Abstract
Background
There are knowledge gaps regarding the relative efficacy of statins for aneurysmal subarachnoid hemorrhage (aSAH). This study aims to examine the comparative effectiveness and determine the ranking of different statins with network meta‑analysis in patients with aSAH.
Methods
MEDLINE, Embase, Pubmed, and Cochrane Central Register of Controlled Trials were searched from database inception until December 15, 2022. Outcomes included delayed cerebral ischemia (DCI), functional recovery, and mortality. Relative risk (RRs) ratios and associated 95% confidence intervals (CIs) were estimated. The values derived from surface under the cumulative ranking curve were obtained to rank the treatment hierarchy in the analysis.
Results
We identified 13 trials involving 1,885 patients. Atorvastatin 20 mg (RR 0.68, 95% CI 0.53–0.86), pravastatin 40 mg (RR 0.51, 95% CI 0.31–0.77), and simvastatin 80 mg (RR 0.54, 95% CI 0.40–0.70) were superior to the placebo in preventing DCI. Additionally, simvastatin 80 mg (RR 0.60, 95% CI 0.42–0.84) and pravastatin 40 mg (RR 0.56, 95% CI 0.32–0.93) were associated with a decreased risk of DCI than simvastatin 40 mg. Comparisons across treatment durations suggested that short-term (RR 0.62, 95% CI 0.50–0.76) statin therapy reduced risk of DCI.
Conclusions
Simvastatin 80 mg might be the most effective intervention in reducing DCI. Additionally, short-term therapy might provide more benefits. Further research with longer follow-up is warranted to validate the current findings in patients with aSAH who are at high risk of DCI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Subarachnoid hemorrhage (SAH) occurs in approximately 9 per 100,000 people yearly, mainly due to the rupture of intracranial aneurysms [1, 2]. About half of patients with SAH are younger than 55 years old, with an inferior prognosis. Up to 75% of survivors of aneurysmal SAH (aSAH) will be left with significant neurological morbidity [3, 4]. Delayed cerebral ischemia (DCI), namely clinical or symptomatic vasospasm, is seen in approximately 20–40% of patients presenting with aSAH, and it is currently believed that DCI is the leading cause of neurological deficits and death in patients with aSAH [5,6,7].
To date, one systematic review has revealed that the prevention of DCI using statin agents effectively improves neurological and functional outcomes and reduces aSAH-related mortality after aSAH [8]. However, most of the current literature did not find that the use of statins improves functional outcomes. This may be attributed to the small population size or the neglect of important confounding factors, such as type and dosage of statin agents [9, 10]. Moreover, previous meta-analyses have been limited primarily to comparing the efficacy of a single agent with a placebo, without seeking to assess their relative effectiveness. To elucidate their comparative superiority, we performed this network meta-analysis of available randomized controlled trials (RCTs) to investigate the therapeutic benefits of different statins treatment in patients presenting with aSAH.
Materials and Methods
Protocol and Guidance
This study was registered with the Open Science Framework portal (https://osf.io/muhw6). The methods and reporting of the systematic review and meta-analysis followed Preferred Reporting Items for Systematic Reviews and Meta-analyses for Network Meta-analyses Extension Statement [11]. Ethical approval by our institutional review board was not required.
Selection Criteria
Eligible studies met the criteria of participants, interventions, comparators, outcomes, and study design. Patient: adult patients (age > 18 years old) with aSAH. Interventions: statin therapy. Dose and type were not limited. Comparisons and controls: placebo treatment, a different statin agent, or the same statin therapy with different dosages. Outcomes: mortality, unfavorable functional outcome (which was defined as Glasgow Outcome Scale score 1–3 or modified Rankin Scale score 3–6), and DCI (which was defined by each trial). Study design: RCTs.
Search Strategy
We searched PUBMED, EMBASE, and Cochrane Central Register of Controlled Trials from inception to December 15, 2022, without language restrictions. We also searched the clinical trial registration portal (ClinicalTrials.gov) and published systematic reviews on the same topic to identify additional studies (Table S1).
