Abstract
Navigated transcranial magnetic stimulation (nTMS) is a novel tool for preoperative functional mapping. It detects eloquent cortical areas directly, comparable to intraoperative direct cortical stimulation (DCS). The aim of this study was to evaluate the advantage of nTMS in comparison with functional magnetic resonance imaging (fMRI) in the clinical setting. Special focus was placed on accuracy of motor cortex localization in patients with rolandic lesions. Thirty consecutive patients were enrolled in the study. All patients received an fMRI and nTMS examination preoperatively. Feasibility of the technique and spatial resolution of upper and lower extremity cortical mapping were compared with fMRI. Consistency of preoperative mapping with intraoperative DCS was assessed via the neuronavigation system. nTMS was feasible in all 30 patients. fMRI was impossible in 7 out of 30 patients with special clinical conditions, pediatric patients, central vascular lesions, or compliance issues. The mean accuracy to localize motor cortex of nTMS was higher than in fMRI. In the subgroup of intrinsic tumors, nTMS produced statistically significant higher accuracy scores of the lower extremity localization than fMRI. fMRI failed to localize hand or leg areas in 6 out of 23 cases. Using nTMS, a preoperative localization of the central sulcus was possible in all patients. Verification of nTMS motor cortex localization with DCS was achieved in all cases. The fMRI localization of the hand area proved to be postcentral in one case. nTMS has fewer restrictions for preoperative functional mapping than fMRI and requires only a limited level of compliance. nTMS scores higher on the accuracy scale than fMRI. nTMS represents a highly valuable supplement for the preoperative functional planning in the clinical routine.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Performing surgery in eloquent brain areas remains a challenge in modern neurosurgery, especially in glial tumors, which spare neurological function while invading eloquent tissue. Functional information about the cortical and subcortical areas at risk is crucial for the avoidance of focal neurological deficits after tumor surgery.
Functional mapping with intraoperative direct cortical stimulation as it was published by Foerster, Penfield, and Jasper in 1954 remains the “gold standard” [17]. This technique requires a wide surgical exposure of eloquent cortical areas, which is not always adequate for the target lesion. Preoperative functional information is required to plan the extent of resection and the least invasive trajectory for the approach [18].
Today, the most commonly used tool for the noninvasive localization of brain functions is the functional magnetic resonance imaging (fMRI). Other methods such as magnet encephalography (MEG) and positron emission computed tomography are limited both in availability and spatial resolution. fMRI is based on a blood oxygenation level-dependent (BOLD) echo planar imaging technique. It allows the mapping of localized cortical blood oxygenation changes, thus identifying neuronal activity. In order to detect the functional motor cortex, the patient has to perform a standardized motor paradigm. The resolution is highly dependent on the patient’s motor task performance. Therefore, the method has limitations in incompliant or severely paretic patients [30]. A promising noninvasive MRI-based method in this regard is resting-state correlation mapping. Zhang et al. demonstrated in 2009 a preoperative visualization of the sensorimotor cortex using the spontaneous fluctuation of the BOLD data in four patients with rolandic lesions which correlated with the intraoperative direct cortical stimulation (DCS) [32]. Further clinical validation of this so far experimental method needs to be performed. Edema, enlarged vessels in arteriovenous malformation (AVMs), and mass effects of adjacent tumors can compromise the validity of fMRI data [1, 8, 9, 31]. MEG shows a higher correlation in identifying motor cortex in these cases; however, it is only available in very few centers [11]. A method that overcomes the abovementioned limitation due to a less sophisticated and more stable physical principle is transcranial magnetic stimulation (TMS). It is the only method detecting eloquent tissue directly comparable to intraoperative DCS and is a well-established tool especially in neurology. TMS is used as a diagnostic and prognostic indicator for measuring central motor latency or detecting epileptic foci. TMS applies a magnetically induced current inside a tissue, thus eliciting a direct electrical stimulation as used in the intraoperative DCS. Using TMS, a coarse location of the central region can easily be obtained. Since TMS is the only noninvasive technique directly determining functional motor cortex, comparable to intraoperative DCS, it is a very promising method for functional mapping. In order to yield accurate localizing results, TMS has to be combined with the anatomical images of the patient. Several solutions have been published combining TMS with various navigational principles [2, 10, 19]. None of these systems, however, was suitable for clinical routine, mainly due to impracticability of the navigational device.
The purpose of this study was the clinical evaluation of the first commercially available navigated transcranial magnetic stimulation (nTMS) system [25]. Three studies have been published so far, addressing the spatial resolution of this system. Picht et al. showed a close correlation of the results of preoperative mapping with nTMS and intraoperative DCS results [20]. Forster et al. and Krieg et al. compared DCS, nTMS, and fMRI in their spatial cortical resolution with promising results of nTMS [7, 12]. Both studies used navigation-based discrimination of two points defining hot spots for each method. This assessment suggests a high accuracy however hides a substantial rate of intrinsic errors. It compares volume-based assessment in fMRI with area-based assessment in DCS and nTMS using single points. DCS has a local cortical resolution of 10 mm within the gyrus, while it has a very precise intergyral resolution [27]. nTMS most likely has a very similar distribution concerning its mode of operation. Taking this into account, spatial resolution of the different techniques is not the key issue. Due to the different physical principles of fMRI and nTMS, it is most likely that both methods have different specifications and limitations. The aim of our study was to point out these factors in the clinical practice. We compared the accuracy of nTMS and fMRI in the gyral localization of the motor cortex in 30 consecutive cases. The results were correlated with the intraoperative DCS.
