Abstract
Statins are drugs used to control cholesterol disorders and prevent cardiovascular diseases. Their denominated pleiotropic effects have demonstrated a broad action spectrum that might profit some neurological and neurosurgical diseases. These effects are correlated to dose and kind of statin. We accomplished a systematic review in PubMed and MEDLINE about studies of statins and main neurosurgical diseases. If statins are administered after subarachnoid hemorrhage, a significant lower incidence of vasospasm as well as delayed ischemic deficits and decreased mortality could be found; the results of a large multicenter trial are expected. In other complex diseases as intracerebral hemorrhage or traumatic brain injury, the evidence for positive effects of a treatment with statin increased. Additionally, promising experimental results indicate that high statin doses are able to promote cell death in tumor cells, especially in gliomas. Moreover, experimental and observational studies suggest the ability of statins to modulate the immune system, by that they can reduce incidence and severity of sepsis. The origin of these multiple effects from neuroprotection to tumoral apoptosis is not totally explained so far. Recent data in literature are discussed in this review. More trials in humans are urgently required to finally determine if statins could contribute to the current management of neurosurgical diseases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Statins are structural analogs of β-hydroxy-β-methylglutaryl coenzyme A (HMG CoA) reductase, a restrictive enzyme in the cholesterol pathway. They are currently used for treatment of dyslipidemias and prevention of cardiovascular diseases [19]. The trials conducted for safety evaluation have suggested other possible benefits. The reduction of stroke, dementia, and incidence of tumors as well as of inflammatory molecules as C-reactive protein has been suggested [19, 26, 59]. Based on these data, many experimental studies have been performed, which describe a lot of unexpected phenomena. During the last years, research has been directed to neuroprotective effects. In this way, diseases like Alzheimer, multiple sclerosis, and other acute pathologies like stroke or subarachnoidal and intracerebral hemorrhage have been assessed [1, 17, 74, 79, 92]. Furthermore, experimental and clinical evidence regarding to anti-tumor activity is growing [26]. The denominated pleiotropic effects of statins seem not to be entirely related to cholesterol pathway [6, 107]. The mechanisms of this variety of effects are complex and not totally explained (Fig. 1).
Spectrum of effects of statins. The conjunction of anti-excitotoxicity (e.g., N-methyl-d-aspartate receptor), improvement of microvascular perfusion (e.g., nitric oxide synthase isoforms = eNOS), dilution of microthromboses (e.g., plasminogen activator inhibitor = PAI and tissue plasminogen activator = tPA), control of free radicals (e.g., superoxide dismutase = SOD) and the modulation of cytokines (e.g., by control of nuclear factor κβ), adhesion molecules (e.g., leukocyte-associated antigens-1 = LFA-1, intercellular adhesion molecule), and immune cells (monocytes, macrophages) generate a neuroprotective phenomenon. Additionally, the promotion of angiogenesis (e.g., vascular endothelial growth factor), neurogenesis (e.g., brain-derived neurotrophic factor), and synaptogenesis could originate neurorestoration. On the other hand, induction of apoptosis (e.g., caspases pathway), cell-cycle arrest, inhibition of angiogenesis (e.g., mitogen-activated proteins pathways), and modulation of immune cells conduce to an opposite global effect of death in tumor cells. TRAIL TNF-related apoptosis-inducing ligand
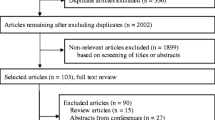
A systematic research on PubMed and MEDLINE (January 1980 to December 2009) for studies in rats and humans with statins and diverse neurosurgical diseases was accomplished. The term “statin” was combined with “subarachnoid hemorrhage”; “intracerebral hemorrhage”; “head injury” or “traumatic brain injury”; “glioma”, “glioblastoma”, or “brain tumors”; “spinal disease”; and “spinal cord injury”. For sepsis, key references were selected. In this review, we discuss the new possible implications of statins on neurosurgical diseases.
Subarachnoid hemorrhage
In 2002, McGuirt et al. reported for the first time a positive effect of statins after experimental subarachnoid hemorrhage (SAH) in mice. In this study, the animals were pre-treated or post-treated with simvastatin. After pre-treatment, an increased middle cerebral artery diameter and reduced neurological deficits were found [62]. A similar modest increase in middle cerebral artery diameter and decreased neurological deficits could be seen after post-treatment [62, 87]. The attenuation of perivascular granulocyte migration and the increment of endothelial nitric oxide synthase (eNOS) are proposed mechanisms for this vasospasm control [63, 87]. Recently, another study showed that the synthetic statin, atorvastatin, prevent the development of vasospasm. The authors suggested a reduced expression of caspase-3 and -8 [11].
Following the animal studies, several trials were achieved in humans (Table 1). In a retrospective study, 115 aneurysmal SAH patients were included, and 13% was receiving statin therapy for at least 1 month before bleeding. The patients with statins experienced less symptomatic vasospasms. The statin therapy on admission produced an odds ratio (OR) for reduction in the risk of symptomatic vasospasm of 0.09 [95% confidence interval (CI), 0.01–0.77] [60]. In a retrospective cohort (matched by age, Hunt and Hess grade at admission, vascular disease/risk history), 60 patients with aneurysmal SAH were examined. Twenty of these patients used statins before hemorrhage and 40 were controls. A reduction of delayed ischemia or vasospasms defined by angiography (30%) or Doppler (33%) was observed and cerebral infarctions of any type were 35% less frequent. Regarding outcome, the statin users showed a significantly better Barthel Index scale on day 14 [73]. Both studies did not consider the dose or type of statin.
Tseng et al. conducted the first randomized clinical trial in 80 aneurysmal SAH patients assigned within 72 h to pravastatin (40 mg) or placebo daily for up to 14 days. The incidences of vasospasm and severe vasospasm were reduced by 32% and 42%, respectively, and the duration of impaired autoregulation was shortened bilaterally. The incidence of vasospasm-related delayed ischemic deficits and mortality was decreased by 83% and 75%, respectively [96]. In a later work, they suggested that the vascular effects of statins are cholesterol independent [98]. Finally, they demonstrated a reduction of unfavorable outcome of 73% at discharge and 71% at 6 months [97]. In another randomized clinical trial with 39 aneurysmal SAH patients allocated within 48 h to simvastatin 80 mg daily by 14 days or placebo, a reduction of clinical vasospasms of 34% confirmed by angiography or transcranial Doppler was described [55]. Recently, a double-blind randomized trial included 39 patients with a Fisher grade 3 SAH, who were allocated to receive simvastatin 80 mg/day (n = 19) or placebo (n = 20). The mortality rate was 0% in the simvastatin group versus 15% in placebo. Differences of 14% (40% placebo versus 26% statin) concerning angiographically confirmed vasospasm and of 15% (25% placebo versus 10% statin) concerning vasospasm-related ischemic infarcts were reported [12].
Interestingly, Kramer et al. did not find any association with improvement or delayed ischemia. Their conclusion, however, was based on a retrospective cohort with slight unbalanced characteristics [43]. In another retrospective study with 308 patients, the age was unbalanced, showing a mean age higher in the statin group. In this study, vasospasm was observed in 31% of patients without statin in comparison to 23% of patients taking a statin [65]. A meta-analysis of three available randomized clinical trials (RTC) determined that the incidence of vasospasm after statin administration is significantly reduced [relative risk (RR) = 0.73; 95% CI, 0.54–0.99] as well as the delayed ischemic deficits (RR = 0.38; 95% CI, 0.17–0.83) and the mortality (RR = 0.22; 95% CI, 0.06–0.82) [81].
