 36].
Prognostic factors affecting the final outcome of peripheral nerve injuries include the following: type of nerve injury, lesion site (proximal, distal, type of nerve), severity of nerve injury, surgery timing, patient’s age, and type of surgical procedure [20, 28]. Proximal nerve injuries have worse outcome than distal ones because the distance that regenerating fibers have to bridge is larger and also because nerve at a proximal level innervates a larger number of muscles. The nerve defect increases with the passage of time between the injury and the surgical treatment, due to fibrotic changes, degeneration, and contraction of nerve stumps. Furthermore, there are time-dependent fibrous atrophic changes in denervated muscles. Unfortunately, the majority of our patients had injury at the arm level (Table 2).
The majority of patients in our study group, 29 (80.99 %), underwent secondary surgical treatment between 6 and 9 months after the injury. Most authors agree that nerve injuries caused by a sharp object should be operated within 24 h after the injury [3]. However, it is prudent to delay treatment of shotgun injuries and blunt injuries. Clinical and EMNG evaluation are done monthly, and if there are no clinical or electrophysiological signs of spontaneous recovery after 3 months of the injury, surgical treatment should be performed. If there are signs of spontaneous recovery, conservative treatment is advised. The authors generally agree that traction injuries should be operated within 3 to 6 months after the injury [31, 37]. The reason for this time limit is because after that period the ability for functional recovery is significantly lower due to the narrowing of endothelial tubules, decreased regenerating potential of nerve cells, and increased resistance to regeneration of motor end plates. In ischemic patients, patients with polytrauma, and those who are unconscious, it is often difficult or even impossible to establish the extent of nerve injury because it is disguised by other injuries. In Shaw et al.’s study, nerve injuries were noticed during vascular surgery in only 3 out of 11 patients with blunt trauma [29]. In our study, nerve injury was recognized in only one case during the primary surgical treatment, and in this case, neurorrhaphy was performed.
Experts generally agree that, if the nerve lesion is recognized during primary surgical procedure, but the nerve was not injured by a sharp object, nerve stumps should only be marked with color sutures to prevent contraction and to alleviate secondary neurosurgical treatment.
The choice of an adequate surgical method is based on the complete evaluation of every patient, which consists of clinical evaluation (patient history, clinical and neurological examination), electrophysiological evaluation (EMNG, SSEP), radiological evaluation (X-ray, CT, MRI, and angiography) and, in selected cases, surgical treatment.
In our study group, complex nerve repair was performed in 23 % of cases. It was done in patients with severe trauma, where nerve grafting alone could not be performed, so a combination of grafting and nerve transfer was necessary [15, 22–24, 27] (Table 5).
Apart from associated nerve and vascular injuries, several patients in our study group had additional associated injuries of other adjacent tissues. This was most often the case in patients who were injured by the impact of high energy force. The high energy force usually occurs in traffic accidents, shotgun injuries, industry-related injuries, falls from a height, and injuries caused by a chainsaw [29, 35]. Other most common associated injuries in our study group, and also in other published papers [4], were fractures—in 16 patients. Hemothorax as the second most frequently associated injury was found in 7 patients, while large skin defects were found in 1 patient.
Conclusion
Studies on associated nerve and vascular injuries in peace time are scarce. Our study shows that there is no significant difference in treatment outcome in patients with associated vascular injuries compared to isolated nerve injuries alone if they are diagnosed in time and treated appropriately. However, there was a slight trend toward better results, especially regarding quality of recovery in the group of patients that had only nerve injury and for earlier timing of nerve repair in the group of patients with associated vascular and nerve injury of the upper extremity. We contend that whenever possible, an attempt should be made to preserve both vascular integrity and nerve function. Furthermore, the revascularization of the injured extremity may be a significant factor for good recovery of nerve function. Extremity amputation should be considered only in severe trauma where there is no salvageable tissue present. Successful treatment can only be accomplished through a multidisciplinary approach undertaken by a highly qualified medical team comprising a neurosurgeon, a vascular surgeon, an emergency medicine specialist, a radiologist, a plastic surgeon, and a physiatrist.