Patients and methods
Patients
From October 2010 to July 2011, all consecutive patients harboring a lesion within or adjacent to the primary motor cortex (e.g., the precentral gyrus) were prospectively enrolled in this study. Exclusion criteria included metal implants that interfere with MRI, an existing cardiac pacemaker or deep brain stimulation electrodes.
All patients underwent a MRI with a 3D magnetization-prepared rapid-acquired gradient echo (MP-RAGE) sequence as a data source for neuronavigation, together with a diffusion tensor imaging (DTI) for fiber tracking of the corticospinal tract and a fMRI (for specifications, see below).
Preoperative fMRI
The fMRI studies were performed on a 1.5 T Magnetom Sonata system (Siemens Medical Solutions, Erlangen, Germany). Structural two-dimensional (2D) T1-weighted data were acquired using a spin echo (5 mm) sequence (repetition time (TR), 618 ms; echo time (TE), 14 ms; 41 transverse slices; and field of view, 512 × 512 mm²).
fMRI was performed using a BOLD-sensitive echo planar imaging sequence (TR, 3470 ms; TE, 50 ms; 41 transverse slices; 0.75 mm gap; voxel size, 3 × 3 × 3 mm; and base resolution, 64 × 64) measured by 2D gradient echo–echo planar imaging.
Subjects were presented visually, projected on a screen mounted in front of the scanner in head-first supine patient’s position. A total of 121 scans were acquired while subjects performed three blocks of alternating movements of the tongue and flexion movements of the fingers and of the foot, each contralateral to the affected brain hemisphere (21 s/condition).
Data processing involved functional statistics by Inline BOLD Imaging (Siemens). Voxels with significant signal increase that correlated with the motor tasks were color coded. The threshold values for the single motor areas were adjusted by visual inspection. The functional areas were superimposed on the anatomical T1-weighted images and exported as DICOM files.
nTMS
nTMS was performed with the NBS System 4 (Nexstim, Helsinki, Finland), which is the first commercially available nTMS system [25]. NBS System 4 is equipped with an optical tracking system as a base for a noninvasive frameless neuronavigation, combined with a navigated figure of eight coil. The NBS System 4 system is connected to a computer interface for calculating the distribution of the electrical field depending on the individual anatomy and coil position (Fig. 1). Neuronavigation was based on the previously obtained MP-RAGE images. fMRI data were not included in the nTMS system in order to blind the examiner for the elicited functional results. The patient was registered in the nTMS neuronavigation system using the integrated protocol of surface and landmark registration. Electromyography (EMG) was recorded on tibialis anterior (TA), quadriceps femoris (QF), abductor pollices brevis (APB), first dorsal interosseus (FDI), and flexor carpi radialis (FCR). Resting motor threshold (RMT) was established using the protocol described by Säisänen et al. in 2008 [26]. Perilesional mapping was performed using 110 % of the RMT. Two pediatric patients were mapped in after motor activation, using the active motor threshold. Perilesional nTMS mapping was done with an approximate distance of stimuli of about 5 mm until the borders of the positive EMG response were reached (Fig. 2). Positive responses above RMT were integrated via DICOM import in the intraoperative neuronavigation software iPlan 2.0 (Brainlab, Feldkirchen, Germany), fused to the MP-RAGE images and exported to the OR.
Preoperative functional mapping with the navigated transcranial magnetic stimulation system. The left side shows the navigated MRI image with the above resting motor threshold responses of the perilesional area. The right side shows an MEP response of the APB, FDI, and flexor carpi radialis FCR at a stimulation intensity of 81 V/M at the displayed area
Assessment of preoperative accuracy
Accuracy of preoperative upper and lower extremity cortex representation area (UE and LE) localization of nTMS and fMRI was assessed with a grading system from 1 to 4 (Fig. 3). Grade 1 represents a distinct gyral localization, grade 2 a projection over the adjacent sulcus, and grade 3 a projection over the adjacent gyrus. Grade 4 characterizes an inability to localize the motor cortex. The ability of each evaluated method to preoperatively localize the central sulcus as well as the concordance of fMRI and nTMS for the same gyrus was assessed with categorical judgment (yes/no).
Schematic drawing of the rolandic area. The accuracy score is projected over the hand knob. Grade 1 represented a distinct gyral localization, grade 2 a projection over the adjacent sulcus, and grade 3 a projection over the adjacent gyrus. Grade 4 characterizes the inability to localize the motor cortex
Microsurgery
The surgical approach was individually planned according to the generally accepted principles of minimal invasiveness. The functional planning of the approach was based upon the fMRI and fiber tracking data. The extent of craniotomy and cortical exposure was limited to the requirements of a save tumor excision-making DCS possible only for the area at risk
Anesthesia
Total intravenous anesthesia with propofol and remifentanil was used in all cases. A short-acting muscle relaxant (atracurium) was used only for intubation.
DCS
DCS and phase reversal via a cortical strip electrode was performed for intraoperative cortical mapping in all cases. We conducted anodal cortical and cathodal subcortical stimulation with a 2-mm DCS probe, which was referenced in the neuronavigation system. EMG was recorded with paired subdermal needle electrodes, placed routinely in TA, QF, FDI, FCR, and APB. Short trains of five stimuli with a pulse width of 0.5 ms and an interstimulus interval of 4 ms at a repetition rate of 0.5 Hz were applied. Stimulation intensity was increased in steps of 1 mA with an upper intensity limit of 25 mA, until an EMG response was recorded. Neurophysiological intraoperativemonitoring was performed with a Nicolet Endeavour neuromonitoring system (Cardinal Health, Madison, WI).