After this meta-analysis, another study appeared in which patients treated with pravastatin were compared with control patients without statin. No positive influence of statins was observed in the incidence of vasospasm in global outcome. In this way, the author argued about the uncertainness of the statins’ use for therapy after subarachnoid hemorrhage [37]. The conclusion, despite reasonable, is based on a study with unclear methodology. It was not randomized and the bias should be great if two series of patients treated after a great time distant were compared. The findings of this study, however, are partially supported by a relative new prospective, randomized, double-blind, placebo-controlled trial. This is the study of Verwougen et al., which was an attempt to assess the pleiotropic effects of statins as acute treatment in SAH patients. In this trial, patients received simvastatin 80 mg or placebo once daily. In a small homogeneous sample size of 32 patients, significant differences for total cholesterol and low-density lipoprotein were found [101]. The assessed parameters of coagulation, fibrinolysis, endothelium function, and inflammation were not different between both groups. Regarding clinical aspects, no differences were observed. A disadvantage of this study is its negative conclusion, which is not totally supported by the results because the trial was not primarily designed to determine clinical effectiveness. Despite systemic markers demonstrated as not altered in this study, the participation of local phenomena is not excluded. For instance, local regulation of NOS sub-types in the microvascular vessels [46], of a fibrinolytic/anti-thrombotic effect more microvascular than systemic [3, 36, 88], or of oxidases and dismutases may be possible explanations. These important actions were not considered by the study [27]. Recently, the existence of a natural domain for statin has been suggested, which leads to conformational changes of LFA-1, a relevant leukocyte activator molecule [107]. The participation of that in vasospasm is unclear and the existence of similar binding sites with other molecules is unknown.
In a population-based case–control study in the Netherlands, Risselada et al. have shown that statin consumers did not display a higher risk of SAH, and recent withdrawal was associated with an increased risk of SAH [76]. This evidence could be matched with the randomized prospective study of Blanco et al., where statin therapy was finished in acute stroke phase. This trial overwhelmingly demonstrated that statin withdrawal significantly worsens the clinical progression and functional outcome [5].
More recently, a meta-analysis of four randomized clinical trials (RCTs), two "pseudo" RCTs, five cohort studies, and one case–control study showed interesting differences. If only RCTs were analyzed, a profit can be demonstrated, but the analysis of the observational studies does not provide any definitive recommendation. The combination of all the trials as well did not present statistical significance [42]. In this way, the meta-analysis of only RCTs shows the same tendency as the previous meta-analysis. The possible implicit bias included in observational studies could explain the controversies.
Up to now, the biggest series of patients was published by McGuirt in 2009 [61]. The prospective cohort with 340 patients was unable to demonstrate a statistical difference in vasospasm or clinical outcome at discharge by using simvastatin 80 mg. This cohort study recruited one group between 2003 and 2005, which was compared with another group recruited between 2005 and 2008. The second one additionally received simvastatin. Contrary to a previous study of the same investigators, a benefit was not found. The authors recognized the lack of randomization in the study, which precludes level I evidence of the results. In this paper, the authors finally suggested many positive effects of statin therapy, and the clinical benefit of these agents may manifest with longer follow-up or as improved general functions months after SAH. In this way, studies assessing long-term outcomes are warranted, considering that the best evidence generated from randomized prospective clinical trials is enhanced by the evidence of negative effects of statin therapy withdrawal in SAH and stroke. It should be through the use of statins after SAH, specifically in regards to the limited alternative therapeutic options against vasospasms and the tolerability of statins. The results of SimvaSTatin in Aneurysmal Subarachnoid Hemorrhage (STASH), a large phase III trial, may provide a definitive conclusion [86].
Intracerebral hemorrhage
The initial experimental evidence generated in animals appeared in a couple of studies in 2004. In one of them, atorvastatin was administered orally beginning 24 h after intracerebral hemorrhage (ICH) and continued daily for 1 week. With low dose of 2 mg/kg, a significant reduction of neurological deficit at 2 to 4 weeks after the ICH was observed, while higher doses of 8 mg/kg did not improve functional outcome or reduce the brain damage [80]. In another study, atorvastatin was examined at 1 and 10 mg/kg for 2 weeks after induced ICH. Consistent with the previous study, a best development of sensomotoric deficits was observed. An effect on hematoma growth was not identified, but total brain water and atrophy were reduced, suggesting a possible limitation of edema formation and neuronal death [32]. A comparison of simvastatin and atorvastatin showed with both two substances a significant improvement with a slight superiority of simvastatin [33].
Supported by these studies, initial attempts at evaluating the effect on humans were accomplished (Table 1). In a retrospective study performed in Johns Hopkins Hospital, the effect of statin given prior to ICH was assessed in 125 consecutive ICH patients. The authors found that patients with prior statin had a smaller perifocal edema in comparison to those without statins. The multivariate analysis showed a significant correlation between prior statin and the reduction of early absolute edema volume [68]. The same group demonstrated that prior use of statins was associated with lower mortality at 30 days. They calculated an odds ratio greater than 12-fold for survival [69]. A third retrospective study of 629 consecutive ICH patients with 24% users of statins before ICH did not find differences on rates of functional independence (28% versus 29%) or mortality (46% versus 45%). Importantly, survivors treated with statins after discharge did not have a higher risk of rebleeding (hazard ratio 0.82, 95% CI, 0.34–1.99) [18].
A prospective series of 18 hypertensive ICH patients treated with rosuvastatin 20 mg for 7 days was compared with 57 retrospective controls. In this study, the mortality rate during hospitalization was lower (difference 10%) and the tendency was sustained at 30 days. A small difference concerning outcome, assessed by National Institute Health Stroke Scale (NIHSS) was observed. The multivariate analysis showed a positive correlation of statin use with the assessed outcomes, especially the possibility to achieve a better NIHSS result (<15) [90]. Recently, the National Acute Stroke Israeli Surveys (NASIS) analyzed data of patients admitted to 28 hospitals between 2003 and 2007. Among 312 ICH patients, 89 of them were receiving statins at the time of the ICH. These patients with statins had a better baseline neurological status (NIHSS <15). An OR of 2.97 for having good outcome (95% CI, 1.25–7.35) at discharge and an OR of 0.25 for death or discharge in a nursing facility (95% CI, 0.09–0.63) were calculated [48]. A consecutive study of this last group compared prior users of statins with non-users. Despite the fact that this trial was able to find lower hematoma volumes and mortality rates, no significant differences were detected by multivariate analysis [15]. A recent study from Spain showed in a retrospective series a significantly better outcome after ICH if statins were used before ICH [23].
Up to now, no randomized clinical trial or epidemiological data present an evidence for the association between low cholesterol and the occurrence of ICH [28, 47, 109, 111]. A population meta-analysis from 29 cohorts in the Asia-Pacific region showed a decreased risk of fatal hemorrhagic stroke with each 1-mmol/l higher level of total cholesterol [113].