Selection Process
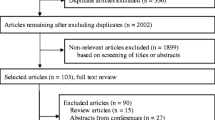
According to the Preferred Reporting Items for Systematic Reviews and Meta-analyses for Network Meta-analyses Extension Statement, two reviewers (XW and YC) excluded publications that were not eligible based on titles and abstracts after deleting duplicates. Then, full-text articles were reviewed by them; the articles were either included or excluded in the analysis based on inclusion and exclusion criteria. The reviewers independently completed this procedure. Conflicts in study selection were resolved by consensus; if the problem was not solved, a third independent reviewer (LM) would make the final decision.
Data Extraction
One reviewer extracted data from eligible studies into an Excel spreadsheet template. The concerning information related to study characteristics, patient characteristics, and treatment characteristics was collected. A second reviewer then checked the information table, and a third reviewer was assigned to examine a sample of 20% of the extracted data. Disagreements were addressed through discussion.
Assessment of Risk of Bias and Certainty of Evidence
We used the Cochrane Collaboration Risk of Bias 2.0 tool to assess the risk of bias in RCTs [12]. The overall risk of bias judgment (low risk of bias, some concerns, or high risk of bias) of the risk of bias tool was made based on five domain-level judgments. Additionally, the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach was applied to evaluate the overall certainty of evidence for each outcome [13]. This approach defines four levels of certainty rated “high,” “moderate,” “low,” or “very low” for each estimate depending on inconsistency, indirectness, imprecision, risk of bias, and publication bias. Two reviewers (XW and YC) completed this procedure. Disagreements regarding the risk of bias and GRADE evaluation were addressed through discussion. If the problem was not solved, a third independent reviewer (LM) would make the final decision.
Statistical Analysis
We used the parameters with four parallel Markov chains of 30,000 samples after a 10,000-sample burn-in for the primary analysis. Trace plots and Gelman–Rubin diagnostic statistics were applied to check the convergence of Markov chains. Model fit was assessed by comparing the posterior total residual deviance with the number of unconstrained data points. Because of the limited number of studies in all connections of the treatment network and given that model fit was adequate, fixed-effect models were considered first for all analyses [14]. We calculated and pooled relative risks (RRs) with 95% confidence intervals (CIs) for dichotomous outcomes.
Furthermore, the surface under the cumulative ranking curve (SUCRA) and forest plots were performed to evaluate and summarize the main results [15, 16]. The rank probabilities were also determined. Briefly, the treatment rankings were assessed by computing the overall SUCRA score for each agent. The magnitude of the SUCRA index can be used to guide drug selection, in which the treatments with the highest (the one closest to 1) and lowest (the one closest to 0) SUCRAs are considered the most and least effective, respectively. The possibility of publication bias was evaluated by a visual estimate of the funnel plot. We used Begg’s adjusted rank correlation test and Egger’s regression test to assess asymmetry of the funnel plot. Heterogeneity was evaluated by the Cochran Q statistic and measured using I2 statistics, which ranges between 0 and 100%. The global statistical heterogeneity across all comparisons was obtained from the established model.
Analyses were done with open-source R software (R Foundation, version 4.0.3), JAGS (version 4.3.1), and Review Manager (version 5.4.1). P values less than 0.05 were considered to represent statistical significance, and all P values were two-tailed.
Results
Eligible Studies and Study Characteristics
The systematic literature search identified 378 articles; nine additional articles were identified by screening the National Clinical Trial registration website. After screening the titles and abstracts of 216 references, 187 were excluded, which left 29 articles for assessment of the full-text articles. After screening and selection, we identified 13 RCTs eligible for inclusion in the systematic review [17,18,19,20,21,22,23,24,25,26,27,28,29]. Figure 1 presents details of the study selection process and reasons for exclusion.