References
Balakrishnan G (2006) Ischaemic contracture of the hand. Indian J Plast Surg 39:94–102
Barmparas G, Inaba K, Talving P, David JS, Lam L, Plurad D, Green D, Demetriades D (2010) Pediatric vs adult vascular trauma: a National Trauma Databank review. J Pediatr Surg 45:1404–1412
Birch R, Raji AR (1991) Repair of median and ulnar nerves. Primary suture is best. J Bone Joint Surg (Br) 73(1):154–157
Chung KC, Spilson SV (2001) The frequency and epidemiology of hand and forearm fractures in the United States. J Hand Surg [Am] 26:908–915
Compton C, Rhee R (2005) Peripheral vascular trauma. Perspect Vasc Surg Endovasc Ther 17:297–307
Dougherty AL, Mohrle CR, Galarneau MR, Woodruff SI, Dye JL, Quinn KH (2009) Battlefield extremity injuries in operation Iraqi Freedom. Injury 40:772–777
Eser E, Aktekin LA, Bodur H, Atan C (2009) Etiological factors of traumatic peripheral nerve injuries. Neurol India 57(4):434–437
Eser F, Aktekin LA, Bodur H, Atan C (2009) Etiological factors of traumatic peripheral nerve injuries. Neurol India 57:434–437
Fakhrai M, Elshimali Y (2007) Repair of the first segment of subclavian artery injury in a trauma patient without thoracotomy. The Internet Journal of Thoracic and Cardiovascular Surgery 12:2
Franz RW, Skytta CK, Shah KJ, Hartman JF, Wright ML (2012) A five-year review of management of upper-extremity arterial injuries at an urban level I trauma center. Ann Vasc Surg 26:655–664
Galanakos SP, Zoubos AB, Ignatiadis I, Papakostas I, Gerostathopoulos NE, Soucacos PN (2011) Repair of complete nerve lacerations at the forearm: an outcome study using Rosén–Lundborg protocol. Microsurg 4:253–262
Gümbel D, Naundorf M, Napp M, Ekkernkamp A, Seifert J (2014) Diagnosis and management of peripheral vascular injuries. Unfallchirurg 117:445–460
Iriz E, Kolbakir F, Sarac A, Akar H, Keçeligil HT, Demirağ MK (2004) Retrospective assessment of vascular injuries: 23 years of experience. Ann Thorac Cardiovasc Surg 10:373–378
Jain DK, Bhardwaj P, Venkataramani H, Sabapathy SR (2012) An epidemiological study of traumatic brachial plexus injury patients treated at an Indian centre. Indian J Plast Surg 45(3):498–503
Kallio PK, Vastamaki M (1993) An analysis of the results of late reconstruction of 132 median nerves. J Hand Surg 188:97–105
Kim DH, Murovic JA, Tiel RL, Kline DG (2004) Mechanisms of injury in operative brachial plexus lesions. Neurosurg Focus 16(5):E2
Kouyoumdjian JA (2006) Peripheral nerve injuries: a retrospective survey of 456 cases. Muscle Nerve 34:785–788
Leclercq DC, Carlier AJ, Khuc T, Depierreux L, Lejeune GN (1985) Improvement in the results in sixty-four ulnar nerve sections associated with arterial repair. J Hand Surg [Am] 10:997–999
Manord J, Gerrard L, Kline D, Sternbergh C, Money S (1998) Management of severe proximal vascular and neural injury of the upper extremity. J Vasc Surg 27:43–9
McAllister RM, Gilbert SE, Calder JS, Smith PJ (1996) The epidemiology and management of upper limb peripheral nerve injuries in modern practice. J Hand Surg (Br) 21(1):4–13
Millesi H (2006) Factors affecting the outcome of peripheral nerve surgery. Microsurgery 26(4):295–302
Novak CB, Anastakis DJ, Beaton DE, Katz J (2009) Patient-reported outcome after peripheral nerve injury. J Hand Surg [Am] 34:281–287