Intraoperative documentation
Screenshots of the neuronavigation system and the neurophysiology system were documented if a positive motor response was elicited with DCS (Fig. 4). After surgery, two authors jointly assessed the correlation of fMRI and nTMS with the intraoperative DCS gyrus localization. DCS was used as final verification of location of motor cortex.
Statistics
Statistic calculations were done using SPSS 15. Statistical comparisons were performed using paired samples only. Thus, cases with data for only on methodology were excluded. Wilcoxon signed-rank test was used to compare the distribution of the nTMS and fMRI accuracy. Spearman’s rho was calculated for the correlation of preoperative paresis medical research council scale for muscle strength (MRC) scale and accuracy of nTMS and fMRI. A p value below 0.05 was defined as statistical significant. Decimal places were not calculated for percentages.
Ethical approval
The study was evaluated by the Baden–Wuerttemberg medical board ethics committee. Since all applied methods are considered to be part of a standard practice of care and since the data collected were assessed in retrospect, no ethics committee approval was considered necessary. In the context of this study, the authors undertook all possible efforts to follow the Declaration of Helsinki.
Results
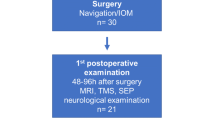
The NBS System 4 became available to us in October 2010. The first 30 consecutive patients with lesions in or adjacent to the primary motor cortex were enrolled in this study. No patient had to be excluded. Most common entities were astrocytoma (30 %), followed by metastasis (20 %) and meningioma (17 %) (Table 1). The patient’s age ranged from 2 to 76 years (median, 54 years). Ten patients (33 %) presented with a preoperative hemiparesis.
nTMS was feasible in all 30 cases. fMRI was impossible in 7 of 30 cases (23 %). In two patients, this was due to an impaired cooperation (dementia in case No. 1 and severe frontal lobe syndrome in case No. 11). Two patients were too young (age 2 and 3 years) to perform the motor paradigm (case No. 4 and 7). Two patients suffered from aphasia and apraxia (case No. 10 and 19) while one patient was hemiplegic (case No. 2), which rendered the motor task impossible (Table 2).
No adverse effects were related to nTMS. No epileptic fit was elicited with stimulation even with a patient suffering from frequent focal epileptic seizures.
Assessment of accuracy was performed in 23 patients using a paired sample comparison when both MRI and nTMS was feasible. The preoperative accuracy for the gyral localization of the UE motor area showed a mean score of 2.4 for nTMS, representing a mean localization with coverage of the adjacent sulcus and a mean score of 2.8 for fMRI which represents a mean projection over the adjacent gyrus. For the LE motor cortex, there was a mean score of 2.1 for nTMS and 2.8 for fMRI (Table 3). No statistically significant difference was seen between both distributions in the Wilcoxon signed-rank test. A tendency towards a statistical significant difference was found in the accuracy scores of nTMS and fMRI of the LE localization with a two tailed significance of p = 0.061. After performing a subgroup analysis of gliomas, we found a significant higher accuracy score in nTMS than in fMRI of LE with a p value of 0.031. The difference of mean scores of UE was higher too, however reached no statistical significance (Table 4).
A distinct gyral localization of the primary motor cortex, representing grade 1, was observed in 23 % of the patients with nTMS while fMRI allowed gyral localization in 13 % only. On the other hand, there was an inability to localize UE motor cortex (grade 4) in 22 % of patients with fMRI versus 7 % of cases with nTMS. LE motor cortex localization was distinct in 18 % with nTMS while there was no grade 1 LE motor cortex identification with fMRI. fMRI failed to localize the motor cortex in 24 % of the patients, which was not encountered with nTMS (Fig. 5).
There was no significant correlation of preoperative paresis and the accuracy score in Spearman’s rho.
The preoperative localization of the central sulcus was possible in all cases with nTMS. Localization of central sulcus was not possible in 5 of 23 cases (22 %) with preoperative fMRI. Both methods yielded concordant results for the localization of the central sulcus in 84 %.
Intraoperative verification of the motor cortex localization with DCS was not feasible due to limited surgical exposure in 7 patients for the UE and in 13 patients for the LE. In five patients, no intraoperative DCS could be performed. One of the cases was a stereotactic biopsy in the central region. The other four cases were patients with frontal lesions bordering the precentral gyrus. Surgical exposure was limited by the surgeon to expose only the tumor reaching the cortical surface rendering a DCS verification impossible. Verification of the central sulcus was performed with a grid electrode using phase reversal. These cases were not included as intraoperative verification of nTMS or fMRI. A verification of the nTMS findings of the motor cortex localization with DCS was seen in all eligible patients for both UE (n = 23) and LE (n = 17). The fMRI localization of the hand area turned out to be postcentral with intraoperative DCS verification in one out of 17 cases (6 %). All fMRI localizations for LE motor cortex were confirmed by DCS (n = 9).
Postoperative, one patient showed a slight deterioration of the UE motor score. All other patients improved or stayed at the same MRC motor scale (Table 2). In the subgroup of intrinsic tumors in 5 of 15 patients, a subtotal resection was performed due to the eloquent intraoperative neurophysiological findings. All extra-axial lesions were resected completely.
