Abstract
Chordomas are extremely rare tumours. They arise in the spheno-occipital region in 35% of cases. Chordomas usually present benign histopathological features but often exhibit a malignant clinical behaviour. Radical surgical removal and high-dose radiation therapy seem to be effective in tumour control and to improve survival rate. Despite the advancements in microsurgical techniques and the development of radiation therapies, clival chordomas still represent a challenge. Nevertheless it appears that chordomas that have been resected to the same extent and that received post-operative radiotherapy might exhibit different rates of regrowth. This result supports the hypothesis that the recurrence rate of chordomas might be dependent on biological variables other than the extent of resection and the post-operative radiotherapy. Genetic and molecular studies on oncogenesis of chordomas are still limited, but they represent the basis for the development of molecular targeted therapies. We present a review of the current knowledge about skull base chordomas biology, therapeutic options and related clinical outcome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chordomas are rare midline primary bone tumours arising from notochord remnants [18]. They have an incidence of 1 in 2 million, a prevalence of 1.21 in 10 million of the population, and constitute only 0.1% to 0.2% of all cranial base tumours [74]. Clinical malignancy of chordomas is related to local invasiveness, tendency of recurrence and potential to metastasize.
Prognosis is poor [25]. In case of untreated lesion, patients live between 6 and 24 months [39]. In treated patients the reported 5-year survival rate ranges from 50% to 85% [16, 17]. Management modalities in the treatment of skull base chordomas are surgery and high-dose radiotherapy (RT). Nevertheless the best treatment strategy is still controversial in terms of aim of surgery and type, indications, and timing of radiation therapy.
Major role in the treatment of chordomas is played by surgery [1, 44, 74, 85]. Aggressive excision provides long-term tumour control, but it is associated with high mortality and morbidity rate [64]. An important role in the management of these tumours is played by high-dose radiation therapies, which increase tumour control rate [4, 13, 36, 74]. Radiosensitivity of chordomas is limited in the 70–80-Gy dose range. The most common delivery methods include charged particle followed by stereotactic radiosurgery [5, 36, 57, 88].
Extent of resection and adjuvant radiation therapies are thought to influence the prognosis [17]. It also appears, however, that chordomas that have been resected to the same extent and that received post-operative radiotherapy might exhibit different rates of regrowth. This result supports the hypothesis that the recurrence rate of chordomas might be dependent on other variables. Molecular and genetic studies have been performed and reported in the literature to correlate biological markers with the clinical outcome. We review the current therapeutic options in skull base chordomas emphasizing the role of novel molecular markers as prognostic factors and as potential target for new biological therapies.
Definition
Chordomas are rare midline primary bone tumours arising from notochord remnants [18]. Remnants of primitive notochord may be found in the clival bone marrow, accounting for the prevalent extradural location of most chordomas [88]. They arise in the spheno-occipital region in 35% of cases [33]. Other locations are the sacro-coccygeal region in 55% of cases and the vertebral column in the remaining 10% of cases [11].
Primary intradural lesions have also been reported, but they are rare [27, 28, 57, 89, 91, 92]. Roberti and colleagues emphasized the therapeutic significance of the diagnostic differentiation between intradural chordomas and benign notochord remnants. They are extremely rare, benign lesions involving the midline cranial base. Giant ecchondrosis is detected in 5% of autopsies and is prevalently located in the prepontine region. They present a better clinical outcome, requiring after surgery only radiological and clinical follow-up. Examination of MIB-1 facilitates differential diagnosis [71].
Epidemiology
Chordomas constitute 0.1% to 0.2% of all cranial base tumours [1, 27, 74, 77] with a prevalence of 1.21 in 10,000,000 of the population [18] and an incidence of 1/2,000,000 per year. Fewer than 5% of chordomas arise in children [1, 8, 16]. There is male predilection with an M/F ratio of 2/1 [16, 51, 58]; mean age of patients with chordomas is 36.9 years [16–18, 28]. The average age of symptoms onset reported by Samii et al., Al-Mefty and Borba, Heffelfinger et al. and Stuer et al. is 38.3 years [1, 32, 74, 85], significantly lower than that reported by Crockard et al. (58.1 years) [18].
Chordomas arise predominantly in the sacro-coccygeal and cranial base areas [17, 25, 58, 88]. Chordomas, which arise in the spheno-occipital region, account for 35% of cases [33].
Radiological patterns
MRI imaging represents the main diagnostic modality for clival chordomas. On short repetition time/short echo time images, they present a low-to-intermediate signal. On long TR (long TE images), they have a very high signal [24]. Some degree of contrast enhancement has been also demonstrated [48]. CT appearance of clival chordomas demonstrated bone destruction with a soft tissue mass and varying degrees of enhancement on the adjacent brain. Other findings are contrast enhancement, soft tissue calcification and areas of low attenuation [47, 48]. The F-18 fluorodeoxyglucose (FDG) PET/CT showed a large destructive mass with associated erosion. Increased uptake of FDG is heterogeneous. Diagnosis of chordoma has to be considered if there is a large osteolytic mass with hypermetabolism on FDG PET/CT [65].
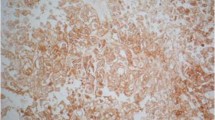
Histopathology
Chordomas appear as encapsulated multilobular lesions but infiltrate surrounding bone along lines of least resistance. Colour is reddish, and consistence is usually gelatinous soft but sometimes it is very firm like a cartilage [17]. The histology is typical, with areas of cartilage or bone destruction and bubble-like or “physaliphorous” cells [73, 88]. A variant of chordoma called the “chondroid chordoma” is recognised with features resembling chondrosarcoma [9, 73, 88]. Microscopically they present foci of chordoma mixed with a large cartilaginous matrix [32]. Although some series have reported a better long-term outcome in patients harbouring chondroid chordoma, this was not borne out in other series [1, 4, 28, 51, 88]. On immunohistochemistry, chordomas stain positively for S100, vimentin, epithelial membrane antigen, and cytokeratins (CK) 8/18. They also express other CKs, such as CK 1/10, CK 7, CK 20, CK 19 and CK 12 to 17 [88].
Biological behaviour and natural history
Clinical malignancy of chordomas is related to local invasiveness, tendency of recurrence and potential to metastasize. They have two distinct biological behaviours. Majority of tumours belong to the first group; they are slow growing lesions and, in rare cases, may not even grow at all. The tumour remains locally confined rather than metastasize to other areas [3, 17, 20, 88]. The second group has a more aggressive behaviour, with rapid local recurrence spread to other areas of the neuroaxis or metastasis to the lung, liver or bone [88]. Some primary tumours and many post-radiation recurrent tumours behave in a more aggressive fashion [34, 43, 88].