The clinical trials with statins that have reduced the cholesterol levels below 70 mg/dl, however, did not find an association with ICH incidence [106, 108, 109]. The Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) study revealed that stroke (fatal and non-fatal) was significantly reduced by 16% on atorvastatin therapy [1]. An extension analysis of SPARCL effectively demonstrated an increased risk of ICH in patients treated with high dose of atorvastatin, especially in those with a previous hemorrhagic stroke, in men, and in those with increased age. Patients with stage II hypertension prior to ICH also have an increased risk (1.6-fold) [22]. A meta-analysis of data from 90,056 individuals in 14 randomized trials of statins demonstrated the reduction in the incidence of first stroke of any type, but no significant difference in hemorrhagic stroke was found [4].
The available data suggest that a low dose of statin during acute phase might be enough to achieve the neuroprotective/restorative effects of statins. In contrast to the therapy for years during SPARCL, a treatment for just some days or weeks seems to be enough for acute management of ICH. In the USA, a study is currently assessing the effect of simvastatin on radiological progression of ICH; similar studies have been required [13].
Traumatic brain injury
Regarding traumatic brain injury (TBI), the experimental studies in animals are broad, although scarce on humans. Rats treated with oral atorvastatin at 1 mg/kg/day after injury and for seven consecutive days demonstrated after 14 days a significant reduction in neurological functional deficits, increase in neuronal survival, and synaptogenesis in the boundary zone of the lesion and in the hippocampus [51]. The same group has described improved perfusion of vessels, reduced intravascular coagulation, prompt recovery of spatial memory, and a quicker resolution of contusions [52, 53]. Wang et al. compared two statins, atorvastatin (20 mg/kg) and simvastatin (20 mg/kg). They reported a reduction in functional neurological deficits, diminished hippocampal degeneration, and suppression of inflammatory cytokine mRNA expression in parenchyma [103]. Another study with simvastatin administered orally at a dose of 1 mg/kg starting at day 1 after TBI and daily for 14 days showed an increased phosphorylation of protein kinases B (Akt), glycogen synthase kinase-3β (GSK-3β), and cAMP response element-binding proteins; increase in cell proliferation and differentiation; and enhanced recovery of spatial learning [110]. Recently, a study with simvastatin confirmed the positive effects in rats after TBI, which was related with the reduction of IL-6, IL-1β, and TNF-α [49]. It has been proposed that simvastatin is superior to atorvastatin for improving spatial learning. This difference could be related to pharmacological properties [54, 59]. Finally, pre-treatment with lovastatin (4 mg/kg) showed similar effects on TBI [10].
Recently, only one very small randomized clinical trial in humans was published. This study included 21 patients with TBI and Glasgow coma score between 9 and 13. Eight patients were treated with rosuvastatin (20 mg single dose daily) within 24 h after injury, and 13 were control patients. The main objective of the trial was the assessment of the amnesia time using the Galveston Orientation Amnesia Test. The proportion of patients with quicker recovery of memory and orientation was higher in the statin group. Multivariate Cox survivor analysis showed an increased probability for recovery of orientation and for decrease of amnesia [91]. In this study, an immunological explanation was supposed. More studies are urgently required before a generalized application can be suggested. This might be difficult for TBI because of the great variability/bias involved. Small clinical studies in a selected group of patients with excellent methodology should provide information about the real role of statins in this affection. A meaningful limitation could result from the galenic formulation of the medicaments that can only be orally administered. The interest of pharmaceutical companies should be attracted to this field.
Glioblastoma multiforme and other tumors
Initial experimental data suggested a potential carcinogenicity and mutagenicity of statins, but other in vitro and in vivo studies have suggested that statins might exert an anti-carcinogenic effect. The data regarding cancer risk after statin administration are confusing [44, 57, 67, 77, 82, 93].
On the other hand, effects on angiogenesis, inhibition of tumor growth, and induction of apoptosis have been described. This anti-tumor activity is dose-related, variable for each statin, and importantly depends on the kind of tumor. Therapeutic assessment in several kinds of tumors has been evaluated; some trials are positive, another unable to detect differences but demonstrate tolerance of the employed doses, and others show some toxicity symptoms (for review, see reference [26]).
Regarding glioblastoma multiforme, the known abnormality of lipid metabolisms supported the intervention of cholesterol pathway as a therapeutic target [75]. Experiments on cell cultures suggested that the inhibition of farnesyl biosynthesis by statins is associated with inactivation of Ras pathway and reduction of MAPK activity [7, 29, 31] (Fig. 2). Additionally, the statins are able to disrupt the actin stress fibers and focal adhesion plaques even at nanomolar concentrations [21, 70] as well as induce apoptosis and cell-cycle arrest [9, 66, 83]. Figure 2 shows the possible molecular pathways involved by statins, which could explain the anti-tumor effects. A summary of the studies in glioma cells with statins is provided in Table 2.
Summary of pathways regulated by statins. The main mechanism (green) implicates the synthesis of isoprenoids as geranylgeranyl pirophosphate (GGPP) and farnesyl pyrophosphate (FPP). The Ras-MAPK cascade and related Raf-1, Rho, Rac (blue) are down-regulated through protein prenylation; in this way, the proliferation rate could decrease. Up to now, the molecules related to control of Akt-mTor are unknown, although this has been described as a possible regulation point. Statins are able to activate the PPARs (peroxisomal proliferation activator receptor) through the p38. The PPARs modulation is an important center for gene regulation, which controls multiple cell-cycle proteins through Wnt/β-catenin pathway. By targeting PPARs or other pathways, statins can regulate caspases and induce apoptosis. The exact mechanism is unknown yet, but the participation of TRAIL (TNF-related apoptosis-inducing ligand) and related Bim proteins seems to be most probable. Statins could modulate IL-18 and other interleukins, which modulate the lymphocytic populations as natural killers (NK). Finally, statins decrease integrins formation by FAK (focal adhesion kinase) inhibition. CCAAT/enhancer binding proteins (C/EBP), cyclin-dependent kinase (CDK), glycogen synthase kinase-3 (GSK), histone deacetylases (HDAC), β-hydroxy-β-methylglutaryl coenzyme A (HMG CoA), interferon (IFN), interleukin (IL), mitogen-activated protein kinases (MAPK = Erk, MEK, MEEK), nuclear factor κβ (NF-κβ), phosphatidylinositol-3 kinase (PI3K), 3-phosphoinositide-dependent protein kinase (PDK), phospholipase C (PLC), protein kinase C (PKC), retinoid X receptor (RXR), tyrosine kinase receptor (TRK = VEGFR, IGF-1R, EGFR)
The combination of statin with other drugs such as thiazolidinediones, gefitinib, BCNU (N,N′-bis(2-chloroethyl)-N-nitrosourea), and β-interferon might increase the anti-tumor activity [8, 85, 112]. Proliferation inhibition of other kinds of tumors such as medulloblastoma and meningioma has been described [30, 56, 104, 105].
Only the results of one clinical trial accomplished in 1998 are available, in which 18 patients with glioma WHO III–IV were included. A scheme of lovastatin 20–30 mg/kg/day with and without radiotherapy was applied. Safety and tolerability of the used doses were reported. However, a minimal effect on response/survival was found [45]. The big weakness of this trial was the administered dose of the statin. In an animal study, Gabryś et al. showed that after administration of lovastatin 50 mg/kg, a tumor concentration between 0.023 and 0.41 μM can be obtained. Nevertheless, the tumor volume was reduced [20]. This lower dose could be an explanation for the poor results published by Larner et al. [45]. According to recent experimental studies and the pharmacological properties of lovastatin, a higher dose should be required [59]. In another recent Mexican phase II study in pediatric patients with brain stem tumors, the effects of four chemotherapeutic courses every 28 days consisting of thalidomide, fluvastatin (alternating every 14 days), and combined with carboplatin and vincristine every 14 days followed by radiotherapy were assessed. This complex schema allowed increasing survival at 24 months with significant tumor reduction [50]. The real part of statins in this very complex approach unfortunately had to be left unexplained.