Illustrative case (No. 26)
nTMS in a patient with an incidential rolandic arteriovenous malformation
A 64-year-old man fell from a height and was unconscious for some minutes. The patient was admitted to the hospital with a GCS of 14. On initial neuroexam, he had no abnormal findings. A CT-Scan demonstrated a subarachnoid hemorrhage in the right sylvian fissure. To rule out an aneurysmatic subarachnoid hemorrhage, we performed an MRI scan with MRI angiography. A small central AVM unrelated to the bleeding was found (Fig. 6a, b). A digital subtraction angiography (DSA) confirmed a Spetzler–Martin grade II AVM (Fig. 6c, d). In our interdisciplinary neurosurgical and neuroradiological conference, we indicated to operate on the lesion after full recovery of the patient.
For preoperative planning an fMRI was performed. The BOLD sequence showed a very precise localization of the LE cortical representation (Fig. 7). However, no conclusive results were found for UE due to the high flow in the cortical venous drainage adjacent to the hand knob in the precentral gyrus. Preoperative nTMS showed a precise gyral localization of the hand and leg area (Fig. 2). Intraoperatively, the localization could be confirmed via DCS and phase reversal (Fig. 4). The AVM was resected with continuous neurophysiological monitoring with MEP and repeated DCS. No decrease of the potentials was seen during surgery. Intraoperative indocyanine green angiography showed complete resection. A conventional DSA on postoperative day 1 confirmed the result.
The patient showed no neurological compromises at discharge.
Discussion
Identifying central sulcus prior to operate on a rolandic lesion is crucial for the neurosurgeon. Even though localization of the central sulcus is possible using anatomical landmarks in most cases, it has been shown that preoperative functional mapping with fMRI enhances accuracy [3, 14]. In modern neurosurgery, functional imaging with fMRI is part of the common practice of care for most neurosurgeons prior to performing surgery in eloquent brain regions. fMRI helps to understand the extent of tumor invasion into functional areas and the eventual displacement of eloquent cortex. It also decreases the patient’s risk for functional impairment after surgery and minimizes the required cortical exposure [18, 24, 28].
With the widespread use of a technology, drawbacks and limitation become apparent. fMRI detects neuronal activation indirectly via the increase of blood flow induced by a specific function, tested in a “paradigm.” The execution of a specific function results in an activation of all related cortical areas. The “functional” image, which is derived from the statistics of the effects of activation versus resting, depends on a threshold set by an investigator. It uses the cortical hemodynamic changes as a surrogate marker for neuronal activity.
For intraoperative neurophysiological mapping in a complex case, several methods are combined to overcome their particular limitations in order to provide an identification of the tissue at risk as accurate as possible. Preoperative functional diagnostic mainly relies on fMRI. In our experience nTMS represents the most promising tool to complement preoperative fMRI for motor cortex localization. It combines the well-established TMS method with the accuracy of a navigation system. It enables noninvasive mapping of the cortical function comparable to intraoperative DCS. We think it is important to overcome each method’s limitation in a combined use of different tools. Due to the different physical principles of fMRI and nTMS, it is most likely that both methods have different specifications and limitation. In our study, we pointed out these factors in the clinical practice.
In this comparative study, it was shown that in a clinical routine setting, there are fewer restrictions for nTMS than for fMRI. nTMS requires only a minimum level of compliance. Aphasic patients and those suffering from dementia or severe frontal lobe syndrome are hardly able to perform a specific fMRI motor paradigm but can be examined accurately with nTMS. In pediatric patients, nTMS might be the only option for preoperative functional testing. Cooperation with the fMRI motor paradigm is often demanding. The youngest patient with a valuable result in an fMRI study focused on presurgical mapping was 5 years old [29]. An alternative is the use of passive range-of-motion testing in sedated children. Children not younger than 3 years could be tested in the fMRI with this method. However, no activation correlate was seen for paretic extremities [16]. TMS is a save and well-accepted diagnostic method in pediatric patients, mostly used for examining maturation, neuronal plasticity, or in epilepsy diagnostics [23]. Eliciting nTMS evoked potentials in principle is applicable even in newborns [6]. Due to immature myelination, high stimulation intensity is needed. Below an age of 3 years, stimulation intensity is usually at a level of 100 % and EMG potentials can often only be elicited after motor activation, which was also the case in our pediatric patients [5]. Additionally, the mapping of rolandic AVMs is a favorable application for nTMS. As seen in the illustrative case, even small AVM are disturbing local blood flow extensively, making reliable fMRI impossible. Reported cases in the literature are supporting our findings [9]. The direct stimulation with nTMS to detect eloquent cortex eliminates this issue.
In our series, we report one case were we demonstrated the localization of the motor cortex in a hemiplegic patient. In this case, the patient was harboring a suspected metastasis with compression of the precentral gyrus. Even in extra-axial lesion we think it is very important to localize motor cortex preoperatively since patients have a high potential of recovery after complete removal of lesion and decrease of perifocal edema. Thus, the approach can be planned according to the expected areas at risk. nTMS is an ideal supplement to DTI in such a case. In general, it might help to identify the region of interest for fiber tracking of the corticospinal tract more precisely. Further studies are needed to identify the role of the method in this regard. The patient in our series recovered and was discharged with a hemiparesis of two for UE and three out of five on the MRC scale.