Table 1 and Table S2 show the characteristics of the included trials. Three (23%) of the studies were conduected in the USA, three (23%) in China, two (15%) in the UK, and the others were conducted in Japan, India, Netherlands, Brazil, and Germany. The studies involved a median of 47 (range 20–803) patients with a median age of 54 (range 47–75.2) years. Nine (69%) studies involved more men participants, two (15%) involved more women participants, and two (15%) studies did not provide data on sex. Seven (54%) trials compared simvastatin against a placebo, two (15%) trials compared pravastatin against a placebo, two (15%) trials compared atorvastatin against a placebo, one (8%) trial compared pitavastatin against a placebo, and one (8%) trial compared two different doses of simvastatin. Seven (54%) trials administered statin therapy for 14 days, five (38%) trials for 21 days, and one (8%) trial did not provide data on treatment duration.
DCI
Across 13 two-group trials involving 1,885 patients that provided usable information, 236 (22.5%) patients developed DCI in the statin treatment group, and 294 (35.3%) developed DCI in the placebo group (Figs. S1 and S2). Atorvastatin 20 mg (RR 0.68, 95% CI 0.53–0.86), pravastatin 40 mg (RR 0.51, 95% CI 0.31–0.77), and simvastatin 80 mg (RR 0.54, 95% CI 0.40–0.70) resulted in a significant decrease in the incidence of DCI compared with a placebo. However, the results did not show a significant difference in the comparison of pitavastatin 4 mg versus a placebo (RR 0.76, 95% CI 0.53–1.07) or in simvastatin 40 mg versus a placebo (RR 0.90, 95% CI 0.68–1.19). Moreover, compared with simvastatin 40 mg, simvastatin 80 mg (RR 0.60, 95% CI 0.42–0.84) and pravastatin 40 mg (RR 0.56, 95% CI, 0.32–0.93) both were associated with lower risk of DCI (Fig. 2a). Sensitivity analysis was performed after excluding the trial with the smallest sample size. In general, the results remained consistent after excluding certain trial (Table S3). Global heterogeneity was presented in Table S4. No significant asymmetry of the funnel plot was observed in the comparison between simvastatin 80 mg and placebo, with the P value of 0.72 in Begg’s test and 0.65 in Egger’s test.
Pravastatin 40 mg (SUCRA 0.87; Fig. 2b) had the highest SUCRA value, suggesting it had the highest likelihood of being the best statin agent in the treatment of DCI; this result was also statistically significant. The second most preferable agent was simvastatin 80 mg (SUCRA 0.85), followed by atorvastatin 20 mg (SUCRA 0.57), pitavastatin 4 mg (SUCRA 0.43), and simvastatin 40 mg (SUCRA 0.22).
Functional Recovery
In ten trials involving 1,719 patients that provided usable information, 300 (30.7%) patients in the statin group and 253 (34.1%) in the placebo group reported unfavorable functional outcomes. Among them, three defined an unfavorable functional outcome as a Glasgow Outcome Scale score of 1–3; five defined the outcome as a modified Rankin Scale score of 3–6; and two did not provide relevant information (Table S2). Considering the disparity of follow-up to assess functional outcomes among included studies, we performed subgroup analysis based on different follow-up period. None of the comparisons were associated with significant differences in functional recovery (Fig. 3).
Mortality Outcome
Across 11 two-group trials involving 1,730 patients that provided usable information, 76 (7.8%) patients died in the statin treatment group and 83 (11.0%) died in the placebo group. Considering the disparity of follow-up to assess mortality among included studies, we performed subgroup analysis based on different follow-up period. None of the comparisons were associated with significant differences in mortality (Fig. 4).