Studies on malignant glioma are restricted to simvastatin and lovastatin. Currently, our group compares the effects of five different statins in cell culture experiments and in animal model in order to apply statins for therapy of glioblastoma in humans. Considerations about potency, dose, solubility, and blood–brain barrier permeability are important before planning a randomized clinical trial.
Other perspectives
Sepsis is a complex and multifaceted syndrome, where the activation of the immune system is associated and related to organ dysfunction. Sepsis-associated mortality is a worldwide leading cause of death, with reported case fatality rates ranging from 30% to 70% [95]. Surgical patients and especially those in intensive care units are the target for this disease. In regards to their pleiotropic properties, statins have been suggested as a potential adjuvant treatment. The suggestion is based on animal models, microorganism cultures, human experimental data, and observational studies. A reduction in overall incidence and severe forms of sepsis has been reported [94]. An extensive review was recently published by Kopterides and Malagas, who analyzed the available studies and provided a list of seven ongoing studies [39].
Concerning lumbar back pain and disc disease, several immunological abnormalities are discussed regarding pathogenesis, even though this issue is poorly understood. Many publications have suggested a central role for monocytes/macrophages on the disease’s progression [2, 25, 35, 38, 78, 89, 102]. Considering this inflammatory background, ten patients with disc herniation-induced severe sciatica receiving an anti-TNF-α (infliximab) were examined and compared to 62 historical control patients. After 1 h the leg pain had decreased by 50%, and after 2 weeks 60% of the infliximab patients were painless versus only 16% of the controls. This difference remains up to 3 months [34]. Following these positive results, the Finnish Infliximab Related Study was performed. In this examination of infliximab, patients with disc herniation-induced sciatica did not show substantial differences on assessed aspects [40]. The disappointing results of this study could be originated by methodological aspects such as a small number of patients. Additionally, time with pain, symptoms at allocation, and anatomical segmental variability such as those suggested in animal studies were not considered for randomization [99]. Statins have been used in chronic arthropathies such as rheumatoid arthritis, where many cytokines and other inflammatory molecules participate [24, 64]. A small study of patients with ankylosing spondylitis who were treated with rosuvastatin suggested the control of the disease’s activity [58, 100]. In consideration of the immunomodulation that may be generated by statins and the hypothesis of a relation between inflammation and progression of disc disease, experimental or epidemiological studies may be promising [24, 89, 99].
Spinal cord injury is another interesting target where statins could find an application. Studies with atorvastatin demonstrated inflammatory modulation and neuroprotection, seen as a motor recovery in rats [71, 72]. Apoptosis prevention by modulating caspase 3 has been implicated as a possible action mechanism [14]. Studies with other statins and attempts in humans are missing.
Finally, results from animal models assessing cerebral ischemia showed that a pre-treatment with statins reduces the ischemia-related consequences [16]. This aspect may be interesting, especially in a neurosurgical context, because elected patients planned for a sophisticated neurosurgical operation might profit of this prophylactic effect. A trial for proving such effect, however, could be very difficult, since multiple factors are influencing the outcome after a neurosurgical procedure. Considering the current evidence of cardiovascular and neurovascular protection with a reasonable pharmacological safety, the use as pre-surgically admitted adjuvant might be thinkable.
In conclusion, statins are interesting, intriguing drugs, which could profit in different directions to neurosurgical patients. Despite growing evidence, more experimental explanations and clinical trials are needed so far.
References
Amarenco P, Bogousslavsky J, Callahan A 3rd, Goldstein LB, Hennerici M, Rudolph AE, Sillesen H, Simunovic L, Szarek M, Welch KM, Zivin JA, The Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) Investigators (2006) High-dose atorvastatin after stroke or transient ischemic attack. N Engl J Med 355:549–559
Arai Y, Yasuma T, Shitoto K, Yamauchi Y, Suzuki G (2000) Immunohistopathological study of intervertebral herniation of lumbar spine. J Orthop Sci 5:229–231
Asahi M, Huang Z, Thomas S, Yoshimura S, Sumii T, Mori T, Qiu J, Amin-Hanjani S, Huang PL, Liao JK, Lo EH, Moskowitz MA (2005) Protective effects of statins involving both eNOS and tPA in focal cerebral ischemia. J Cereb Blood Flow Metab 25:722–729
Baigent C, Keech A, Kearney PM, Blackwell L, Buck G, Pollicino C, Kirby A, Sourjina T, Peto R, Collins R, Simes R, Cholesterol Treatment Trialists’ (CTT) Collaborators (2005) Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet 366:1267–1278
Blanco M, Nombela F, Castellanos M, Rodriguez-Yáñez M, García-Gil M, Leira R, Lizasoain I, Serena J, Vivancos J, Moro MA, Dávalos A, Castillo J (2007) Statin treatment withdrawal in ischemic stroke: a controlled randomized study. Neurology 69:904–910
Bösel J, Gandor F, Harms C, Synowitz M, Harms U, Djoufack PC, Megow D, Dirnagl U, Hörtnagl H, Fink KB, Endres M (2005) Neuroprotective effects of atorvastatin against glutamate-induced excitotoxicity in primary cortical neurones. J Neurochem 92:1386–1398
Bouterfa HL, Sattelmeyer V, Czub S, Vordermark D, Roosen K, Tonn JC (2000) Inhibition of Ras farnesylation by lovastatin leads to downregulation of proliferation and migration in primary cultured human glioblastoma cells. Anticancer Res 20:2761–2771
Cemeus C, Zhao TT, Barrett GM, Lorimer IA, Dimitroulakos J (2008) Lovastatin enhances gefitinib activity in glioblastoma cells irrespective of EGFRvIII and PTEN status. J Neurooncol 90:9–17
Chan DY, Chen GG, Poon WS, Liu PC (2008) Lovastatin sensitized human glioblastoma cells to TRAIL-induced apoptosis. J Neurooncol 86:273–283
Chen SF, Hung TH, Chen CC, Lin KH, Huang YN, Tsai HC, Wang JY (2007) Lovastatin improves histological and functional outcomes and reduces inflammation after experimental traumatic brain injury. Life Sci 81:288–298
Cheng G, Wei L, Zhi-Dan S, Shi-Guang Z, Xiang-Zhen L (2009) Atorvastatin ameliorates cerebral vasospasm and early brain injury after subarachnoid hemorrhage and inhibits caspase-dependent apoptosis pathway. BMC Neurosci 10:7
Chou SH, Smith EE, Badjatia N, Nogueira RG, Sims JR 2nd, Ogilvy CS, Rordorf GA, Ayata C (2008) A randomized, double-blind, placebo-controlled pilot study of simvastatin in aneurysmal subarachnoid hemorrhage. Stroke 39:2891–2893
http://clinicaltrials.gov/ct2/show/NCT00718328. Accessed 06 Jan 2009.