Puzovic V, Samardzic M, Jovanovic M, Zivkovic B, Savic A, Rasulic L (2015) Etiology and mechanisms of ulnar and median forearm nerve injuries. Vojnosanit Pregl 72(11):961–7
Rasulic L, Puzović V, Krešimir R, Jovanović M, Samardžić M, Živković B, Savić A (2015) The epidemiology of forearm nerve injuries—a retrospective study. Acta Clin Croat 54(1):19–24
Rasulic L, Samardzic M (2015) Nerve grafting methods. In: Tubbs S (ed) Nerves and nerve injuries: vol 2: pain, treatment, injury, disease and future directions. Academic Press, San Diego, p 237–248
Razmadze A (1999) Vascular injuries of the limbs: a fifteen-year Georgian experience. Eur J VascEndovascSurg 18:235–239
Saadat S, Eslami V, Rahimi-Movaghar V (2011) The incidence of peripheral nerve injury in trauma patients in Iran. UlusTravmaAcilCerrahiDerg 17:539–44
Samardzic M, Rasulic L, Grujicic D, Milicic B (2000) Results of nerve transfer to the musculocutaneous and axillary nerves. Neurosurgery 46:93–103
Secer HI, Daneyemez M, Gonul E, Izci Y (2007) Surgical repair of ulnar nerve lesions caused by gunshot and shrapnel: results in 407 lesions. J Neurosurg 107:776–783
Shaw AD, Milne AA, Christie J, Jenkins AM, Murie JA, Ruckley CV (1995) Vascular trauma of the upper limb and associated nerve injuries. Injury 26:515–518
Shi L (2013) The delayed management of main arterial injuries in extremity trauma: surgical challenges and outcomes. Pak J Med Sci 29:64–67
Siqueira MG, Martins RS (2011) Surgical treatment of adult traumatic brachial plexus injuries: an overview. Arq Neuropsiquiatr 69(3):528–535
Stanec S, Tonković I, Stanec Z, Tonković D, Dzepina I (1997) Treatment of upper limb nerve war injuries associated with vascular trauma. Injury 28:463–468
Tan TW, Joglar FL, Hamburg NM, Eberhardt RT, Shaw PM, Rybin D, Doros G, Farber A (2011) Limb outcome and mortality in lower and upper extremity arterial injury: a comparison using the National Trauma Data Bank. Vasc Endovascular Surg 45:592–597
Topal AE, Eren MN, Celik Y (2010) Lower extremity arterial injuries over a six-year period: outcomes, risk factors, and management. Vasc Health Risk Manag 6:1103–1110
Troupis TG, Michalinos A, Manou V, Vlastos D, Johnson EO, Demesticha T, Skandalakis P (2014) Report of an unusual combination of arterial, venous and neural variations in a cadaveric upper limb. J Brachial Plex Peripher Nerve Inj 9:2
Vastamäki M, Kallio PK, Solonen KA (1993) The results of secondary microsurgical repair of ulnar nerve injury. J Hand Surg 18:323–326
Acknowledgments
We would like to thank our medical staff from Clinic of Neurosurgery in Belgrade, especially nurses and our colleagues from the Physiatry Department, for good work they have been doing all these years and without whom surgical treatment of patients with peripheral nerve injuries would not be nearly as successful.
No funding or other financial support was received for this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rasulic, L., Cinara, I., Samardzic, M. et al. Nerve injuries of the upper extremity associated with vascular trauma—surgical treatment and outcome. Neurosurg Rev 40, 241–249 (2017). https://doi.org/10.1007/s10143-016-0755-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-016-0755-2