Duration of Therapy and Dosage
Considering the contribution of treatment duration and dosage to end points, these factors were investigated in further analyses (Table 2). In general, treatment duration included 14 days (seven trials; 561 patients) and 21 days (five trials; 1,226 patients). Accordingly, short-term therapy with statin was defined as 14-day treatment; long-term therapy was defined as 21-day treatment. Overall, 11 studies involving 1,532 patients provided data on the duration of therapy. According to direct analysis, short-term duration of treatment (RR 0.54, 95% CI 0.35–0.84) was associated with reduced risk of DCI compared with placebo. Similarly, network analysis showed that compared with placebo, short-term therapy (RR 0.62, 95% CI 0.50–0.76) and long-term therapy (RR 0.74, 95% CI 0.60–0.90) both result in a decreased risk of DCI irrespective of the agent applied.
On the other hand, treatment regimens included simvastatin 20 mg, pitavastatin 4 mg, simvastatin 80 mg, simvastatin 40 mg, and pravastatin 40 mg. We defined low-dose therapy as simvastatin with ≤ 20 mg, atorvastatin with ≤ 10 mg, pravastatin with ≤ 40 mg, and pitavastatin with ≤ 2 mg [30]. Overall, 12 studies involving 1,630 patients provided data on the treatment dosage. The results from direct analysis revealed that high-dose therapy (RR 0.66, 95% CI 0.49–0.87) was associated with reduced risk of DCI compared with the placebo. Similar results were observed from network analysis. Both low-dose (RR 0.51, 95% CI 0.31–0.77) and high-dose treatments (RR 0.70, 95% CI 0.60–0.80) were associated with decreased risk of DCI.
Assessment of the Risk of Bias and Certainty of Evidence
The estimations of the overall bias of the included studies were generally low. Most studies had a low risk of bias. Three studies were assessed at high risk for inadequate allocation concealment and study blinding. The motivations guiding the assignment of the risk of bias judgments are available in Fig. S3–4 in the supplementary material.
Using the GRADE system (Table S5), the certainty of evidence score of simvastatin 80 mg versus placebo in reducing mortality was “moderate”; simvastatin 80 mg versus simvastatin 40 mg in reducing mortality was “low.” The certainty of evidence score was “moderate’” in the comparison of simvastatin 80 mg versus placebo in reducing DCI; “low” in the comparison of simvastatin 80 mg versus simvastatin 40 mg in reducing DCI; whereas that of atorvastatin 20 mg versus placebo, pitavastatin 4 mg versus placebo, and pravastatin 40 mg versus simvastatin 40 mg in reducing DCI was rated as “low.”
Discussion
Main Findings
To our knowledge, this is the largest network meta-analysis to date to systematically assess the effects of different statin agents in patients with aSAH (13 RCTs involving 1,885 participants). Our findings showed that atorvastatin 20 mg, pravastatin 40 mg, and simvastatin 80 mg might be more efficacious than placebo for reducing the risk of DCI. Moreover, our results suggested that pravastatin 40 mg, and simvastatin 80 mg significantly reduced the risk of DCI than simvastatin 40 mg. Additionally, our analysis suggested that patients with aSAH might obtain more benefits from short-term statin therapy in preventing DCI. Overall, the certainty of evidence ranged from low to moderate.
Comparison with Other Studies
To date, no prior network meta-analysis investigated the effects of statins for the prevention of DCI and mortality secondary to aSAH. Previous meta-analyses that investigated the effect of statin therapy after aSAH reported inconsistent results. Generally, in many previous meta-analyses, statin therapy was found to be associated with decreased risk of DCI. However, whether treatment with statins reduces mortality remains uncertain [8, 31, 32]. Recent systematic reviews have summarized the evidence for the management of DCI and death after SAH; however, they did not explore the comparative effectiveness of different treatment agents and did not consider the overall certainty of the evidence [10, 30]. The inconsistency between previous studies and the present findings might be explained by the following reasons. First, current studies may have been too small to draw solid conclusions, in other words, it is possible to get false negative results due to small sample size regarding functional outcomes. Thus, we use the trial sequential analysis to detect whether the cumulative data would be of sufficiently high power to evaluate the effect of statin on the functional outcomes [33]. The results demonstrated that more evidence was needed to draw firm conclusions (Fig. S5). Second, in the course of treatment with statins, an important factor of attention is the duration of therapy. Our study as well as current research showed the benefits of short-term therapy [10]. Previous studies have not considered this critical confounding factor, which may also account for the inconsistency with our findings. Third, in the present analysis, we applied a network approach to increase the precision of each effect estimate and make the best use of all available evidence to date. Overall, our network meta-analysis used a more comprehensive classification of statin agents, offering more precise details applied to specific drugs and generating more clinically relevant information.