Déry MA, Rousseau G, Benderdour M, Beaumont E (2009) Atorvastatin prevents early apoptosis after thoracic spinal cord contusion injury and promotes locomotion recovery. Neurosci Lett 453:73–76
Eichel R, Khoury ST, Ben-Hur T, Keidar M, Paniri R, Leker RR (2010) Prior use of statins and outcome in patients with intracerebral haemorrhage. Eur J Neurol 17:78–83
Endres M, Laufs U, Liao JK, Moskowitz MA (2004) Targeting eNOS for stroke protection. Trends Neurosci 27:283–289
Fandino J, Fathi AR, Graupner T, Jacob S, Landolt H (2007) Perspectives in the treatment of subarachnoid hemorrhage-induced cerebral vasospasm. Neurocirugía 18:16–27, Spanish
FitzMaurice E, Wendell L, Snider R, Schwab K, Chanderraj R, Kinnecom C, Nandigam K, Rost NS, Viswanathan A, Rosand J, Greenberg SM, Smith EE (2008) Effect of statins on intracerebral hemorrhage outcome and recurrence. Stroke 39:2151–2154
Fletcher B, Berra K, Ades P, Braun LT, Burke LE, Durstine JL, Fair JM, Fletcher GF, Goff D, Hayman LL, Hiatt WR, Miller NH, Krauss R, Kris-Etherton P, Stone N, Wilterdink J, Winston M, Council on Cardiovascular Nursing, Council on Arteriosclerosis, Thrombosis, and Vascular Biology, Council on Basic Cardiovascular Sciences, Council on Cardiovascular Disease in the Young, Council on Clinical Cardiology, Council on Epidemiology and Prevention, Council on Nutrition, Physical Activity, and Metabolism, Council on Stroke, Preventive Cardiovascular Nurses Association (2005) Managing abnormal blood lipids: a collaborative approach. Circulation 112:3184–3209
Gabryś D, Dörfler A, Yaromina A, Hessel F, Krause M, Oertel R, Baumann M (2008) Effects of lovastatin alone or combined with irradiation on tumor cells in vitro and in vivo. Strahlenther Onkol 84:48–53
Gliemroth J, Zulewski H, Arnold H, Terzis AJ (2003) Migration, proliferation, and invasion of human glioma cells following treatment with simvastatin. Neurosurg Rev 26:117–124
Goldstein LB, Amarenco P, Szarek M, Callahan A 3rd, Hennerici M, Sillesen H, Zivin JA, Welch KM, SPARCL Investigators (2008) Hemorrhagic stroke in the stroke prevention by aggressive reduction in cholesterol levels study. Neurology 70:2364–2370
Gomis M, Ois A, Rodríguez-Campello A, Cuadrado-Godia E, Jiménez-Conde J, Subirana I, Dávalos A, Roquer J (2009) Outcome of intracerebral haemorrhage patients pre-treated with statins. Eur J Neurol 17:443–448
Greenwood J, Steinman L, Zamvil SS (2006) Statin therapy and autoimmune disease: from protein prenylation to immunomodulation. Nat Rev Immunol 6:358–370
Habtemariam A, Grönblad M, Virri J, Seitsalo S, Karaharju E (1998) Comparative immunohistochemical study of inflammatory cells in acute-stage and chronic-stage disc herniations. Spine 23:2159–2165
Hindler K, Cleeland CS, Rivera E, Collard CD (2006) The role of statins in cancer therapy. Oncologist 11:306–315
Hong H, Zeng JS, Kreulen DL, Kaufman DI, Chen AF (2006) Atorvastatin protects against cerebral infarction via inhibiting NADPH oxidase-derived superoxide in ischemic stroke. Am J Physiol Heart Circ Physiol 291:H2210–H2215
Iso H, Jacobs DR Jr, Wentworth D, Neaton JD, Cohen JD (1989) Serum cholesterol levels and six-year mortality from stroke in 350,977 men screened for the Multiple Risk Factor Intervention Trial. N Engl J Med 320:904–910
Jiang Z, Zheng X, Lytle RA, Higashikubo R, Rich KM (2004) Lovastatin-induced up-regulation of the BH3-only protein, Bim, and cell death in glioblastoma cells. J Neurochem 89:168–178
Johnson MD, Woodard A, Okediji EJ, Toms SA, Allen GS (2002) Lovastatin is a potent inhibitor of meningioma cell proliferation: evidence for inhibition of a mitogen associated protein kinase. J Neurooncol 56:133–142
Jones KD, Couldwell WT, Hinton DR, Su Y, He S, Anker L, Law RE (1994) Lovastatin induces growth inhibition and apoptosis in human malignant glioma cells. Biochem Biophys Res Commun 205:1681–1687
Jung KH, Chu K, Jeong SW, Han SY, Lee ST, Kim JY, Kim M, Roh JK (2004) HMG-CoA reductase inhibitor, atorvastatin, promotes sensorimotor recovery, suppressing acute inflammatory reaction after experimental intracerebral hemorrhage. Stroke 35:1744–1749
Karki K, Knight RA, Han Y, Yang D, Zhang J, Ledbetter KA, Chopp M, Seyfried DM (2009) Simvastatin and atorvastatin improve neurological outcome after experimental intracerebral hemorrhage. Stroke 40:3384–3389
Karppinen J, Korhonen T, Malmivaara A, Paimela L, Kyllönen E, Lindgren KA, Rantanen P, Tervonen O, Niinimäki J, Seitsalo S, Hurri H (2003) Tumor necrosis factor-alpha monoclonal antibody, infliximab, used to manage severe sciatica. Spine 28:750–754
Kawaguchi S, Yamashita T, Yokogushi K, Murakami T, Ohwada O, Sato N (2001) Immunophenotypic analysis of the inflammatory infiltrates in herniated intervertebral discs. Spine 26:1209–1214
Kearney D, Fitzgerald D (1999) The anti-thrombotic effects of statins. J Am Coll Cardiol 33:1305–1307
Kern M, Lam MM, Knuckey NW, Lind CR (2009) Statins may not protect against vasospasm in subarachnoid haemorrhage. J Clin Neurosci 16:527–530
Koike Y, Uzuki M, Kokubun S, Sawai T (2003) Angiogenesis and inflammatory cell infiltration in lumbar disc herniation. Spine 28:1928–1933
Kopterides P, Falagas ME (2009) Statins for sepsis: a critical and updated review. Clin Microbiol Infect 15:325–334
Korhonen T, Karppinen J, Paimela L (2006) The treatment of disc-herniation-induced sciatica with infliximab—one year follow up results of FIRST II, a randomized clinical trial. Spine 31:2759–2766
Koyuturk M, Ersoz M, Altiok N (2004) Simvastatin induces proliferation inhibition and apoptosis in C6 glioma cells via c-jun N-terminal kinase. Neurosci Lett 370:212–217
Kramer AH, Fletcher JJ (2009) Statins in the management of patients with aneurysmal subarachnoid hemorrhage: a systematic review and meta-analysis. Neurocrit Care 42(12):285–296
Kramer AH, Gurka MJ, Nathan B, Dumont AS, Kassell NF, Bleck TP (2008) Statin use was not associated with less vasospasm or improved outcome after subarachnoid hemorrhage. Neurosurgery 62:422–430
Lamprecht J, Wojcik C, Jakobisiak M, Stoehr M, Schrorter D, Paweletz N (1999) Lovastatin induces mitotic abnormalities in various cell lines. Cell Biol Int 23:51–60
Larner J, Jane J, Laws E, Packer R, Myers C, Shaffrey M (1998) A phase I–II trial of lovastatin for anaplastic astrocytoma and glioblastoma multiforme. Am J Clin Oncol 21:579–583