Prognosis of patients harbouring chordomas is poor. Eriksson et al. reported a series of 14 patients harbouring skull base chordomas. Patients who did not undergo surgery were dead within 18 months. In cases in which biopsy alone was performed, there was a life expectancy of 1.5 years [18, 25]. Menezes et al. estimated instead an average survival for patients with untreated chordomas being 28 months after the onset of symptoms [17, 46]. Kamrin et al. reported an average survival for untreated patients ranging from 6 to 24 months [39].
Clinical presentation
Patients usually complain headache and double vision due to one or more cranial nerve deficit at clinical onset. The first sign of the disease is usually an isolated abducent nerve palsy: in 46% of cases according to Volpe et al. [74, 89], 57% according to Forsyth et al. [27, 74], 90% according to Heffelfinger et al. [32, 74] and 47% in the series reported by Samii and colleagues [74].
This may be explained by the location and growth pattern of the tumours. Incidence of headache and double vision as presenting symptoms in patients harbouring clival chordoma are summarized in Table 1 [1, 16–18, 27, 64, 74]. At first clinical evaluation, the most physical findings are sixth nerve palsy, visual filed defect, extraocular motility defect due to other cranial nerve deficits, loss of visual acuity and lower cranial nerve palsy as shown in Table 2 [1, 16–18, 27, 64, 74].
Treatment philosophies
There are three different philosophies regarding the treatment of chordomas: aggressive surgical resection with radiotherapy given only in patients who have remnants, aggressive resection followed by radiotherapy given regardless the presence of remnants and partial resection followed by radiotherapy [88]. Crockard et al. have followed the policy of aggressive surgical resection and no radiotherapy unless distinct remnants remain [18, 88]. Al-Mefty administered radiotherapy to all patients postoperatively, regardless of resection [1, 88]. Application of radiotherapy as adjuvant treatment in the multimodal management of chordomas is still debated in literature as shown in Table 3 [1, 17, 18, 27, 64, 74, 78, 79, 88, 92].
Surgery
Major role in the treatment of chordomas is played by extensive surgical resection even with multiple-staged combined approaches via anterior and lateral approaches [1, 44, 78, 79, 84]. Goals of surgery are to remove as much neoplastic tissue as possible and to preserve or improve patient's functional status [17, 26, 28, 40, 64]. In cases in which radical resection is not possible without the risk of a severe morbidity, surgery could be aimed to obtain neural decompression and tumour volume reduction in order to make radiotherapy more effective and safe [1, 7, 18, 44, 63].
Gay and colleagues proposed aggressive tumour removal, especially at the initial surgery and if no previous radiotherapy has been administered. In this surgical series, radical removal was achieved in 67%, subtotal in 23% and partial in 10% of the patients [28, 74]. Correlation between extent of surgery and complications rate is still a matter of debate. Aggressive surgical strategy of Gay and colleagues was associated with a high complication rate. They reported new cranial nerve deficits in 80% of the patients; these deficits were transient in the majority of cases. Incidence of abducent nerve palsy, hearing loss, permanent facial palsy and visual decline were respectively 28%, 15%, 8% and 8%. In 30% of cases a cerebrospinal fluid (CSF) leak was reported [28, 74]. Menezes instead reported no cases of CSF leakage or new cranial nerve deficits in his surgical series [17, 46].
Postoperative cranial nerve palsy rate reported by Colli and Al-Mefty was 58.7% with an additional permanent or transient postoperative neurological deficit rate respectively occurred in 28.6% and 22.2% of patients [17]. They observed also that the best chance of postoperative deficit recovery was associated with sixth cranial nerve palsy, followed by seventh, third and fifth cranial nerve palsies [17].
They supported the hypothesis that complication rate and extension of surgical resection are not correlated. In their study complication rate after radical excision was 61.3% and after subtotal excision was 72.2% with no statistical difference between the two groups (p value 0.541) [17].
Sekhar and colleagues proposed complete tumour removal in primary treated patients with a total removal rate of 59% and an incidence of CSF leakage, vessel injury and new cranial nerve deficit respectively of 20%, 12% and 33% [74, 77]. Perioperative death rate was 12% [17].
Pamir et al. achieved 50% of gross total removal rate with an estimated mortality and major complications rates of 5% and 10%, respectively. Post-operative CSF leak was reported in 30% of surgical procedures [64].
Al-Mefty and Borba (25 patients) instead reported a radical removal rate of 43.5%, subtotal removal rate of 47.8% and partial removal rate of 8.7% of the patients, with only one case of perioperative death and three other cases of deaths [1]. Pallini et al. achieved total removal in 42% of cases with a lower CSF leakage rate of 11% and a meningitis rate of 8% [63]. Tzorzidis reported a higher total removal rate of 72%, with only 1% of CSF leak rate and a perioperative mortality rate of 3% [88]. Extent of resection and postoperative complications rate are summarized respectively in Tables 4 [1, 16–18, 27, 63, 74, 77–79, 88] and 5 [1, 17, 18, 28, 63, 64, 74, 77–79, 88].
Surgery for recurrence is challenging. Recurrent tumours are not only more difficult to remove but also carry a higher mortality and complication rate [88]. Crockard et al. obtained complete tumour removal in 72% of cases with an incidence of CSF leak of 21% at first surgery and 56% at re-operation and a perioperative death rate of 4.3%. Meningitis occurred in 8% of cases [18]. Samii and colleagues achieved complete tumour removal in 49.4% of cases with a mortality rate of 2% at first surgery and 5.3% at re-operation [74].
Operative approaches are selected on the basis of the predominant tumour extension and the tumour size. Extension through the base of the skull is a crucial characteristic of skull base chordomas and the mainly limiting factor in their surgical removal and management with radiation therapy. Lateral and anterior cranial base approaches have all their proponents as shown in Table 6 [1, 16–18, 28, 63, 64, 74, 88].
Application of endonasal endoscopy to cranial base surgery led to the development of new surgical approaches. The endoscopic endonasal approach (EEA) takes advantage of the natural sinus corridor and may provide a less invasive approach for these midline tumours, providing a similar resection compared with traditional cranial base approaches while potentially limiting surgical morbidity [84]. Sometimes two or more staged surgical procedures may be necessary to achieve a radical removal. Pamir reported that in order to achieve 50% rate of complete tumour removal, 16–50% of patients require multiple skull base operations [1, 17, 28, 64]. To clarify the best approach to these tumours, Al-Mefty and colleagues defined an anatomo-surgical classification of the lesions. The classification is based on the patterns of extension of the tumour. Type I tumours are small and can be symptomatic or asymptomatic. This type has the best prognosis because it can be radically removed; type II tumours reach a relatively large size, but radical surgical removal can be performed using only one skull base approach. This type is the most common. Type III tumours extended through the skull base and require two or more skull base procedures to achieve radical removal [1]. Sen and colleagues argued that although the surgical approach should be planned according to the location, size and distribution of the tumour, the use of a midline anterior approach or a lateral approach does not show comparative superiority [79].