Study Implications
The most recent guideline from the European Stroke Organization on the use of statins, published in 2013, did not provide a recommendation (“Statins are under study”) for its use in patients with aSAH because of insufficient evidence [34]. These decisions were based on evidence from two small single-center studies. Our work is of great importance in this area. We found evidence suggesting that atorvastatin 20 mg, pravastatin 40 mg, and simvastatin 80 mg reduced the incidence of DCI. Moreover, simvastatin 80 mg reduced mortality risk in patients with aSAH. Our review shows that the beneficial effects of statin therapy were more likely to be accomplished through short-term therapy. These findings provide essential support for further investigation of comparisons between different statin agents and for shortening the duration of statin therapy in RCT design. Our results support a more extensive use of statin therapy following aSAH in the prevention of DCI. Given these new observations, updated guidelines are warranted.
Strengths and Limitations of the Study
The strengths of our study included a comprehensive search encompassing five databases without language restriction, a preregistered protocol, and successfully constructing a network to compare five statin agents. We also used GRADE assessments to evaluate the certainty in effect estimates. Furthermore, this study produced rankings of various statin agents based on computed probabilities according to SUCRA, which is helpful and novel in this field. To confirm the benefit of short-term therapy, differences in treatment effects across the duration of treatment were also investigated in this study. Accordingly, our meta-analyses give a more comprehensive picture of the efficacies of different treatment strategies.
There are several limitations that should be considered. First, there was some heterogeneity in the design and reporting of the included RCTs, as in other meta-analyses. For example, age, definition of outcomes, severity of the disease, agent used, and posttreatment follow-up time were not uniform. However, subgroup analysis or meta-regression could not be performed because of insufficient data. Therefore, interpretations of our findings need to be explained with caution. Although we noticed short-term and low-dose therapy with statin might be associated with reduced risk of DCI. The agent used is also an important consideration to be addressed. However, because of the limitations of insufficient data, it is difficult to perform detailed analyses of a specific agent. Second, there were also nearly 15 years between the first (2005) and most recent (2020) trials, resulting in substantial variabilities, such as differences in drug bioavailability and pharmaceutical manufacturers. Third, future research needs to address this issue, as individual patient characteristics may have a substantial influence on treatment efficacy. Fourth, there was an imbalance in the number of patients included in some comparisons. For instance, only one trial compared pitavastatin 4 mg with a placebo, and two compared atorvastatin 20 mg with placebo. Because these studies did not provide death data, it was impossible to assess the effects of these two classes of drugs on mortality. In addition, the majority of comparison groups consisted of a limited number of studies (one or two studies), making it challenging to reliably evaluate publication bias within each specific comparison group. Fifth, we included a relatively small sample size of RCTs in this study, which should be addressed when designing future trials.
Conclusions
In this analysis, it appears that simvastatin 80 mg and pravastatin 40 mg may exhibit superiority over placebo and simvastatin 40 mg in preventing DCI. Our study suggests that short-term statin therapy might potentially reduce the risk of DCI in patients with aSAH. Given the absence of head-to-head RCTs encompassing all commonly used statin agents for aSAH treatment, our findings serve as a crucial and pragmatic guide for treatment decisions. Further research, featuring extended follow-up periods, is imperative to validate these current findings, especially in high-risk patients with aSAH who are prone to DCI.
References
Macdonald RL, Schweizer TA. Spontaneous subarachnoid haemorrhage. Lancet. 2017;389(10069):655–66.