Laufs U, Endres M, Stagliano N, Amin-Hanjani S, Chui DS, Yang SX, Simoncini T, Yamada M, Rabkin E, Allen PG, Huang PL, Böhm M, Schoen FJ, Moskowitz MA, Liao JK (2000) Neuroprotection mediated by changes in the endothelial actin cytoskeleton. J Clin Invest 106:15–24
Lee SH, Bae HJ, Yoon BW, Kim H, Kim DE, Roh JK (2002) Low concentration of serum total cholesterol is associated with multifocal signal loss lesions on gradient-echo magnetic resonance imaging: analysis of risk factors for multifocal signal loss lesions. Stroke 33:2845–2849
Leker RR, Khoury ST, Rafaeli G, Shwartz R, Eichel R, Tanne D, NASIS Investigators (2009) Prior use of statins improves outcome in patients with intracerebral hemorrhage. Prospective data from the National Acute Stroke Israeli Surveys (NASIS). Stroke 40:2581–2584
Li B, Mahmood A, Lu D, Wu H, Xiong Y, Qu C, Chopp M (2009) Simvastatin attenuates microglial cells and astrocyte activation and decreases interleukin-1beta level after traumatic brain injury. Neurosurgery 65:179–186
López-Aguilar E, Sepúlveda-Vildósola AC, Betanzos-Cabrera Y, Rocha-Moreno YG, Gascón-Lastiri G, Rivera-Márquez H, Wanzke-del-Angel V, Cerecedo-Díaz F, de la Cruz-Yañez H (2008) Phase II study of metronomic chemotherapy with thalidomide, carboplatin–vincristine–fluvastatin in the treatment of brain stem tumors in children. Arch Med Res 39:655–662
Lu D, Goussev A, Chen J, Pannu P, Li Y, Mahmood A, Chopp M (2004) Atorvastatin reduces neurological deficit and increases synaptogenesis, angiogenesis, and neuronal survival in rats subjected to traumatic brain injury. J Neurotrauma 21:21–32
Lu D, Mahmood A, Goussev A, Schaller T, Qu C, Zhnag ZG, Li Y, Lu M, Chopp M (2004) Atorvastatin reduction of intravascular thrombosis, increase in cerebral microvascular patency and integrity, and enhancement of spatial learning in rats subjected to traumatic brain injury. J Neurosurg 101:813–821
Lu D, Mahmood A, Qu C, Goussev A, Lu M, Chopp M (2004) Atorvastatin reduction of intracranial hematoma volume in rats subjected to controlled cortical impact. J Neurosurg 101:822–825
Lu D, Qu C, Goussev A, Jiang H, Lu C, Schallert T, Mahmood A, Chen J, Li Y, Chopp M (2007) Statins increase neurogenesis in the dentate gyrus, reduce delayed neuronal death in the hippocampal CA3 region, and improve spatial learning in rat after traumatic brain injury. J Neurotrauma 24:1132–1146
Lynch JR, Wang H, McGirt MJ, Floyd J, Friedman AH, Coon AL (2005) Simvastatin reduces vasospasm after aneurysmal subarachnoid hemorrhage results of a pilot randomized clinical trial. Stroke 36:2024–2026
Macaulay RJ, Wang W, Dimitroulakos J, Becker LE, Yeger H (1999) Lovastatin-induced apoptosis of human medulloblastoma cell lines in vitro. J Neurooncol 42:1–11
MacDonald JS, Gerson RJ, Kornbrust DJ, Kloss MW, Prahalada S, Berry PH, Alberts AW, Bokelman DL (1988) Preclinical evaluation of lovastatin. Am J Cardiol 62:16J–27J
Maksymowych WP (2008) Do bisphosphonates and statins have a role in spondyloarthritis management? Curr Rheumatol Rep 10:364–370
Mason RP, Walter MF, Day CA, Jacob RF (2005) Intermolecular differences of 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors contribute to distinct pharmacologic and pleiotropic actions. Am J Cardiol 96(suppl):11F–23F
McGirt MJ, Blessing R, Alexander MJ, Nimjee SH, Woodworth GF, Friedman AH, Graffagnino C, Laskowitz DT, Lynch JR (2006) Risk of cerebral vasopasm after subarachnoid hemorrhage reduced by statin therapy: a multivariate analysis of an institutional experience. J Neurosurg 105:671–674
McGirt MJ, Garces Ambrossi GL, Huang J, Tamargo RJ (2009) Simvastatin for the prevention of symptomatic cerebral vasospasm following aneurysmal subarachnoid hemorrhage: a single-institution prospective cohort study. J Neurosurg 110:968–974
McGirt MJ, Lynch JR, Parra A, Sheng H, Pearlstein RD, Laskowitz DT, Pelligrino DA, Warner DS (2002) Simvastatin increases endothelial nitric oxide synthase and ameliorates cerebral vasospasm resulting from subarachnoid hemorrhage. Stroke 33:2950–2956
McGirt MJ, Pradilla G, Legnani FG, Thai QA, Recinos PF, Tamargo RJ, Clatterbuck RE (2006) Systemic administration of simvastatin after the onset of experimental subarachnoid hemorrhage attenuates cerebral vasospasm. Neurosurgery 58:945–951
Meroni PL, Ventura D (2004) Statins and autoimmune diseases. APLAR J Rheumatol 7:278–284
Moskowitz SI, Ahrens C, Provencio JJ, Chow M, Rasmussen PA (2009) Prehemorrhage statin use and the risk of vasospasm after aneurysmal subarachnoid hemorrhage. Surg Neurol 71(3):311–317
Murakami M, Goto T, Saito Y, Goto S, Kochi M, Ushio Y (2001) The inhibitory effect of simvastatin on growth in malignant gliomas—with special reference to its local application with fibrin glue spray in vivo. Int J Oncol 19:525–531
Narisawa T, Fukaura Y, Terada K, Umezawa A, Tanida N, Yazawa K, Ishikawa C (1994) Prevention of 1, 2-dimethylhydrazineinduced colon tumorigenesis by HMG-CoA reductase inhibitors, pravastatin and simvastatin, in ICR mice. Carcinogenesis 15:2045–2048
Naval NS, Abdelhak TA, Urrunaga N, Zeballos P, Mirski MA, Carhuapoma JR (2008) An association of prior statin use with decreased perihematomal edema. Neurocrit Care 8:13–18
Naval NS, Abdelhak TA, Zeballos P, Urrunaga N, Mirski MA, Carhuapoma JR (2008) Prior statin use reduces mortality in intracerebral hemorrhage. Neurocrit Care 8:6–12
Obara S, Nakata M, Takeshima H, Kuratsu J, Maruyama I, Kitajima I (2002) Inhibition of migration of human glioblastoma cells by cerivastatin in association with focal adhesion kinase (FAK). Cancer Lett 185:153–161
Pannu R, Barbosa E, Singh AK, Singh I (2005) Attenuation of acute inflammatory response by atorvastatin after spinal cord injury in rats. J Neurosci Res 79:340–350
Pannu R, Christie DK, Barbosa E, Singh I, Singh AK (2007) Post-trauma Lipitor treatment prevents endothelial dysfunction, facilitates neuroprotection, and promotes locomotor recovery following spinal cord injury. J Neurochem 101:182–200
Parra A, Kreiter KT, Williams S, Sciacca R, Mack WJ, Naidech AM (2005) Effect of prior statin use on functional outcome and delayed vasospasm after acute aneurysmal subarachnoid hemorrhage: a matched controlled cohort study. Neurosurgery 56:476–484
Paul F, Waiczies S, Wuerfel J, Bellmann-Strobl J, Dörr J, Waiczies H, Haertle M, Wernecke KD, Volk HD, Aktas O, Zipp F (2008) Oral high-dose atorvastatin treatment in relapsing–remitting multiple sclerosis. PLoS ONE 3:e1928