The comparison of the accuracy scores as shown in Fig. 3 demonstrated a higher number of distinct localizations in nTMS both for UE and LE while the rate of nonlocalizations was lower. The mean scores for UE and LE accuracy were lower in nTMS than in fMRI, without reaching statistical significance. This might be due to the small number of cases with a high variance of data in this study. The significant results in the subgroup of axial tumors for LE are most promising since this is the scope of the application in the clinical use. In a clinical setting, the preoperative localization of the central sulcus is crucial information for the planning of the tumor approach. fMRI failed to localize the central sulcus in five patients (24 %). The seven patients in whom an fMRI was not feasible from the start are excluded. Without the use of nTMS, we would not have had preoperative functional information in 12 out of 30 cases (40 %).
DCS was able to confirm the gyral localization of nTMS in all patients. In one patient of this series, fMRI localized the motor cortex in a misleading way to the postcentral gyrus. This carries a certain risk for the patient or might at least require an intraoperative revision of the surgical approach. A study comparing the accuracy of MEG and fMRI even showed 4 of 15 cases with a false postcentral localization of the motor cortex in fMRI [11].
Most observations of a close correlation of fMRI and intraoperative neurophysiology refer to patients with a normal anatomy of the rolandic cortex. A study of Lehericy et al. in 120 patients shows a concordance of fMRI and DCS in 92 % [14]. Studies assessing rolandic tumors describe a correct localization of the central sulcus with fMRI in only 65–80 % of the patients [11, 13, 22]. The accuracy of our fMRI examinations are above the reported average, which emphasizes the positive results of the nTMS technique for preoperative functional planning.
The intraoperative verification of fMRI and nTMS by DCS, which is considered to be the gold standard, was limited due to the minimal invasive surgical approach. Planning of the approach for all patients was performed as if no intraoperative evaluation of the nTMS method was performed. For truly confirming the localization of the nTMS potentials, a direct exposure of the hand or leg area is mandatory. In many cases, this is not necessary for safe resection of the lesion. Therefore, no areas of the central sulcus that did not need to be inspected were exposed (e.g., the leg area in a lesion bordering the hand knob). A thorough intraoperative neurophysiological mapping was performed using grid electrodes and subcortical mapping additionally to DCS in all cases. However, the results of these tests were not included in the study. In approximately one third of the patients, an exposure of the entire motor cortex was not necessary to safely remove the tumor.
This is the largest published study on nTMS for preoperative planning of rolandic tumor surgery. Two case reports have been published, demonstrating that nTMS can be performed in severely paretic and incompliant patients, not suitable for fMRI [4, 21]. Our series shows the limitations of fMRI for an unselected clinical cohort of patients with tumors of the rolandic region. These restrictions can be overcome by nTMS. Picht et al. compared nTMS with DCS in 20 patients and found a mean distance of the hotspots of 7.07 mm [17]. The recently published series of Krieg et al. comparing nTMS and fMRI in 14 patients with rolandic tumors and 12 patients with tumors in the subcortical white matter showed a good correlation of nTMS and DCS with 4.4 mm and a much higher deviation of fMRI and nTMS with 9 to 15 mm. No significant differences could be found for both techniques [12]. There is only one series by Foerster et al., which compared fMRI and nTMS with intraoperative DCS in ten patients [7]. Their data suggest a higher correlation of nTMS and DCS with a mean distance of 10.5 mm in contrast to 15.03 mm for DCS and fMRI, without reaching significance. Given the fact that the spatial resolution of DCS is 10 mm within a gyrus and a confined stimulation of one muscle is hardly possible, it seems very difficult to evaluate the clinical use of nTMS with respect to spatial cortical resolution. A distance of 10 mm in the rolandic area can be crucial for eloquent tissue. Additionally, a high error rate is found when comparing a volume-based method like BOLD MRI and area-based methods like nTMS and DCS with single-point discrimination. We therefore used the above-described accuracy score, even though there might be an additional rater bias, since it takes the local gyral architecture into account and hence provides clinically valuable information about the method.
The presented data suggest that nTMS is a promising tool for the preoperative functional mapping of the motor cortex. The precision to localize motor cortex seems to be high, although further studies with larger number of patients are needed to evaluate accuracy more in detail. nTMS is easy to use in the clinical routine setting. A nTMS examination takes about 20–30 min. The examiner bias and the risk of false-positive results due to overstimulation are low since a standardized method to establish RMT is used. A medical technical assistant can perform preoperative nTMS examinations as part of a standard practice of care. Despite these advantages, nTMS presently cannot replace preoperative fMRI and preoperative identification of subcortical pathways with diffusion tensor imaging-MRI (DTI-MRI). fMRI remains the only available option for preoperative language mapping so far. It is a future perspective to develop reliable language mapping based on nTMS. Technically, language mapping similar to awake craniotomy is possible [15]. However, establishing adequate stimulation intensity and frequency remains difficult since a standardized protocol like for RMT does not yet exist.
Conclusions
nTMS has fewer restrictions for preoperative functional mapping of the motor cortex than fMRI. A low level of compliance is required. It represents the only option for preoperative functional motor cortex assessment of patients that cannot perform the motor paradigm of fMRI (e.g., pediatric, demented, and hemiplegic patients). No adverse effects were encountered in our first 30 nTMS patients. The cortical spatial resolution of nTMS is more precise than of fMRI. nTMS represents a highly valuable tool for preoperative functional planning in the clinical routine. It can complement or eventually replace fMRI for preoperative motor cortex mapping. Future studies with a larger number of patients are needed to evaluate accuracy more in detail.