Postoperative functional outcome
Preoperative, postoperative and follow-up assessment of disability, as reflected by Karnofsky performance status (KPS) score allows surgeons to detect patients whose conditions have worsened due to surgical treatment or due to tumour regrowth or recurrence. Gay et al. reported a permanent postoperative functional deterioration, usually in 10 points, in 40% of patients [28]. Colli and Al-Mefty described no oscillation in KPS scores after surgery, but 7.5% of patients experienced worsened function due to tumour removal and none of them improved, and another 5.6% experienced worsened function during the first 6 months postoperatively due to tumour regrowth or recurrence [17]. Post-operative stay in the intensive care unit reflects some of the immediate post-operative problems. The mean length of stay in hospital in the series reported by Sen et al. was 4.3 days with five patients out of this range. In the majority of patients, preoperative KPS was maintained. A reduction of 10 points occurred in eight patients due to aggravation of a cranial nerve deficit or new cranial nerve deficits. The patients for whom the KPS showed a decrease of more than 10 points were ultimately the ones that died of disease progression [78]. In his updated clinical series published in 2010, Sen reported that in 51% of cases, postoperative KPS remains stable, in 18% it improved and in 31% it declined [79]. Gay et al. noted that the majority of the patients with worsened KPS score demonstrated immediately after surgery recovered in the following 6 to 12 months [28]. Variations in KPS after surgery and at the last follow-up control as reported in literature are summarized in Table 7 [16, 17, 27, 28, 64, 77–79, 88].
Radiotherapy
An important role in the management of chordomas is played by high-dose radiotherapy, which provides a good tumour control [4, 13, 37]. Chordomas are considered relatively resistant to conventional radiotherapy. Radiosensitivity of chordomas is limited in the 70–80-Gy dose range. The most common delivery methods applied in the treatment of chordomas include high-dose radiotherapy with proton beam radiation and radiosurgery using Gamma Knife and CyberKnife [4, 51, 52, 58, 59, 66, 88]. Application of radiotherapy as adjuvant treatment in the multimodal management of chordomas is still debated in literature as shown in Table 3 [1, 17, 18, 27, 64, 74, 78, 79, 88, 92].
Radiotherapy provides better local control when administered postoperatively than when delivered after recurrence following surgical resection [1, 2]. Main delivery methods are conventional radiotherapy, proton beam radiotherapy, radiosurgery and radioactive sources. Proton beam radiotherapy, radiosurgery and conventional radiotherapy all have their proponents as shown by Table 8 [17, 64, 74, 88].
Conventional radiotherapy doesn't improve survival time but has significant effect on prolonging progression-free survival (PFS) [2, 14, 15, 17, 19, 25, 27, 68, 78, 79]. Tai et al. reported a better median survival time with surgery and adjuvant PBRT (7.5 years), rather than with surgery alone (0.25 years) [87]. Kondziolka et al. reported in their series no tumour progression after stereotactic radiosurgery with a mean margin delivered dose of 20 Gy. Austin-Seymour reported a 5-year PFS rate of 76% with a 69 CGE median tumour dose [42].
In patients treated with stereotactic fractionated photon or proton beam therapy or combined proton–photon irradiation, the 5-year actuarial tumour control rate ranges from 68% to 85% [4, 5, 7, 17, 21, 36, 72]. Local recurrence occurs in 15–31% of patients with a median survival time to local treatment failures of 32 to 60 months [5, 17, 21, 86].
Therapeutic effect is dose related as described by Pearlman et al. They obtained a tumour growth control (TGC) rate of 80% in patients treated with an average dose of 80 Gy and a TGC rate of 20% in patients treated with an average dose of 40–60 Gy [66].
The effectiveness is also related to the volume of residual tumour [7]. Hug et al. reported that in all patients in whom tumours volumes were smaller than 25 ml, the tumour remained controlled compared with 56% of tumours greater than 25 ml [17, 36]. O'Connell et al. identified a critical volume of 70 ml, above which the local failure rate was much higher [59, 78].
Colli and Al-Mefty suggested that the risk of recurrence is related to the delivery method applied in the treatment. They reported a significantly lower risk of recurrence in patients treated with proton beam therapy than those treated with conventional radiotherapy (p < 0.05) [17]. Large lesion size, extent of infiltrated tissue and dose limitation by sensitivity of adjacent structures make difficult to treat chordomas with radiotherapy alone [42, 63].
Castro et al. reported an overall complication rate after RT of 27% [13]. Al-Mefty and Borba observed radionecrosis in 17.6% of patients treated with RT [1]. Main clinical complications due to radiation therapy described by Austin-Seymour et al. are those involving the visual apparatus (4.4%) and pituitary insufficiency (13.2%) [5].
Chemotherapy
In patients with recurrent disease not even eligible for surgery or radiotherapy, chemotherapy with imatinib mesylate (IM) represents a therapeutic option. IM is a tyrosine kinase inhibitor targeting platelet-derived growth factor receptor-beta (PDGFRB), and tyrosine protein kinases BCR-ABL and kit.
Inhibition of PDGFRB is likely to mediate antitumour activity of IM in chordoma [12]. Patients harbouring skull base chordomas were found to demonstrate positive expression of PDGFRB [61]. Casali and colleagues studied early results in a small clinical series of six cases. They documented after a treatment period of more than 1 year a decrease in glucose uptake on the PET scan, a midterm sign of a decrease in tumour density on the CT scan and a change in the signal intensity on the MRI scan even with a noticeable impact on tumour size, which indeed also may increase. Delayed signs showed a decrease in the size of the tumour and/or tumour stabilization with altered tumour density. Histologically, signs of response were cellular depletion with varying degrees of an apoptotic tumour cell population and a stromal myxoid degeneration [12].
The role of the epidermal growth factor receptor (EGFR) in chordoma pathogenesis was also studied, as a potential therapeutic target for novel molecular approaches for the treatment of chordomas. Shalaby and colleagues analysed 173 chordomas samples [80]. They revealed a total EGFR expression in 69% of cases. By performing FISH analysis on the samples, they found high level of EGFR polysomy in 38% of cases, high-level polysomy with focal amplification in 4%, low-level polysomy in 18% and disomy in 39%. As second step, they sequenced EGFR (exons 18–21), the Ras protein superfamily members KRAS, NRAS, HRAS (exons 2, 3) and BRAF (exons 11, 15), without finding any mutations in the 62 analysed samples. In addiction they observed that phosphatase and tensin homolog gene expression was absent in 13% of analysed chordomas, and only one of these revealed a high-level polysomy of EGFR. The EGFR inhibitor tyrphostin (AG 1478) markedly inhibited proliferation of the chordoma cell line U-CH1 in vitro and diminished EGFR phosphorylation in a dose-dependent manner. These finding was supported by the inhibition of phosphorylated kinases Erk1/2. They concluded that aberrant EGFR signalling played a role in the pathogenesis of chordoma, providing a strategy for patient stratification for treatment with EGFR antagonists [80].