Prasanna P, Thibault A, Liu L, Samid D (1996) Lipid metabolism as a target for brain cancer therapy: synergistic activity of lovastatin and sodium phenylacetate against human glioma cells. J Neurochem 66:710–716
Risselada R, Straatman H, van Kooten F, Dippel DW, van der Lugt A, Niessen WJ, Firouzian A, Herings RM, Sturkenboom MC (2009) Withdrawal of statins and risk of subarachnoid hemorrhage. Stroke 40:2887–2892
Robison RL, Suter W, Cox RH (1994) Carcinogenicity and mutagenicity studies with fluvastatin, a new, entirely synthetic HMG-CoA reductase inhibitor. Fundam Appl Toxicol 23:9–20
Rothoerl R, Woertgen C, Holzschuh M, Brehme K, Rüschoff J, Brawanski A (1998) Macrophage tissue infiltration, clinical symptoms, and signs in patients with lumbar disc herniation. A clinicopathological study on 179 patients. Acta Neurochir (Wien) 140:1245–1248
Scheen AJ, Radermecker RP, Sadzot B (2008) Statin for the brain: update in 2008. Rev Méd Liège 63:287–292, French
Seyfried D, Han Y, Lu D, Chen J, Bydon A, Chopp M (2004) Improvement in neurological outcome after administration of atorvastatin following experimental intracerebral hemorrhage in rats. J Neurosurg 101:104–107
Sillberg VA, Wells GA, Perry JJ (2008) Do statins improve outcomes and reduce the incidence of vasospasm after aneurysmal subarachnoid hemorrhage: a meta-analysis. Stroke 39:2622–2626
Smith PF, Grossman SJ, Gerson RJ, Gordon LR, Deluca JG, Majka JA, Wang RW, Germershausen JI, MacDonald JS (1991) Studies on the mechanism of simvastatin-induced thyroid hypertrophy and follicular cell adenoma in the rat. Toxicol Pathol 19:197–205
Soma MR, Baetta R, Bergamaschi S, De Renzis MR, Davegna C, Battaini F, Fumagalli R, Govoni S (1994) PKC activity in rat C6 glioma cells: changes associated with cell cycle and simvastatin treatment. Biochem Biophys Res Commun 200:1143–1149
Soma MR, Baetta R, De Renzis MR, Mazzini G, Davegna C, Magrassi L, Butti G, Pezzotta S, Paoletti R, Fumagalli R (1995) In vivo enhanced antitumor activity of carmustine [N, N′-bis(2-chloroethyl)-N-nitrosourea] by simvastatin. Cancer Res 55:597–602
Soma MR, Pagliarini P, Butti G, Paoletti R, Paoletti P, Fumagalli R (1992) Simvastatin, an inhibitor of cholesterol biosynthesis, shows a synergistic effect with N, N′-bis(2-chloroethyl)-N-nitrosourea and beta-interferon on human glioma cells. Cancer Res 52:4348–4355
http://www.stashtrial.com/home.html. Accessed 12 Sep 2009
Sugawara T, Ayer R, Jadhav V, Chen W, Tsubokawa T, Zhang JH (2008) Simvastatin attenuation of cerebral vasospasm after subarachnoid hemorrhage in rats via increased phosphorylation of Akt and endothelial nitric oxide synthase. J Neurosci Res 86:3635–3643
Szapary L, Horvath B, Marton Z, Alexy T, Kesmarky G, Habon T, Szots M, Koltai K, Juricskay I, Czopf J, Toth K (2004) Short-term effect of low-dose atorvastatin on haemorrheological parameters, platelet aggregation and endothelial function in patients with cerebrovascular disease and hyperlipidaemia. CNS Drugs 18:165–172
Tapia-Pérez H (2008) Intervertebral disc pathologies from an immunological perspective. Rev Neurol 46:751–757, Spanish
Tapia-Pérez JH, Sánchez-Aguilar M, Torres-Corzo JG, González-Aguirre D, Gordillo-Moscoso A, Rodríguez-Leyva I, Chalita-Williams JC (2009) Use of statins for the treatment of spontaneous intracerebral hemorrhage: results of a pilot study. Cen Eur Neurosurg 70:15–20
Tapia-Pérez JH, Sanchez-Aguilar M, Torres-Corzo JG, Gordillo-Moscoso A, Martinez-Perez P, Madeville P, de la Cruz-Mendoza E, Chalita-Williams J (2008) Effect of rosuvastatin on amnesia and disorientation after traumatic brain injury (NCT003229758). J Neurotrauma 25:1011–1017
Tapia-Pérez H, Sanchez-Aguilar M, Torres-Corzo J, Rodriguez-Leyva I, Herrera-Gonzalez LB (2007) Statins and brain protection mechanisms. Rev Neurol 45:359–364, Spanish
Tatsuta M, Iishi H, Baba M, Iseki K, Yano H, Uehara H, Yamamoto R, Nakaizumi A (1998) Suppression by pravastatin, an inhibitor of p21ras isoprenylation, of hepatocarcinogenesis induced by N-nitrosomorpholine in Sprague–Dawley rats. Br J Cancer 77:581–587
Terblanche M, Almog Y, Rosenson RS, Smith TS, Hackam DG (2006) Statins: panacea for sepsis? Lancet Infect Dis 6:242–248
Terblanche M, Almog Y, Rosenson RS, Smith TS, Hackam DG (2007) Statins and sepsis: multiple modifications at multiple levels. Lancet Infect Dis 7:358–368
Tseng MY, Czosnyka M, Richards H, Pickard JD, Kirkpatrick PJ (2005) Effects of acute treatment with pravastatin on cerebral vasospasm, autoregulation, and delayed ischemic deficits after aneurysmal subarachnoid hemorrhage: a phase II randomized placebo-controlled trial. Stroke 36:1627–1632
Tseng MY, Hutchinson PJ, Czosnyka M, Richards H, Pickard JD, Kirkpatrick PJ (2007) Effects of acute pravastatin treatment on intensity of rescue therapy, length of inpatient stay, and 6-month outcome in patients after aneurysmal subarachnoid hemorrhage. Stroke 38:1545–1550
Tseng MY, Hutchinson PJ, Turner CL, Czosnyka M, Richards H, Pickard JD, Kirkpatrick PJ (2007) Biological effects of acute pravastatin treatment in patients after aneurysmal subarachnoid hemorrhage: a double-blind, placebo-controlled trial. J Neurosurg 107:1092–1100
Ulrich JA, Liebenberg EC, Thuillier DU, Lotz JC (2007) ISSLS prize winner: repeated disc injury causes persistent inflammation. Spine 32:2812–2819
van Denderen JC, Peters MJ, van Halm VP, van der Horst-Bruinsma IE, Dijkmans BA, Nurmohamed MT (2006) Statin therapy might be beneficial for patients with ankylosing spondylitis. Ann Rheum Dis 65:695–696
Vergouwen MD, Meijers JC, Geskus RB, Coert BA, Horn J, Stroes ES, van der Poll T, Vermeulen M, Roos YB (2009) Biologic effects of simvastatin in patients with aneurysmal subarachnoid hemorrhage: a double-blind, placebo-controlled randomized trial. J Cereb Blood Flow Metab 29:1444–1453
Virri J, Grönblad M, Seitsalo S, Habtemariam A, Kääpä E, Karaharju E (2001) Comparison of the prevalence of inflammatory cells in subtypes of disc herniations and associations with straight leg raising. Spine 26:2311–2315
Wang H, Lynch JR, Song P, Yang HJ, Yates RB, Mace B, Warner DS, Guyton JR, Laskowitz DT (2007) Simvastatin and atorvastatin improve behavioral outcome, reduce hippocampal degeneration, and improve cerebral blood flow after experimental traumatic brain injury. Exp Neurol 206:59–69