Bian LH, Liu YF, Nichols LT, et al. Epidemiology of subarachnoid hemorrhage, patterns of management, and outcomes in China: a hospital-based multicenter prospective study. CNS Neurosci Ther. 2012;18(11):895–902.
Yundt KD, Grubb RL Jr, Diringer MN, Powers WJ. Autoregulatory vasodilation of parenchymal vessels is impaired during cerebral vasospasm. J Cereb Blood Flow Metab. 1998;18(4):419–24.
Takeuchi H, Handa Y, Kobayashi H, Kawano H, Hayashi M. Impairment of cerebral autoregulation during the development of chronic cerebral vasospasm after subarachnoid hemorrhage in primates. Neurosurgery. 1991;28(1):41–8.
Roos YB, de Haan RJ, Beenen LF, et al. Complications and outcome in patients with aneurysmal subarachnoid haemorrhage: a prospective hospital based cohort study in the Netherlands. J Neurol Neurosurg Psychiatry. 2000;68(3):337–41.
Frontera JA, Fernandez A, Schmidt JM, et al. Defining vasospasm after subarachnoid hemorrhage: what is the most clinically relevant definition? Stroke. 2009;40(6):1963–8.
Lee H, Perry JJ, English SW, et al. Clinical prediction of delayed cerebral ischemia in aneurysmal subarachnoid hemorrhage. J Neurosurg. 2018;130:1–8.
Shen J, Shen J, Zhu K, et al. Efficacy of statins in cerebral vasospasm, mortality, and delayed cerebral ischemia in patients with aneurysmal subarachnoid hemorrhage: a systematic review and meta-analysis of randomized controlled trials. World Neurosurg. 2019;131:e65-73.
Connolly ES Jr, Rabinstein AA, Carhuapoma JR, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American heart association/American stroke association. Stroke. 2012;43(6):1711–37.
Liu T, Zhong S, Zhai Q, et al. Optimal course of statins for patients with aneurysmal subarachnoid hemorrhage: is longer treatment better? A meta-analysis of randomized controlled trials. Front Neurosci. 2021;15: 757505.
Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med. 2009;151(4):W65-94.
Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343: d5928.
Atkins D, Best D, Briss PA, et al. Grading quality of evidence and strength of recommendations. BMJ. 2004;328(7454):1490.
Toft N, Innocent GT, Gettinby G, Reid SW. Assessing the convergence of Markov Chain Monte Carlo methods: an example from evaluation of diagnostic tests in absence of a gold standard. Prev Vet Med. 2007;79(2–4):244–56.
Salanti G, Ades AE, Ioannidis JP. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol. 2011;64(2):163–71.
Mbuagbaw L, Rochwerg B, Jaeschke R, et al. Approaches to interpreting and choosing the best treatments in network meta-analyses. Syst Rev. 2017;6(1):79.
Chen J, Li M, Zhu X, et al. Atorvastatin reduces cerebral vasospasm and infarction after aneurysmal subarachnoid hemorrhage in elderly Chinese adults. Aging (Albany NY). 2020;12(3):2939–51.
Naraoka M, Matsuda N, Shimamura N, et al. Long-acting statin for aneurysmal subarachnoid hemorrhage: a randomized, double-blind, placebo-controlled trial. J Cereb Blood Flow Metab. 2018;38(7):1190–8.
Diringer MN, Dhar R, Scalfani M, et al. Effect of high-dose simvastatin on cerebral blood flow and static autoregulation in subarachnoid hemorrhage. Neurocrit Care. 2016;25(1):56–63.
Wong GK, Chan DY, Siu DY, et al. High-dose simvastatin for aneurysmal subarachnoid hemorrhage: multicenter randomized controlled double-blinded clinical trial. Stroke. 2015;46(2):382–8.
Kirkpatrick PJ, Turner CL, Smith C, Hutchinson PJ, Murray GD. Simvastatin in aneurysmal subarachnoid haemorrhage (STASH): a multicentre randomised phase 3 trial. Lancet Neurol. 2014;13(7):666–75.