EGFR antagonist showed to be effective as alternative treatment in patients refractory to imatinib. From this point of view, Singhal et al. reported a case where treatment with erlotinib, an EGFR tyrosine kinase inhibitor, induced symptomatic and radiological response in a patient with disease refractory to IM and vascular disrupting agent [81].
Methylthioadenosine phosphorylase (MTAP) and activated insulin-like growth factor-1 receptor/insulin (IGF1R) receptor were also studied as potential therapeutic targets in chordoma. Sommer et al. investigated paraffin-embedded tissue samples from 30 chordomas [82]. The samples were analysed by immunohistochemistry for expression of the phosphorylated isoforms of the IGF1R or the insulin receptor (pIGF1R/pIR), of the cyclin-dependent kinase inhibitor 2A and of the MTAP. Selected downstream signalling molecules, including bcl-2-associated agonist of cell death protein (BAD), were also studied. As comparison chondrosarcoma samples, benign notochordal cell tumours and fetal notochord were studied. They detected phosphorylated IGF1R/IR in 41% of cases, together with activated downstream signalling molecules, whereas pIGF1R/pIR was absent in benign notochordal cell tumours and fetal notochord. Chordomas resulted to be negative for MTAP immunoreactivity in 39% of cases. They compared molecular data with clinical follow-up, reporting that patients with pIGF1R/pIR-positive tumours showed significantly decreased median disease-free survival. Phosphorylation of BAD at serine-99 was found to be associated with a favourable prognosis. Forty percent of chordomas demonstrated evidence of activation of the IGF1R/IR signalling pathway or loss of a key enzyme in the purine salvage pathway. They argued that this aberrant signalling cascade may represent the target for novel molecular therapies for the treatment of chordoma [82].
In view of the association of chordoma and tuberous sclerosis complex syndrome, and the available therapeutic agents against molecules in the PI3K/AKT/TSC1/TSC2/mTOR pathway, Presneau et al. studied this molecular pathway to identify potential molecular targets for the treatment of chordoma [67]. They analysed tissue microarray of 50 chordoma cases. Expression of PI3K/AKT/TSC1/TSC2/mTOR pathway was determined. As conclusion they argued that on the basis of mammalian target of rapamycin protein (p-mTOR) and or p70S6 kinase (p-p70S6K) expression profile in the analysed specimens, there was evidence indicating that 65% of the cases may be responsive to mTOR inhibitors, rapamycin or its analogues, and that these patients may benefit from combined therapy including drugs that inhibit serine/threonine protein kinase Akt/PKB (AKT) [67].
Schwab and colleagues tested 13 chordoma samples for activation of the PI3K/mTOR pathway [76]. They treated the cell line UHC-1 with increasing dose of phosphoinositide-103 (PI-103) and examined consequent inhibition of AKT and mTOR, finally assays assessing proliferation and apoptosis were performed. As result they demonstrated activation of the PI3K/mTOR pathway in the samples and that PI-103 inhibited the AKT and mTOR activation in the UCH-1 cell line. PI-103 action inhibited proliferation and induced cell apoptosis. As conclusion they argued that PI3K/AKT and mTOR signalling pathway is constitutively activated in chordoma and that PI-103 decreases proliferation and induces apoptosis in the UCH-1 via inhibition of the PI3K/mTOR pathway [76].
Association of IM and other chemotherapeutic agents such as mTOR inhibitor molecules showed to be effective in the treatment of IM-resistant chordomas. Stacchiotti et al. combined an mTOR inhibitor, sirolimus, to IM in IM-resistant advanced chordoma. They argued that in addition to PDGFRB, mTOR pathway can be activated in chordomas and the combination of IM plus rapalogs may be effective in IM-resistant chordomas.
Resistance to chemotherapy and radiotherapy were also studied as result of molecular pattern expressed in chordoma cell lines [83]. Ji and colleagues investigated the expression of three genes: multidrug resistance gene 1 (MDR1), hypoxia-inducible factor 1 alpha (HIF-1alpha) and multidrug resistance-associated protein 1 (MRP1) as associated with resistance to chemotherapy and radiotherapy in chordoma and chordoma cell line CM-319 [38]. Performing immunohistochemical techniques, they studied the expression of MDR1, HIF-1alpha and MRP1 in 50 chordoma specimens. Expression of MDR1, HIF-1alpha and MRP1 was observed in 10%, 80% and 74% of all cases, respectively. They found a correlation between MRP1expression and HIF-1alpha. On the contrary expression of MDR1 was not correlated with the expression of HIF-1alpha or MRP1. The expression of HIF-1alpha and MRP1 was observed, but MDR1was not observed in chordoma and CM-319. Analysing the data they concluded that HIF-1alpha and MRP1 may play a role in the multidrug resistance of chordoma to chemotherapy [38].
An alternative therapeutic option to systemic chemotherapy is intratumoral chemotherapy. Guiu and colleagues reported the use of direct intratumoral chemotherapy to treat recurrent chordoma, using 5-mg/ml carboplatin solution, combined with epinephrine (to increase the concentration and antitumour effect of carboplatin) at a final concentration of 0.01 mg/ml and an iodinated contrast agent [30]. A marked clinical response with regression of the spinal cord compression was observed, without specific toxicity. A good partial response was obtained with a 42% decrease in tumour volume (from 69 to 40 cm3). Moreover, the central part of the tumour showed tumour necrosis, as confirmed by histological examination. Intratumoral chemotherapy in combination with surgical treatment should be considered to improve the local control rate [30].
In paediatric patients ifosfamide and etoposide may play a role in the treatment of chordoma. Dhall and colleagues reviewed the role of chemotherapy in the treatment, management and outcome of children harbouring clival chordomas [23]. They reported the medical records of six paediatric chordoma patients. All the patients underwent an initial surgical resection. Chemotherapeutic agents included ifosfamide and etoposide in all four surviving patients. They concluded that chemotherapy with ifosfamide and etoposide may play a role in the treatment of paediatric clival chordomas when used alone or in combination with irradiation [23].
Survival and recurrence
Chordomas are generally lethal with a 5-year survival rate reported at 75% [79]. Survival time after surgery or radiation therapy or both range from 3.6 to 6.6 years [17, 39, 68, 69]. Estimated overall survival (OS) rates for patients with chordoma are 13–51% and 18–35% at, respectively, 5 and 10 years after resection [17, 27, 62]. In a series of 51 patients, Forsyth reported a 5- and 10-year survival rate respectively of 36% and 0% in patients who underwent biopsy and respectively of 55% and 45% for those who underwent subtotal resection [27].