References
Bittar RG, Olivier A, Sadikot AF, Andermann F, Reutens DC (2000) Cortical motor and somatosensory representation: effect of cerebral lesions. J Neurosurg 92(2):242–248. doi:10.3171/jns.2000.92.2.0242
Boroojerdi B, Foltys H, Krings T, Spetzger U, Thron A, Topper R (1999) Localization of the motor hand area using transcranial magnetic stimulation and functional magnetic resonance imaging. Clin Neurophysiol 110(4):699–704
Campero A, Ajler P, Martins C, Emmerich J, de Alencastro LF, Rhoton A Jr (2011) Usefulness of the contralateral omega sign for the topographic location of lesions in and around the central sulcus. Surg Neurol Int 2:164
Coburger J, Musahl C, Weissbach C, Bittl M (2011) Navigated transcranial magnetic stimulation-guided resection of a left parietal tumor: case report. Minim Invasive Neurosurg 54(1):38–40. doi:10.1055/s-0031-1273732
Eyre JA, Miller S, Ramesh V (1991) Constancy of central conduction delays during development in man: investigation of motor and somatosensory pathways. J Physiol 434:441–452
Fietzek UM, Heinen F, Berweck S, Maute S, Hufschmidt A, Schulte-Monting J, Lucking CH, Korinthenberg R (2000) Development of the corticospinal system and hand motor function: central conduction times and motor performance tests. Dev Med Child Neurol 42(4):220–227
Forster MT, Hattingen E, Senft C, Gasser T, Seifert V, Szelenyi A (2011) Navigated transcranial magnetic stimulation and functional magnetic resonance imaging—advanced adjuncts in preoperative planning for central region tumors. Neurosurgery 68:1317–1324. doi:10.1227/NEU.0b013e31820b528c
Giussani C, Roux FE, Ojemann J, Sganzerla EP, Pirillo D, Papagno C (2010) Is preoperative functional magnetic resonance imaging reliable for language areas mapping in brain tumor surgery? Review of language functional magnetic resonance imaging and direct cortical stimulation correlation studies. Neurosurgery 66(1):113–120. doi:10.1227/01.neu.0000360392.15450.c9
Juenger H, Ressel V, Braun C, Ernemann U, Schuhmann M, Krageloh-Mann I, Staudt M (2009) Misleading functional magnetic resonance imaging mapping of the cortical hand representation in a 4-year-old boy with an arteriovenous malformation of the central region. J Neurosurg Pediatr 4(4):333–338. doi:10.3171/2009.5.peds08466
Kantelhardt SR, Fadini T, Finke M, Kallenberg K, Siemerkus J, Bockermann V, Matthaeus L, Paulus W, Schweikard A, Rohde V, Giese A (2010) Robot-assisted image-guided transcranial magnetic stimulation for somatotopic mapping of the motor cortex: a clinical pilot study. Acta Neurochir (Wien) 152(2):333–343. doi:10.1007/s00701-009-0565-1
Korvenoja A, Kirveskari E, Aronen HJ, Avikainen S, Brander A, Huttunen J, Ilmoniemi RJ, Jaaskelainen JE, Kovala T, Makela JP, Salli E, Seppa M (2006) Sensorimotor cortex localization: comparison of magnetoencephalography, functional MR imaging, and intraoperative cortical mapping. Radiology 241(1):213–222. doi:10.1148/radiol.2411050796
Krieg SM, Shiban E, Buchmann N, Gempt J, Foerschler A, Meyer B, Ringel F (2012) Utility of presurgical navigated transcranial magnetic brain stimulation for the resection of tumors in eloquent motor areas. J Neurosurg 116(5):994–1001. doi:10.3171/2011.12.JNS111524
Lee CC, Ward HA, Sharbrough FW, Meyer FB, Marsh WR, Raffel C, So EL, Cascino GD, Shin C, Xu Y, Riederer SJ, Jack CR Jr (1999) Assessment of functional MR imaging in neurosurgical planning. AJNR Am J Neuroradiol 20(8):1511–1519
Lehericy S, Duffau H, Cornu P, Capelle L, Pidoux B, Carpentier A, Auliac S, Clemenceau S, Sichez JP, Bitar A, Valery CA, Van Effenterre R, Faillot T, Srour A, Fohanno D, Philippon J, Le Bihan D, Marsault C (2000) Correspondence between functional magnetic resonance imaging somatotopy and individual brain anatomy of the central region: comparison with intraoperative stimulation in patients with brain tumors. J Neurosurg 92(4):589–598. doi:10.3171/jns.2000.92.4.0589
Lioumis P, Zhdanov A, Makela N, Lehtinen H, Wilenius J, Neuvonen T, Hannula H, Deletis V, Picht T, Makela JP (2012) A novel approach for documenting naming errors induced by navigated transcranial magnetic stimulation. J Neurosci Methods 204(2):349–354
Ogg RJ, Laningham FH, Clarke D, Einhaus S, Zou P, Tobias ME, Boop FA (2009) Passive range of motion functional magnetic resonance imaging localizing sensorimotor cortex in sedated children. J Neurosurg Pediatr 4(4):317–322. doi:10.3171/2009.4.peds08402
Penfield W, Jasper H (1954) Epilepsy and the functional anatomy of the human brain. Little, Brown & Co, Boston
Petrella JR, Shah LM, Harris KM, Friedman AH, George TM, Sampson JH, Pekala JS, Voyvodic JT (2006) Preoperative functional mr imaging localization of language and motor areas: effect on therapeutic decision making in patients with potentially resectable brain tumors1. Radiology 240(3):793–802