Wang W, Macaulay RJ (1999) Mevalonate prevents lovastatin-induced apoptosis in medulloblastoma cell lines. Can J Neurol Sci 26:305–310
Wang W, Macaulay RJ (2003) Cell-cycle gene expression in lovastatin-induced medulloblastoma apoptosis. Can J Neurol Sci 30:349–357
Waters DD (2005) Safety of high-dose atorvastatin therapy. Am J Cardiol 96(suppl):69F–75F
Weitz-Schmidt G, Welzenbach K, Dawson J, Kallen J (2004) Improved lymphocyte function-associated antigen-1 (LFA-1) inhibition by statin derivatives: molecular basis determined by x-ray analysis and monitoring of LFA-1 conformational changes in vitro and ex vivo. J Biol Chem 279:46764–46771
Wiviott SD, Cannon CP, Morrow DA, Ray KK, Pfeffer MA, Braunwald E, PROVE IT-TIMI 22 Investigators (2005) Can low-density lipoprotein be too low? The safety and efficacy of achieving very low low-density lipoprotein with intensive statin therapy: a PROVE IT-TIMI 22 substudy. J Am Coll Cardiol 46:1411–1416
Woo D, Kissela BM, Khoury JC, Sauerbeck LR, Haverbusch MA, Szaflarski JP, Gebel JM, Pancioli AM, Jauch EC, Schneider A, Kleindorfer D, Broderick JP (2004) Hypercholesterolemia, HMG-CoA reductase inhibitors, and risk of intracerebral hemorrhage: a case–control study. Stroke 35:1360–1364
Wu H, Lu D, Jiang H, Xiong Y, Qu C, Li B, Mahmood A, Zhou D, Chopp M (2008) Simvastatin-mediated upregulation of VEGF and BDNF, activation of the PI3K/Akt pathway, and increase of neurogenesis are associated with therapeutic improvement after traumatic brain injury. J Neurotrauma 25:130–139
Yano K, Reed DM, MacLean CJ (1989) Serum cholesterol and hemorrhagic stroke in the Honolulu Heart Program. Stroke 20:1460–1465
Yao CJ, Lai GM, Chan CF, Cheng AL, Yang YY, Chuang SE (2006) Dramatic synergistic anticancer effect of clinically achievable doses of lovastatin and troglitazone. Int J Cancer 118:773–779
Zhang X, Patel A, Horibe H, Wu Z, Barzi F, Rodgers A, MacMahon S, Woodward M, Asia Pacific Cohort Studies Collaboration (2003) Cholesterol, coronary heart disease, and stroke in the Asia Pacific region. Int J Epidemiol 32:563–572
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Atos Alves de Sousa, Rafael Augusto Castro Santiago Brandão, Belo Horizonte, Brazil
Tapia-Perez et al. have done an excellent job when researching into and grouping the most updated literature on the application of statins in neurosurgical diseases. The current use of statins is well established in the prevention of cardiovascular diseases and dyslipidemia, and even though their application in several neurological pathologies is still being studied, it seems that their potential benefits are progressively becoming clear. In the beginning of the 1970s, the microbiologist Akira Endo1 was searching for a new antibiotic when he observed that certain fungi were also capable of producing a strong inhibitor of cholesterol production. Endo isolated and analyzed this compound which gave origin to the matrix of statins. The importance of such discovery was not so clear at the time, but 39 years later many new benefits of these drugs are being reported. These points to the relevance of constant research on the already used medications, even after years after their initial description.
As well reported by the authors, the neuroprotector effects and anti-tumor activity of statins enlarge their field of application and open new opportunities for new research into the use of these substances. Their application to rachimedular traumas has not yet been studied in humans, but in animal models it has been associated to a better motor recovery and their positive effect on the inflammatory response has also been proved. Their benefit in neuro-oncology is still uncertain, but they have been related to inhibition of tumor cell proliferation and to apoptosis induction. According to the authors, the works that have been published were experimental or involved small series.
In regards to subarachnoid hemorrhage (SAH), randomized studies with large series so as to confirm the positive effects of statins have not been done yet. When analyzing the data displayed in Table 1, it is clear that the studies involve a small number of patients and so it is not possible to conclude anything yet. The largest series (340 patients) did not find any reduction in the incidence of symptomatic vasospasm or mortality, or any difference in SAH prognosis, comparing the control group and the simvastatin group. The results of phase II of STASH, with 80 patients, demonstrated a potential benefit of statins on SAH. But it is necessary to wait for the results of phase III in order to have a more consistent conclusion about the effects of statins on SAH.
Reference
1. Endo A. The origin of the statins. Atheroscler Suppl. 2004 Oct;5(3):125–30.
Susanne Mink, Zurich, Switzerland
In this comprehensive review, the authors summarize the research development regarding the effect of statins in neurosurgery. Statins are a remarkable group of drugs with multiple and very different primary and secondary effects. The increasing knowledge in the field of statins has significant implications for medicine in general, especially in neurosurgery.
Most often the published studies included only a small number of patients, and the results are controversial. But it seems to be of growing evidence that there is no beneficial effect of statins in the treatment of vasospasm in patients suffering from aneurysmal subarachnoid hemorrhage (Vergouwen et al. Stroke. 2010 Jan;41(1):e47–52). Furthermore, a recently published study of Danesh et al. (JAMA. 2009 Nov;302(18):1993–2000) provides convincing data that non-HDL cholesterol levels are modestly associated with ischemic stroke but not with hemorrhage. It is not only interesting to study different statins, but as well the different predictive values of other lipid markers, including novel apolipoproteins.
With this paper, the authors give us a succeeded update of the statin research results concerning neurosurgery and a useful overview with the tables of relevant neurosurgical topics and statin application studies.
Rights and permissions
About this article
Cite this article
Tapia-Pérez, J.H., Sanchez-Aguilar, M. & Schneider, T. The role of statins in neurosurgery. Neurosurg Rev 33, 259–270 (2010). https://doi.org/10.1007/s10143-010-0259-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-010-0259-4