Overall 5-year PFS rates for patients in whom total or near total resections and subtotal or partial resections are achieved and range from 55% to 84% and from 36% to 64%, respectively [6, 15, 17, 28]. Gay reported a PFS at 5 years of 84% in patients in which total or near total removal was achieved and 64% for cases in which there was partial or subtotal removal [28]. In the series reported by Al-Mefty and Borba (25 patients), recurrence was observed in 5 patients, 2 of whom had early recurrence (3 and 7 months) [1]. The estimated PFS rates ranged from 33% to 76% at 5 years and from 24% to 76% at 10 years [17, 27, 28].
The most recent data in the literature evidence that the extent of resection is correlated with a lower risk of recurrence. With modern skull base techniques, more than 90% resection can be achieved in 58–78.5% of patients with intracranial chordoma. The reported PFS rate at 5 years range from 55–84%, and the corresponding range for cases of subtotal or partial resection is 36–64% [17, 18, 28, 64, 78, 79]. OS and PFS rates as reported in literature are summarized respectively in Tables 9 and 10 [16–18, 27, 74, 92].
Prognostic factors
Extent of resection, previous treatment, adjuvant proton beam therapy and the karyotype are thought to influence the prognosis [17]. Forsyth et al. recognised as prognostic factors the age of the patient (better outcome was observed if patient's age was under 40 years), the presence of double vision at diagnosis (better outcome was observed, if diplopia was present at diagnosis), the adjuvant RT (they observed that radiotherapy didn't improve survival time), the chondroid histology (it was not associated with significant longer survival), the presence of mitosis and necrosis (poor prognostic factors) and presence of metastasis (poor prognostic factor) [27].
Tumour volume at diagnosis is considered to be a significant prognostic factor for tumour recurrence. Pamir suggested that tumour progression after treatments is almost the rule if initial tumour volume exceeds 20 cc [64].
Despite the possibility of a long progression-free survival after gross total or subtotal resection and radiation therapy, ultimately the majority of patients will experience recurrence and will die of local progression of their disease. It also appears, however, that chordomas that have been resected to the same extent and that received post-operative radiotherapy might exhibit different rates of regrowth. This result supports the hypothesis that the recurrence rate of chordomas might be dependent on variables other than the extent of resection and the post-operative radiotherapy. Previous studies have investigated the classic pathological paradigms in relation to the biological and clinical behaviour of clival chordomas; the results suggested that the pathological features studied are poor predictors of outcome [17, 18, 28, 59]. In particular Naka and colleagues in their retrospective multi-centric study on 72 cases of skull base chordomas didn't find any pathological variant significantly correlated with survival; they only found that the proliferative ability of skull base chordomas appears to be closely associated with recurrence and nuclear pleomorphism [53].
Matsuno et al. studied the immunohistochemical expression of MIB-I, p53, cyclin D1 and identified these markers as important predictors of recurrence [45]. Naka et al. demonstrated that the proliferative potential of these tumours was correlated with the combination of p53 overexpression, anaplasty, high-grade atypia and diffuse proliferation [54].
Holton et al. showed that tumour doubling time correlated with age, sex, histological parameters and Ki-67 labelling index [34]. Pallini et al. suggested that expression of telomerase transcriptase m-RNA and mutation of p53 may indicate cases at risk for early recurrence [63].
Riva and colleagues performed a genetic characterization of chordomas samples centred on the loss of heterozygosity (LOH) analysis on 1p36 and on the determination of the expression profile of apoptotic genes mapped to this region [70]. They compared chordoma molecular data and patients' clinical outcome considering as clinical endpoint tumour recurrence and patient death. Molecular data demonstrated no events of recurrence or death occurred in the group of patients without LOH in 1p36 or with tumour necrosis factor TNFRSF8 gene expression. This suggests a possible correlation between the clinical outcome and absence of LOH in 1p36 or the expression of TNFRSF8 [70]. Molecular and genetic studies performed on chordoma samples to investigate molecular candidates to define prognosis are summarized in Table 11 [10, 18, 20, 22, 29, 31, 34, 35, 38, 41, 45, 49, 50, 53–56, 60, 63, 67, 70, 75, 76, 80, 82, 90].
Conclusions
Clival chordomas are extremely rare tumours. Surgical treatment and radiation therapies have a definitive role in the management of these tumours. Different treatment philosophies have been reported in the literature. Clinical outcome seems to be affected by the extent of surgical resection and by the following adjuvant therapies.
Nevertheless it appears that chordomas that have received the same treatment might exhibit different rates of regrowth. This result supports the hypothesis that the recurrence rate of chordomas might be dependent on biological variables other than the extent of resection and the post-operative radiotherapy. Genetic and molecular studies on oncogenesis of chordomas have revealed significant correlation between molecular patterns and clinical behaviour. These studies have been also the basis for the experimental use of molecular targeted therapies; preliminary encouraging clinical results have been reported in small groups of patients. A more accurate and complete biological characterization of these tumours and the consequent development of effective molecular targeted therapies will probably improve the clinical outcome in skull base chordomas patients.