Picht T, Mularski S, Kuehn B, Vajkoczy P, Kombos T, Suess O (2009) Navigated transcranial magnetic stimulation for preoperative functional diagnostics in brain tumor surgery. Neurosurgery 65(6 Suppl):93–98. doi:10.1227/01.NEU.0000348009.22750.59, discussion 98–99
Picht T, Schmidt S, Brandt S, Frey D, Hannula H, Neuvonen T, Karhu J, Vajkoczy P, Suess O (2011) Preoperative functional mapping for rolandic brain tumor surgery: comparison of navigated transcranial magnetic stimulation to direct cortical stimulation. Neurosurgery 69(3):581–588. doi:10.1227/NEU.0b013e3182181b89
Picht T, Schmidt S, Woitzik J, Suess O (2011) Navigated brain stimulation for preoperative cortical mapping in paretic patients: case report of a hemiplegic patient. Neurosurgery 68(5):E1475–E1480. doi:10.1227/NEU.0b013e318210c7df
Pirotte B, Neugroschl C, Metens T, Wikler D, Denolin V, Voordecker P, Joffroy A, Massager N, Brotchi J, Levivier M, Baleriaux D (2005) Comparison of functional MR imaging guidance to electrical cortical mapping for targeting selective motor cortex areas in neuropathic pain: a study based on intraoperative stereotactic navigation. AJNR Am J Neuroradiol 26(9):2256–2266
Quintana H (2005) Transcranial magnetic stimulation in persons younger than the age of 18. J ECT 21(2):88–95
Roux FE, Ranjeva JP, Boulanouar K, Manelfe C, Sabatier J, Tremoulet M, Berry I (1997) Motor functional MRI for presurgical evaluation of cerebral tumors. Stereotact Funct Neurosurg 68(1–4 Pt 1):106–111
Ruohonen J, Karhu J (2010) Navigated transcranial magnetic stimulation. Neurophysiol Clin 40(1):7–17. doi:10.1016/j.neucli.2010.01.006
Saisanen L, Julkunen P, Niskanen E, Danner N, Hukkanen T, Lohioja T, Nurkkala J, Mervaala E, Karhu J, Kononen M (2008) Motor potentials evoked by navigated transcranial magnetic stimulation in healthy subjects. J Clin Neurophysiol 25(6):367–372. doi:10.1097/WNP.0b013e31818e7944
Schiffbauer H, Berger MS, Ferrari P, Freudenstein D, Rowley HA, Roberts TP (2002) Preoperative magnetic source imaging for brain tumor surgery: a quantitative comparison with intraoperative sensory and motor mapping. J Neurosurg 97(6):1333–1342. doi:10.3171/jns.2002.97.6.1333
Schulder M, Maldjian JA, Liu WC, Holodny AI, Kalnin AT, Mun IK, Carmel PW (1998) Functional image-guided surgery of intracranial tumors located in or near the sensorimotor cortex. J Neurosurg 89(3):412–418. doi:10.3171/jns.1998.89.3.0412
Shurtleff H, Warner M, Poliakov A, Bournival B, Shaw DW, Ishak G, Yang T, Karandikar M, Saneto RP, Browd SR, Ojemann JG (2010) Functional magnetic resonance imaging for presurgical evaluation of very young pediatric patients with epilepsy. J Neurosurg Pediatr 5(5):500–506. doi:10.3171/2009.11.peds09248
Stippich C, Kress B, Ochmann H, Tronnier V, Sartor K (2003) Preoperative functional magnetic resonance tomography (FMRI) in patients with rolandic brain tumors: indication, investigation strategy, possibilities and limitations of clinical application. Rofo 175(8):1042–1050. doi:10.1055/s-2003-40920
Ulmer JL, Hacein-Bey L, Mathews VP, Mueller WM, DeYoe EA, Prost RW, Meyer GA, Krouwer HG, Schmainda KM (2004) Lesion-induced pseudo-dominance at functional magnetic resonance imaging: implications for preoperative assessments. Neurosurgery 55(3):569–579, discussion 580–561
Zhang D, Johnston JM, Fox MD, Leuthardt EC, Grubb RL, Chicoine MR, Smyth MD, Snyder AZ, Raichle ME, Shimony JS (2009) Preoperative sensorimotor mapping in brain tumor patients using spontaneous fluctuations in neuronal activity imaged with functional magnetic resonance imaging: initial experience. Neurosurgery 65(6 Suppl):226–236. doi:10.1227/01.neu.0000350868.95634.ca
Acknowledgments
We thank Claudia Weissbach and Klarissa Belicke for performing neurophysiological recordings with outstanding motivation and enthusiasm.
Disclosure
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Hugues Duffau, Montpellier, France
The authors compared navigated transcranial magnetic stimulation (nTMS) with preoperative functional magnetic resonance imaging (fMRI) and intraoperative direct cortical stimulation (DCS) to identify the primary motor cortex in a consecutive series of patients who underwent surgery for a lesion near or within the central region. They found that the cortical spatial resolution of nTMS was higher than of fMRI. Moreover, verification of nTMS motor cortex localization with DCS was achieved in all cases.
A very important message in this article is that nTMS was feasible in all cases, contrary to fMRI which was impossible in seven patients. Thus, preoperative nTMS may represent an interesting alternative to fMRI in pediatric, demented, or hemiplegic patients.