Garg K, Sinha S, Kale SS, et al. Role of simvastatin in prevention of vasospasm and improving functional outcome after aneurysmal sub-arachnoid hemorrhage: a prospective, randomized, double-blind, placebo-controlled pilot trial. Br J Neurosurg. 2013;27(2):181–6.
Li X. Efficacy of atorvastatin in preventing symptomatic cerebral vasospasm after subarachnoid hemorrhage. China Tropical Med. 2010;10(7):865–6.
Vergouwen MD, Meijers JC, Geskus RB, et al. Biologic effects of simvastatin in patients with aneurysmal subarachnoid hemorrhage: a double-blind, placebo-controlled randomized trial. J Cereb Blood Flow Metab. 2009;29(8):1444–53.
Macedo S, Bello Y, Silva A, et al. Effects of simvastatin in prevention of vasospasm in nontraumatic subarachnoid hemorrhage: preliminary data. Crit Care. 2009;13(Suppl 1):315.
Jaschinski U, Scherer K, Lichtwarck M, Forst H. Impact of treatment with pravastatin on delayed ischemic disease and mortality after aneurysmal subarachnoid hemorrhage. Crit Care. 2008;12(2):1–2.
Chou SH, Smith EE, Badjatia N, et al. A randomized, double-blind, placebo-controlled pilot study of simvastatin in aneurysmal subarachnoid hemorrhage. Stroke. 2008;39(10):2891–3.
Tseng MY, Czosnyka M, Richards H, Pickard JD, Kirkpatrick PJ. Effects of acute treatment with statins on cerebral autoregulation in patients after aneurysmal subarachnoid hemorrhage. Neurosurg Focus. 2006;21(3):E10.
Lynch JR, Wang H, McGirt MJ, et al. Simvastatin reduces vasospasm after aneurysmal subarachnoid hemorrhage: results of a pilot randomized clinical trial. Stroke. 2005;36(9):2024–6.
To MS, Prakash S, Poonnoose SI, Bihari S. Dose-dependent effects of statins for patients with aneurysmal subarachnoid hemorrhage: meta-regression analysis. World Neurosurg. 2018;113:153–62.
Bohara S, Gaonkar VB, Garg K, et al. Effect of statins on functional outcome and mortality following aneurysmal subarachnoid haemorrhage—results of a meta-analysis, metaregression and trial sequential analysis. Clin Neurol Neurosurg. 2021;207: 106787.
Vergouwen MD, de Haan RJ, Vermeulen M, Roos YB. Effect of statin treatment on vasospasm, delayed cerebral ischemia, and functional outcome in patients with aneurysmal subarachnoid hemorrhage: a systematic review and meta-analysis update. Stroke. 2010;41(1):e47-52.
Wetterslev J, Jakobsen JC, Gluud C. Trial sequential analysis in systematic reviews with meta-analysis. BMC Med Res Methodol. 2017;17(1):39.
Steiner T, Juvela S, Unterberg A, et al. European stroke organization guidelines for the management of intracranial aneurysms and subarachnoid haemorrhage. Cerebrovasc Dis. 2013;35(2):93–112.
Funding
This research was supported by the National Natural Science Foundation of China (Grant No. 82371318) and Sichuan Provincial Natural Science Foundation (Grant No. 2023NSFSC1564).
Author information
Authors and Affiliations
Contributions
XW, LM, and CY designed the meta-analysis, XW and QG searched for relevant studies, XW and QG selected the studies, extracted the relevant information, XW and QG synthesized the data, and XW wrote the first draft of the article. All authors revised the manuscript and approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical Approval
Ethical approvals (institutional review board) are not applicable for this type of article because this article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, X., Gan, Q., You, C. et al. Effect of Statin Treatment in Patients with Aneurysmal Subarachnoid Hemorrhage: A Network Meta-Analysis. Neurocrit Care 41, 49–58 (2024). https://doi.org/10.1007/s12028-024-01957-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-024-01957-9