References
Al-Mefty O, Borba LA (1997) Skull base chordomas: a management challenge. J Neurosurg 86(2):182–189
Amendola BE, Amendola MA, Oliver E et al (1986) Chordoma: role of radiation therapy. Radiology 158:839–843
Arnautovic KI, Al-Mefty O (2001) Surgical seeding of chordomas. J Neurosurg 95:798–803
Austin JP, Urie MM, Cardenosa G et al (1993) Probabile causes of recurrence in patients with chordoma and chondrosarcoma of the base of skull and cervical spine. Int J Radiat Oncol Biol Phys 25:439–444
Austin-Seymour M, Munzenrider J, Goitein M et al (1989) Fractionated proton radiation therapy of chordoma and low-grade chondrosarcoma of the base of the skull. J Neurosurg 70:13–17
Benk V, Liebsch NJ, Munzenrider JE et al (1995) Base of skull and cervical spine chordomas in children treated by high-dose irradiation. Int J Radiat Oncol Biol Phys 31:577–581
Berson AM, Castro JR, Petti P et al (1988) Charged particle irradiation of chordoma and chondrosarcoma of the base of skull and cervical spine: the Lawrence Berkeley Laboratory experience. Int J Radiat Oncol Biol Phys 15:559–565
Borba LA, Al-Mefty O, Mrak RE et al (1996) Cranial chordomas in children and adolescents. J Neurosurg 84:584–591
Brooks JJ, LiVolsi VA, Trojanowski J (1987) Does chondroid chordoma exist? Acta Neuropathol (Berl) 72:229–235
Camacho-Arroyo I, González-Agüero G, Gamboa-Domínguez A et al (2000) Progesterone receptor isoforms expression pattern in human chordomas. J Neurooncol 49(1):1–7
Carpentier A, Polivka M, Blanquet A et al (2002) Suboccipital and cervical chordomas: the value of aggressive treatment at first presentation of the disease. J Neurosurg 97(5):1070–7
Casali PG, Messina A, Stacchiotti S et al (2004) Imatinib mesylate in chordoma. Cancer 101(9):2086–2097
Castro JR, Linstadt DE, Bahary JP et al (1994) Experience in charged particle irradiation of tumors of the skull base: 1977–1992. Int J Radiat Oncol Biol Phys 29:647–655
Chetiyawardana AD (1984) Chordoma: results of treatment. Clin Radiol 35:159–161
Chetty R, Levin CV, Kalan MR (1991) Chordoma: a 20-year clinicopathologic review of the experience at Groote Schuur Hospital, Cape Town. J Surg Oncol 46:261–264
Cho YH, Kim JH, Khang SK et al (2008) Chordomas and chondrosarcomas of the skull base: comparative analysis of clinical results in 30 patients. Neurosurg Rev 31(1):35–43
Colli BO, Al-Mefty O (2001) Chordomas of the skull base: follow-up review and prognostic factors. Neurosurg Focus 10(3):E1
Crockard HA, Steel T, Plowman N et al (2001) A multidisciplinary team approach to skull base chordomas. J Neurosurg 95(2):175–183
Dahlin DC, MacCarty CS (1952) Chordoma: a study of fifty-nine cases. Cancer 5:1170–1178
Dalpra L, Malgara R, Miozzo M et al (1999) First cytogenetic study of a recurrent familial chordoma of the clivus. Int J Cancer 81:24–30
Debus J, Schulz-Ertner D, Schad L et al (2000) Stereotactic fractionated radiotherapy for chordomas and chondrosarcomas of the skull base. Int J Radiat Oncol Biol Phys 47:591–596
Deniz ML, Kiliç T, Almaata I et al (2002) Expression of growth factors and structural proteins in chordomas: basic fibroblast growth factor, transforming growth factor alpha, and fibronectin are correlated with recurrence. Neurosurgery 51(3):753–760
Dhall G, Traverso M, Finlay JL et al (2010) The role of chemotherapy in pediatric clival chordomas. J Neurooncol 103(3):657–662
Erdem E, Angtuaco EC, Van Hemert R et al (2003) Comprehensive review of intracranial chordoma. Radiographics 23(4):995–1009
Eriksson B, Gunterberg B, Kindblom LG (1981) Chordoma. A clinicopathologic and prognostic study of a Swedish national series. Acta Orthop Scand 52(1):49–58
Fagundes MA, Hug EB, Liebsch NJ et al (1995) Radiation therapy for chordomas of the base of skull and cervical spine: patterns of failure and outcome after relapse. Int J Radiat Oncol Biol Phys 33(3):579–584
Forsyth PA, Cascino TL, Shaw EG et al (1993) Intracranial chordomas: a clinicopathological and prognostic study of 51 cases. J Neurosurg 78(5):741–747
Gay E, Sekhar LN, Rubinstein E et al (1995) Chordomas and chondrosarcomas of the cranial base: results and follow-up of 60 patients. Neurosurgery 36(5):887–896
Gottschalk D, Fehn M, Patt S et al (2001) Matrix gene expression analysis and cellular phenotyping in chordoma reveals focal differentiation pattern of neoplastic cells mimicking nucleus pulposus development. Am J Pathol 158(5):1571–1578
Guiu S, Guiu B, Feutray S et al (2009) Direct intratumoral chemotherapy with carboplatin and epinephrine in a recurrent cervical chordoma: case report. Neurosurgery 65(3):E629–30
Haeckel C, Krueger S, Kuester D et al (2000) Expression of cathepsin K in chordoma. Hum Pathol 31(7):834–840
Heffelfinger MJ, Dahlin DC, MacCarty CS et al (1973) Chordomas and cartilaginous tumors at the skull base. Cancer 32:410–420
Higinbotham NL, Phillips RF, Farr HW et al (1967) Chordoma. Thirty-five-year study at memorial hospital. Cancer 20(11):1841–1850
Holton JL, Steel T, Luxsuwong M et al (2000) Skull base chordoma: correlation of tumor doubling time with age, mitosis and Ki67 proliferation index. Neuropathol Appl Neurobiol 26:497–503
Hu B, McPhaul L, Cornford M et al (1999) Expression of tau proteins and tubulin in extraskeletal myxoid chondrosarcoma, chordoma, and other chondroid tumors. Am J Clin Pathol 112(2):189–193
Hug EB, Fitzek MM, Liebsch NJ et al (1995) Locally challenging osteo and chondrogenic tumors of the axial skeleton: results of combined proton and photon radiation therapy using three-dimensional treatment planning. Int J Radiat Oncol Biol Phys 31:467–476
Hug EB, Slater JD (2000) Proton radiation therapy for chordomas and chondrosarcomas of the skull base. Neurosurg Clin N Am 11:627–638
Ji Z, Long H, Hu Y et al (2010) Expression of MDR1, HIF-1alpha and MRP1 in sacral chordoma and chordoma cell line CM-319. J Exp Clin Cancer Res 29(1):158
Kamrin RP, Potanos JN, Pool JL et al (1964) An evaluation of the diagnosis and treatment of chordoma. J Neurol Neurosurg Psychiatry 27:157–165
Keisch ME, Garcia DM, Shibuya RB et al (1991) Retrospective long-term follow-up analysis in 21 patients with chordomas of various sites treated at a single institution. J Neurosurg 75(3):374–377
Kilgore S, Prayson RA (2002) Apoptotic and proliferative markers in chordomas: a study of 26 tumors. Ann Diagn Pathol 6(4):222–228
Kondziolka D, Lunsford LD, Flickinger JC (1991) The role of radiosurgery in the management of chordoma and chondrosarcoma of the cranial base. Neurosurgery 29(1):38–46
Korten A, Berg H, Spincemaille GH et al (1998) Intracranial chondrosarcoma: review of the literature and report of 15 cases. J Neurol Neurosurg Psychiatry 65:88–92
Lanzino G, Dumont AS, Lopes MB et al (2001) Skull base chordomas: overview of disease, management options, and outcome. Neurosurg Focus 10(3):E12
Matsuno A, Sasaki T, Nagashima T et al (1997) Immunohistochemical examination of proliferative potentials and the expression of cell cycle-related proteins of intracranial chordomas. Hum Pathol 28(6):714–719
Menezes AH, Sato Y (1995) Primary tumors of the spine in children—natural history and management. 1990. Pediatr Neurosurg 23(2):101–113
Meyer JE, Oot RF, Lindfors KK (1986) CT appearance of clival chordomas. J Comput Assist Tomogr 10(1):34–38
Meyers SP, Hirsch WL Jr, Curtin HD et al (1992) Chordomas of the skull base: MR features. Am J Neuroradiol 13(6):1627–1636