However, it is worth noting that, in this series, there were no significant differences between fMRI and nTMS. Therefore, the authors have to be cautious before to claim that the cortical spatial resolution of nTMS is higher than of fMRI, because this conclusion is not yet validated by their data. In addition, when Coburger et al. compared nTMS with DCS, they wrote that DCS had a cortical resolution of 10 mm within the gyrus, and that nTMS most likely had a very similar distribution. It is not totally true. Indeed, in glioma surgery, it was demonstrated that the combination of direct subcortical stimulation of the white matter pathways with DCS increased the spatial resolution, allowing an optimization of the resection until functional tracts have been encountered, with no margin [1, 2]. As a consequence, one should be aware about the impossibility for nTMS to perform subcortical mapping—which represents a main limitation in surgery for intra-axial brain tumor. This is the reason why it is dangerous to claim that “technically language mapping (using nTMS) similar to awake craniotomy is possible”, due to the fact that neural foundations of language are constituted by a subcortical connectivity which should absolutely be mapped and preserved intraoperatively because not able to be compensated when damaged [3, 4]. For all these reasons, intrasurgical direct electrical mapping remains the gold standard in glioma surgery, as recently demonstrated in a meta-analysis with more than 8,000 tumors [5].
References
1. Duffau H, Gatignol P, Mandonnet E, Capelle L, Taillandier L (2008) Intraoperative subcortical stimulation mapping of language pathways in a consecutive series of 115 patients with grade II glioma in the left dominant hemisphere. J Neurosurg 109:461–471
2. Gil Robles S, Duffau H (2010) Surgical management of World Health Organization Grade II gliomas in eloquent areas: the necessity of preserving a margin around functional structures? Neurosurg Focus 28(2):E8
3. Duffau H (2009) Does post-lesional subcortical plasticity exist in the human brain? Neurosci Res 65:131–135
4. Ius T, Angelini E, Thiebaut de Schotten M, Mandonnet E, Duffau H (2011) Evidence for potentials and limitations of brain plasticity using an atlas of functional resectability of WHO grade II gliomas: towards a “minimal common brain”. Neuroimage 56:992–1000
5. De Witt Hamer PC, Gil Robles S, Zwinderman AH, Duffau H, Berger MS (2012) Impact of intraoperative stimulation brain mapping on glioma surgery outcome: a meta-analysis. J Clin Oncol (in press)
Matthias Krammer, Christianto B. Lumenta, Munich, Germany
This article is a good amendment to the existing literature dealing with the new method of navigated transcranial magnetic stimulation (nTMS) in comparison to functional MRI in patients with tumors in the rolandic area.
There are only few articles that describe the method of nTMS itself already.
The authors compare the two methods in 30 patients with very different benign and malignant tumors and vascular lesions. We think this is tolerable in such a paper that introduce a new method and is even necessary for further investigations. There exists up to date no articles with a bigger patient group. One problem is that it was not possible to perform fMRI in seven patients (23 %) due to compliance or other problems. This is a well-known problem of this method but makes statistical statements comparing the two methods in a patient group with 30 cases questionable.
The authors report about a patient where the fMRI showed the motor hand area postcentral and concluded that this is an error. According to the intraoperative control performed in this study with negative direct cortical stimulation this is really a false-positive localization. Kombos et al. (Acta Neurochir 799 (Wien) (1999) 141: 1295–1301) identified true functional motor areas 800 in the postcentral parietal location using direct monopolar and bipolar 801 stimulation results in 7.85 % few cases.
The authors report further about identification of the motor cortex even in hemiplegic patients. Do we look forward to get an improvement after tumor resection? This could be possible in our opinion in a hemiparetic patient and in hemiplegic patients with motor function improvement after antiedematous therapy, but in really hemiplegic patients? Is the surgical procedure in this case the same for infiltrating tumors in comparison to, e.g., meningioma? Do the authors stop tumor resection in a true hemiplegic patient with a glioblastoma when they reach the identified motor cortex and there is still vital and visible tumor?
Although it is not part of this study, we think that the most important tools for surgery in the rolandic area are the neurophysiological methods looking for the central sulcus with the phase reversal, direct cortical, and subcortical stimulation. Independent from the cortical localization of a tumor, it is also important during the resection to save the subcortical pathways. In opposite to nTMS, subcortical pathways could be identified by fMRI and MRI-DTI. A good new method is the combination of nTMS and DTI using the nTMS motor cortex region as starting point for the DTI generation.
Christopher Nimsky, Marburg, Germany
Preoperative functional mapping is an important part of preoperative planning and decision making in lesions close to eloquent brain areas. Magnetoencephalography (MEG) and functional magnetic resonance imaging (fMRI) were among the first techniques to identify these eloquent brain areas. Despite having different physical principles being the bases of these methods, a quite reliable identification of the motor cortex or language-related areas is possible. fMRI has the advantage to be widely available; however, the method is not able to identify the proper structures in all cases, so some groups prefer to combine the results of fMRI and MEG. The authors demonstrate the application of navigated transcranial magnetic stimulation (nTMS) and could show that it had fewer restrictions than fMRI in their series to identify the motor cortex. So potentially nTMS might also be an alternative for MEG, which is measuring the electrical activity directly, in contrast to fMRI measuring oxygen consumption. It will be interesting to see, whether nTMS will also be able to localize speech relevant areas, which might be even more interesting in a clinical setting.
Rights and permissions
About this article
Cite this article
Coburger, J., Musahl, C., Henkes, H. et al. Comparison of navigated transcranial magnetic stimulation and functional magnetic resonance imaging for preoperative mapping in rolandic tumor surgery. Neurosurg Rev 36, 65–76 (2013). https://doi.org/10.1007/s10143-012-0413-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-012-0413-2