Miozzo M, Dalprà L, Riva P et al (2000) A tumor suppressor locus in familial and sporadic chordoma maps to 1p36. Int J Cancer 87(1):68–72
Mori K, Chano T, Kushima R et al (2002) Expression of E-cadherin in chordomas: diagnostic marker and possible role of tumor cell affinity. Virchows Arch 440(2):123–127
Munzenrider JE, Liebsch NJ (1999) Proton therapy for tumors of the skull base. Strahlendher Onkol 175(Suppl 2):57–63
Muthukumar N, Kondziolka D, Lunsford LD et al (1998) Stereotactic radiosurgery for chordoma and chondrosarcoma: further experiences. Int J Radiat Oncol Biol Phys 41:387–392
Naka T, Boltze C, Samii A et al (2003) Skull base and nonskull base chordomas: clinicopathologic and immunohistochemical study with special reference to nuclear pleomorphism and proliferative ability. Cancer 98(9):1934–1941
Naka T, Fukuda T, Chuman H et al (1996) Proliferative activities in conventional chordoma: a clinicopathologic, DNA flow cytometric, and immunohistochemical analysis of 17 specimens with special referente to anaplastic chordoma showing a diffuse proliferation and nuclear atypia. Hum Pathol 27(4):381–388
Naka T, Iwamoto Y, Shinohara N et al (1997) Cytokeratin subtyping in chordomas and the fetal notochord: an immunohistochemical analysis of aberrant expression. Mod Pathol 10(6):545–551
Naka T, Oda Y, Iwamoto Y et al (2001) Immunohistochemical analysis of E-cadherin, alpha-catenin, beta-catenin, gamma-catenin, and neural cell adhesion molecule (NCAM) in chordoma. J Clin Pathol 54(12):945–950
Nishigaya K, Kaneko M, Ohashi Y et al (1998) Intradural retroclival chordoma without bone involvement: no tumor regrowth 5 years after operation. Case report. J Neurosurg 88(4):764–768
Noel G, Feuvret L, Calugaru V et al (2005) Chordomas of the base of the skull and upper cervical spine. One hundred patients irradiated by a 3D conformal technique combining photon and proton beams. Acta Oncol 44:700–708
O'Connell JX, Renard LG, Liebsch NJ et al (1994) Base of skull chordoma: a correlative study and clinical features of 62 cases. Cancer 74:2261–2267
O'Hara BJ, Paetau A, Miettinen M (1998) Keratin subsets and monoclonal antibody HBME-1 in chordoma: immunohistochemical differential diagnosis between tumors simulating chordoma. Hum Pathol 29(2):119–126
Orzan F, Terreni MR, Longoni M et al (2007) Expression study of the target receptor tyrosine kinase of Imatinib mesylate in skull base chordomas. Oncol Rep 18(1):249–252
Paavolainen P, Teppo L (1967) Chordoma in Finland. Acta Orthop Scand 47:46–51
Pallini R, Maira G, Pierconti F et al (2003) Chordoma of the skull base: predictors of tumor recurrence. J Neurosurg 98(4):812–822
Pamir MN, Kiliç T, Türe U et al (2004) Multimodality management of 26 skull-base chordomas with 4-year mean follow-up: experience at a single institution. Acta Neurochir (Wien) 146(4):343–354
Park SA, Kim HS (2008) F-18 FDG PET/CT evaluation of sacrococcygeal chordoma. Clin Nucl Med 33(12):906–908
Pearlman AW, Friedman M (1970) Radical radiation therapy of chordoma. Am J Roentgenol Radium Ther Nucl Med 108:333–341
Presneau N, Shalaby A, Idowu B et al (2009) Potential therapeutic targets for chordoma: PI3K/AKT/TSC1/TSC2/mTOR pathway. Br J Cancer 100(9):1406–1414
Raffel C, Wright DC, Gutin PH et al (1985) Cranial chordoma: clinical presentation and results of operative and radiation therapy in twenty-six patients. Neurosurgery 17:703–710
Rich TA, Schiller A, Suit HD et al (1985) Clinical and pathologic review of 48 cases of chordoma. Cancer 56:182–187
Riva P, Crosti F, Orzan F et al (2003) Mapping of candidate region for chordoma development to 1p36.13 by LOH analysis. Int J Cancer 107(3):493–497
Roberti F, Sekhar LN, Jones RV et al (2007) Intradural cranial chordoma: a rare presentation of an uncommon tumor. Surgical experience and review of the literature. J Neurosurg 106(2):270–274
Rosenberg AE, Nielsen GP, Keel SB et al (1999) Chondrosarcoma of the base of the skull: a clinicopathologic study of 200 cases with emphasis on its distinction from chordoma. Am J Surg Pathol 23:1370–1378
Russel DS, Rubinstein LJ (1989) Pathology of tumors of the nervous system. Edward Arnold, London
Samii A, Gerganov VM, Herold C et al (2007) Chordomas of the skull base: surgical management and outcome. J Neurosurg 107(2):319–324
Scheil S, Brüderlein S, Liehr T et al (2001) Genome-wide analysis of sixteen chordomas by comparative genomic hybridization and cytogenetics of the first human chordoma cell line, U-CH1. Genes Chromosomes Cancer 32(3):203–211
Schwab J, Antonescu C, Boland P et al (2009) Combination of PI3K/mTOR inhibition demonstrates efficacy in human chordoma. Anticancer Res 29(6):1867–1871
Sekhar LN, Pranatartiharan R, Chanda A et al (2001) Chordomas and chondrosarcomas of the skull base: results and complications of surgical management. Neurosurg Focus 10(3):E2
Sen C, Triana A (2001) Cranial chordomas: results of radical excision. Neurosurg Focus 10(3):E3
Sen C, Triana AI, Berglind N et al (2010) Clival chordomas: clinical management, results, and complications in 71 patients. J Neurosurg 113(5):1059–1071
Shalaby A, Presneau N, Ye H et al (2011) The role of epidermal growth factor receptor in chordoma pathogenesis: a potential therapeutic target. J Pathol 223(3):336–346
Singhal N, Kotasek D, Parnis FX (2009) Response to erlotinib in a patient with treatment refractory chordoma. Anticancer Drugs 20(10):953–955
Sommer J, Itani DM, Homlar KC et al (2010) Methylthioadenosine phosphorylase and activated insulin-like growth factor-1 receptor/insulin receptor: potential therapeutic targets in chordoma. J Pathol 220(5):608–617
Stacchiotti S, Marrari A, Tamborini E et al (2009) Response to imatinib plus sirolimus in advanced chordoma. Ann Oncol 20(11):1886–1894
Stippler M, Gardner PA, Snyderman CH et al (2009) Endoscopic endonasal approach for clival chordomas. Neurosurgery 64(2):268–278
Stüer C, Schramm J, Schaller C (2006) Skull base chordomas: management and results. Neurol Med Chir (Tokyo) 46(3):118–125
Suit HD, Goitein M, Munzenrider J et al (1982) Definitive radiation therapy for chordoma and chondrosarcoma of base of skull and cervical spine. J Neurosurg 56:377–385
Tai PT, Craighead P, Bagdon F (1995) Optimization of radiotherapy for patients with cranial chordoma. A review of dose-response ratios for photon techniques. Cancer 75(3):749–756
Tzortzidis F, Elahi F, Wright D et al (2006) Patient outcome at long-term follow-up after aggressive microsurgical resection of cranial base chordomas. Neurosurgery 59(2):230–237
Volpe NJ, Liebsch NJ, Munzenrider JE et al (1993) Neuro-ophthalmologic findings in chordoma and chondrosarcoma of the skull base. Am J Ophthalmol 115:97–104
Walker WP, Landas SK, Bromley CM et al (1991) Immunohistochemical distinction of classic and chondroid chordomas. Mod Pathol 4(5):661–666
Warnick RE, Raisanen J, Kaczmar T Jr et al (1991) Intradural chordoma of the tentorium cerebelli. Case report. J Neurosurg 74(3):508–511
Watkins L, Khudados ES, Kaleoglu M et al (1993) Skull base chordoma: a review of 38 patients, 1958–88. Br J Neurosurg 7:241–248
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Benedicto Oscar Colli, Ribeirão Preto, Brasil
I would like to congratulate the authors by this laborious and good work. The authors performed a detailed review of the literature on chordoma. This review includes epidemiological, pathological and clinical aspects, but the focus is on the current treatment and on the molecular biology findings of the disease.
The topic on molecular biology should be outstanding because better understanding of this disease and further development of new therapeutic techniques probably will be based on these knowledge. Therefore, this review will be a very helpful resource for clinical and basic sciences researchers interested on the treatment of patients with chordomas.
Bernard George, Paris, France
This is a very useful review of literature about chordomas of the skull base, taking out the relevant data regarding all the aspects of this challenging pathology. Chordomas are a supposedly benign tumors but which behave at least as a locally malignant tumor. In fact about 20% present with metastases along their evolution. All the others exhibit more or less rapidly a recurrence. In our series of more than a hundred cases of various locations, we have never seen a single case that could be cured. The best results are two cases: one recurred after surgery and radiotherapy after 21 years; the other recurred after surgery only, without radiotherapy after 11 years. On the other side, there are more than 10% which recurred in less than 2 or even 1 year. This is a fact: there is a huge heterogeneity in the biological behaviour among chordomas; it must be added that there is also a lack of markers indicating the level of aggressiveness for each chordoma. As it is well reviewed in this paper that no clear parameter, whether it is clinical, radiological, histological or biological, permits to adjust the adequate therapy to each case. This explains the still existing controversies about the therapeutic strategy. One is non-aggressive, proposing a simple decompression more or less followed by radiotherapy, therefore waiting for a better appreciation of the evolution in each case; at the opposite is the strategy of being very aggressive at first presentation with as radical a surgery as possible followed by protontherapy, in every case even those which will prove to be slow growing. This is the strategy we apply at Lariboisiere after a study on chordomas of the cranio-cervical junction (1) and confirmed in a following study on chordomas of any location (2). Radical surgery plus protontherapy provided the best results when applied at first presentation. On the contrary, the same policy was not really beneficial in recurrent cases. For these recurrent cases, we still need a complementary treatment. In this paper there is an extensive review of the current data on chemotherapy. This is sometimes hard to follow but is absolutely worthy of reading and understanding, first because this is by these studies that biological markers can be expected to be found and consequently that new efficient treatments will be discovered. This part of this paper is absolutely crucial, and the authors should be thanked for the efforts they made to summarize these studies and to present them as clearly as possible. However for the moment, no treatment has been demonstrated to improve the results.
For the moment surgery remains the key element of the treatment, any effort should be done to remove as much tumor as possible and especially in the regions where radiotherapy cannot be applied safely (near the brain stem and optic pathways). Obviously without knowing what the speed of growth of each case is, this must not be done at any mean and quality of life should be preserved. New developments of surgical technique, particularly endoscopic endonasal approach permit today to better achieve this goal.
References
1. Carpentier A, Polivka M, Blanquet A, George B (2002) Suboccipital and cervical chordomas: the value of aggressive treatment at first presentation of the disease. J Neurosurg 97(5) 1070–1077
2. Yasuda M, Bresson D, Chibbaro S, Polivka M, George B (2011) Chordomas of the skull base and cervical spine: clinical outcomes associated with a multidisciplinary surgical resection combined with proton beam radiation in 40 patients. Neurosurg Rev (in press)
Amir Samii, Venelin Gerganov, Hannover, Germany
The authors performed an extensive review on the current knowledge about skull base chordomas biology, management and outcome of treatment. A promising new trend—the development of molecular targeted therapies and the application of chemotherapy that may revolutionize chordoma management in the future—has been highlighted. The authors point that that the recurrence rate of chordomas is related mainly to the biological tumor characteristics and to a lesser extent on the extent of resection and the post-operative radiotherapy. Some chordomas have a milder evolution and grow slowly, while others have more aggressive behaviour, with rapid local recurrence and even distal spread.
The generally accepted optimal treatment of skull base chordomas is radical surgery followed by proton or photon radiotherapy. The surgical approach should be selected individually taking into consideration the clinical symptoms and tumor characteristics, in particular its size, extension pattern, involvement of neurovascular structures and bone destruction. If only partial removal is possible, a second procedure via a different approach should be considered. Importantly, the attempt at complete tumor removal should not endanger important neural and vascular structures and should not impact the patients quality of life. In case radical tumor removal is impossible, every effort should be made to decompress nervous structures and allow safe and effective radiotherapy.
The refinement of the endoscopic technique and the elaboration of the endonasal endoscopic approach to the clival region have been a major recent advancement. This technique promotes more radical and safe tumor removal and has become a mainstay of the operative strategy of skull base chordomas. Extensive tumors may be removed via a combined endonasal and transcranial approaches, optimally with interdisciplinary cooperation. The utilization of neuronavigation during surgery allows for precise trajectory planning, accurate performing of the approach and control of extent of tumor resection. Important technological development in view of the significance of radical chordoma removal was the introduction of high-field intraoperative MRI devices, which allow almost real-time control of the extent of resection and detection of hidden tumor remnants. The combined use of these tools—as in the navigation-guided endonasal endoscopic approach with intraoperative high-field MRI control, promoted by us—is best suited to achieve the goals of skull base chordoma surgery.
Rights and permissions
About this article
Cite this article
Gagliardi, F., Boari, N., Riva, P. et al. Current therapeutic options and novel molecular markers in skull base chordomas. Neurosurg Rev 35, 1–14 (2012). https://doi.org/10.1007/s10143-011-0354-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-011-0354-1